Abstract
Objective:
Prior research indicates that adults’ implicit identification with death can be used to predict suicidal thoughts and behaviors (STBs) in the community. However, no studies have examined whether this effect is found among adolescents—a group for whom suicide is the 2nd leading cause of death. The current study tested the utility of implicit identification with death, using a Death Implicit Association Test (Death IAT), for detecting and predicting STBs in adolescents.
Method:
Participants were 141 adolescents aged 12–19 years (81.6% female; 74.5% White) with a current psychiatric disorder and/or currently receiving outpatient psychiatric treatment. All participants completed the Death IAT and self-report measures of STBs at baseline, as well as self-report measures of STBs at 6-month and 1-year follow-ups.
Results:
At baseline, stronger implicit identification with death (higher Death IAT score) was related to greater suicide ideation (SI) frequency, severity, and duration, but did not differ based on suicide attempt history. Prospectively, higher Death IAT scores predicted any occurrence (but not frequency) of SI over the subsequent year, but not when controlling for prior SI. Death IAT scores were higher among adolescents with prior attempts who reattempted suicide over the follow-up. Examination of stimuli-level results suggested that Death IAT differences may be driven by responses on trials with specific words, including “Suicide” and “Die”.
Conclusions:
Implicit identification with death may be a useful behavioral indicator of suicide risk in adolescents. Preliminary findings suggest that the Death IAT may aid in predicting STBs among youth receiving outpatient treatment.
Keywords: adolescence, implicit association test, prediction, suicide, suicide attempts
Suicidal thoughts and behaviors (STBs) are serious public health concerns in youth. Suicide is the 2nd leading cause of death among 10–19 year-olds (CDC, 2017a), and, in 2017, 17.2% of high school students reported seriously considering suicide and 7.4% reported at least one suicide attempt (SA) in the past year (CDC, 2017b). STBs are associated with significant academic and social impairment (Copeland, Goldston, & Costello, 2017) and substantial cost to the healthcare system (CDC, 2017a).
One major limitation of current approaches to suicide risk determination is the reliance on self-reported risk. Although asking patients directly about their suicidal thinking is currently best practice (NAASP, 2014), self-reports of suicide risk may be limited by: (a) motivation to conceal suicide risk (e.g., to avoid hospitalization), (b) the transient nature of suicidal thoughts (Kleiman et al., 2017), and (c) limited access to psychological processes underlying behavior (Nisbett & Wilson, 1977). These limitations are exemplified in an inpatient study finding that nearly 80% of patients who died by suicide had denied suicidal thoughts during their last communication with hospital staff (Busch, Fawcett, & Jacobs, 2003). Moreover, two commonly used self-report suicide risk scales (Beck Hopelessness Scale and Beck Suicide Intent Scale) demonstrated low-to-moderate sensitivity and low specificity when predicting suicide in high-risk samples (Chan et al., 2016). Thus, assessing suicide risk by self-report alone seems insufficient and may be improved by augmenting existing approaches with more objective tools.
Implicit identification with death
One more objective approach to suicide risk assessment comes from research indicating that implicit identification with self-harm may provide unique information about suicide risk beyond both patient and clinician reports of risk. The most commonly used tool to examine implicit self-harm cognitions is the Implicit Association Test (IAT; Greenwald, McGhee, & Schwartz, 1998), specifically measuring implicit identification with non-suicidal self-injury (Self-Injury IAT), death (Death IAT), and suicide methods (Suicide IAT; Glenn, Werntz et al., 2017). Implicit measures may overcome some important shortcomings of self-reports because they do not rely on introspection (Greenwald & Banaji, 1995), may be more resistant to faking good than explicit self-reports (Banse, Seise, & Zerbes, 2001), and fluctuate in accordance with changes in clinical symptoms (Teachman, Marker, & Smith-Janik, 2008).
The most tested and promising of the self-harm IATs is the Death IAT, which examines implicit identification with the concepts of death and life (Nock et al., 2010).1 Previous research indicates that stronger implicit identification with death correlates with the frequency, severity, and recency of STBs among adults in the community (Glenn, Werntz, et al., 2017; Millner, Coppersmith, Teachman, & Nock, 2018). Moreover, several studies have found that stronger implicit identification with death predicts future suicide ideation (SI; Ellis, Rufino, & Green, 2016) and SA among acute clinical samples of adults (Barnes et al., 2017; Nock et al., 2010; Randall, Rowe, Dong, Nock, & Colman, 2013). However, little research has examined these effects among adolescents.
Three studies have examined the Death IAT among youth receiving acute psychiatric treatment.2 Two studies combined the Death IAT with other self-harm IATs (Dickstein et al., 2015; Millner, Augenstein, et al., 2018) and one exclusively tested the Death IAT (Glenn, Kleiman, et al., 2017). Cross-sectional findings indicate small (Glenn, Kleiman, et al., 2017) to medium (Millner, Augenstein, et al., 2018) associations between the Death IAT and self-reported SI frequency and severity. STB group differences on the Death IAT are mixed. In one study, the Death IAT did not distinguish suicide attempters from ideators (Glenn, Kleiman, et al., 2017), whereas Death/Suicide combined IATs distinguished attempters from nonsuicidal controls in one study (Millner, Augenstein, et al., 2018) but another study failed to find such differences (Dickstein et al., 2015). Prospective research revealed that higher Death IAT scores at hospital admission predicted greater SI at hospital discharge, controlling for SI at admission (Glenn, Kleiman, et al., 2017). However, no studies have specifically examined the Death IAT’s utility for predicting SA in youth.
Current study
This study extended research on the Death IAT to youth outside of acute psychiatric care and had three main aims. First, we examined whether adolescents with more recent and severe STBs exhibited stronger implicit identification with death, similar to adult studies. Second, we tested whether stronger implicit identification with death predicted STBs (i.e., SI and suicide reattempts [see Data Analysis]) over a 1-year follow-up, consistent with adult findings. Our third aim was exploratory and tested (cross-sectionally and prospectively) whether implicit identification with any particular Death IAT word predicted STBs.
Method
Participants
Adolescents were recruited as part of a larger study aimed at identifying objective risk markers for STBs. Inclusion criteria were: 12–19 years-old, fluent in English, and a current mood or anxiety disorder and/or receiving current outpatient psychiatric treatment. Exclusion criteria were: color-blindness (for a separate color-naming task), high/imminent risk for suicide (referred to treatment instead), acute psychosis, violence risk, developmental or neurological disorder, or cognitive impairment preventing informed consent or participation. Based on these criteria, 158 adolescents were enrolled from November 2012-August 2015. Seventeen adolescents (10.8%) were excluded from analyses for: absence of a psychiatric disorder (n=5), significant cognitive impairment (n=6), unreliable/incomplete STB data (n=3), or unusable Death IAT data (n=3). The final sample for the baseline analyses included 141 adolescents (Table 1).3 Prospective STB analyses included 131 adolescents at the 6-month follow-up and 124 at the 1-year follow-up. Prediction of suicidal behavior focused on adolescent who reattempted suicide over the 1-year follow-up (n=5; see Data Analysis).
Table 1.
Sample sociodemographics and current major psychiatric disorders based on history of suicidal thoughts and behaviors.
| Total Sample (N=141) | Nonsuicidal Psychiatric Controls (n=35) | Lifetime Suicide Ideators (n=12) | Past-year Suicide Ideators (n=42) | Lifetime Suicide Attempters (n=30) | Past-year Suicide Attempters (n=22) | |
|---|---|---|---|---|---|---|
| Age: Mean (SD) | 17.52 (1.64) | 17.40 (1.63) | 18.00 (1.65) | 17.37 (1.67) | 18.03 (1.07) | 17.05 (2.10) |
| Gender: % (n) | ||||||
| Female | 81.6% (115) | 80.0% (28) | 75.0% (9) | 76.2% (32) | 93.3% (28) | 81.8% (18) |
| Male | 16.3% (23) | 20.0% (7) | 25.0% (3) | 19.0% (8) | 3.3% (1) | 18.2% (4) |
| Other/Non-binary | 2.1% (3) | --- | --- | 4.8% (2) | 3.3% (1) | --- |
| Race and Ethnicity1: % (n) | ||||||
| White/Caucasian | 74.5% (105) | 74.3% (26) | 50.0% (6) | 78.6% (33) | 80.0% (24) | 72.7% (16) |
| Black/African American | 5.0% (7) | 8.6% (3) | 8.3% (1) | 7.1% (3) | --- | --- |
| Asian | 5.0% (7) | --- | 16.7% (2) | 9.5% (4) | --- | --- |
| American Indian/Alaskan Native | 0.7% (1) | --- | 8.3% (1) | --- | --- | --- |
| Other/Multi-racial | 13.5% (19) | 14.3% (5) | 16.7% (2) | 4.8% (2) | 16.7% (5) | 22.7% (5) |
| Hispanic/Latinx | 14.9% (21) | 20.0% (7) | --- | 11.9% (5) | 20.0% (6) | 13.6% (3) |
| Annual Household Income1: % (n) | ||||||
| < $40,000 | 21.3% (30) | 28.6% (10) | 16.7% (2) | 19.0% (8) | 20.0% (6) | 18.2% (4) |
| $40,000-$80,000 | 30.5% (43) | 25.7% (9) | 25.0% (3) | 28.6% (12) | 43.4% (13) | 27.3% (6) |
| > $80,000 | 46.8% (66) | 45.7% (16) | 58.3% (7) | 52.4% (22) | 30.0% (9) | 54.5% (12) |
| Current Major Psychiatric Disorders2: % (n) | ||||||
| Anxiety Disorder | 70.9% (100) | 74.3% (26) | 58.3% (7) | 71.4% (30) | 66.7% (20) | 77.3% (17) |
| ADHD | 12.1% (17) | 2.9% (1) | 16.7% (2) | 16.7% (7) | 10.0% (3) | 18.2% (4) |
| Bipolar Disorder | 0.7% (1) | --- | --- | 2.4% (1) | --- | --- |
| Depressive Disorder | 43.3% (61) | 28.6% (10) | 8.3% (1) | 42.9% (18) | 53.3% (16) | 72.7% (16) |
| DBD | 20.6% (29) | 11.4% (4) | 16.7% (2) | 16.7% (7) | 30.0% (9) | 31.8% (7) |
| Eating Disorder | 8.5% (12) | 5.7% (2) | --- | 7.1% (3) | 10.0% (3) | 18.2% (4) |
| OCD | 7.1% (10) | 5.7% (2) | --- | 7.1% (3) | 10.0% (3) | 9.1% (2) |
| PTSD | 18.4% (26) | 5.7% (2) | 25% (3) | 19% (8) | 16.7% (5) | 36.4% (8) |
| SUD | 30.5% (43) | 22.9% (8) | 41.7% (5) | 14.3% (6) | 46.7% (14) | 45.5% (10) |
Two missing values for race and one missing value for annual household income.
Anxiety disorder includes any of the following current disorders: panic disorder, agoraphobia, social phobia, specific phobia, or generalized anxiety disorder; ADHD=Attention-Deficit Hyperactivity Disorder includes any of the following current subtypes: combined, inattentive, or hyperactive/impulsive; Bipolar Disorder includes current bipolar I or II disorder; Depressive Disorder includes current major depressive disorder or dysthymia; DBD=Disruptive Behavior Disorder includes current conduct disorder or oppositional defiant disorder; Eating Disorder includes current anorexia nervosa or bulimia nervosa; OCD=Obsessive Compulsive Disorder; PTSD=Posttraumatic Stress Disorder; SUD=Substance Use Disorder includes current alcohol abuse/dependence or substance (drug) abuse/dependence.
Measures
Suicidal thoughts and behaviors.
The Self-Injurious Thoughts and Behaviors Interview (SITBI; Nock, Holmberg, Photo, & Michel, 2007) assessed the frequency of STBs and nonsuicidal self-injury (NSSI) over adolescents’ lifetime and past year. Adolescents were classified at baseline based on the severity and recency of STBs.4 An abbreviated version of the SITBI was administered during the follow-up assessments to measure the presence, frequency, and recency of STBs over the 1-year follow-up. The SITBI has demonstrated good-excellent reliability and validity with community and outpatient adolescents (Nock et al., 2007). Additionally, the first 19 items of the Beck Scale for Suicide Ideation (BSI; Beck & Steer, 1991) were used to assess severity of past-week suicidal thinking at baseline.
Implicit identification with death.
The Death Implicit Association Test (Death IAT) is a brief (5-minute), computer-based behavioral task that uses reaction times (RT) when classifying words to measure implicit associations between death and the self (vs. life and the self; Nock et al., 2010). Specifically, words related to “Death” (e.g., Die, Suicide) and “Life” (e.g., Alive, Survive) are paired with either “Me” or “Not Me” stimuli (i.e., Death & Me/Life & Not Me are paired on ½ trials and Life & Me/Death & Not Me on the other ½ trials). Implicit identification with death is indexed with a difference (D) score for each participant between trials when Death & Me/Life & Not Me are paired compared to trials when Life & Me/Death & Not Me are paired: positive D scores indicate stronger implicit identification with death (i.e., faster RT on Death & Me paired trials than on Life & Me paired trials), whereas negative D scores indicate stronger implicit identification with life (Nock et al., 2010).5
Major psychiatric disorders.
The Mini International Neuropsychiatric Interview for children and adolescents (MINI-Kid; Sheehan et al., 2010) is a structured diagnostic interview used in this study to assess the presence of current major DSM-IV diagnoses. The MINI-Kid has demonstrated good psychometric properties in youth (Sheehan et al., 2010) and has been used in previous studies with community and outpatient adolescents (e.g., Miller et al., 2017).
Procedure
Study procedures were approved by the University’s Institutional Review Board. Participants were recruited through online (e.g., Facebook, craigslist) and printed advertisements posted in clinical settings, community bulletin boards, and other public spaces. Interested participants completed a brief phone screening based on the inclusion and exclusion criteria. Eligible participants were referred for the initial lab-based assessment.
Participants completed three assessments. Adolescent assent/consent and parent permission (for adolescents 12–17 years-old) was provided prior to study initiation. The first assessment (baseline) was a 3-hour lab visit that included: self-report measures (e.g., BSI), diagnostic interviews (i.e., MINI-Kid, SITBI) administered by a PhD-level clinical psychologist, and behavioral tasks (e.g., Death IAT was administered using Inquisit software v.3.0.6). Risk assessments and safety plans were completed with each adolescent at the end of the lab visit.
The second and third assessments occurred over the phone approximately six months (M=190.01 days, SD=12.41) and one year (M=371.16 days, SD=12.69) after baseline. Retention over the follow-up was 92.9% at 6-months and 87.9% at 1-year. Follow-ups, measuring STBs since the prior assessment using an abbreviated SITBI, lasted 15–30 minutes and were conducted by the same PhD-level clinical psychologist or by a post-baccalaureate research assistant trained to reliability with the PhD-level interviewer. Risk assessments were performed at the end of each follow-up. Participants were compensated with cash (baseline) and gift cards (follow-ups).
Data analysis
Cross-sectional associations between the Death IAT and STBs were tested in the following ways: (1) One-way ANOVA examined differences in Death IAT scores based on severity and recency of STBs.4 Significant omnibus tests were explored with post-hoc comparisons (Tukey’s HSD). If group variances were significantly unequal, groups were compared using Welch’s F test, omega squared for effect size, and Games-Howell post-hoc comparisons. The Benjamini–Hochberg procedure (Benjamini & Hochberg, 1995) was used to control the familywise error rate. (2) Spearman correlations (for non-normally distributed data) examined associations between continuous STBs (e.g., BSI scores) and the Death IAT. (3) A negative binomial hurdle model (NBH) examined cross-sectional associations of Death IAT scores with any SI (dichotomous) and days of SI (continuous) at baseline using the pscl package in R (Zeileis, Kleiber, & Jackman, 2008). A NBH model was selected to account for excessive zero counts and overdispersion in the SI data (Hilbe, 2014), and enabled examination of the Death IAT’s association with any occurrence of SI and frequency (days) of SI among those endorsing SI.
Prospective associations were examined between the Death IAT at baseline and STBs over the 1-year follow-up. A NBH model was used to examine the Death IAT’s prediction of the occurrence and frequency (days) of SI at the 6-month and 1-year follow-up in two steps: (1) the Death IAT examined alone, and (2) the Death IAT examined controlling for past-year SI, past-year NSSI, and SA history. To account for overdispersion and outliers, and to improve the interpretability of estimates, past-year SI and NSSI were ranked and standardized prior to being entered in the model. Participants with longitudinal data missing at the assessment or measure level were dropped from the analyses (listwise deletion).
For prospective suicidal behavior, we examined Death IAT differences between adolescents who attempted suicide over the 1-year follow-up period and those who did not. Of the six adolescents (4.3% of baseline sample) who attempted suicide over the follow-up, five were reattempts (i.e., those with a prior SA who reattempted over the follow-up). To be conservative, we tested the predictive utility of the Death IAT only among adolescents with a prior SA who were retained over the follow-up (n=45). Due to the small sample, a series of independent samples t tests compared: (1) adolescents with a prior attempt who did not reattempt over follow-up (non-reattempters; n=40) and (2) adolescents with a prior attempt who did reattempt over follow-up (suicide reattempters; n=5). We also examined how reattempters and non-reattempters differed in their explicit prediction of suicide risk at baseline by comparing groups on the SITBI item, “What are the chances that you will make a suicide attempt in the future?” rated from 0=Not at all to 4=Extremely.
Next, we calculated classification metrics (i.e., area under the curve for the receiver operator characteristic curve; AUC-ROC) to test how well the Death IAT classified follow-up reattempters from non-reattempters. We tested two AUC-ROCs; one based on whether the D score was above or below zero (i.e., zero threshold) and the other based on a non-zero D score (i.e., the criterion threshold could be set at any D score value). We provide 95% bootstrapped confidence intervals with 2,000 re-samples for each ROC.
Finally, exploratory analyses (cross-sectional and prospective) examined whether some IAT stimuli were more predictive than others by creating D scores for each “Death” and “Life” category IAT word. Prior studies have used a similar approach to explore overall IAT effects (e.g., Karpinski & Hilton, 2001). Like the overall D score, stimuli-level positive D scores indicate faster RT when categorizing an IAT word (e.g., “Die”) on Death & Me/Life & Not Me paired trials and negative D scores represent faster RT when categorizing the word on Life & Me/Death & Not Me paired trials (Table 3). We used the same approach as the planned analyses (ANOVA for cross-sectional and t tests for prospective) and did not correct for multiple comparisons because analyses were exploratory.
Table 3.
Performance on the Death IAT among adolescents with a suicide attempt history who did (Suicide Reattempters) or did not reattempt suicide (Non-reattempters) over the 1-year follow-up period.
| Suicide Reattempters (n=5) | Non-reattempters (n=40) | Group comparison1 | |||
|---|---|---|---|---|---|
| M (SD) | M (SD) | t | p | d | |
| Overall Death IAT D score | .06 (.37) | −.45 (.35) | 3.04 | .004 | 1.45 |
| Individual “Death” & “Me” | |||||
| D scores:2 | |||||
| “Deceased” | .15 (1.39) | −.69 (.99) | 1.72 | .093 | 0.82 |
| “Die” | .29 (.54) | −.66 (.87) | 2.37 | .022 | 1.12 |
| “Funeral” | −1.15 (.59) | −.93 (.66) | −0.73 | .471 | −0.35 |
| “Lifeless” | .42 (1.03) | −.53 (1.02) | 1.96 | .057 | 0.93 |
| “Suicide” | .65 (1.00) | −.09 (1.10) | 1.42 | .163 | 0.67 |
| Individual “Life” & “Not Me” | |||||
| D scores:2 | |||||
| “Alive” | −.35 (1.15) | −.67 (0.82) | 0.79 | .435 | 0.37 |
| “Breathing” | −.22 (1.00) | −.46 (1.08) | 0.47 | .642 | 0.22 |
| “Live” | .48 (.80) | −.80 (.90) | 3.05 | .004 | 1.44 |
| “Survive” | −.09 (.72) | −.42 (1.01) | 0.71 | .482 | 0.33 |
| “Thrive” | −.01 (.85) | −.48 (.89) | 1.11 | .272 | 0.53 |
Categorical group differences were examined using independent samples t tests and Cohen’s d for effect size.
Positive scores indicate faster reaction times (i.e., stronger associations) when classifying a word on trials when “Death” & “Me” / “Life” & “Not Me” are paired compared to the reverse pairing (i.e., trials when “Death” & “Not Me” / “Life” & “Me” are paired).
Results
Cross-sectional examination of the Death IAT
Death IAT scores did not differ based on lifetime severity of STBs at baseline. Although there was a trend toward higher Death IAT scores among suicide attempters (M=−.35, SD=.43) and suicide planners (M=−.34, SD=.43) compared to suicide ideators (M=−.55, SD=.39) and nonsuicidal controls (M=−.52, SD=.36), the overall group effect was not statistically significant, F(3,139)=2.41, p=.069, η2=.050.
The NBH model indicated that the Death IAT was positively associated with the occurrence of past-year SI at baseline (b=0.54, SE=0.19, OR=1.71, 95% CI[1.18,2.50]), but not with SI frequency among those with any SI occurrence (b=0.12, SE=0.12, IRR=1.12, 95% CI[0.90,1.41]). The Death IAT remained significantly associated with the occurrence of past-year SI when controlling for past-year NSSI and SA history (b=0.55, SE=0.22, OR=1.73, 95% CI [1.12,2.68]). In terms of associations with SI severity and duration, there was a small correlation between Death IAT scores and severity of past-week SI (BSI), rs(139)=.28, p=.001, and duration (years) of SI prior to baseline: rs(139)=.18, p=.037.
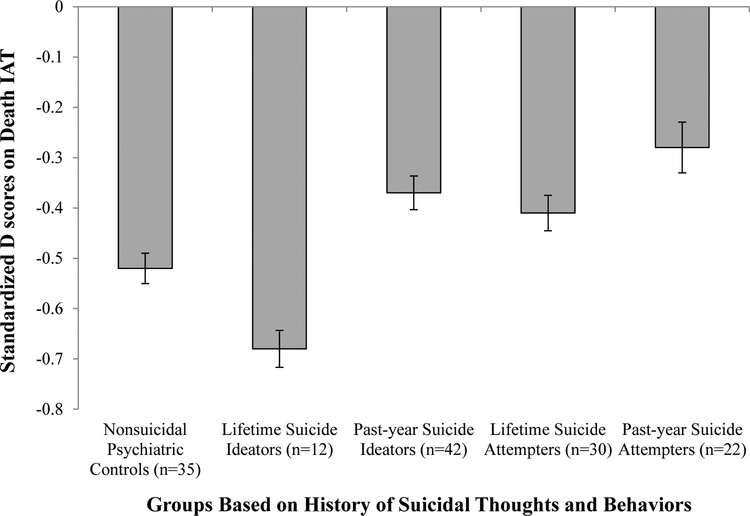
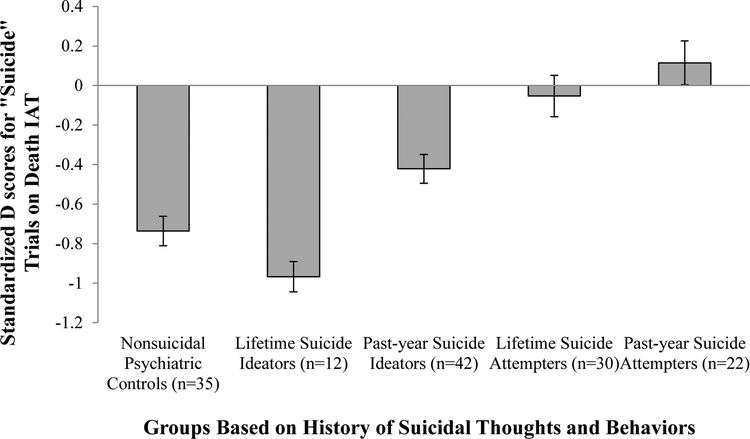
Next, we examined how Death IAT scores varied as a function of severity and recency of STBs (Figure 1). Although the overall ANOVA revealed significant between-group differences (p=.037, η2=0.07), no groups significantly differed from each other (ps>.18). However, there was a trend for higher D scores among past-year attempters compared to lifetime ideators (p=.053). In stimuli-level exploratory analyses, there was a significant group effect on trials with the word “Suicide” (p=.001, ω2=.12). That is, groups with more recent and severe STBs showed higher D scores for “Suicide” trials and past-year suicide attempters showed a positive D score (Figure 2). There was a trend group difference for the word “Die” (F[4,136]=2.21, p=.072), but no other stimuli-specific group differences (ps>.15).
Figure 1.
Performance on the Death IAT at the baseline assessment among adolescents based on history of suicidal thoughts and behaviors, F(4, 136)=2.64, p=.037, η2=0.07. Post-hoc comparisons (Tukey’s HSD) indicated that no groups were statistically significantly different from each other. However, lifetime suicide ideators had more negative D scores than past-year suicide attempters at a trend level (p=.053). Error bars indicate standard error of the mean.
Figure 2.
Performance on “Suicide” word trials of the Death IAT at the baseline assessment among adolescents based on history of suicidal thoughts and behaviors, Welch’s F(4, 54.98)=5.84, p=.001, ω2=.12. Post-hoc comparisons (Games-Howell) indicated significant differences between: lifetime suicide ideators < past-year suicide attempters (p=.003), lifetime suicide ideators < lifetime suicide attempters (p=.009), and nonsuicidal psychiatric controls < past-year suicide attempters (p=.023). Error bars indicate standard error of the mean.
Predictive utility of the Death IAT
Results from the prospective NBH models are presented in Table 2. Examined alone, the Death IAT predicted the occurrence of any SI at the 6-month follow-up at a trend level (OR=1.48, 95% CI[0.98,2.23]) and significantly at the 1-year follow-up (OR=1.58, 95% CI[1.05,2.40]). However, the effects were no longer significant after controlling for past-year SI, past-year NSSI, and SA history. Among those reporting SI over the follow-up, the Death IAT was not a significant predictor of SI frequency.
Table 2.
Negative binomial hurdle model results for Death IAT predicting suicide ideation (SI) over the 6-month and 1-year follow-ups.
| 6-Month Follow-up | |||||||
|---|---|---|---|---|---|---|---|
| Predicting Any Occurrence of SI (n=131) | Predicting Days of SI (n=43) | ||||||
| Predictors | b | SE | P | b | SE | P | |
| Step 1: | |||||||
| Death IAT D score | 0.39 | 0.21 | .069 | −0.12 | 0.18 | .489 | |
| Step 2: | |||||||
| Death IAT D score | 0.15 | 0.24 | .530 | −0.12 | 0.12 | .306 | |
| Days of SI in year before baseline | 1.63 | 0.31 | <.001 | 1.04 | 0.30 | <.001 | |
| Days of NSSI in year before baseline | -0.34 | 0.30 | .257 | 0.07 | 0.23 | .758 | |
| Suicide attempt history (Yes/No) at baseline | 0.24 | 0.53 | .656 | −0.53 | 0.36 | .151 | |
| 1-Year Follow-up | |||||||
|---|---|---|---|---|---|---|---|
| Predicting Any Occurrence of SI (n=124) | Predicting Days of SI (n=40) | ||||||
| Predictors | b | SE | P | b | SE | P | |
| Step 1: | |||||||
| Death IAT D score | 0.46 | 0.21 | .032 | −0.03 | 0.21 | .898 | |
| Step 2: | |||||||
| Death IAT D score | 0.17 | 0.24 | .475 | −0.11 | 0.22 | .621 | |
| Days of SI from baseline to 6-month follow-up | 1.32 | 0.26 | <.001 | −0.10 | 0.29 | .727 | |
| Days of NSSI in year before baseline | 0.28 | 0.33 | .404 | 0.17 | 0.22 | .428 | |
| Suicide attempt history (Yes/No) at baseline | 0.006 | 0.60 | .992 | -0.02 | 0.65 | .972 | |
NSSI=nonsuicidal self-injury
For the full model at the 6-month follow-up: -LL(11)=−219.4; AIC=460.82; BIC=492.28; α=1.11; dispersion=1.37. For the full model at the 1-year follow-up: -LL(11)=−211.4; AIC=444.38; BIC=475.13; α=3.35; dispersion=1.03. To account for any additional extradispersion, robust sandwich standard errors were estimated and are presented in this table (Hilbe, 2014).
Results indicated significantly higher Death IAT scores at baseline among adolescents who reattempted suicide over the 1-year follow-up compared to adolescents who did not reattempt (p=.004).6 When predicting suicide reattempts over the 1-year follow-up, the Death IAT (continuous score) produced an AUC of 0.85 (95% CI[0.64, 0.99]), indicating good accuracy. In addition, a clinically useful, zero-threshold Death IAT score (i.e., D scores were coded as either <0=stronger identification with life or >0=stronger identification with death) produced an AUC of 0.76 (95% CI[0.50, 0.97]), indicating fair accuracy in predicting suicide reattempts, and resulted in fair sensitivity (60%) and positive predictive value (50%) and strong specificity (93%) and negative predictive value (95%).7 However, adolescents’ own prediction of their future SA did not distinguish reattempters from non-reattempters, t(43)=0.81, p=.422.
Finally, stimuli-specific exploratory analyses demonstrated that, compared to non-reattempters, reattempters had significantly higher (positive) D scores for “Die” (p=.022) and “Live” (p=.004) trials, indicating faster RT for these words when Death & Me/Life & Not Me were paired than during the reverse pairing (Table 3).
Discussion
This study extends prior research examining how implicit identification with death (using the Death IAT) may help detect and predict STBs. In cross-sectional analyses, the Death IAT exhibited small, but significant, associations with SI frequency, severity, and duration. Additionally, implicit identification with death was marginally stronger among adolescents with more recent and severe STBs (i.e., past-year suicide attempters). Exploratory analyses indicated that these group differences were driven by implicit identification on trials with the word “Suicide.” In prospective analyses, the Death IAT was related to any SI occurrence (but not to SI frequency), but not when controlling for past STBs. Notably, among adolescents with a prior SA, implicit identification with death was stronger for those who reattempted suicide over the follow-up compared to non-reattempters, particularly on trials with the words “Die” and “Live.” However, explicit prediction of future suicidal behavior did not distinguish these groups. Overall, the Death IAT exhibited good accuracy in predicting suicide reattempts over the follow-up period.
These findings partially replicate and extend prior research testing the Death IAT. Consistent with previous research in adults (Barnes et al., 2017; Chiurliza et al., 2016) and adolescents (Dickstein et al., 2015; Glenn, Kleiman, et al., 2017), we did not find robust overall differences on the Death IAT between lifetime attempters and non-attempters. However, we did find a trend for higher Death IAT scores among adolescents who had attempted suicide more recently (i.e., past year), similar to prior adult studies (Glenn, Werntz, et al., 2017; Nock et al., 2010).
Prospective analyses also partially replicate and extend prior work. Consistent with prior studies in adults (Ellis et al., 2016) and adolescents (Glenn, Kleiman, et al., 2017; Millner, Augenstein, et al., 2018), the Death IAT was modestly related to SI over the follow-up period, but not after controlling for baseline SI. Findings may have been weak, and somewhat inconsistent, due to the relative stability of SI between time points. A novel, but preliminary, finding from this study was the Death IAT’s prospective relation to suicidal behavior. Among prior attempters, adolescents who reattempted suicide over the follow-up exhibited stronger implicit identification with death at baseline. This effect was not accounted for by adolescents’ explicit prediction of their suicide risk, consistent with previous adult studies (Barnes et al., 2017; Nock et al., 2010; Randall et al., 2013). Taken together, this research suggests that implicit identification with death may be more useful for tracking state-like changes in suicide severity and recency than broadly distinguishing attempters from ideators.
Finally, this study extends prior Death IAT research by identifying specific stimuli that may drive the utility of this behavioral tool. For instance, identification on trials with “Suicide” (cross-sectional) and “Die” (prospective) were stronger than words like “Funeral.” These findings are in line with recent imaging research indicating that suicidal young adults exhibit more activation in self-referential brain regions when viewing words such as “death” and “lifeless” compared to nonsuicidal adults (Just et al., 2017). Although stimuli-level analyses predicting reattempts were exploratory, this study provides preliminary evidence that identification with certain death-related words (e.g., “Die”) may prospectively predict suicide risk in youth. Moreover, these results may be useful for constructing a briefer, and more robust, IAT for suicide risk detection (Millner, Coppersmith, et al., 2018).
There were several limitations of this study. Although a goal was to examine the Death IAT across the spectrum of STB severity and recency, some STB groups were small (e.g., lifetime ideators), which limited examination of diagnostic differences across groups. Additionally, there were few suicide reattempts over the follow-up, which limited statistical power for the prospective analyses (e.g., unable to examine the Death IAT’s prediction of attempts beyond known risk factors). Thus, these findings are preliminary and in need of replication in larger samples. Finally, the sample was primarily female and Caucasian; replication in more diverse sociodemographic groups is needed.
Despite these limitations, this study significantly extends prior research by demonstrating that the Death IAT may be useful for predicting STBs in youth outside of acute psychiatric treatment. An important future direction is to examine the prospective specificity of the Death IAT and Self-Injury IAT for predicting nonsuicidal and suicidal self-injury, which are likely to co-occur among clinical samples (Glenn, Kleiman, et al., 2017). Moreover, before the Death IAT can be disseminated to clinical settings, future studies need to test how this behavioral tool can be used most effectively in conjunction with other measures (across multiple methods and informants) to enhance suicide risk prediction. Specifically, it is important to determine how to integrate Death IAT scores with other, and potentially discrepant, information gathered in a suicide risk assessment (e.g., Death IAT indicates “high-risk” but patient denies any SI).
Supplementary Material
Acknowledgments
The research was partially supported by the National Institute of Mental Health (F32 MH097354 [CRG]) and with support from the John D. and Catherine T. MacArthur Foundation (MKN). The authors have no conflicts of interest to disclose.
The authors would like to thank Daniel Coppersmith, Amy Falk, Kristen Fuller, Jaclyn Kearns, Elizabeth Lanzillo, Angela Santee, and Suzie Shdo for their assistance collecting data for this project.
Footnotes
The “Death IAT” has previously been referred to as the “Death/Suicide IAT” (Nock et al., 2010). This IAT primarily includes words related to death (e.g., “Die”, “Deceased”) as well as the word “Suicide”. Since this first “Death/Suicide IAT” study by Nock et al. (2010), a suicide-specific version of the IAT has been created (the “Suicide IAT”), which includes words related to specific suicide methods (e.g., “Hanging”). For clarity and consistency with other recent publications (e.g., Glenn, Kleiman, et al., 2017; Glenn, Werntz, et al., 2017), we refer to the version of the IAT that includes words related to death and the word “Suicide” on some trials as the “Death IAT”.
Nock and Banaji (2007) examined how performance on a Self-Injury (cutting) IAT, but not the Death IAT, prospectively predicted STBs in adolescents. Cha, Augenstein, et al. (2016) utilized the Self-Injury IAT, but not the Death IAT, to predict nonsuicidal self-injury among adolescent psychiatric inpatients. Cha, Glenn, et al. (2016) examined iatrogenic effects of all self-harm IATs among adolescent psychiatric inpatients (and found only a small mood decline and minimal change in individuals’ desire for self-injury or death from pre- to post-IAT), but did not report group differences in performance on these IATs.
Excluded participants did not significantly differ from included participants in race (p=.656), ethnicity (p=.311), or family income (p=.282), but were significantly younger (M=15.29 years, SD=2.31; t[156]=5.03, p<.001), and had a greater proportion of male participants (47.1%; χ2[1, N=153]=11.26, p<.001).
We first compared the following mutually exclusive groups based on history of STB severity: no history of STBs (nonsuicidal psychiatric controls; n=35), lifetime suicide ideation but no planning or attempts (suicide ideators; n=25), lifetime suicide planning but no attempts (suicide planners; n=29), and lifetime suicide attempts (suicide attempters; n=52). Next, we examined the following mutually exclusive groups based on their history of STB severity and recency: nonsuicidal psychiatric controls (see above), lifetime suicide ideation but not in past year and no prior attempts (lifetime ideators; n=12), suicide ideation in past year but no prior attempts (past-year ideators; n=42), lifetime suicide attempt but no attempt in past year (lifetime attempters; n=30), and suicide attempt in past year (past-year attempters; n=22). (See Supplementary Material for this article.)
Most recent versions of the Death IAT include seven blocks, four of which are scored and the other three are practice blocks (Glenn, Werntz, et al., 2017). The current task is an older version (data collection began in 2012) that contains practice trials with unrelated concepts (bugs and flowers) and then two blocks with death-related concepts. For the current task, D scores were derived from 40 trials without any weighting procedure (as compared to more recent versions in which D scores are derived from 60 trials with the first 20 weighted equally to the last 40). See Nock et al. (2010) for additional Death IAT scoring details.
History of prior suicide attempts was not driving the group differences as suicide reattempters (M=1.0 [SD=0]) did not have a history of more suicide attempts at baseline compared to the non-reattempters (M=1.90 [SD=1.26]), t(39)=4.53, p<.001, d=1.01. Moreover, group differences in Death IAT scores were similar if we compared all six adolescents who attempted suicide over follow-up (IAT D score M=−.45 [SD=.35]) to the 40 adolescents who did not reattempt during follow-up (IAT D score M=.01 [SD=.35], t(44)=2.98, p=.005, d=1.31.
Adolescents’ explicit reports of suicidal thinking and prediction of future suicidal behavior (obtained during the baseline assessment) were poor classifiers of suicide reattempts over the 1-year follow-up period. For instance, when predicting suicide reattempts, SI frequency at baseline produced an AUC of 0.34 (95% CI[0.15–0.54]) and adolescents’ explicit prediction of future suicide attempts produced an AUC of 0.39 (95% CI[0.21–0.66]). Of note, both classifiers were in the opposite direction meaning that lower SI and lower prediction of suicidal behavior predicted suicide reattempts; even in the opposite direction, both were poor classifiers.
References
- Banse R, Seise J, & Zerbes N (2001). Implicit attitudes towards homosexuality: Reliability, validity, and controllability of the IAT. Zeitschrift für experimentelle Psychologie, 48(2), 145–160. [DOI] [PubMed] [Google Scholar]
- Barnes SM, Bahraini NH, Forster JE, Stearns-Yoder KA, Hostetter TA, Smith G, … Nock MK (2017). Moving beyond self-report: Implicit associations about death/life prospectively predict suicidal behavior among Veterans. Suicide and Life-Threatening Behavior, 47(1), 67–77. [DOI] [PubMed] [Google Scholar]
- Beck AT, & Steer RA (1991). Manual for the Beck scale for suicide ideation. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B(Methodological), 289–300. [Google Scholar]
- Busch KA, Fawcett J, & Jacobs DG (2003). Clinical correlates of inpatient suicide. Journal of Clinical Psychiatry, 64(1), 14–19. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2017b). Youth Risk Behavior Survey Questionnaire. Retrieved September 5, 2018 Available at: http://www.cdc.gov/yrbs
- Centers for Disease Control and Prevention (CDC). Web-based Injury Statistics Query and Reporting System (WISQARS). (2017a). National Center for Injury Prevention and Control, Center for Disease Control and Prevention. Available from http://www.cdc.gov/injury/wisqars/index.html
- Cha CB, Augenstein TM, Frost KH, Gallagher K, D’Angelo EJ, & Nock MK (2016). Using implicit and explicit measures to predict nonsuicidal self-injury among adolescent inpatients. Journal of the American Academy of Child & Adolescent Psychiatry, 55(1), 62–68. [DOI] [PubMed] [Google Scholar]
- Chan MKY, Bhatti H, Meader N, Stockton S, Evans J, Connor RC, … Kendall T (2016). Predicting suicide following self- harm: Systematic review of risk factors and risk scales. The British Journal of Psychiatry, 209, 277–283. [DOI] [PubMed] [Google Scholar]
- Chiurliza B, Hagan CR, Rogers ML, Podlogar MC, Hom MA, Stanley IH, & Joiner TE (2016). Implicit measures of suicide risk in a military sample. Assessment. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Goldston DB, & Costello EJ (2017). Adult associations of childhood suicidal thoughts and behaviors: a prospective, longitudinal analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 56(11), 958–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickstein DP, Puzia ME, Cushman GK, Weissman AB, Wegbreit E, Kim KL, … Spirito A (2015). Self-injurious implicit attitudes among adolescent suicide attempters versus those engaged in nonsuicidal self-injury. Journal of Child Psychology and Psychiatry, 56(10), 1127–1136. [DOI] [PubMed] [Google Scholar]
- Ellis TE, Rufino KA, & Green KL (2016). Implicit measure of life/death orientation predicts response of suicidal ideation to treatment in psychiatric inpatients. Archives of Suicide Research, 20(1), 59–68. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Kleiman EM, Coppersmith DDL, Santee AC, Esposito EC, Cha CB, … Auerbach RP (2017). Implicit identification with death predicts change in suicide ideation during psychiatric treatment in adolescents. Journal of Child Psychology and Psychiatry, 58(12), 1319–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn JJ, Werntz AJ, Slama SJ, Steinman SA, Teachman BA, & Nock MK (2017). Suicide and self-injury-related implicit cognition: A large-scale examination and replication. Journal of Abnormal Psychology, 126(2), 199–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, & Banaji MR (1995). Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychological Review, 102(1), 4–27. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, & Schwartz JL (1998). Measuring individual differences in implicit cognition: The implicit association test. Journal of Personality and Social Psychology, 74(6), 1464–1480. [DOI] [PubMed] [Google Scholar]
- Hilbe JM (2014). Modeling Count Data: Cambridge University Press. [Google Scholar]
- Just MA, Pan L, Cherkassky VL, McMakin DL, Cha C, Nock MK, & Brent DA (2017). Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nature Human Behaviour, 1(12), 911–919. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Karpinski A, & Hilton JL (2001). Attitudes and the Implicit Association Test. Journal of Personality and Social Psychology, 81(5), 774–788. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. [DOI] [PubMed] [Google Scholar]
- Miller AB, Eisenlohr-Moul T, Giletta M, Hastings PD, Rudolph KD, Nock MK, & Prinstein MJ (2017). A within-person approach to risk for suicidal ideation and suicidal behavior: Examining the roles of depression, stress, and abuse exposure. Journal of Consulting and Clinical Psychology, 85(7), 712–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millner AJ, Augenstein TM, Visser KH, Gallagher K, Vergara GA, D’Angelo EJ, & Nock MK (2018). Implicit cognitions as a behavioral marker of suicide attempts in adolescents. Archives of Suicide Research. [DOI] [PubMed] [Google Scholar]
- Millner AJ, Coppersmith DDL, Teachman BA, & Nock MK (2018). The Brief Death Implicit Association Test: Scoring recommendations, reliability, validity, and comparisons with the Death Implicit Association Test. Psychological Assessment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Action Alliance for Suicide Prevention (NAASP): Research Prioritization Task Force. (2014). A prioritized research agenda for suicide prevention: An action plan to save lives National Institute of Mental Health and the Research Prioritization Task Force. Rockville, MD. [Google Scholar]
- Nisbett RE, & Wilson TD (1977). Telling more than we can know: Verbal reports on mental processes. Psychological Review, 84(3), 231–259. [Google Scholar]
- Nock MK, & Banaji MR (2007). Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. Journal of Consulting and Clinical Psychology, 75(5), 707–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-injurious thoughts and behaviors interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19(3), 309–317. [DOI] [PubMed] [Google Scholar]
- Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, & Banaji MR (2010). Measuring the suicidal mind: Implicit cognition predicts suicidal behavior. Psychological Science, 21(4), 511–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall JR, Rowe BH, Dong KA, Nock MK, & Colman I (2013). Assessment of self-harm risk using implicit thoughts. Psychological Assessment, 25(3), 714–721. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, … Wilkinson B (2010). Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). Journal of Clinical Psychiatry, 71(3), 313–326. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Marker CD, & Smith-Janik SB (2008). Automatic associations and panic disorder: Trajectories of change over the course of treatment. Journal of Consulting and Clinical Psychology, 76(6), 988–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeileis A, Kleiber C, & Jackman S (2008). Regression models for count data in R. Journal of Statistical Software, 27(8), 1–25. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.