Abstract
In China, where there are few mental health resources, the majority of HIV-related efforts have focused on medical treatment and transmission prevention rather than psychosocial support. Yet people living with HIV/AIDS (PLWHA) report high levels of psychological distress, especially upon first receiving their HIV diagnosis. We conducted mixed methods research of a qualitative study with (N = 31) individual interviews and 3 focus groups (n = 6 in each group) of HIV-affected participants, and a quantitative survey (N = 200) with individuals living with HIV in Shanghai and Beijing, China. Our qualitative data revealed themes of forms of distress experienced and types of psychosocial support that our participants wished they could have accessed upon diagnosis as well as suggestions for intervention structure that would be most feasible and acceptable. Our quantitative surveys provided further evidence of the high degree of psychosocial distress among recently diagnosed PLWHA. Our findings informed the development of the Psychology Toolbox intervention, a brief CBT skills-based intervention comprising cognitive restructuring, behavioral activation, and paced breathing, designed to be integrated into primary care for recently diagnosed PLWHA. This study describes the intervention development process and contents of each session. Future research should evaluate the intervention for efficacy as well as examine best strategies for eventual implementation and dissemination.
Keywords: HIV, China, recently diagnosed, intervention
At the end of 2014, there were 296,000 individuals living with HIV and 205,000 with AIDS in China (UNAIDS, 2015). People living with HIV/AIDS (PLWHA) in China experience significant mental health distress (Niu, Luo, Liu, Silenzio, & Xiao, 2016). While transmission prevention efforts have been the focus of governmental energy, there has been limited attention paid to the mental health of PLWHA (Shao, 2006). There is a relative lack of research conducted on the psychological experiences of Chinese PLWHA.
The available work, however, has consistently demonstrated a high rate of psychological distress among Chinese PLWHA, with considerable variation among groups based on transmission routes. A convenience sample of HIV treatment-seeking adults in Beijing found a 54.2% endorsement of “significant depressive symptomatology” as indicated by a score of 10 or above on the brief 10-item Center for Epidemiological Studies Depression Scale (CES-D), as well as a 42.9% positive screen for panic attacks, and a 30.8% positive screen for generalized anxiety disorder (Yang et al., 2015). Among HIV-positive former plasma/ blood donors, Meade et al. (2010) reported 47% moderate and 36% severe depression, while Wang et al. (2005) found that 92% of their rural sample were depressed (both studies used the Chinese version of the Beck Depression Inventory (BDI; Beck, Steer, & Garbin, 1988; Zheng, Wei, Goa, Zhang, & Wong, 1988)). Meade et al. (2010) also reported that 52% met criteria for mild-moderate and 8% marked-severe anxiety (using the Chinese version of the Zung Self-rating Anxiety Scale; Zhang et al., 2015; Zung, 1971). In urban areas of Henan and Guangdong provinces, Su et al. (2013) reported that 72% of their general PLWHA sample had depression. Jin et al. (2013) reported on psychological distress in HIV-positive intravenous drug users (IDU) seeking methadone treatment in Yunnan province, finding that 43.1% endorsed suicidality, compared to 8.5% in controls (HIV-negative, non-IDU) using the BDI. Another study of general HIV-positive participants reported that nearly 80% met criteria for lifetime major depressive disorder, compared to 4% of their HIV-negative counterparts, and 20% expressed current suicidal ideation (assessed with the Chinese Composite International Diagnostic Interview and the BDI; Jin et al., 2006).
In addition to diagnosable mental health conditions, PLWHA experience specific HIV-related distress such as disclosure distress (Yang et al., 2016; Simoni et al., 2015), concerns related to medication adherence (Simoni, Yang, & Porricolo, 2012), and medication side effects (Chen, Shiu, Yang, Simoni, et al., 2013; Chen, Shiu, Yang, Lee, et al., 2013).
People who have recently received an HIV diagnosis are particularly vulnerable to psychological distress (Martinez, Israelski, Walker, & Koopman, 2002). While there is a relative absence of research on the mental health of recently diagnosed HIV patients in China, the existing global literature has emphasized the critical nature of psychological adjustment to an HIV diagnosis. In fact, the event of receiving an HIV diagnosis itself is so distressing that it qualifies as an index trauma for a posttraumatic stress disorder (PTSD) diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000). Kelly et al. (1998) found that 30% of homosexual/bisexual men in an Australian sample met criteria for PTSD in response to receiving an HIV diagnosis. While there is contention in the PTSD literature about the validity and utility of classifying receiving an HIV diagnosis as a “trauma” (Bakelaar, Rosenstein, Kagee, & Seedat, 2011; Mundy & Baum, 2004), it is undoubtedly a stressful experience. Upon receiving a diagnosis, many individuals exhibit PTSD symptoms such as recurrent and intrusive thoughts and nightmares about death and illness, as well as situational avoidance of HIV-related stimuli including other people, hospital sites, and life activities (Acierno, Resnick, & Kilpatrick, 1997; Breslau, Davis, Andreski, & Peterson, 1991). Olley et al. (2005) assessed a sample of recently diagnosed PLWHA (mean duration since diagnosis was less than 6 months) in South Africa using expert-administered MINI International Neuropsychiatric Interviews and found that up to 29% of participants met criteria for major depression, 54% for suicidality, and 40% for social anxiety disorder.
In addition to the inherent dysfunction associated with having diagnosable mental disorders, psychological distress in PLWHA has negative repercussions for HIV disease and risk management as well (Delahanty, Bogart, & Figler, 2004). Recently diagnosed individuals include a higher proportion of those with a recent infection, which is characterized by high viral load and increased HIV-transmission potential (Koopman et al., 1997; Quinn et al., 2000). Depression and PTSD diagnoses have been linked to reduced antiretroviral treatment adherence, which can result in reduced viral suppression, again leading to greater chances of HIV transmission (Sherr et al., 2011; Wagner et al., 2011). Researchers have highlighted the need for mental health treatment to reduce HIV transmission risk behavior, including both sexual risk behavior and HIV care and treatment adherence (Grossman & Gordon, 2010; Sikkema et al., 2010). The first year after receiving an HIV diagnosis can be a critical period for intervention, especially to target risk reduction, linkage to care, and mental health (Bhatia, Hartman, Kallen, Graham, & Giordano, 2011; Rao et al., 2012; Weinhardt, 2005). Intervening early in the HIV disease experience may be useful to mitigate the high rates of depression and anxiety described above as well as prevent future suffering and lifetime psychiatric diagnoses.
The majority of intervention research for recently diagnosed PLWHA has not focused on psychological well-being, but rather transmission risk reduction, such as the “Positive Choices” intervention (Sikkema et al., 2011; Sikkema et al., 2014), and linkage to medical care, such as the “Antiretroviral Treatment Access Study Case Management Intervention” (Gardner et al., 2005) and “Outreach Initiative” (Naar-King et al., 2007). We could not locate any intervention research in China for newly diagnosed PLWHA.
Given that the number of individuals diagnosed with HIV in China each year continues to increase (China Center for Disease Control and Prevention, 2013, 2015), research is needed to address their mental health needs. In this paper, we conducted a two-stage mixed methods project to better understand the concerns and psychological distress experienced by Chinese individuals soon after receiving a diagnosis of HIV in order to develop a behavioral intervention to address these needs.
Method
A qualitative Study 1 and quantitative Study 2 are described separately below. The studies were conducted at Shanghai Public Health Clinical Center (SPHCC) and Beijing Ditan Hospital, premier HIV treatment centers in two major metropolitan areas of China. All study procedures were approved by ethics review boards at SPHCC, Ditan Hospital, and the University of Washington.
Study 1: Qualitative Study
For the qualitative component, in 2010–2011 we conducted in-depth interviews with recently diagnosed HIV-positive patients to understand their HIV-related mental health needs and acceptance of psychosocial interventions. We also conducted three focus groups with six participants each, one with recently diagnosed PLWHA, one with their family caregivers (including parents and spouses), and one with their HIV health care providers (including doctors and nurses). A community advisory board (CAB) of stakeholders including patients who had successfully coped with living with HIV for a long period of time, volunteers at Red Ribbon Society (an HIV/AIDS nongovernmental association), seasoned HIV care providers, and supportive family caregivers were also consulted, prior to collecting our in-depth interviews as well as after synthesizing our qualitative findings.
The qualitative study was advertised with posters in the waiting rooms and through staff. Potential participants were invited to speak with clinic staff that connected them to a research coordinator who explained the study details and obtained informed consent. Inclusion criteria were receiving an HIV diagnosis in the last year and ongoing HIV-related care at SPHCC or Beijing Ditan Hospital, 18 years or older, and Mandarin speaking. Participants who were cognitively impaired as informally assessed by medical providers were excluded. Participants received 100 RMB (~USD 15) for their participation in the study.
Researchers experienced in qualitative methods (including the first author) conducted the semistructured individual interviews and focus groups in Mandarin with participants at Beijing Ditan Hospital and SPHCC. Individual interviews were based on an interview guide (see Appendix A) with open-ended prompts designed to collect exploratory information about participants’ psychological experiences of being HIV-positive, beginning with their diagnosis story and how HIV has affected their daily life, well-being, and family functioning. Focus group questions followed the same interview guide but were framed as relating to the PLWHA in their family or under their care. Participants were also queried specifically about the psychological impact of the diagnosis, how they had coped, as well as what resources and support they wished they had access to, or would have been helpful.
Each interview lasted 1 to 2 hours, was audio recorded and transcribed. A total of N = 31 participants were recruited for the individual interviews (n = 12 from Beijing Ditan Hospital and n = 19 from SPHCC) in addition to 3 focus groups, yielding 34 transcripts for analysis.
Participants
Individual interview participants ranged in age from 23 to 66 years (M = 41.6, SD = 10.4); 15 were male and 16 were female. Almost half of the male participants (46.7%) acquired HIV from having sex with other men, and just over one third of female participants (36.8%) acquired HIV through heterosexual sex, the two most common transmission routes. Other common transmission routes reported were blood plasma selling, medical procedures, and needle use. In terms of socioeconomic status, participants ranged in educational history with some completing middle school and others obtaining graduate degrees; some were fully employed while others were unemployed.
Data Analysis
All audio recordings of interviews and focus groups were transcribed verbatim in Chinese by experienced transcribers. At least one member of the research team also reviewed each transcript for accuracy to the recording. Three teams of Mandarin-speaking Chinese research assistants independently coded each transcript in ATLAS.ti qualitative software using an iterative codebook developed from a constant comparison analysis framework (Miles & Huberman, 1994). Preliminary codes were identified by extracting key phrases from answers (Denzin & Lincoln, 1994) that appeared relevant to mental health or were repeated by other transcripts, suggesting possible patterns. We chose mental health as our central topic based on existing empirical literature reviewed in the introduction, highlighting Chinese PLWHA’s needs for mental health support. The interviews were systematically reviewed and coded; the first author (research supervisor) facilitated reconciliation of discrepancies in codes through group discussion and consensus (Hill et al., 2005). Illustrative quotes were extracted and then translated into English for publication.
Study 2: Quantitative Study
For the quantitative phase of the project, we conducted a survey in 2012 at Beijing Ditan Hospital to assess a larger sample of recently diagnosed PLWHA for descriptive information on HIV-related mental health. Participants (N = 200) completed an hour-long paper-and-pencil survey of demographics and psychometrically validated measures of mental health symptomology. We followed the same procedures for advertising, recruitment, inclusion criteria, and participant compensation as Study 1 described above. Per recommendations by our ethics review board described in the informed consent, safeguards were in place in the event of imminent suicidality. As no participants in our study demonstrated imminent suicide risk, no referrals were made.
Measures
Beck Depression Inventory-II (BDI-II)
The BDI-II is a well-established measure (Beck, Steer, & Brown, 1996) for detecting depressive symptoms and has been psychometrically validated in several Chinese populations (e.g., Shek, 1990), including those living with chronic illness (Harris & D’Eon, 2008). This 21-item scale rates, over the past 2 weeks, depressive symptoms such as sadness, pessimism, and irritability on a 4-point Likert-type scale. Compared to other assessments of depression, the BDI includes more items on somatic symptoms (Smarr & Keefer, 2011), which may be better suited for assessing depression in Chinese populations (Kleinman, 1985; Parker, Cheah, & Roy, 2001). Cronbach’s α (Cronbach, 1951) in our sample for the C-BDI-II was 0.921. M = 18.3 (SD = 11.7).
Zung Self-Rating Anxiety Scale (SAS)
The SAS is a 20-item measure assessing anxiety symptoms on a 4-point Likert-type scale ranging from A little of the time to Most of the time (Zung, 1971). Because this measure details many somatic symptoms of anxiety, such as shaking and trembling, increased heart rate, indigestion, and aches and pains, it was chosen for this study due to frequent somatization of psychological problems in Chinese populations (Kleinman, 1982). The measure has cognitive, autonomic, motor and central nervous system symptoms. Reliability and validity of the Chinese version have been established by many studies (e.g., Liu, Oda, Peng, & Asai, 1997; Zhang et al., 2015). Cronbach’s α in our sample for the SAS was 0.815.
Data Analysis Plan
Descriptive statistics will be conducted on survey measures. Inferential statistics of comparing the somatic and affective subscales of the C-BDI-II will be conducted, as previous literature suggests this phenomenon affects Chinese samples.
Results
Study 1: Qualitative Findings
Our analyses of qualitative interview and focus group data revealed themes in two primary categories: (a) types of distress experienced by recently diagnosed PLWHA, and (b) thoughts they had about what resources would be helpful (for themselves at the time and others in a similar situation), including suggestions for intervention timing, location, format, and characteristics of the interventionist.
Theme 1: Types of Distress
Participants reported experiencing significant negative emotion following receiving an HIV positive diagnosis, including suicidal ideation, anxiety, and hopelessness. Participants also engaged in catastrophic thinking and self-isolating behaviors.
Suicidal ideation
Participants described suicidal ideation following receiving a diagnosis both as thoughts for immediate action in their periods of severe distress as well as a plan for the future when their HIV progressed.
I just couldn’t believe I was HIV-positive. It is too hard to describe such a feeling … the most terrible period I have ever experienced … I was thinking about suicide. —Male participant
Anxiety
Participants reported anxiety in the form of fear of transmitting HIV to loved ones, worry about the future, consequences of others finding out about their status, and avoidance of HIV-related information.
I’m scared, really scared. I asked a lot of people, some of them told me that saliva is not contagious; some of them told me that saliva is contagious. I’m confused. I don’t know if it is really contagious or not. —Female participant
My anxiety is family pressure. What will happen to them in the future? – Male participant
In the countryside, if they know you are HIV-positive, your whole family cannot live any more. —Male participant
I forced myself not to know more about it [HIV/AIDS]. I was afraid that that kind of information would make me even more distressed. —Male participant
Hopelessness
Many participants described feelings of hopelessness about their future, even in the face of scientific information from credible sources.
When I heard the news [HIV-positive diagnosis] … I collapsed. It seemed like there is no hope, nothing. —Female participant
Catastrophic thinking
Participants showed evidence of catastrophic thinking, anticipating the worst possible outcomes (Beck, Rush, Shaw, & Emery, 1979).
Our condition is not like how others say we can still live for twenty years. Even for ten years, I feel that is not true. I feel that I could not live that long. —Female participant
Self-isolation
In addition to thoughts and emotions, participants also described behaviors they engaged in, as a result of their negative emotions. These behaviors were often of self-isolation and could contribute to further negative emotion, as they were removing themselves from sources of positive social support (See Xie, Yang, Simoni, Shiu, Chen, Lu, et al., in press for further exploration of self-isolation).
I used to be an outgoing person … but now I feel self-hate. I used to have a lot of friends, but now I never go out and socialize with my friends. —Female participant
Theme 2: Useful Resources
Our qualitative data also showed evidence of types of psychosocial support that our participants wished they could have accessed upon diagnosis. Our interviewees gave suggestions for intervention structure and design for greatest feasibility and acceptability, such as timing, format of the intervention, and acceptable interventionists.
Timing of intervention
In terms of timing of intervention, participants referred to a critical window of time immediately following the diagnosis that was particularly difficult.
I spent a week in fear of my HIV test results … I cried several times a day … I walked around with an aimless feeling all day. —Male participant
That first half year, it was so difficult to adapt. First, I was afraid for my family and the second, I was afraid that my friends would know. I just did not know what to do or how to respond. —Female participant
Type of intervention
Participants described that learning ways to cope with what they were feeling would be helpful. They also described wanting individual time with an interventionist, whether it was delivered face-to-face or over the phone.
At the time I had so much fear I did not know what to do. What was I supposed to do? I think one-on-one treatment would have helped me get through that lonely time. —Female participant
Interventionist characteristics
In addition to a mental health counselor as a professional source of support, participants described being amenable to receiving support from more experienced peers as well as doctors or nurses.
Chatting with peers helps a lot. … Most people in this situation have the same feeling. Peers who have been diagnosed longer, they are experienced and they know more. —Female participant
If the doctor or nurse could provide one-on-one intervention … that would be effective since they could answer the questions I have. —Female participant
Intervention location
Participants described the need for the intervention to be practical and accessible for them, including having the intervention be located at the hospital where they were already receiving medical and primary care.
I have to travel far and take time off work to come here [SPHCC], so if it can be at the same time, that would be good. —Male participant
Study 2: Quantitative Findings
Participants
Of our 200 participants, 81% were male, ranging in age from 19 to 78 years with a mean of 37 (SD = 9.1). Ninety-five of our male participants reported having same-sex sexual partners (either only same sex, or both same and opposite sex). Monthly income was reported on a scale categorizing income in increments of RMB 1,000, with the mean response corresponding to earning between RMB 2,000–2,999 per month, which is comparable to the average national wage of RMB 2,396 per month (International Labour Organization, 2013. Demographic characteristics are presented in Table 1.
Table 1.
Sociodemographic Characteristics of Recently Diagnosed Patients Living With HIV/AIDS in Beijing and Shanghai, China (N = 200)
| Characteristic | n (%*) |
|---|---|
| Sex | |
| Female | 38 (19.0) |
| Male | 162 (81.0) |
| Age in years; M(SD) | 37 (9.1) |
| Marital status | |
| Married or steady partner | 69 (34.5) |
| Single, never married | 84 (42.0) |
| Other (divorced, widowed, separated) | 44 (22.5) |
| Sexual partner | |
| Same sex | 84 (42.6) |
| Opposite sex | 67 (33.5) |
| Both | 11 (5.5) |
| Refuse to answer | 27 (13.5) |
| Missing data | 11 (5.5) |
| Education | |
| Primary or lower | 8 (4.1) |
| Middle school graduation | 27 (13.5) |
| High school graduation | 39 (19.5) |
| Professional/vocational training school | 25 (12.5) |
| Above high school (college & post-college) | 98 (49.0) |
| Employment | |
| Full time | 96 (48.0) |
| Part time | 22 (11.0) |
| Unemployed | 78 (39.0) |
| Monthly household income (RMB) | |
| ≤ 2,000 | 70 (35.7) |
| 2,001 – 5,000 | 87 (43.5) |
| ≥ 5,000 | 29 (14.5) |
Percentages may not add up to 100 due to missing data
Depression
The majority of our participants (68.5%) were above threshold for current depression on the C-BDI-II (scores below 13 are considered “normal”) according to Chinese norms (Chinese Behavioral Sciences Society, 2000), with 24.5% screening positive for moderate depression, and 17.0% falling in the range of severe depression. The C-BDI-II has a somatic and affective subscale; the mean somatic subscale score was 11.3 (SD = 7.7) and the mean affective subscale score was 7.0 (SD = 4.9). A dependent samples t test indicated that the scores are different t (199) = 11.3, p < .001. This phenomenon has been reported in the past, where somatic symptoms are often more endorsed than affective symptoms by Chinese populations (Parker et al., 2001). Suicidality was measured by Item 9 on the C-BDI-II, with 34% of our sample endorsing, “1— I have thoughts of killing myself, but I would not carry them out”; 4% endorsing, “2— I would like to kill myself”; and 5% endorsing, “3— I would kill myself if I had the chance.”
Anxiety
The total score for anxiety on the Zung Self Rating Anxiety Scale was M = 38.7 (SD = 7.9), indicating that the mean responses endorsed by participants was experiencing every anxiety symptom Some of the time (scale ranges from 1= A little of the time, 2 = Some of the time, 3 = A good part of the time, 4 = Most of the time). Items with particularly high endorsement were, “I feel more nervous and anxious than usual”; “I feel weak and get tired easily”; “I am bothered by dizzy spells”; and “I am bothered by stomach aches or indigestion.”
Intervention Development
Our mixed methods study sought to better understand the mental health needs of recently diagnosed individuals, including their levels of distress and resources that they hoped to access. In our qualitative data, our participants reported experiencing significant negative emotion following receiving an HIV positive diagnosis, including suicidal ideation, anxiety, hopelessness, as well as catastrophic thinking and self-isolating behaviors. They also gave suggestions for intervention design, in particular highlighting the critical window after diagnosis when they experienced maximum stress, and their desire for one-on-one psychological support. In our quantitative data, 68.5% of participants were above threshold for depression, 43% endorsed some degree of suicidality, and the mean responses for anxiety were experiencing every symptom assessed at least “some of the time.”
To develop our intervention, we used the first three phases of the Formative Method for Adapting Psychotherapy (FMAP; Hwang, 2006, 2009): (a) generate knowledge in collaboration with stakeholders, (b) integrate information with expert theoretical, empirical, and clinical knowledge, and (c) review initial intervention with stakeholders. Specifically, we synthesized our qualitative and quantitative data analysis with an extensive literature review of evidence-based behavioral strategies as well as consultation with Chinese mental health experts and our Community Advisory Board to develop a brief three-session skills-based distress reduction intervention called the Psychology Toolbox. We created all the materials in English and Chinese simultaneously. It was developed to be integrated into an HIV primary care setting with minimal burden to patients and disruption to clinic routine. Sessions are to be scheduled as close to a weekly basis as possible to coincide with initial HIV primary care visits as this minimizes participant burden, thereby increasing the likelihood that the intervention will be a feasible model of care. Research suggests that timing psychotherapeutic sessions a week apart is useful and highly common as it allows ample time for skills acquisition, practice, and consolidation, while allowing maintenance of momentum and therapeutic alliance (Erekson, 2013).
The intervention was developed with a cognitive behavioral therapy (CBT) skills-based theoretical framework (Linehan, 1993) due to literature on predictors of better outcomes of mental health interventions with both local and overseas Chinese populations (Leong, 2007). These include having the interventionist adopt a more authoritative versus collaborative role to convey expertise in the therapeutic relationship (Lee, 1997), use of educational approaches such as psychoeducation, role-play, and assignment of tasks at home (Uba, 1994), and goal-directed problem-solving behavioral strategies over an insight-oriented approach (Ng & James, 2013), which are in line with a CBT skills-based framework. An intervention of individual CBT skills is also more easily manualized and non-mental-health professionals can be trained to deliver it (Montgomery, Kunik, Wilson, Stanley, & Weiss, 2010; Simoni et al. 2015).
Additionally, we developed our intervention to be implemented within a brief intervention in primary care context (O’Donnell, Wallace, & Kaner, 2014). Brief interventions in a primary care context have been demonstrated to be efficacious for a number of public health concerns ranging from increasing fruit and vegetable intake (Buyuktuncer, Kearney, Ryan, Thurston, & Ellahi, 2014) to decreasing alcohol-related problems (Kaner et al., 2007) as well as with HIV-positive populations (St. Lawrence et al., 1997). Opportunistic brief interventions in primary care typically use a contact model of between 1–5 sessions, with a mean of 25 minutes per session with an upper bound of 50 minutes per session, with overall treatment exposure ranging between 60–175 minutes (about three 50-minute sessions) (O’Donnell et al., 2014).
The participants in our qualitative and quantitative data reported that their main difficulties were fear and anxiety about their HIV, including thinking about worst-case scenarios resulting from their HIV, thereby leading to isolation and depression. To address these difficulties, three skills are taught in the intervention: Session 1—a cognitive restructuring skill in the form of an automatic thought record to address catastrophic thinking about HIV and subsequent elevated distress; Session 2—a behavioral engagement skill to address isolation and depressive feedback cycles; Session 3—a paced breathing skill to address anxiety.
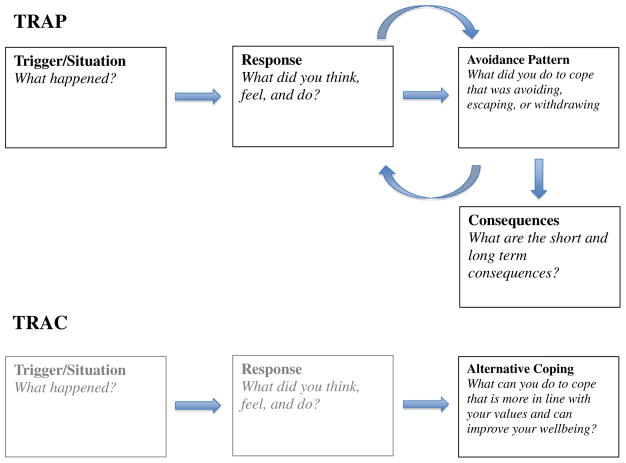
An Automatic Thought Record (J. Beck, 2011) is a component of evidence-based cognitive therapy to restructure unhelpful core beliefs (e.g., Bennett-Levy, 2003; De Oliveira et al., 2012). The behavioral engagement skills Trigger, Response, Avoidance Pattern (TRAPs) and Trigger, Response, Alternative Coping (TRACs; Martell, Dimidjian, Herman-Dunn, 2010) are part of an evidence-based behavioral activation for depression package (e.g., Gortner, Gollan, Dobson, & Jacobson, 1998), with some evidence also suggesting utility as an early intervention for posttraumatic stress disorder (Wagner, Zatzick, Ghesquiere, & Jurkovich, 2007). Paced Breathing (Linehan, 1993) is part of an evidence-based dialectical behavioral therapy skills course (e.g., Panos, Jackson, Hasan, & Panos, 2013). Below we describe each session, with a summary of agenda, goals, and suggested language in Table 2 (contact first author for full manual).
Table 2.
Detailed Intervention Outline
| SESSION 1
|
|
|---|---|
| Agenda item | Goal and Sample Text |
| Overview of intervention goals |
|
| Explore diagnosis story |
|
| Explore existing coping skills |
|
| Explore current functioning, including family functioning, social support, and distress |
|
| Highlight example of catastrophic thinking; psychoeducation of automatic thought cycle |
|
| Psychoeducation of the cognitive-behavioral triangle |
|
| Teach Automatic Thought Record |
- In the second column we write down the emotions you felt at the time (e.g., sad, angry, scared), and on a scale of 0 – 100 with 0 being not intense at all and 100 being very intense. E.g., you felt fear at an 80 and sadness at an 80 - In the third column, we write down the automatic thoughts that went through your mind. E.g., “I am going to die”, “I brought shame to my family”. How much did you believe them? - In the fourth column, we take a step back and think about the FACTS (remember, facts are points about reality that are completely true and not just our interpretation) that support this automatic thought. E.g., “HIV can lead to a disease that sounds scary and I know people who have died from it” - In the fifth column, we will think about facts that do NOT support this automatic though. E.g., “I know people who have lived with HIV for a long time” - In the sixth column, we think of a more realistic/balanced thought, e.g., “Having HIV can be and people are able to live with it” - In the last column, we re-rate your feeling of fear and sadness. Are they both still at 80? |
| Assign homework |
|
| Close session |
|
| SESSION 2
|
|
| Agenda item | Goal and Sample Text |
|
| |
| Review homework |
- Let’s review the worksheet (if you did not do it, that is okay, let’s do it together now). Tell me about the situation that happened that caused you to have strong negative emotions. What happened at that moment? What were the emotions you felt, and how intense on a scale of 0 – 100? What were the automatic catastrophic thoughts you had? How much did you believe in them? What were the facts supporting those beliefs? What were the facts that did NOT support those beliefs? What was the more realistic thought that you arrived at? And after all of this, what were your emotions at the end again, from 0 – 100? - What was it like going through this automatic thought record? What did you find helpful or unhelpful about it? Can you think of a time in the future when you might want to use this, or anybody in your life that you might want to teach this skill/tool to? |
| Teach TRAP/TRAC |
- Xiao Ming is a 30-year-old man who has just received an HIV diagnosis. After receiving the diagnosis, he has many emotions of sadness, shame, and fear. The Trigger – His friends call him to go out to dinner with them, something they do often. The emotional Response – As he sees his friend’s contact image coming up on his phone, he feels shame about his HIV status and worries that if he eats with his friends and they find out later he has HIV, they might be upset at him, so he doesn’t pick up the phone call. The Avoidance Pattern – Because he doesn’t pick up the phone, he doesn’t make plans with his friends to go out to dinner. He ends up staying at home and just staying in bed. This isolation means that he doesn’t get to have the positive experience of going out with his friends to enjoy a good time hanging out. As a result, he feels even worse. The Avoidance Pattern feeds on itself as a feedback cycle that gets more severe over time. Each time his friends call, he doesn’t pick up the phone, so his friends start to call him less and less. - Instead of perpetuating this avoidance pattern, Alternative Coping is a more adaptive way to address the situation. With the same Trigger and emotional Response (where Xiao Ming’s friends call him to have dinner and he feels shame when he sees the incoming call), an Alternative Coping method would be for him to engage in opposite action to the shame, pick up the phone and make plans to meet up with his friends. He goes out and has a good time with his friends, just like they usually do. By doing this action, he has allowed himself to receive evidence that his friends still care about him as they always have, he gets to engage in a positive evening, and therefore he feels better. Additionally, he maintains good relationships with his friends, rather than in the avoidance situation where he distances himself from them. As a result, he breaks the cycle of isolation and avoidance, and feels better overall. - So as you can see, instead of AVOIDING, when he APPROACHES it is very likely that he starts to feel more energized, better, and cared for, and he can see that his friends still like him and want to be around him. This is called an alternative coping method that breaks the vicious cycle of avoidance. |
| Use participant example for TRAP/TRAC worksheet |
- We will use your example to fill in this worksheet. The Trigger refers to the situation that happens; Response is what you typically think, feel and do, and Avoidance Pattern refers to what you do that is withdrawing, avoiding, or escaping. We will fill the boxes in based on your example. What are the short and long term consequences of this avoidance pattern? - What are some possibilities we put instead for Alternative Coping, where you respond in a way that is more in line with your values and will keep you from an avoidance pattern? |
| Create a plan for Alternative Coping and assign homework |
- What would it look like for you to take some steps in terms of alternative coping this week? - Your homework for this week is to take X of those steps we discussed. If you'd like to, you may take home this TRAP/TRAC worksheet as a reminder of the pattern and the coping steps to take. |
| SESSION 3
|
|
| Agenda Item | Goal and Sample Text |
|
|
|
| Review homework |
- Troubleshoot barriers that participant experienced in terms of taking active steps, reinforce any movement toward change that participant engaged in. |
| Teach Paced Breathing |
- In situations like what we just discussed, when you notice an increase in your anxiety, a skill called "paced breathing" could be really helpful. - Paced breathing is simply breathing out longer than breathing in. We do this because the human peripheral autonomic nervous system is divided into two parts, a parasympathetic nervous system and sympathetic nervous system. The parasympathetic nervous system is responsible for rest and digest functions whereas the sympathetic nervous system is responsible for fight or flight. - When we breathe in, the sympathetic fight or flight nervous system is activated; when we breathe out, the parasympathetic rest and digest nervous system is activated. Both of these are necessary for different versions of equilibrium for daily living. For example, if you breathe in more than you breathe out and do it rapidly, it can feel like you’re getting ready to move quickly or even hyperventilating/gasping if you do it long enough. We’ll try it together; can you feel your body getting activated? - When we do paced breathing for anxiety, we are going for the opposite effect. Just like breathing in a lot and rapidly can quickly elevate your heart rate and kick you into gear, breathing out more deeply can lower your arousal. - We are going to try it out together. We want our out-breath to be longer than our in-breath. Pay attention to your breathing right now without trying to change it. What is your natural breath count? A comfortable paced breathing count depends on each person’s own lung capacity and comfort with deep breathing. For example, my natural breath is about 4 counts, so when I do paced breathing, I will breathe in for 4 counts and breathe out for 6 counts. We will try paced breathing together with our individual counts for a few minutes. - What do you notice in your body after that exercise? - In the future when you notice yourself getting anxious, try to pace breathe for a few minutes. This skill is useful because it is easy to do and you can do it anywhere, even when people are around without them even realizing. |
| Review all 3 skills |
|
Session 1
The first session focuses on quickly building rapport with participants through understanding their HIV diagnosis story, in particular the thoughts and emotions immediately upon confirmation of an HIV-positive status. An unstructured assessment of the patient’s mental health, substance use, suicidality, disclosure story, and coping skills will be conducted for adequate tailoring.
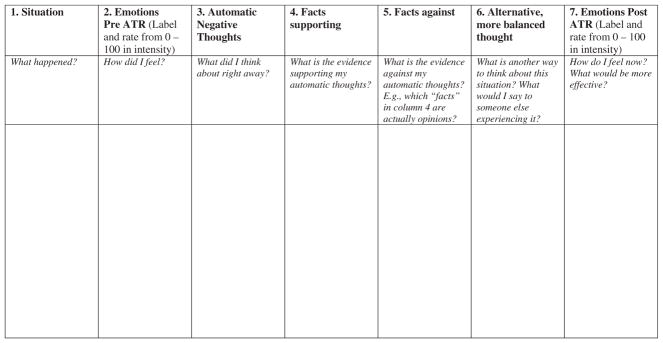
An Automatic Thought Record (J. Beck, 2011; see Figure 1) is taught using the following case example (derived from aggregating stories from our qualitative data), with the interventionist helping the participant fill in the columns to teach the skills. The situation (Column 1) is the following: Da Wei is a 25-year-old man who went to the CDC with his friend Li Hong who is a long-time member of a QQ community (a Chinese instant-messaging platform) for gay men and regularly gets HIV and other STD testing. Since Da Wei was there, he decided to get tested as well. A few days later, the CDC called him and told him to come back in to collect his results. Immediately, Da Wei feels fear and anxiety (Column 2) at about 95/100 in intensity. He starts to experience many automatic thoughts that come up immediately (Column 3), such as “I am HIV-positive”; “I am going to die”; “My parents will have no one to take care of them”; “I have brought shame to my entire family.” The interventionist and Da Wei assign a percentage rating of how much Da Wei believes in each of the automatic thoughts..
Figure 1.
Automatic Thought Record (ATR) Note. Adapted from Beck (2011).
It is important to understand that automatic thoughts are often catastrophic and the worst-case scenarios possible; it is not hard to understand that because of fear, these thoughts can happen very quickly and often we don’t have control over them. However, what happens afterwards, we can do something about. We want to think about the facts of the situation that support the automatic thoughts (Column 4), not our interpretation, meaning these are points about reality that are completely true. For example, “HIV is a disease that sounds scary and I know that people have died from it.” Next, we think about facts that do not support the automatic thought (Column 5), such as, “I know many people who have HIV and live for a long time”; “These people are still close to their families and are able to work and do normal things”; “Just because the CDC is calling me, it does not mean that my entire family knows already”; “I can deal with disclosure later on as I have more time to make a good decision.” After coming up with facts supporting and against the automatic thought, we work to list a more balanced and realistic thought (Column 6), such as “HIV can lead to a scary disease, and if I do have it, I will be able to live with it and face the problems that come up because of it.” In the last column (Column 7), we re-rate what we think Da Wei’s emotion of fear is in the moment, maybe a 60/100. We can see that he has decreased from his initial very intense emotion of 95/100. Also, we will go through and re-rate how much Da Wei believes in each automatic thought as well, and notice the changes.
For homework, participants are asked to complete at least one Automatic Thought Record during the week when they suddenly notice feeling particularly distressed. Participants are encouraged to fill the record out as soon as possible in order for it to be the most useful. If they do not have access to the record immediately, filling it out later is acceptable as well.
Session 2
The second session begins with reviewing the Automatic Thought Record homework assignment from the previous week. If homework has not been completed, troubleshoot barriers to completion such as forgetting, lack of buy-in to the skill, or lack of opportunity to practice the skill. The skill is then practiced in session in order to consolidate learning; the interventionist will assist participant in filling out a record for something that occurred in the week when the participant was particularly distressed.
The focus of the second session is to increase behavioral engagement by exploring avoidance patterns that have arisen in the participant’s life as a result of HIV, in particular, ones that may contribute to negative affect or lower mood. Participants are given a behavioral activation TRAP (Trigger, Response, Avoidance Pattern) and TRAC (Trigger, Response, Alternative Coping) visual cycle (Martell et al., 2010; see Figure 2) delineating a real-life example from our qualitative data. Again, the interventionist assists the participant in filling out the cycle worksheet.
Figure 2.
TRAP/TRAC Worksheet Note. Adapted from Martell, Dimidjian, & Herman-Dunn (2010)
The following case example is used to illustrate TRAP/ TRAC: Xiao Ming is a 30-year-old man who has just received an HIV diagnosis. After receiving the diagnosis, he has many emotions of sadness, shame, and fear. The Trigger— His friends call him to go out to dinner with them, something they do often. The emotional Response—As he sees his friend’s contact image coming up on his phone, he feels shame about his HIV status and worries that if he eats with his friends and they find out later he has HIV, they might be upset at him, so he doesn’t pick up the phone call. The Avoidance Pattern— Because he doesn’t pick up the phone, he doesn’t make plans with his friends to go out to dinner. He ends up staying at home and just staying in bed. This isolation means that he doesn’t get to have the positive experience of going out with his friends to enjoy a good time hanging out. As a result, he feels even worse. The Avoidance Pattern feeds on itself as a feedback cycle that gets more severe over time. Each time his friends call, he doesn’t pick up the phone, which means that his friends start to call him less and less. Instead of perpetuating this avoidance pattern, Alternative Coping is a more adaptive way to address the situation. With the same Trigger and emotional Response (where Xiao Ming’s friends call him to have dinner and he feels shame when he sees the incoming call), an Alternative Coping method would be for him to engage in opposite action to the shame, pick up the phone and make plans to meet up with his friends. He goes out and has a good time with his friends, just like they usually do. By doing this action, he has allowed himself to receive evidence that his friends still care about him as they always have, he gets to engage in a positive evening, and therefore he feels better. Additionally, he maintains good relationships with his friends, rather than in the avoidance situation where he distances himself from them. As a result, he breaks the cycle of isolation and avoidance, and feels better over all.
The interventionist then works with the participant to fill out a TRAP/TRAC that is relevant to his or her own life. Collaboratively, they brainstorm an alternative coping strategy. For homework, participants are asked to complete at least one iteration of the alternative coping strategy.
Session 3
The third session again begins with homework review of the participant trying out an alternative coping behavior when noticing experiencing the TRAPs discussed in the previous session. Similarly, if homework has not been completed, troubleshoot barriers to alternative coping and create a new plan to engage in the behavior.
The focus on the third session is on experiences of anxiety as a result of having an HIV diagnosis. Assess whether the participant has ever had an anxiety attack, such as symptoms of increased heart rate, sweating, shaking, or difficulty breathing. Also assess for situations when participant often notices feeling anxious or worrying as opportunities to practice paced breathing. Provide psychoeducation about paced breathing: the human peripheral autonomic nervous system is divided into two parts, a parasympathetic nervous system and sympathetic nervous system. The parasympathetic nervous system is responsible for rest and digestive functions whereas the sympathetic nervous system is responsible for fight or flight. In other words, the parasympathetic nervous system is the one we want to activate to get relaxation and calming to occur when we feel anxious. In order to do that, we engage in a simple breathing exercise. Breathing out activates the parasympathetic nervous system, whereas breathing in activates the sympathetic nervous system (both of these are necessary for different versions of equilibrium for daily living). The participant is asked to experience this for him- or herself by trying to breathe in rapidly a few times, similar to gasping. This may feel like getting anxious and ready to run. The objective is the opposite effect to calm the body down. Therefore, paced breathing is done, where the out-breath is longer than the in-breath. While it depends on each individual’s own lung capacity and comfort with deep breathing, breathing in for 4 counts and breathing out for 6 counts can be a good place to start. After paced breathing is taught, all three skills are reviewed with the participant to consolidate learning.
Discussion
Individuals who have recently received an HIV diagnosis experience significant stress with adjusting to their new status. In China, PLWHA have a particularly difficult time as they are faced with significant HIV stigma (Rao et al., 2012; Zhang et al., 2016), while having little access to psychosocial support (Yang et al., 2015). Indeed, we were unable to locate existing research on behavioral interventions for recently diagnosed PLWHA. We conducted what we believe is the first study focusing on intervening for mental health of individuals recently diagnosed with HIV in China. Our qualitative and quantitative data converged to demonstrate the primary areas of stressors for recently diagnosed PLWHA, as well as the structural factors surrounding the resources they need and are able to access. Participants experienced significant depression, suicidality, and anxiety as a result of receiving an HIV diagnosis. Our findings informed the development of an evidence-based brief intervention focused on cognitive behavioral skills to reduce HIV-related distress, which we described in some detail.
This study has several limitations. We recruited convenience samples from premier HIV treatment centers in the major metropolitan areas of Shanghai and Beijing. Given that these settings have better resources for PLWHA (indeed, many individuals travel specifically to these locations to receive HIV-related care), our findings may not be generalizable to other areas in China. Specifically, participants in our sample may have atypical demographics including higher education (although a range was seen in our quantitative data where 17.6% had completed middle school or less), which may contribute to a more nuanced understanding of mental health as well as higher acceptance of psychosocial resources. Furthermore, our development of an intervention for reducing psychological distress for recently diagnosed PLWHA for integration into HIV primary care also presupposes the availability of a primary care structure amenable to this integration. This infrastructure may not exist in other less developed areas of China.
Despite these limitations, our intervention provides the first attempt that we know of to address psychosocial stress of individuals recently diagnosed with HIV in China, using evidence-based behavioral strategies. As our intervention was designed with Beijing Ditan Hospital and SPHCC stakeholder input and oversight from its initiation, it is well-suited for preliminary testing at these sites. Ongoing work is addressing the feasibility and acceptability of the intervention to understand the facilitators and barriers of implementation (Yang et al., under review). Intervention testing with samples of recently diagnosed PLWHA in order to examine intervention efficacy will also be critical. In addition, as the availability of trained mental health professionals in China is scarce (WHO, 2005), our brief, manualized intervention of concrete skills may be amenable to a variety of strategies of adaptation for this resource-constrained setting.
For example, with the recommendation of task-shifting of health care duties to less specialized health workers, given task-specific training when appropriate, in order to reduce global health inequities (WHO, 2008), other staff or lay counselors may be trained to deliver the manualized Psychology Toolbox intervention. A previous study in a similar setting successfully trained HIV nurses to deliver a manualized intervention to support HIV-positive individuals through the disclosure decision-making process (Simoni et al., 2015). A similar training and supervision structure may be examined for our intervention, in order to allow for implementation at HIV treatment centers across China that may not have designated mental health professionals on staff.
Additionally, an ongoing open skills group format that occurs at regular intervals at the hospitals may allow for many individuals who receive their HIV diagnosis at a similar time to acquire skills together as well as practice with each other and build a peer community. Different versions of the skills in the Psychology Toolbox have been delivered successfully in a group format in other resource-constrained settings with other populations (e.g., Linehan, 1993; Porter, Spates, & Smitham, 2004), suggesting the utility of group skills training here.
Future research is necessary to test the intervention on samples of recently diagnosed PLWHA in order to examine intervention efficacy and implementation likelihood, as well as to examine the permutations described above. If shown to be acceptable, future work is needed to demonstrate efficacy, and ultimately, effectiveness in real-world settings across China, in order to improve the well-being of individuals recently diagnosed with HIV.
Acknowledgments
We would like to thank our participants, as well as Mi Hu, Yi-An Lo Burleson, Tianyi Xie, and Xiangyu Tao for their support and help with this project. Research reported in this publication was supported by National Institute of Mental Health under award numbers F31MH099925 and K24MH093243. Additional support was provided by the University of Washington Center for AIDS Research (CFAR) under award number AI027757 and the University of Washington Department of Psychology.
Appendix A
Semistructured Qualitative Interview Guide
1. Experience of the diagnosis
In this part, I will ask you about your experience when you first heard you were HIV+.
→ Please describe the experience of how you found out you were HIV+.
Additional prompts if necessary. Please make sure participant addresses the following:
When/how did you first learn you were HIV+?
Who told you?
What was your reaction to the news?
Who knows about your HIV status? How did they learn about it?
2. Impact of the diagnosis
In this part, I will ask you about the impact HIV has had on your life.
→ How has becoming HIV+ impacted you emotionally and psychologically?
Additional prompts if necessary. Please make sure participant addresses the following:
-
Experience with mental health problems, e.g.
Stigma
Adjustment: difficulty adjusting to HIV+ status?
Anxiety: being so worried or anxious that you’ve had difficulty doing things?
Depression: feeling sad and down? Suicidal thoughts?
Substance abuse: using alcohol and other drugs?
PTSD: avoidance?
3. Process of coping
In this part, I will ask you about what you have done to cope with your diagnosis.
→ What have you done to feel better since and/or respond to your HIV diagnosis?
Additional prompts if necessary. Please make sure participant addresses the following:
-
What kinds of resources have been accessed, e.g.,
Family support
Social network support
Mental health services including counseling
Traditional Chinese medicine, Western medicine
4. Helpful resources
In this part, I will ask you about what you might want to tell someone else in your situation in order for them to learn from your experience.
→ What resources do you think would be helpful to someone else in your situation?
Additional prompts if necessary. Please make sure participant addresses the following:
Would it be helpful to talk about some of the issues you faced with someone in the clinic, such as a doctor, nurse, another patient, other patients’ families?
Would you bring a family member or other caregiver with you to access this resource?
Would it be feasible for you come into the clinic regularly in order to talk about the problems you have been dealing with?
What are some areas that you need the most assistance with?
Contributor Information
Joyce P. Yang, University of Washington, Seattle
Jane M. Simoni, University of Washington, Seattle
Sapna Cheryan, University of Washington, Seattle.
Cheng-shi Shiu, University of Washington, Seattle.
Weiti Chen, Yale University, School of Nursing.
Hongxin Zhao, Beijing Ditan Hospital.
Hongzhou Lu, Shanghai Public Health Clinical Center, Fudan University.
References
- Acierno R, Resnick HS, Kilpatrick DG. Health impact of interpersonal violence. 1: Prevalence rates, case identification, and risk factors for sexual assault, physical assault, and domestic violence in men and women. Behavioral Medicine. 1997;23(2):53–64. doi: 10.1080/08964289709596729. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision. [Google Scholar]
- Bakelaar SY, Rosenstein D, Kagee A, Seedat S. HIV as an index stressor for PTSD: challenges and pitfalls in applying DSM criteria. African Journal of Psychiatry. 2011;14(4):259–261. doi: 10.4314/ajpsy.v14i4.2. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- Beck J. Cognitive therapy: Basics and beyond. 2. New York: Guilford Press; 2011. [Google Scholar]
- Bennett-Levy J. Mechanisms of change in cognitive therapy: The case of automatic thought records and behavioural experiments. Behavioural and Cognitive Psychotherapy. 2003;31(03):261–277. doi: 10.1017/S1352465803003035. [DOI] [Google Scholar]
- Bhatia R, Hartman C, Kallen MA, Graham J, Giordano TP. Persons Recently Diagnosed with HIV Infection are at High Risk for Depression and Poor Linkage to Care: Results from the Steps Study. AIDS and Behavior. 2011;15(6):1161–1170. doi: 10.1007/s10461-010-9778-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48(3):216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Buyuktuncer Z, Kearney M, Ryan CL, Thurston M, Ellahi B. Fruit and vegetables on prescription: A brief intervention in primary care. Journal of Human Nutrition and Dietetics. 2014;27(Suppl 2):186–193. doi: 10.1111/jhn.12109. [DOI] [PubMed] [Google Scholar]
- Chen W-T, Shiu C-S, Yang JP, Lee S-Y, Lee TS-H, Simoni JM, … Lu H-Z. Fatigue and sleep disturbance related to perceived stress in Chinese HIV-positive individuals: A mixed methods study. Journal of AIDS & Clinical Research. 2013;4(6) doi: 10.4172/2155-6113.1000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Shiu CS, Yang JP, Simoni JM, Fredriksen-Goldsen K, Lee TSH, Zhao H. Antiretroviral Therapy (ART) side effect impacted on quality of life, and depressive symptomatology: A mixed-method study. Journal of AIDS & Clinical Research. 2013;4:218. doi: 10.4172/2155-6113.1000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinese Behavioral Sciences Society. The Chinese version of the Beck Depression Inventory. 2. New York: Harcourt Brace; 2000. [Google Scholar]
- Chinese Center for Disease Control and Prevention. 2012 National report on notifiable infectious disease. 2013 Retrieved from http://www.nhfpc.gov.cn/jkj/s3578/201304/b540269c8e5141e6bb2d00ca539bb9f7.shtml.
- Chinese Center for Disease Control and Prevention. 2014 National report on notifiable infectious disease. 2015 Retrieved from: http://www.nhfpc.gov.cn/jkj/s3578/201502/847c041a3bac4c3e844f17309be0cabd.shtml.
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. doi: 10.1007/BF02310555. [DOI] [Google Scholar]
- De Oliveira IR, Hemmany C, Powell VB, Bonfim TD, Duran EP, Novais N … Brazilian TBTR Study Group. Trial-based psychotherapy and the efficacy of trial-based thought record in changing unhelpful core beliefs and reducing self-criticism. CNS Spectrums. 2012;17(1):16–23. doi: 10.1017/S1092852912000399. [DOI] [PubMed] [Google Scholar]
- Delahanty DL, Bogart LM, Figler JL. Posttraumatic stress disorder symptoms, salivary cortisol, medication adherence, and CD4 levels in HIV-positive individuals. AIDS Care. 2004;16(2):247–260. doi: 10.1080/09540120410001641084. [DOI] [PubMed] [Google Scholar]
- Denzin N, Lincoln Y, editors. Handbook of qualitative research. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- Erekson DM. Unpublished dissertation. Brigham Young University; Salt Lake City, UT: 2013. Scheduled healing: The relationship between session frequency and psychotherapy outcome in a naturalistic setting. [DOI] [PubMed] [Google Scholar]
- Gardner LI, Metsch LR, Anderson-Mahoney P, Loughlin AM, del Rio C, Strathdee S … Antiretroviral Treatment and Access Study Group. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS. 2005;19(4):423–431. doi: 10.1097/01.aids.0000161772. [DOI] [PubMed] [Google Scholar]
- Gortner ET, Gollan JK, Dobson KS, Jacobson NS. Cognitive-behavioral treatment for depression: Relapse prevention. Journal of Consulting and Clinical Psychology. 1998;66(2):377–384. doi: 10.1037/0022-006X.66.2.377. [DOI] [PubMed] [Google Scholar]
- Grossman CI, Gordon CM. Mental health considerations in secondary HIV prevention. AIDS and Behavior. 2010;14(2):263–271. doi: 10.1007/s10461-008-9496-8. [DOI] [PubMed] [Google Scholar]
- Harris CA, D’Eon JL. Psychometric properties of the Beck Depression Inventory-Second Edition (BDI-II) in individuals with chronic pain. Pain. 2008;137(3):609–622. doi: 10.1016/j.pain.2007.10.022. [DOI] [PubMed] [Google Scholar]
- Hill CE, Knox S, Thompson BJ, Williams EN, Hess SA, Ladany N. Consensual qualitative research: An update. Journal of Counseling Psychology. 2005;52(2):196–205. doi: 10.1037/0022-0167.52.2.196. [DOI] [Google Scholar]
- Hwang WC. The psychotherapy adaptation and modification framework: Application to Asian Americans. American Psychologist. 2006;61(7):702–715. doi: 10.1037/0003-066X.61.7.702. [DOI] [PubMed] [Google Scholar]
- Hwang WC. The Formative Method for Adapting Psychotherapy (FMAP): A community-based developmental approach to culturally adapting therapy. Professional Psychology: Research and Practice. 2009;40(4):369–377. doi: 10.1037/a0016240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Labour Organization. Global Wage Report 2012/13. Geneva, Switzerland: International Labour Organization; 2013. Retrieved from: http://www.ilo.org/wcmsp5/groups/public/-dgreports/-dcomm/-publ/documents/publication/wcms_194843.pdf. [Google Scholar]
- Jin H, Atkinson JH, Duarte NA, Yu X, Shi C, Riggs PK … HNRC China Collaboration Group. Risks and predictors of current suicidality in HIV-infected heroin users in treatment in Yunnan, China: A controlled study. Journal of Acquired Immune Deficiency Syndromes (1999) 2013;62(3):311–316. doi: 10.1097/QAI.0b013e31827ce513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin H, Hampton Atkinson J, Yu X, Heaton RK, Shi C, Marcotte TP … HNRC China collaboration group. Depression and suicidality in HIV/AIDS in China. Journal of Affective Disorders. 2006;94(1–3):269–275. doi: 10.1016/j.jad.2006.04.013. [DOI] [PubMed] [Google Scholar]
- Kaner EFS, Dickinson HO, Beyer FR, Campbell F, Schlesinger C, Heather N, … Pienaar ED. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2007. Effectiveness of brief alcohol interventions in primary care populations. [DOI] [PubMed] [Google Scholar]
- Kelly B, Raphael B, Judd F, Perdices M, Kernutt G, Burnett P, … Burrows G. Posttraumatic stress disorder in response to HIV infection. General Hospital Psychiatry. 1998;20(6):345–352. doi: 10.1016/S0163-8343(98)00042-5. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Neurasthenia and depression: A study of somatization and culture in China. Culture, Medicine and Psychiatry. 1982;6(2):117–190. doi: 10.1007/BF00051427. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Culture and depression: Studies in the anthropology and cross-cultural psychiatry of affect and disorder. Berkeley, CA: University of California Press; 1985. [Google Scholar]
- Koopman JS, Jacquez JA, Welch GW, Simon CP, Foxman B, Pollock SM, … Lange K. The role of early HIV infection in the spread of HIV through populations. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1997;14(3):249–258. doi: 10.1097/00042560-199703010-00009. [DOI] [PubMed] [Google Scholar]
- Lee E, editor. Working with Asian Americans: A guide for clinicians. New York: Guilford Press; 1997. [Google Scholar]
- Leong FTL. Cultural accommodation as method and metaphor. The American Psychologist. 2007;62(8):913–927. doi: 10.1037/0003-066X.62.8.916. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Liu XC, Oda S, Peng X, Asai K. Life events and anxiety in Chinese medical students. Social Psychiatry and Psychiatric Epidemiology. 1997;32(2):63–67. doi: 10.1007/BF00788922. [DOI] [PubMed] [Google Scholar]
- Martell CR, Dimidjian S, Herman-Dunn R. Behavioral activation for depression: A clinician’s guide. New York: Guilford Press; 2010. [Google Scholar]
- Martinez A, Israelski D, Walker C, Koopman C. Posttraumatic Stress Disorder in Women Attending Human Immunodeficiency Virus Outpatient Clinics. AIDS Patient Care and STDs. 2002;16(6):283–291. doi: 10.1089/10872910260066714. [DOI] [PubMed] [Google Scholar]
- Meade CS, Wang J, Lin X, Wu H, Poppen PJ. Stress and coping in HIV-positive former plasma/blood donors in China: A test of cognitive appraisal theory. AIDS and Behavior. 2010;14(2):328–338. doi: 10.1007/s10461-008-9494-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: SAGE; 1994. [Google Scholar]
- Montgomery EC, Kunik ME, Wilson N, Stanley MA, Weiss B. Can paraprofessionals deliver cognitive-behavioral therapy to treat anxiety and depressive symptoms? Bulletin of the Menninger Clinic. 2010;74(1):45–62. doi: 10.1521/bumc.2010.74.1.45. [DOI] [PubMed] [Google Scholar]
- Mundy E, Baum A. Medical disorders as a cause of psychological trauma and posttraumatic stress disorder. Current Opinion in Psychiatry. 2004;17(2):123–127. doi: 10.1097/00001504-200403000-00009. [DOI] [Google Scholar]
- Naar-King S, Bradford J, Coleman S, Green-Jones M, Cabral H, Tobias C. Retention in Care of Persons Recently Diagnosed with HIV: Outcomes of the Outreach Initiative. AIDS Patient Care and STDs. 2007;21(s1):S-40. doi: 10.1089/apc.2007.9988. [DOI] [PubMed] [Google Scholar]
- Ng CTC, James S. “Directive approach” for Chinese clients receiving psychotherapy: Is that really a priority. Frontiers in Psychology. 2013;4:49. doi: 10.3389/fpsyg.2013.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu L, Luo D, Liu Y, Silenzio VMB, Xiao S. The mental health of people living with HIV in China, 1998–2014: A systematic review. PLOS ONE. 2016;11(4):e0153489. doi: 10.1371/journal.pone.0153489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell A, Wallace P, Kaner E. From efficacy to effectiveness and beyond: What next for brief interventions in primary care? Frontiers in Psychiatry. 2014;5:113. doi: 10.3389/fpsyt.2014.00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olley BO, Zeier MD, Seedat S, Stein DJ. Post-traumatic stress disorder among recently diagnosed patients with HIV/AIDS in South Africa. AIDS Care. 2005;17(5):550–557. doi: 10.1080/09540120412331319741. [DOI] [PubMed] [Google Scholar]
- Panos PT, Jackson JW, Hasan O, Panos A. Meta-analysis and systematic review assessing the efficacy of dialectical behavior therapy (DBT) Research on Social Work Practice. 2013;24(2):213–223. doi: 10.1177/1049731513503047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker G, Cheah YC, Roy K. Do the Chinese somatize depression? A cross-cultural study. Social Psychiatry and Psychiatric Epidemiology. 2001;36(6):287–293. doi: 10.1007/s001270170046. [DOI] [PubMed] [Google Scholar]
- Porter JF, Spates CR, Smitham S. Behavioral activation group therapy in public mental health settings: A pilot investigation. Professional Psychology: Research and Practice. 2004;35(3):297–301. doi: 10.1037/0735-7028.35.3.297. [DOI] [Google Scholar]
- Quinn TC, Wawer MJ, Sewankambo N, Serwadda D, Li C, Wabwire-Mangen F, … Gray RH. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. The New England Journal of Medicine. 2000;342(13):921–929. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- Rao D, Chen WT, Pearson CR, Simoni JM, Fredriksen-Goldsen K, … Zhang F. Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. International Journal of STD & AIDS. 2012;23(7):481–484. doi: 10.1258/ijsa.2009.009428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao Y. AIDS epidemic at age 25 and control efforts in China. Retrovirology. 2006;3:87. doi: 10.1186/1742-4690-3-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shek DT. Reliability and factorial structure of the Chinese version of the Beck Depression Inventory. Journal of Clinical Psychology. 1990;46(1):35–43. doi: 10.1002/1097-4679(199001)46:1<35::AID-JCLP2270460106>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- Sherr L, Nagra N, Kulubya G, Catalan J, Clucas C, Harding R. HIV infection associated post-traumatic stress disorder and post-traumatic growth – A systematic review. Psychology, Health & Medicine. 2011;16(5):612–629. doi: 10.1080/13548506.2011.579991. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Abler L, Hansen NB, Wilson PA, Drabkin AS, Kochman A, … Nazareth W. Positive Choices: Outcomes of a brief risk reduction intervention for recently HIV-diagnosed men who have sex with men. AIDS and Behavior. 2014;18(9):1808–1819. doi: 10.1007/s10461-014-0782-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Kochman A, Santos J, Watt MH, Wilson PA, … Mayer G. The development and feasibility of a brief risk reduction intervention for recently HIV-diagnosed men who have sex with men. Journal of Community Psychology. 2011;39(6):717–732. doi: 10.1002/jcop.20463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Watt MH, Drabkin AS, Meade CS, Hansen NB, Pence BW. Mental health treatment to reduce HIV transmission risk behavior: A positive prevention model. AIDS and Behavior. 2010;14(2):252–262. doi: 10.1007/s10461-009-9650-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Yang JP, Porricolo M. Families and HIV Medication Adherence. In: Pequegnat W, Bell CC, editors. Family and HIV/AIDS. New York: Springer; 2012. pp. 209–226. [Google Scholar]
- Simoni JM, Yang JP, Shiu CS, Chen WT, Udell W, Bao M, … Lu H. Nurse-delivered counselling intervention for parental HIV disclosure: Results from a pilot randomized controlled trial in China. AIDS. 2015;29(Suppl 1):S99–S107. doi: 10.1097/QAD.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9) Arthritis Care & Research. 2011;63(S11):S454–S466. doi: 10.1002/acr.20556. [DOI] [PubMed] [Google Scholar]
- St Lawrence JS, Eldridge GD, Shelby MC, Little CE, Brasfield TL, O’Bannon RE., III HIV risk reduction for incarcerated women: A comparison of brief interventions based on two theoretical models. Journal of Consulting and Clinical Psychology. 1997;65(3):504–509. doi: 10.1037/0022-006X.65.3.504. [DOI] [PubMed] [Google Scholar]
- Su X, Lau JTF, Mak WWS, Choi KC, Chen L, Song J, … Cheng J. Prevalence and associated factors of depression among people living with HIV in two cities in China. Journal of Affective Disorders. 2013;149(1–3):108–115. doi: 10.1016/j.jad.2013.01.011. [DOI] [PubMed] [Google Scholar]
- Uba L. Asian Americans: Personality patterns, identity, and mental health. New York: The Guilford Press; 1994. [Google Scholar]
- UNAIDS. 2015 China AIDS Response Progress Report. 2015 Retrieved from: http://www.unaids.org/sites/default/files/country/documents/CHN_narrative_report_2015.pdf.
- Wagner AW, Zatzick DF, Ghesquiere A, Jurkovich GJ. Behavioral activation as an early intervention for posttraumatic stress disorder and depression among physically injured trauma survivors. Cognitive and Behavioral Practice. 2007;14(4):341–349. doi: 10.1016/j.cbpra.2006.05.002. [DOI] [Google Scholar]
- Wagner GJ, Goggin K, Remien RH, Rosen MI, Simoni J, Bangsberg DR, Liu H. A closer look at depression and its relationship to HIV antiretroviral adherence. Annals of Behavioral Medicine. 2011;42(3):352–360. doi: 10.1007/s12160-011-9295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Lin X, Wu H, Qu W. The mood state of paid blood donors with HIV and its relation to stress and cognitive appraisal. Acta Psychologica Sinica. 2005;37:106–112. Retrieved from: http://en.cnki.com.cn/Article_en/CJFDTOTAL-XLXB200501015.htm. [Google Scholar]
- Weinhardt LS. HIV diagnosis and risk behavior. In: Kalichman SC, editor. Positive prevention: Reducing HIV transmission among people living with HIV/AIDS. New York: Kluwer Academic; 2005. [Google Scholar]
- World Health Organization. Mental Health Atlas. Geneva, Switzerland: WHO Press; 2005. [Google Scholar]
- World Health Organization. Task shifting: Global recommendations and guidelines. Geneva, Switzerland: WHO Press; 2008. [Google Scholar]
- Xie TY, Yang JP, Simoni JM, Shiu CS, Chen WT, Lu HZ, Zhao HX. “Unable to be a human being in front of other people”: A study of self-isolation among people living with HIV/AIDS in China. Journal of Clinical Psychology in Medical Settings. 2017 doi: 10.1007/s10880-017-9513-z. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang JP, Leu J, Simoni JM, Chen WT, Shiu CS, Zhao H. “Please Don’t Make Me Ask for Help”: Implicit social support and mental health in Chinese individuals living with HIV. AIDS and Behavior. 2015;19(8):1501–1509. doi: 10.1007/s10461-015-1041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang JP, Simoni JM, Dorsey S, Lin Z, Sun M, Bao M, Lu Z. Pilot-testing a distress reduction intervention among MSM recently HIV-diagnosed in China Under review; a. [Google Scholar]
- Yang JP, Xie T, Simoni JM, Shiu CS, Chen WT, Zhao H, Lu H. A Mixed-Methods Study Supporting a Model of Chinese Parental HIV Disclosure. AIDS and Behavior. 2016;20(1):165–173. doi: 10.1007/s10461-015-1070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Li X, Liu Y, Qiao S, Zhang L, Zhou Y, … Tang ZZ. Emotional, physical, and financial burdens of stigma against people living with HIV/AIDS in China. AIDS Care. 2016;28(Sup1):124–131. doi: 10.1080/09540121.2016.1146206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Liu R, Li G, Mao S, Yuan Y. The reliability and validity of a Chinese-version Short Health Anxiety Inventory: An investigation of university students. Neuropsychiatric Disease and Treatment. 2015;11:1739–1747. doi: 10.2147/NDT.S83501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng YP, Wei LA, Goa LG, Zhang GC, Wong CG. Applicability of the Chinese Beck Depression Inventory. Comprehensive Psychiatry. 1988;29(5):484–489. doi: 10.1016/0010-440X(88)90063-6. [DOI] [PubMed] [Google Scholar]
- Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]