Abstract
Background
Standardization of evidence‐based medical therapies has improved outcomes for patients with non–ST‐segment–elevation myocardial infarction (NSTEMI). Although racial differences in NSTEMI management have previously been reported, it is uncertain whether these differences have been ameliorated over time.
Methods and Results
The ARIC (Atherosclerosis Risk in Communities) Community Surveillance study conducts hospital surveillance of acute myocardial infarction in 4 US communities. NSTEMI was classified by physician review, using a validated algorithm. From 2000 to 2014, 17 755 weighted hospitalizations for NSTEMI (patient race: 36% black, 64% white) were sampled by ARIC. Black patients were younger (aged 60 versus 66 years), more often female (45% versus 38%), and less likely to have medical insurance (88% versus 93%) but had more comorbidities. Black patients were less often administered aspirin (85% versus 92%), other antiplatelet therapy (45% versus 60%), β‐blockers (85% versus 88%), and lipid‐lowering medications (68% versus 76%). After adjustments, black patients had a 24% lower probability of receiving nonaspirin antiplatelets (relative risk: 0.76; 95% confidence interval, 0.71–0.81), a 29% lower probability of angiography (relative risk: 0.71; 95% confidence interval, 0.67–0.76), and a 45% lower probability of revascularization (relative risk: 0.55; 95% confidence interval, 0.50–0.60). No suggestion of a changing trend over time was observed for any NSTEMI therapy (P values for interaction, all >0.20).
Conclusions
This longitudinal community surveillance of hospitalized NSTEMI patients suggests black patients have more comorbidities and less likelihood of receiving guideline‐based NSTEMI therapies, and these findings persisted across the 15‐year period. Focused efforts to reduce comorbidity burden and to more consistently implement guideline‐directed treatments in this high‐risk population are warranted.
Keywords: guideline adherence, myocardial infarction, quality of care, race
Subject Categories: Race and Ethnicity, Epidemiology, Health Services
Clinical Perspective
What Is New?
In this community‐based surveillance of patients hospitalized with non–ST‐segment–elevation myocardial infarction over a 15‐year period, black patients were younger and had more medical comorbidities than white patients
In comparison to white patients, black patients had less likelihood of receiving guideline‐based non–ST‐segment–elevation myocardial infarction therapies, including invasive angiography and revascularization.
Racial differences in management persisted across the 15‐year period.
What Are the Clinical Implications?
Focused efforts are required to ameliorate the comorbidity burden in black communities by implementing population‐based policies to influence health behavior.
Measures for more consistent implementation of guideline‐directed treatments in the black population are warranted.
Introduction
In the United States, black adults have the highest burden of cardiovascular diseases, and this contributes to a wide disparity in life expectancy relative to white adults.1, 2 Some of this burden is attributable to the preponderance of cardiometabolic risk factors, such as diabetes mellitus, hypertension, obesity, and dyslipidemia among the black population.3 However, other important factors, such as socioeconomics, contribute to these observed disparities in health.3 In response, the American Heart Association (AHA) recently released a scientific statement emphasizing the need for new strategies to promote better cardiovascular health in the African American community.1 Beyond variation in overall risk factor and disease burden in the community, acute management of cardiovascular diseases, such as non–ST‐segment–elevation myocardial infarction (NSTEMI), may also vary by race. Unlike ST‐segment–elevation myocardial infarction (MI), which is primarily managed by protocol‐driven strategies, management of NSTEMI may depend more heavily on the treating physician or health system.4 Previous studies suggest lower utilization of invasive procedures in black patients and racial differences in medical management of NSTEMI.3, 4, 5, 6, 7, 8, 9, 10, 11 Although these differences are well documented, it is unknown whether these disparities have been mitigated or have worsened over time. Most prior evaluations have relied on administrative claims data rather than direct chart abstraction,12 and few have evaluated racial trends over time. International Classification of Diseases (ICD) coding practices have varied over time and also exhibit geographic heterogeneity. The ARIC (Atherosclerosis Risk in Communities) Community Surveillance study classifies NSTEMI by physician review and a standardized algorithm that has not changed since 1987, allowing a unique opportunity to investigate management trends among black and white patients hospitalized with NSTEMI.
Methods
ARIC Community Surveillance Study
The ARIC study's data and materials are publicly available.13, 14 Since 1987, the ARIC study has conducted community surveillance of hospitalizations for MI in 4 geographically defined regions of the United States (Forsyth County, North Carolina; Washington County, Maryland; Jackson, Mississippi; and 8 northwest suburbs of Minneapolis, Minnesota). All surveillance protocols were approved by local institutional review boards. Informed consent was not required because all data were anonymized by redacting personal identifiers. As described previously,15, 16 eligible hospitalizations were selected on the basis of age (35–74 years from 1987–2004 and 35–84 years from 2005 onward), residence in the community, and discharge ICD, Ninth Revision, Clinical Modification (ICD‐9) codes 402, 410 to 414, 427, 428 and 518.4. Hospitalizations were selected by random sampling within strata of ICD‐9 codes and demographic groups based on race and sex. For the purposes of this analysis, hospital surveillance was limited to white and black patients discharged from January 1, 2000, to December 31, 2014.
Clinical Covariates and Demographic Data
Clinical and demographic data were collected from the hospital records by trained abstractors using physician notes, laboratory reports, patient histories, and discharge summaries. Patient race was abstracted from the medical history. Diabetes mellitus was defined as documented history of diabetes mellitus or glucose‐lowering therapy use. Hypertension was defined as documented hypertension, systolic blood pressure ≥140 mm Hg, or diastolic blood pressure ≥90 mm Hg. Acute heart failure or pulmonary edema was abstracted if noted in the physical examination or chest radiography. Cardiogenic shock was recorded if documented at admission or within 24 hours of symptom onset. Ventricular fibrillation and cardiac arrest were recorded if documented in the progress notes, medical record, or discharge summary.
Electrocardiography
The first, third, and last 12‐lead ECGs over the course of hospitalization were obtained from the medical record and coded electronically at the Minneapolis ECG Reading Center.17 For the purposes of this analysis, patients identified with ST‐segment elevations were excluded.
Chest Pain
Presence of chest pain was abstracted from the medical record. Any mention of substernal pressure, tightness, or pain precipitated by exertion or excitement was considered evidence of chest pain of cardiac origin. Chest pain starting after hospitalization was considered evidence of hospital‐onset MI, and cases were excluded from the analysis.
Acute MI Classification
As described previously,16, 17 events were classified by the ARIC study as definite, probable, suspect, or no MI, based on ECG evidence (evolving diagnostic, diagnostic, evolving ST‐T wave changes, equivocal, or absent/uncodable), presence of chest pain, and cardiac biomarkers (which were considered abnormal if ≥2× the upper limit of normal and equivocal if exceeding but <2× the upper limit of normal).12 Classification criteria remained constant over the study period and is detailed in the ARIC Study surveillance manual.18 To qualify as definite or probable NSTEMI, one of the following conditions in the absence of ST‐segment elevation was required: 1) diagnostic ECG pattern and abnormal biomarkers, 2) cardiac pain and abnormal biomarkers, 3) cardiac pain and equivocal biomarkers with evolving ST‐T wave pattern or diagnostic ECG pattern, or 4) abnormal biomarkers with evolving ST‐T wave pattern.16
Biomarkers
Laboratory values for biomarkers of cardiac injury were recorded for the first 4 days of hospitalization. The laboratory‐specified upper limit of normal was recorded, and biomarker values were abstracted chronologically, recording up to 3 measurements per day.
Medical Therapies
Medications were recorded if administered during the course of hospitalization or prescribed at hospital discharge. Aspirin required routine rather than pro re nata administration for abstraction. Nonaspirin antiplatelet therapy was recorded as a single category and included P2Y12 inhibitors (cangrelor, clopidogrel, prasugrel, ticagrelor, ticlopidine), glycoprotein IIb/IIIa inhibitors (abciximab, eptifibatide, tirofiban, xemilofiban), phosphodiesterase type 3 inhibitors (cilostazol), phosphodiesterase type 5 inhibitors (dipyridamole), and protease‐activated receptor 1 (PAR‐1) antagonists (vorapaxar). β‐Blockers included β1 adrenergic antagonists. Angiotensin‐converting enzyme inhibitors and angiotensin II receptor blockers were recorded as a single category. Lipid‐lowering agents included statins, niacin, and fibrates.
Procedures
Echocardiography, stress testing, angiography, and revascularization procedures were abstracted from the medical record. Echocardiography included transthoracic and transesophageal echocardiograms. Stress testing included exercise testing (treadmill or bicycle ergometer), stress echocardiography, cardiac stress magnetic resonance imaging, and nuclear stress tests. Revascularization included percutaneous coronary intervention or coronary artery bypass grafting surgery.
Mortality Outcomes
All‐cause mortality outcomes were ascertained for all patients by linking hospitalizations with the National Death Index.
Statistical Analysis
All statistical analyses were carried out using SAS 9.4 (SAS Institute). Statistical tests and models accounted for the stratified sampling design and were weighted by the inverse of the sampling probability because sampling fractions varied across the sampling strata.19 Continuous variables were assessed for normality and compared using the difference in least square means from weighted linear regression. Categorical variables were compared using Rao‐Scott χ2 tests. The relative probability of black versus white patients receiving NSTEMI medications (aspirin, other antiplatelets, β‐blockers, and lipid‐lowering medications) or undergoing invasive procedures (angiography and revascularization) were compared in yearly and in aggregate (2000–2014) analyses. Associations were derived from multivariable logistic regression, with odds ratios converted into relative risks and 95% confidence intervals.20 Racial differences in posthospitalization mortality (28‐day and 1‐year) were analyzed with multivariable Cox regression. Modeling decisions were made a priori, with adjustment for variables routinely abstracted from the medical record. Models for NSTEMI therapies were adjusted for demographics (age, sex, geographic region, year of admission), and comorbidities and clinical course (diabetes mellitus, acute heart failure or pulmonary edema, cardiogenic shock, and ventricular fibrillation or cardiac arrest). Models for mortality outcomes were additionally adjusted for medications (aspirin, other antiplatelet agents, β‐blockers, angiotensin‐converting enzyme inhibitors and angiotensin II receptor blockers, and lipid‐lowering agents) and revascularization. Annual trends in medical management were visualized by plotting the adjusted relative probabilities of black versus white patients receiving recommended therapies21 each year from 2000 to 2014. Significant changes in annual relative probabilities across 2000–2014 were analyzed by modeling the multiplicative interaction between race and calendar year of hospital admission.
Several sensitivity analyses were also conducted. Racial differences in NSTEMI management were compared within each of the 4 ARIC communities and among patients known to have medical insurance. We also conducted a sensitivity analysis excluding patients with previous MI because guideline‐directed therapies may have been initiated before the hospital visit under surveillance. Because the ARIC Community Surveillance study uses a standardized, physician‐adjudicated definition of NSTEMI that has not changed since 1987, we were able to examine trends over time; however, discrepancies may exist between the ARIC classification of NSTEMI and the treating physician's diagnosis. Consequently, we also examined racial differences in patients classified with definite NSTEMI (excluding cases of probable NSTEMI), in patients discharged with a primary ICD‐9 code of 410 to 414, and in the subset of patients not presenting with acute heart failure or pulmonary edema.
Results
All presented results are weighted by the inverse of the sampling probability.19 From January 1, 2000, to December 31, 2014, 8060 hospitalizations for definite or probable NSTEMI were sampled by the ARIC Community Surveillance study, corresponding to 17 755 weighted events. Of these, 36% of the patients were black. As shown in Table 1, black patients were younger (aged 60 versus 66 years) and more often female (45% versus 38%) but less likely to have medical insurance (88% versus 93%). History of diabetes mellitus (50% versus 37%), chronic kidney disease (38% versus 29%), and stroke (16% versus 10%) were more prevalent among black patients, but history of prior MI was comparable to white patients (30% versus 32%). During the hospital stay, acute pulmonary edema or congestive heart failure was more common in black patients (41% versus 29%). In contrast, cardiogenic shock (2% versus 4%) and ventricular fibrillation or cardiac arrest were less common (5% versus 7%). Overall, black patients were less likely than white patients to be transferred to or from another hospital (1% versus 8%). As shown in Table S1, comparisons of demographic factors, comorbidities, and in‐hospital clinical courses were consistent when analyzed at 5‐year intervals of 2000–2004, 2005–2009, and 2010–2014.
Table 1.
Baseline Characteristics of Black and White Patients Hospitalized With NSTEMI; ARIC Community Surveillance Study, 2000–2014
| Black Patients (n=6343) | White Patients (n=11 412) | P Value | |
|---|---|---|---|
| Demographics | |||
| Age, y | 60±0.3 | 66±0.2 | <0.0001 |
| Female | 2834 (45) | 4324 (38) | <0.0001 |
| Geographic location | |||
| Forsyth County, NC | 2507 (40) | 4647 (41) | <0.0001 |
| Jackson, MS | 3113 (49) | 1025 (9) | |
| Minneapolis, MN | 624 (10) | 3664 (32) | |
| Washington, MD | 99 (2) | 2077 (19) | |
| Medical insurancea | 4427 (88) | 7887 (93) | <0.0001 |
| Year of hospitalization | 2009±0.1 | 2008±0.1 | <0.0001 |
| Medical history | |||
| Current smoker | 2299 (36) | 3286 (29) | <0.0001 |
| Diabetes mellitus | 3169 (50) | 4258 (37) | <0.0001 |
| Chronic kidney diseaseb | 1980 (38) | 2579 (29) | <0.0001 |
| Prior MI | 1890 (30) | 3615 (32) | 0.3 |
| Prior angioplasty | 1326 (21) | 2880 (25) | 0.001 |
| Prior CABG | 726 (11) | 2399 (21) | <0.0001 |
| Valvular heart disease/cardiomyopathy | 1718 (27) | 2225 (20) | <0.0001 |
| Stroke | 1002 (16) | 1162 (10) | <0.0001 |
| Hospital visit | |||
| Chest pain | 5110 (81) | 9477 (83) | 0.07 |
| Elevated enzymes (>2× ULN) | 6332 (99.8) | 11 242 (98.5) | <0.0001 |
| ST‐segment depression | 4135 (65) | 7168 (63) | 0.1 |
| Ventricular fibrillation/cardiac arrest | 341 (5) | 791 (7) | 0.02 |
| Acute pulmonary edema/heart failure | 2595 (41) | 3302 (29) | <0.0001 |
| Cardiogenic shock | 143 (2) | 407 (4) | 0.0009 |
| Weekend admission | 1627 (26) | 2928 (26) | 1.0 |
| Transferred to/from other hospital | 71 (1) | 914 (8) | <0.0001 |
Data are shown as mean±SEM or n (%). ARIC indicates Atherosclerosis Risk in Communities; CABG, coronary artery bypass grafting; MI, myocardial infarction; NSTEMI, non–ST‐segment–elevation myocardial infarction; ULN, upper limit of normal.
Medical insurance not routinely abstracted before 2005 and based on a subset (n=13 505) of patients.
Serum creatinine not routinely abstracted before 2005. Chronic kidney disease defined by estimated glomerular filtration rate <45 mL/min/1.73 m2 by the Chronic Kidney Disease Epidemiology Collaboration equation, in a subset (n=14 309) of patients with available creatinine assessments or receipt of hemodialysis.
In the aggregate, black patients were less often administered aspirin (85% versus 92%), nonaspirin antiplatelet therapy (45% versus 60%), β‐blockers (85% versus 88%), and lipid‐lowering medications (68% versus 76%) and were less likely to undergo invasive angiography (45% versus 61%) or revascularization (25% versus 45%; Figure 1. However, black patients were more commonly administered angiotensin‐converting enzyme inhibitors and angiotensin II receptor blockers (67% versus 61%) and were more often imaged by echocardiography during the hospitalization (67% versus 58%). The percentage of patients undergoing stress testing was comparable for both races (7% for both). Although the proportion of black patients varied across the 4 ARIC communities, similar race‐specific patterns in NSTEMI management were observed in all communities (Table S2). Guideline‐directed medications were more balanced between races in patients undergoing coronary revascularization (n=6700; Table S3).
Figure 1.
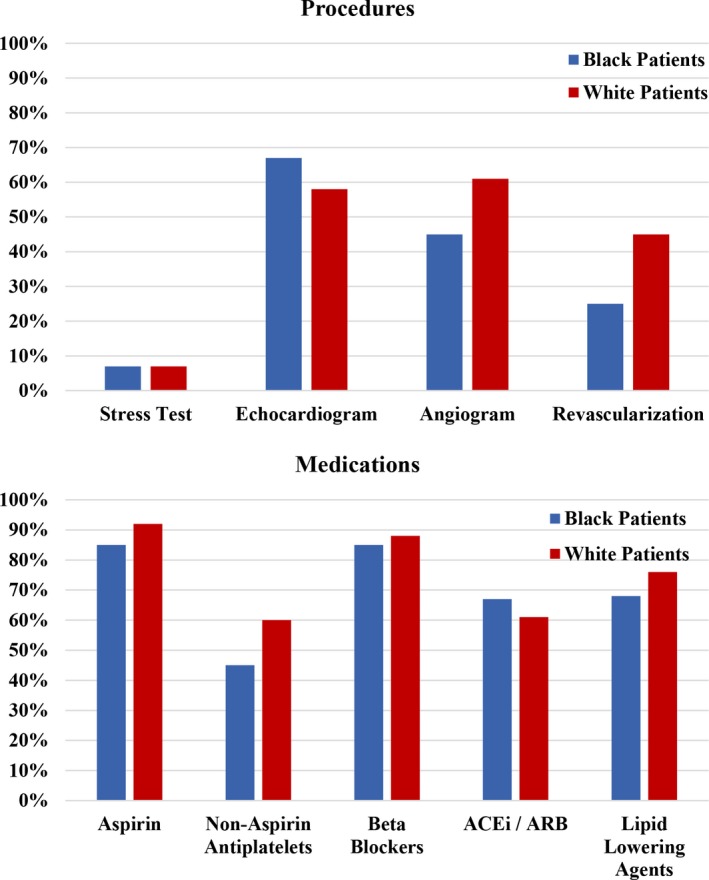
Distributions of various guideline‐directed medications and therapies, stratified by black and white patients hospitalized with non–ST‐segment–elevation myocardial infarction. ACEi indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
After accounting for demographics, year of admission, and comorbidities and clinical course, black patients had a 24% lower probability of receiving nonaspirin antiplatelet therapy, a 9% lower probability of receiving lipid‐lowering agents, a 6% lower probability of receiving aspirin, a 29% lower probability of undergoing angiography, and a 45% lower probability of revascularization, when aggregated across 2000–2014 (Figure 2). Racial differences in NSTEMI management persisted in several sensitivity analyses (Tables S4–S8). When subdivided by ARIC community, the risk‐adjusted probability of receiving an invasive strategy remained consistently lower for black patients, although some heterogeneity across geographic regions was evident (Table S9).
Figure 2.
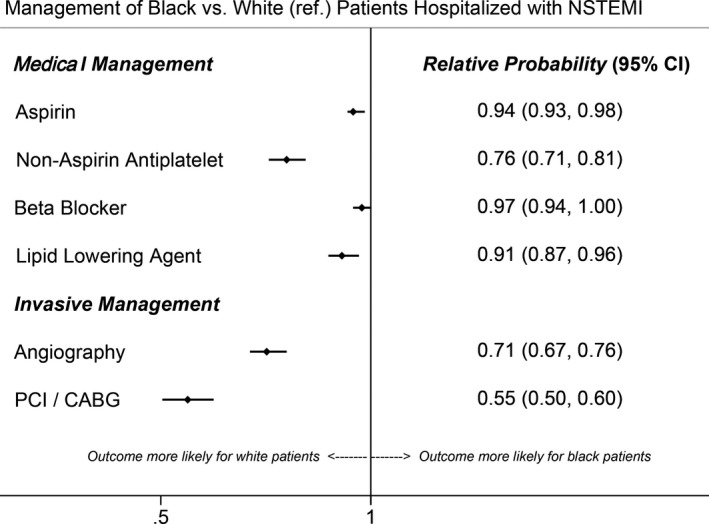
Risk‐adjusted relative probabilities of black vs white patients receiving various evidenced‐based therapies for non–ST‐segment–elevation myocardial infarction (NSTEMI). Models adjusted for demographics (age, sex, hospital geographic location [Forsyth County, NC; Jackson, MS; Minneapolis, MN; Washington County, MD] and year of admission) and comorbidities and clinical course (diabetes mellitus, acute heart failure/pulmonary edema, cardiogenic shock, and ventricular fibrillation/cardiac arrest]. CABG indicates coronary artery bypass grafting; CI, confidence interval; PCI, percutaneous coronary intervention.
The annual percentages of black and white patients receiving evidence‐based NSTEMI therapies are shown in Figure 3. When analyzed across 5‐year intervals (2000–2004, 2005–2009, and 2010–2014), the risk‐adjusted relative probabilities of evidence‐based NSTEMI therapies remained consistently lower for black compared with white patients (Table 2). No suggestion of a changing trend over time was observed for any NSTEMI therapy (P values for interaction, all >0.20).
Figure 3.
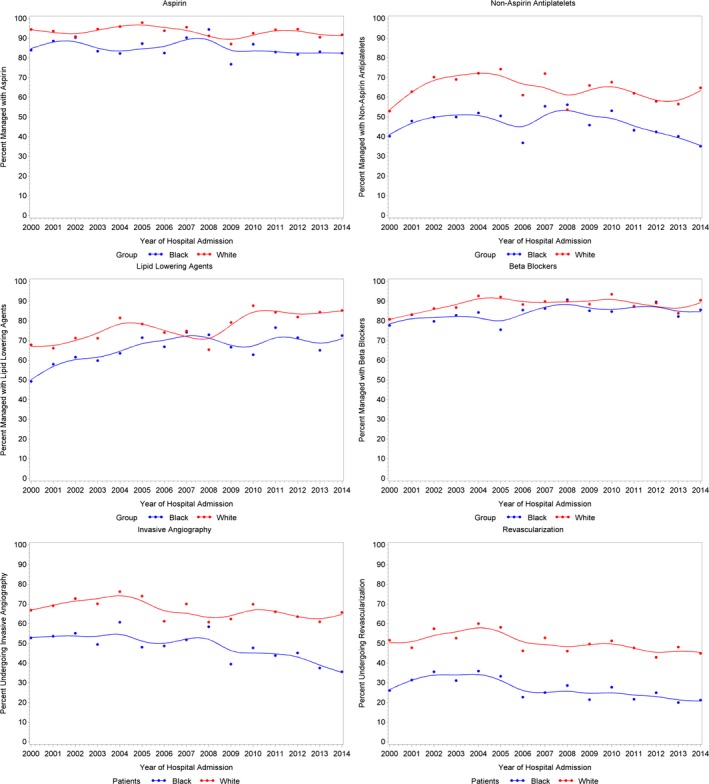
Annual percentages of black and white patients receiving various evidenced‐based therapies for non–ST‐segment–elevation myocardial infarction. Annual percentages are limited to patients aged 35 to 74 years.
Table 2.
Risk‐Adjusted Relative Probabilities of Black vs White Patients Receiving Various Therapies for NSTEMI: ARIC Community Surveillance Study, 2000–2014
| NSTEMI Therapies | 2000–2004 | 2005–2009 | 2010–2014 | Trenda |
|---|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | P Value | |
| Medical management | ||||
| Aspirin | 0.93 (0.90–0.99) | 0.96 (0.92–1.02) | 0.96 (0.92–1.02) | 0.7 |
| Nonaspirin antiplatelet | 0.76 (0.69–0.86) | 0.78 (0.71–0.86) | 0.75 (0.68–0.84) | 0.3 |
| β‐Blocker | 0.99 (0.93–1.09) | 0.97 (0.93–1.04) | 0.96 (0.93–1.02) | 0.9 |
| Lipid‐lowering agent | 0.80 (0.75–0.88) | 0.99 (0.91–1.10) | 0.92 (0.86–0.99) | 0.4 |
| Invasive management | ||||
| Angiography | 0.75 (0.70–0.83) | 0.76 (0.69–0.84) | 0.67 (0.61–0.74) | 0.8 |
| Revascularization | 0.60 (0.53–0.680 | 0.55 (0.48–0.64) | 0.52 (0.46–0.60) | 0.7 |
Models adjusted for demographics [age, sex, hospital geographic location (Forsyth County, NC; Jackson, MS; Minneapolis, MN; Washington County, MD) and year of admission] and comorbidities and clinical course (diabetes mellitus, acute heart failure/pulmonary edema, cardiogenic shock, and ventricular fibrillation/cardiac arrest). ARIC indicates Atherosclerosis Risk in Communities; CI, confidence interval; NSTEMI, non–ST‐segment–elevation myocardial infarction; RR, relative risk.
Annual trends derived from aggregate risk‐adjusted model (2000–2014), testing the multiplicative interaction between race and calendar year of admission.
Overall, 480 deaths occurred in hospital, 1187 deaths occurred within 28 days, and 2619 deaths occurred within 1 year of hospitalization. Unadjusted all‐cause mortality was comparable for black and white patients, whether in hospital (2% versus 3%), at 28 days (6% versus 7%), or at 1 year of follow‐up (15% for each). After adjustments for demographics, year of admission, comorbidities and clinical course, medications, and revascularization, the postdischarge hazard of death was comparable for black relative to white patients, both at 28 days (hazard ratio: 1.10; 95% confidence interval, 0.83–1.45) and 1 year (hazard ratio: 1.05; 95% confidence interval, 0.85–1.32).
Discussion
In this community‐based surveillance of patients hospitalized with NSTEMI from 2000 to 2014 black patients (1) were more likely to be younger and female and to have more comorbidities than white patients, (2) were less likely to receive evidence‐based NSTEMI therapies (ie, aspirin, lipid‐lowering agents, and nonaspirin antiplatelets), and 3) were less likely to undergo invasive angiography and revascularization. Unfortunately, despite standardization of evidence‐based therapies, persistent differences were observed over the15‐year period from 2000 to 2014, with no significant changes in trends over time. However, postdischarge mortality was similar for black and white patients, as was administration of medical therapies among the subset undergoing coronary revascularization.
Racial comparisons of patients presenting with NSTEMI have previously been described and are largely consistent with the population from the ARIC Community Surveillance study.3, 11 The younger age at presentation for black patients likely stems from the earlier onset of cardiovascular risk factors.1, 22, 23 In support of this, we observed more prevalent smoking, diabetes mellitus, chronic kidney disease, and history of stroke in black patients presenting with NSTEMI. Similarly, a higher prevalence of cardiovascular comorbidities was reported in black patients from 400 US hospitals participating in the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC (American College of Cardiology)/AHA Guidelines (CRUSADE) registry.11 Higher rates of cardiovascular disease and fatal coronary heart disease in black patients were also noted in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) cohort.24 Of concern is a recent analysis from the ARIC Cohort study that reported widening racial differences in coronary risk factors for individuals from the general population who were followed longitudinally from 1987 to 2013.25
In the ARIC Community Surveillance study, black patients underwent invasive procedures less frequently and were less likely to receive evidence‐based NSTEMI medications—findings that are consistent with multiple prior studies.3, 4, 5, 6, 7, 8, 9, 10, 11 However, the prolonged follow‐up in the ARIC Community Surveillance study uniquely allows an evaluation of contemporary trends, which are useful for assessing the impact of quality initiatives. Unfortunately, the differences in nonaspirin antiplatelet therapy, lipid‐lowering medications, invasive angiography, and revascularization seem to have persisted from 2000 to 2014. The underlying reasons for the observed racial differences in NSTEMI management are likely multifactorial. Black patients may compose a sicker population, a category less likely to undergo an invasive strategy and for which evidence‐based treatments are systematically underutilized.23, 26, 27 However, the associations in the ARIC Community Surveillance study remained significant after accounting for comorbid conditions and in‐hospital clinical course.
Another potential explanation for the disparity in guideline‐directed therapies may be greater incidence of type 2 MI in black patients, given their greater comorbidity burden. However, racial differences in NSTEMI management remained after excluding patients with acute heart failure or pulmonary edema, when limiting the analysis to patients with definite NSTEMI, and for those with a primary discharge ICD‐9 code of 410–414. We also observed that black patients were less often insured than white patients. This may have affected clinical decision making by both the patients and the physicians, although the lower utilization of NSTEMI therapies persisted in a sensitivity analysis limited to patients with known medical insurance. Another explanation for the observed differences in NSTEMI management may be that black populations are concentrated in geographic areas with lower access to care than their white counterparts. Although access to percutaneous and surgical revascularization has continued to expand in recent years, geographical imbalances remain.28 However, we observed a consistent pattern of racial differences in NSTEMI management across the 4 ARIC communities.
Although these differences in use of evidence‐based therapies and utilization of invasive strategy are concerning, the rates of postdischarge mortality among black and white patients did not differ. Whether this is attributable to equalization of care following discharge is uncertain. An analysis of 443 hospitals participating in Get With The Guidelines–Coronary Artery Disease program reported a reduction or elimination of racial and ethnic differences in post‐MI care.29 The ARIC Community Surveillance study, however, does not follow patients after discharge except for all‐cause mortality outcomes, and we were unable to examine racial differences in post‐MI care. Encouragingly, among the patients undergoing coronary revascularization, medications were similarly administered, regardless of race. This likely reflects national standardization of postrevascularization care, supporting the role of protocol‐driven care for the mitigation of racial disparities in NSTEMI management.30
The Centers for Medicare and Medicaid Services Hospital Inpatient Quality Reporting program measures and publicly reports quality of care for acute coronary syndromes, which has led to improved outcomes for patients regardless of race.31 Nevertheless, measures focused on tackling the disproportionately high cardiovascular disease burden among black patients and the lower utilization of evidence‐based therapies are needed. Dedicated industry‐based and federal efforts, such as the PLATINUM Diversity study, have gained momentum recently in identifying evidence‐based interventions to improve clinical outcomes of racial‐ and ethnic‐minority patients.32 Recent reports suggest the burden of cardiovascular disease may be ameliorated by improving socioeconomic status in black communities.33 In addition, ample evidence suggests that population‐based strategies to influence health behavior may improve cardiovascular risk in the black population.1 These strategies should include a population approach to improve physical activity, diet, and smoking habits.34
Our study has several limitations. The ARIC Community Surveillance study is localized to 4 US communities and may not be generalizable to the entire nation. The majority (89%) of black patients included in the ARIC Community Surveillance study were sampled from North Carolina and Mississippi. Clinical data were limited by availability in the medical record and abstraction priority. Granular data regarding angiographic outcomes were not available for analysis. Serum creatinine and medical insurance status were not routinely abstracted until 2005 and were missing for 31% and 19% of the hospitalizations, respectively. The fact that we did not observe any racial differences in long‐term all‐cause mortality is reassuring; however, we were not able to compare other important longitudinal outcomes, such as recurrent MI, need for revascularization, or cardiovascular death. Our study also has several noteworthy strengths. The ARIC Community Surveillance study provides large multiyear surveillance of 4 diverse US communities. Clinical and laboratory values were meticulously collected by certified abstractors following standardized protocols. NSTEMI was classified using consistent criteria based on standardized physician review of the medical record, thus allowing an analysis of trends spanning several decades. Mortality outcomes were verified by the National Death Index. These protocols support greater standardization of these observational data.
Conclusion
In this community‐based surveillance of black and white patients hospitalized with NSTEMI from 2000 to 2014, black patients were younger, had more medical comorbidities, and were less likely to undergo revascularization or be discharged on evidence‐based medications. Despite measures to standardize NSTEMI care, differences have persisted between black and white patients during this time interval. Overall reduction in comorbidity burden and consistent implementation of guideline‐directed strategies are crucial to mitigate racial disparities in NSTEMI management.
Sources of Funding
The ARIC (Atherosclerosis Risk in Communities) study is carried out as a collaborative study supported by NHLBI (National Heart, Lung, and Blood Institute) contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C).
Disclosures
Dr Vaduganathan is supported by the NHLBI T32 postdoctoral training grant (T32HL007604). Dr Qamar is supported by the NHLBI T32 postdoctoral training grant (T32HL007604) and the American Heart Association Strategically Focused Research Network in Vascular Disease grant (18SFRN3390085). Dr Bhatt discloses the following relationships—Advisory Board: Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Cleveland Clinic, Duke Clinical Research Institute, Harvard Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine, Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice‐Chair, ACC Accreditation Committee), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), Harvard Clinical Research Institute (clinical trial steering committee), HMP Communications (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Population Health Research Institute (clinical trial steering committee), Slack Publications (Chief Medical Editor, Cardiology Today's Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR‐ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Amarin, Amgen, AstraZeneca, Bristol‐Myers Squibb, Chiesi, Eisai, Ethicon, Forest Laboratories, Ironwood, Ischemix, Lilly, Medtronic, Pfizer, Roche, Sanofi Aventis, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald's Heart Disease); Site Co‐Investigator: Biotronik, Boston Scientific, St. Jude Medical (now Abbott); Trustee: American College of Cardiology; Unfunded Research: FlowCo, Merck, PLx Pharma, Takeda. The remaining authors have no disclosures to report.
Supporting information
Table S1. Characteristics of Black and White Patients Hospitalized With Non–ST‐Segment–Elevation Myocardial Infarction; ARIC (Atherosclerosis Risk in Communities) Community Surveillance Study, 2000–2014
Table S2. Medical Management of Black and White Patients Hospitalized With Non–ST‐Segment–Elevation Myocardial Infarction From 2000–2014, Stratified by ARIC Community
Table S3. Various Medications and Procedures Administered to Black and White Patients Undergoing Coronary Revascularization During Hospitalization for Non–ST‐Segment–Elevation Myocardial Infarction (n=6700)
Table S4. Risk‐Adjusted Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction Therapies Among Black vs White (Reference) Patients Known to Have Health Insurance (n=12 314)
Table S5. Risk‐Adjusted Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction Therapies Among Black vs White (Reference) Patients Not Presenting With Acute Heart Failure/Pulmonary Edema (n=11 858)
Table S6. Risk‐Adjusted Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction Therapies Among Black vs White (Reference) Patients Presenting With First‐Occurring Acute Myocardial Infarction (n=12 250)
Table S7. Risk‐Adjusted Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction (NSTEMI) Therapies Among Black vs White (Reference) Patients Classified With Definite NSTEMI (n=9688)
Table S8. Risk‐Adjusted* Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction Therapies Among Black vs White (Reference) Patients Discharged With International Classification of Diseases, 9th Revision, Clinical Modification codes 410 to 414 (n=9165)
Table S9. Risk‐Adjusted Relative Probabilities of Invasive Strategy Among Black vs White (Reference) Patients Hospitalized With Non–ST‐Segment–Elevation Myocardial Infarction, Stratified by Geographic Region; ARIC (Atherosclerosis Risk in Communities) Community Surveillance Study, 2000–2014
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions.
(J Am Heart Assoc. 2018;7:e010203 DOI: 10.1161/JAHA.118.010203.)
References
- 1. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA Jr, Willis M, Yancy CW; American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology ; and Stroke Council. Cardiovascular Health in African Americans: a Scientific Statement from the American Heart Association. Circulation. 2017;136:e393–e423. [DOI] [PubMed] [Google Scholar]
- 2. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics‐2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Graham G. Racial and ethnic differences in acute coronary syndrome and myocardial infarction within the United States: from demographics to outcomes. Clin Cardiol. 2016;39:299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. LaVeist TA, Morgan A, Arthur M, Plantholt S, Rubinstein M. Physician referral patterns and race differences in receipt of coronary angiography. Health Serv Res. 2002;37:949–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329:621–627. [DOI] [PubMed] [Google Scholar]
- 6. Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269:2642–2646. [PubMed] [Google Scholar]
- 7. Peterson ED, Wright SM, Daley J, Thibault GE. Racial variation in cardiac procedure use and survival following acute myocardial infarction in the Department of Veterans Affairs. JAMA. 1994;271:1175–1180. [PubMed] [Google Scholar]
- 8. Peterson ED, Shaw LK, DeLong ER, Pryor DB, Califf RM, Mark DB. Racial variation in the use of coronary‐revascularization procedures: are the differences real? Do they matter? N Engl J Med. 1997;336:480–486. [DOI] [PubMed] [Google Scholar]
- 9. Chen MS, Bhatt DL, Chew DP, Moliterno DJ, Ellis SG, Topol EJ. Outcomes in African Americans and whites after percutaneous coronary intervention. Am J Med. 2005;118:1019–1025. [DOI] [PubMed] [Google Scholar]
- 10. Chen J, Rathore SS, Radford MJ, Wang Y, Krumholz HM. Racial differences in the use of cardiac catheterization after acute myocardial infarction. N Engl J Med. 2001;344:1443–1449. [DOI] [PubMed] [Google Scholar]
- 11. Sonel AF, Good CB, Mulgund J, Roe MT, Gibler WB, Smith SC Jr, Cohen MG, Pollack CV Jr, Ohman EM, Peterson ED; CRUSADE Investigators . Racial variations in treatment and outcomes of black and white patients with high‐risk non‐ST‐elevation acute coronary syndromes: insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?). Circulation. 2005;111:1225–1232. [DOI] [PubMed] [Google Scholar]
- 12. Singh JA, Lu X, Ibrahim S, Cram P. Trends in and disparities for acute myocardial infarction: an analysis of Medicare claims data from 1992 to 2010. BMC Med. 2014;12:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. National Heart Lung and Blood Institute. Available at: https://biolincc.nhlbi.nih.gov/home/. Accessed August 28, 2018.
- 14. Atherosclerosis Risk in Communities Study. Available at: https://www2.cscc.unc.edu/aric/. Accessed August 28, 2018.
- 15. White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years' experience. J Clin Epidemiol. 1996;49:223–233. [DOI] [PubMed] [Google Scholar]
- 16. Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty‐two‐year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125:1848–1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Myerson M, Coady S, Taylor H, Rosamond WD, Goff DC Jr; ARIC Investigators . Declining severity of myocardial infarction from 1987 to 2002: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2009;119: 503–514. [DOI] [PubMed] [Google Scholar]
- 18. Atherosclerosis Risk in Communities Study. Available at: https://www2.cscc.unc.edu/aric/sites/default/files/public/manuals/Updates%20Manual3_20151112.pdf/. Accessed August 28, 2018.
- 19. Mansournia MA, Altman DG. Inverse probability weighting. BMJ. 2016;352:i189. [DOI] [PubMed] [Google Scholar]
- 20. Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. [DOI] [PubMed] [Google Scholar]
- 21. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ; ACC/AHA Task Force Members . 2014 AHA/ACC guideline for the management of patients with non‐ST‐elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e344–e426. [DOI] [PubMed] [Google Scholar]
- 22. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. [DOI] [PubMed] [Google Scholar]
- 23. Bhatt DL, Roe MT, Peterson ED, Li Y, Chen AY, Harrington RA, Greenbaum AB, Berger PB, Cannon CP, Cohen DJ, Gibson CM, Saucedo JF, Kleiman NS, Hochman JS, Boden WE, Brindis RG, Peacock WF, Smith SC Jr, Pollack CV Jr, Gibler WB, Ohman EM; CRUSADE Investigators . Utilization of early invasive management strategies for high‐risk patients with non‐ST‐segment elevation acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. JAMA. 2004;292:2096–2104. [DOI] [PubMed] [Google Scholar]
- 24. Safford MM, Brown TM, Muntner PM, Durant RW, Glasser S, Halanych JH, Shikany JM, Prineas RJ, Samdarshi T, Bittner VA, Lewis CE, Gamboa C, Cushman M, Howard V, Howard G; REGARDS Investigators. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308:1768–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nadruz W Jr, Claggett B, Henglin M, Shah AM, Skali H, Rosamond WD, Folsom AR, Solomon SD, Cheng S. Widening racial differences in risks for coronary heart disease. Circulation. 2018;137:1195–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zia MI, Goodman SG, Peterson ED, Mulgund J, Chen AY, Langer A, Tan M, Ohman EM, Gibler WB, Pollack CV Jr, Roe MT. Paradoxical use of invasive cardiac procedures for patients with non‐ST segment elevation myocardial infarction: an international perspective from the CRUSADE Initiative and the Canadian ACS Registries I and II. Can J Cardiol. 2007;23:1073–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Steg PG, Dabbous OH, Feldman LJ, Cohen‐Solal A, Aumont MC, Lopez‐Sendon J, Budaj A, Goldberg RJ, Klein W, Anderson FA Jr; Global Registry of Acute Coronary Events Investigators . Determinants and prognostic impact of heart failure complicating acute coronary syndromes: observations from the Global Registry of Acute Coronary Events (GRACE). Circulation. 2004;109:494–499. [DOI] [PubMed] [Google Scholar]
- 28. Langabeer JR, Henry TD, Kereiakes DJ, Dellifraine J, Emert J, Wang Z, Stuart L, King R, Segrest W, Moyer P, Jollis JG. Growth in percutaneous coronary intervention capacity relative to population and disease prevalence. J Am Heart Assoc. 2013;2:e000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cohen MG, Fonarow GC, Peterson ED, Moscucci M, Dai D, Hernandez AF, Bonow RO, Smith SC Jr. Racial and ethnic differences in the treatment of acute myocardial infarction: findings from the Get With the Guidelines‐Coronary Artery Disease program. Circulation. 2010;121:2294–2301. [DOI] [PubMed] [Google Scholar]
- 30. Sabatine MS, Blake GJ, Drazner MH, Morrow DA, Scirica BM, Murphy SA, McCabe CH, Weintraub WS, Gibson CM, Cannon CP. Influence of race on death and ischemic complications in patients with non‐ST‐elevation acute coronary syndromes despite modern, protocol‐guided treatment. Circulation. 2005;111:1217–1224. [DOI] [PubMed] [Google Scholar]
- 31. Trivedi AN, Nsa W, Hausmann LR, Lee JS, Ma A, Bratzler DW, Mor MK, Baus K, Larbi F, Fine MJ. Quality and equity of care in U.S. hospitals. N Engl J Med. 2014;371:2298–2308. [DOI] [PubMed] [Google Scholar]
- 32. Batchelor W, Kandzari DE, Davis S, Tami L, Wang JC, Othman I, Gigliotti OS, Haghighat A, Singh S, Lopez M, Giugliano G, Horwitz PA, Chandrasekhar J, Underwood P, Thompson CA, Mehran R. Outcomes in women and minorities compared with white men 1 year after everolimus‐eluting stent implantation: insights and results from the PLATINUM diversity and PROMUS element plus post‐approval study pooled analysis. JAMA Cardiol. 2017;2:1303–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Min YI, Anugu P, Butler KR, Hartley TA, Mwasongwe S, Norwood AF, Sims M, Wang W, Winters KP, Correa A. Cardiovascular disease burden and socioeconomic correlates: findings from the Jackson Heart Study. J Am Heart Assoc. 2017;6:e004416 DOI: 10.1161/JAHA.116.004416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, Jacobs DR Jr, Kraus WE, Kris‐Etherton PM, Krummel DA, Popkin BM, Whitsel LP, Zakai NA; American Heart Association Council on Epidemiology and Prevention Council on Nutrition, Physical Activity and Metabolism Council on Clinical Cardiology, Council on Cardiovascular Disease in the Young, Council on the Kidney in Cardiovasc . Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126:1514–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Characteristics of Black and White Patients Hospitalized With Non–ST‐Segment–Elevation Myocardial Infarction; ARIC (Atherosclerosis Risk in Communities) Community Surveillance Study, 2000–2014
Table S2. Medical Management of Black and White Patients Hospitalized With Non–ST‐Segment–Elevation Myocardial Infarction From 2000–2014, Stratified by ARIC Community
Table S3. Various Medications and Procedures Administered to Black and White Patients Undergoing Coronary Revascularization During Hospitalization for Non–ST‐Segment–Elevation Myocardial Infarction (n=6700)
Table S4. Risk‐Adjusted Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction Therapies Among Black vs White (Reference) Patients Known to Have Health Insurance (n=12 314)
Table S5. Risk‐Adjusted Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction Therapies Among Black vs White (Reference) Patients Not Presenting With Acute Heart Failure/Pulmonary Edema (n=11 858)
Table S6. Risk‐Adjusted Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction Therapies Among Black vs White (Reference) Patients Presenting With First‐Occurring Acute Myocardial Infarction (n=12 250)
Table S7. Risk‐Adjusted Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction (NSTEMI) Therapies Among Black vs White (Reference) Patients Classified With Definite NSTEMI (n=9688)
Table S8. Risk‐Adjusted* Relative Probabilities of Various Non–ST‐Segment–Elevation Myocardial Infarction Therapies Among Black vs White (Reference) Patients Discharged With International Classification of Diseases, 9th Revision, Clinical Modification codes 410 to 414 (n=9165)
Table S9. Risk‐Adjusted Relative Probabilities of Invasive Strategy Among Black vs White (Reference) Patients Hospitalized With Non–ST‐Segment–Elevation Myocardial Infarction, Stratified by Geographic Region; ARIC (Atherosclerosis Risk in Communities) Community Surveillance Study, 2000–2014


