Our cellphones rang. Sally, a long-time diabetic who had recently restarted dialysis after decades with a transplant was on the line from the Emergency Department. She seldom called us directly, but now she was panicky and shouting into the phone. “If this is the way it’s going to be, if my mind is going to be messed up, then I might as well quit dialysis. I don’t want to live this way.” She was stuttering and confused, possibly related to the newly diagnosed osteomyelitis or its treatment, but she was oriented enough to know what she was saying. She’d had this conversation many times with her nephrology team. Sally had weathered innumerable complications of type 1 diabetes over more than 50 years and had watched many of her counterparts deteriorate and die. Sally was never one to say, “I quit,” but she always articulated the importance of quality of life over quantity. As she often told us, “There are worse things than death.”
Sally’s all too common situation personalizes the experience reported by Butler et al.1 in this issue of the Journal of the American Society of Nephrology. This is not the first report on the comorbidity of peripheral vascular disease in ESRD, but it captures the effect alarmingly. Peripheral vascular disease, like other chronic conditions (such as heart failure, chronic obstructive pulmonary disease, and malignancy), presages poor prognosis and death, particularly in patients with ESRD. Decades of outcome data confirm a 15%–20% average annual mortality in the general ESRD population,2 and it is even higher among patients with frailty, dementia, and institutionalization.3,4
Watching patients deteriorate and die is an unavoidable part of our work, and up to 20% of ESRD deaths are the direct result of voluntary withdrawal from dialysis.2,5 However, not all nephrologists feel comfortable discussing end-of-life options. By not openly discussing prognosis when complications mount and quality of life declines, we consign patients to more time in the emergency room, hospital, and intensive care unit. Too often, the result is unnecessary pain and suffering, with death in the hospital rather than a place of the patient’s choosing.
Our own experience as a renal team suggests that discussing goals and prognosis early in the course of illness fosters ongoing relationships and trust, empowers more informed decisions, and promotes closure at the end of life for patients, families, and their renal team as well.6 Surveys, however, suggest that these discussions often do not occur, and physicians cite uncertainty and lack of sufficient prognostic information as obstacles.7,8 We would argue that information is abundant,2 bolstered by Butler et al.1 in this issue, and that physicians, despite their protestations to the contrary, actually sense prognosis intuitively as shown by Moss et al.9 using the surprise question (“Would I be surprised if this patient died in the next year”).
All of this is not to discount the difficulty of talking about end of life with patients. Medicine is haunted by the notion that “a death is a failure” or that “we can’t give up.”10 Nephrologists often fear that patients will misunderstand or perceive a lack of compassion if the topic of death and dying is brought up, and on a more personal note, nephrologists who have developed relationships with patients may dread losing “old friends.” That being said, as chronic illness progresses, aggressive treatments prove less and less effective, and a different approach is called for. This is a particularly helpful time for nephrologists to request input from others on the renal team (e.g., social worker, nurse, dietician, and technician); they may have talked with patients and families and gotten signals that it is time to discuss quality of life and have an “enough is enough” conference together. Nephrologists (physicians) too often think that they have to handle this alone, but collaboration with the renal team during this difficult phase of the journey can foster decision making and closure for all involved. Additionally, as Sally recently has said, this conference may be a “dress rehearsal for future ones, closer to that final discussion.”
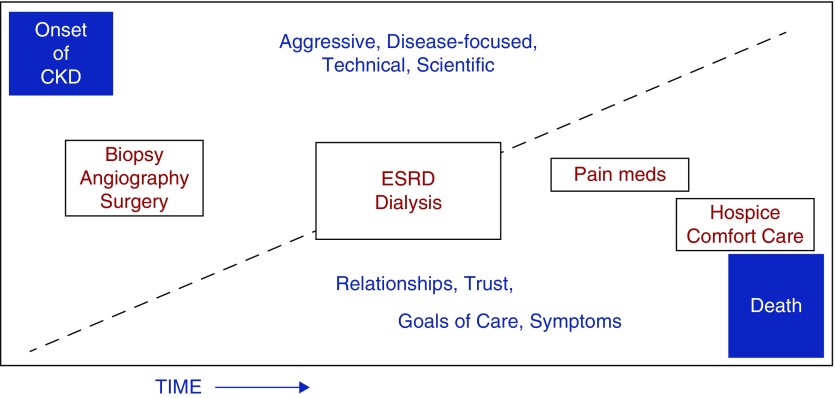
The study by Butler et al.1 provides an important opportunity to consider the trajectory of CKD depicted in Figure 1. At some point as CKD progresses despite our efforts, dialysis becomes necessary and may be the destination therapy for patients who are not transplantable. Our broader view is that critical decisions to initiate or continue dialysis, whether acute or chronic, can be viewed in a palliative manner. The ESRD population is increasingly older, infirm, and disabled. Kurella Tamura et al.11 have shown that initiating chronic dialysis in patients with CKD and progressive limitation in activities of daily living did not improve quality of life and resulted in very high short-term mortality. Furthermore, optimizing general care without dialysis in elderly patients with CKD compares favorably with dialysis in terms of longevity and wellbeing.12,13 Much the same could be said for acute dialysis treatment in the intensive care unit, where general mortality is high and where the initiation or continuation of dialysis ought to be reconsidered when complications mount and the ultimate quality of survival is at stake. Starting (or continuing) dialysis is not obligatory if it does not contribute to perceived quality of life. The effectiveness of palliative care was studied in patients with metastatic (stage IV) nonsmall cell lung cancer, where standard therapy was compared with standard therapy plus palliative care. The outcome was better quality of life without shortening survival.14
Figure 1.
As CKD progresses over time through ESRD toward end of life, the medical choices shift progressively from aggressive interventions toward more palliative treatments.
Although successfully treated for the osteomyelitis and back at home, Sally agrees.
As a patient with type 1 diabetes for 52 years and ESRD for 33 years, I have had my share of challenges. Recently I started hemodialysis after the decline of a 32-year kidney transplant. I have lost much of my energy, and I’m fatigued most of the time. A toe amputation reminds me how the complications of diabetes can plague me. I also learned that my eligibility for a second transplant is doubtful because of cardiovascular disease. I have discussed “enough is enough” with my health care team since I do not want to live without a decent quality of life. My current condition, though not great, is tolerable, but I do not want to live if I’m just “existing.” I welcome any approach that will help me carry on with the challenges of daily living and help my family and me decide which treatments are really going to support quality of life when enough is enough.
Disclosures
None.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related article, “Lower Extremity Amputation and Health Care Utilization in the Last Year of Life among Medicare Beneficiaries with ESRD,” on pages 481–491.
References
- 1.Butler C, Schwarze M, Katz R: Lower extremity amputation and health care utilization in the last year of life among Medicare beneficiaries with ESRD. J Am Soc Nephrol 30: 481–491, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Renal Data Service: United States Renal Data Service Annual Report 2017 (and Previous Years). Available at: http:www.usrds.org/2017. Accessed December 14, 2018
- 3.McAdams-DeMarco MA, Law A, Salter ML, Boyarsky B, Gimenez L, Jaar BG, et al. : Frailty as a novel predictor of mortality and hospitalization in individuals of all ages undergoing hemodialysis. J Am Geriatr Soc 61: 896–901, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swidler M: Considerations in starting a patient with advanced frailty on dialysis: Complex biology meets challenging ethics. Clin J Am Soc Nephrol 8: 1421–1428, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neu S, Kjellstrand CM: Stopping long-term dialysis. An empirical study of withdrawal of life-supporting treatment. N Engl J Med 314: 14–20, 1986 [DOI] [PubMed] [Google Scholar]
- 6.Swartz RD, Perry E: Advance directives are associated with “good deaths” in chronic dialysis patients. J Am Soc Nephrol 3: 1623–1630, 1993 [DOI] [PubMed] [Google Scholar]
- 7.Davison SN: End-of-life care preferences and needs: Perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol 5: 195–204, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mandel EI, Bernacki RE, Block SD: Serious illness conversations in ESRD. Clin J Am Soc Nephrol 12: 854–863, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moss AH, Ganjoo J, Sharma S, Gansor J, Senft S, Weaner B, et al. : Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol 3: 1379–1384, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brown T: When it’s the doctor who can’t let go. New York Times, September 7, 2014. SR4, National Edition.
- 11.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE: Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 361: 1539–1547, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown MA, Collett GK, Josland EA, Foote C, Li Q, Brennan FP: CKD in elderly patients managed without dialysis: Survival, symptoms, and quality of life. Clin J Am Soc Nephrol 10: 260–268, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hussain JA, Mooney A, Russon L: Comparison of survival analysis and palliative care involvement in patients aged over 70 years choosing conservative management or renal replacement therapy in advanced chronic kidney disease. Palliat Med 27: 829–839, 2013 [DOI] [PubMed] [Google Scholar]
- 14.Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. : Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363: 733–742, 2010 [DOI] [PubMed] [Google Scholar]