Abstract
Background:
More than 50% of lower limb prosthesis (LLP) users report falling at least once a year, placing them at high risk for adverse health outcomes like reduced mobility and diminished quality-of-life. Efforts to reduce falls among LLP users have traditionally focused on developing clinical tests to assess fall risk, designing prosthetic components to improve patient safety, and identifying risk factors to recognize potential fallers. Little attention has been directed towards recording, reporting, and characterizing the circumstances of falls among LLP users. Identifying the most common types of falls may help guide and prioritize clinical and research needs.
Objective:
To characterize the frequency and circumstances of falls reported by unilateral LLP users.
Design:
Secondary analysis of data from two cross-sectional studies.
Setting:
Outpatient clinic and research laboratory.
Participants:
Ambulatory unilateral transtibial and transfemoral LLP users (n=66).
Intervention:
None.
Main Outcome Measure(s):
A fall type classification framework was developed based on biomechanical theory and published falls terminology. Self-reported falls and accompanying narrative descriptions of LLP users’ falls in the previous 12 months were analyzed with the framework. Frequencies, estimated proportions, and estimated counts were compared across fall circumstances using 95% confidence intervals.
Results:
Thirty-eight participants (57.6%) reported 90 falls during the previous year. All reported falls were successfully categorized using the proposed framework. The majority of falls arose from disruptions to the base-of-support (BoS), intrinsic destabilizing factors, and a diverse set of fall patterns. Walking on level terrain was the most common activity at the time of a fall.
Conclusion:
This secondary analysis revealed that falls remain frequent among ambul4atory LLP users, and that clinicians and researchers may wish to prioritize falls owing to disruptions of BoS that occur while walking. Additional research with a larger sample is required to confirm and expand upon these results.
Level III Retrospective Study
Keywords: balance, accidental falls, amputee, artificial limb, rehabilitation
Introduction
More than 50% of lower limb prosthesis (LLP) users report falling at least once a year [1–5], placing them at a high risk for adverse health outcomes like reduced mobility and diminished quality of life [3,6,7]. Attempts to reduce the prevalence of falls among LLP users have traditionally focused on developing and validating clinical tests to assess fall risk[8–12], designing and testing prosthetic components to improve patient safety [13–16], characterizing the biomechanics of key balance strategies to identify deficits in those at risk for falls [17–23], and identifying risk factors to help recognize potential fallers [2,5,7,24,25]. However, little attention has been directed towards recording, reporting, and characterizing the circumstances surrounding falls among LLP users [1,4,7]. For example, are falls primarily due to external factors imposed by the environment, or initiated by internal physiological factors? Are LLP users more susceptible to trips, slips, or prosthetic failures? What activities are LLP users most commonly engaged in at the time of a fall? Answers to these questions may help direct treatment to the most prevalent and consequential types of falls [26–29], prioritize research needs in areas related to fall assessment (e.g., screening methods and diagnostic tests) [30], and generate evidence to develop and revise reimbursement policies (e.g., prosthetic components that reduce falls). The primary objective of this project was therefore to provide an initial characterization of the circumstances of falls among ambulatory unilateral LLP users.
The characterization of fall-related circumstances among LLP users is limited by the lack of a universal fall type classification framework and taxonomy suited to LLP users. The use of incomplete and study-specific terminology [1,4] has limited comparisons between studies, and prevented a more comprehensive characterization of fall circumstances among LLP users. Several classification frameworks have been used to characterize falls among older adults [26,31,32], but they are not entirely applicable to the experiences of LLP users [33]. A fall type classification framework for LLP users would provide a structured approach to soliciting, recording, reporting, and studying falls experienced by LLP users. A secondary objective of this project was therefore to propose and evaluate a LLP user-specific fall type classification framework and taxonomy.
Methods
Study Design
A secondary analysis of self-report falls data collected in two previous studies [11,12] was conducted to address the study objectives. Data were combined owing to similar study instruments, data collection methods, and participants. Both studies sought to evaluate the validity of clinical balance tests among ambulatory LLP users. No a-priori power analysis was performed for this secondary analysis. Original study protocols were reviewed and approved by institutional review boards at the XXXX and XXXX. All individuals provided written informed consent prior to participation.
Participants
Participants who met the following inclusion and exclusion criteria were selected from the datasets in both studies [11,12]: age greater than or equal to 18 years old; unilateral, transtibial or transfemoral amputation; greater than or equal to one year since amputation; and able to walk with or without an assistive device. Exclusion criteria included congenital or upper extremity limb loss, and comorbidities limiting mobility (e.g., knee replacement, severe pulmonary disease, ulcers).
Measurements
Participant demographics, prosthetic-related information, and retrospective falls data
Age, sex, amputation level, cause of amputation, and time since amputation were collected via interview with a study investigator. Study investigators also measured height and weight. To assess fall history, participants were each asked, “In the past 12 months have you had any falls including a slip or trip in which you inadvertently lost your balance and landed on the ground or lower level?” [34]. Participants reporting a fall were asked to provide a narrative description of the event (i.e., the circumstances surrounding their fall(s)) [29,31].
Development of the fall type classification framework and taxonomy
A fall type classification framework and taxonomy was developed based on biomechanical theory, published terminology, and fall descriptions reported by or observed among LLP users [1,4,33] and older adults [26,27,29,31,35–38]. Fall circumstances reported by older adults were referenced when developing the framework to supplement the limited reporting of fall circumstances in LLP users.
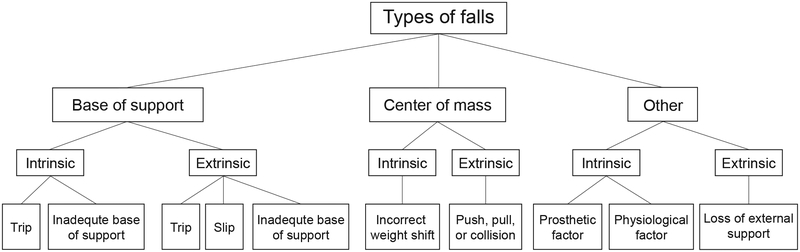
The fall type classification framework (Figure 1) is a three-level hierarchical system describing the location of the destabilizing force, the source of the destabilization, and the ensuing fall pattern. The first level of the framework characterizes the location of the destabilization with respect to the body. First-level descriptors are based on a simple biomechanical model wherein falling results from uncorrected disruptions between the base-of-support (BoS) and center-of-mass (CoM) [27,29,39–42]. Disruption may occur as a result of a destabilizing force acting to displace the BoS (i.e., feet) from beneath the CoM (i.e., a BoS fall), or displace the CoM (i.e., body) beyond its existing BoS (i.e., a CoM fall) [4,27,29,33,36]. Falls with no apparent biomechanical disruption between the BoS or the CoM are classified as “other” types of falls [27]. Characterizing the most common location of destabilizing forces leading to a fall may help determine the most suitable targets for mitigating fall risk through balance training, clinical balance assessment, and/or prosthetic design [1,28].
Figure 1.
Fall type classification framework. The proposed framework is a 3-level hierarchical system that characterizes falls based upon the location of the destabilizing force (level one), the source of the destabilizing force (level two), and the fall pattern (level three).
The second level of the framework characterizes the source of the destabilization. A destabilizing force that acts on the CoM or BoS can originate from intrinsic or extrinsic sources. Intrinsic sources are personal factors, often physiological in nature (e.g., muscle weakness). Extrinsic sources are external factors imposed by the environment that result in unexpected disruptions (e.g., icy walkway, being bumped by someone) [1,29,31,35,43]. Categorizing falls as intrinsic or extrinsic can guide clinical decision making in several ways. First, it can highlight potential preventative strategies. Falls attributed to extrinsic sources are often addressed via patient education and/or environmental modifications [44–46]. Falls attributed to intrinsic sources may require interventions that target specific neuromusculoskeletal deficits. Second, individuals who experience falls due to intrinsic sources are more likely to fall again because such sources often indicate systemic issues [47]. Thus, categorizing falls as intrinsic or extrinsic may help identify individuals who are likely to be recurrent fallers. Finally, contemporary clinical balance tests largely probe intrinsic over extrinsic factors. If the majority of falls experienced by LLP users are attributed to extrinsic sources of destabilization, clinically feasible tests that replicate such extrinsic sources of destabilization may need to be developed.
The final level of the framework describes fall patterns [1,20,28]. For example, a destabilizing force acting on the BoS from an extrinsic source can produce a fall due to a trip, a slip, or an inadequate BoS [26]. This level of the framework also includes prosthetic-related factors (e.g., prosthetic knee buckling) [1], physiological factors (e.g., collapse due to muscle weakness), and loss of external support (e.g., support structure or assistive device moving unexpectedly) [26,31]. Characterizing fall patterns may be important for selecting treatment and preventative strategies with a level of specificity that is needed for balance training, yet beyond what is offered by the first two levels of the framework [28,48–51]. If certain fall patterns are more prevalent resources should be directed towards their investigation. Inclusion of fall patterns within the framework also introduces terminology consistent with that used by clinicians and patients. A complete set of definitions and examples for each component of the fall type classification framework is provided in Appendix 1.
Classifying falls
Two reviewers independently classified each reported fall using the fall type framework. Participants’ narrative descriptions of fall events were first analyzed to determine whether the BoS or CoM was disrupted (level one). If participants described neither, the fall was assigned to “other”. Each type of level one fall was further characterized based on whether participants described extrinsic (i.e., environmental) or intrinsic (i.e., personal) factors as the source of the destabilization (level two). If both intrinsic and extrinsic factors were reported, the source was categorized as intrinsic [31]. Falls were subsequently classified with greater detail based on reported movements during the fall (level three). For example, if a participant reported that he or she caught their foot on crack in the sidewalk and fell forward, the fall was classified as a BoS extrinsic trip.
In addition to fall type, activity at the time of the fall was also categorized. The same two reviewers extracted details regarding the specific form of activity at the time of the fall from the narrative description provided by each participant. Previously reported activities at the time of a fall (e.g., walking, transfer, reaching) [7,26,33,36] were used as an initial guideline for categorization. Falls were classified as “unknown” when participants were unable to recall the events surrounding the fall.
Statistical Analysis
For each fall type and activity at the time of a fall, we tabulated the total number of reported falls (i.e., frequency), the proportion of participants falling at least once (i.e., estimated proportion), and the average number of falls per participant (i.e., estimated count). Frequencies were expressed as both a number and percentage of all reported falls. Estimated proportions were calculated as the ratio of participants who reported at least one fall for each type or activity with respect to all participants, multiplied by 100. Estimated counts were calculated as the ratio of all falls reported for each type or activity with respect to the total number of participants. To determine whether there were any differences in the estimated proportions or counts across the various types of falls and activities at the time of a fall, 95% confidence intervals (CI) were computed from a t-distribution and compared across fall types and activities. Overlap between 95% CI was taken as a conservative estimate of no significant difference. All statistical analyses were performed using SPSS v.24 (Chicago, IL).
We also sought to ascertain the ability of the proposed fall type classification framework to accurately capture the range of fall types reported by LLP users. To that end, following classification, the framework was reviewed for: i) categories that did not align with any reported fall events, which would suggest they may be unnecessary and could be removed, and ii) falls that did not fit into the framework, which would suggest that additional categories may be required.
Results
Participants
Records of seventy LLP users who participated in the original studies [11,12] were reviewed. Three participants were excluded due to amputation level (two bilateral; one ankle disarticulation), while data from a fourth participant was excluded because time since amputation was less than one year. Data from sixty-six participants were included (Table 1).
Table 1.
Sociodemographic and amputation-related characteristics
| Age (years) | Height (cm) | Weight (kg) | Time since amputation (years) | Sex | Amputation level | Amputation etiology | |
|---|---|---|---|---|---|---|---|
| Mean | 50.6 | 173 | 81.6 | 16.3 | 37 male | 36 transtibial | 39 trauma |
| SD | 14.1 | 8.65 | 16.9 | 13.0 | 29 female | 30 transfemoral | 13 dysvascular |
| 5 cancer | |||||||
| Range | 21–76 | 155–189 | 104–266 | 1.6 – 57 | 7 infections | ||
| 2 congenital |
SD = standard deviation
Fall Prevalence
Sixty-six participants reported a total of ninety falls (i.e., 1.36 falls per participant). Thirty-eight participants (57.6%) reported one or more falls in the past 12 months. Fourteen participants (22.1%) reported one fall, nine (13.6%) reported two falls, and fifteen (22.7%) reported three or more falls in the past 12 months. Based on the narrative description provided by the participants’ of their fall(s) and activities at the time of the falls, all reported falls were considered to have occurred while wearing a prosthesis.
Suitability of the fall type classification framework
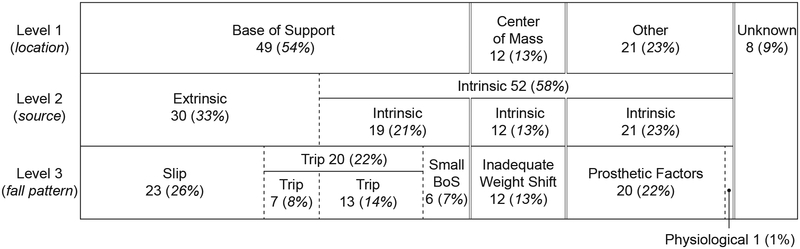
Eight falls (9%) were categorized as “unknown” (Figure 2), seven due to incomplete data collection forms, and one owing to a participant’s inability to recall the specific circumstances of a fall. Three framework categories did not align with at least one reported fall event: “a loss of external support”, “push, pull, or collision”, and “inadequate base-of-support”.
Figure 2.
Number and frequency of fall types among lower limb prosthesis users as categorized by the classification framework. The base-of-support was the most common location of a destabilizing force resulting in a fall (level one). Intrinsic factors were the most common source of a destabilizing force resulting in a fall (level two). Slip, trips, and prosthetic factors accounted for nearly three-quarters of the reported fall patterns (level three).
Base-of-support versus center-of-mass falls
The BoS was the most commonly reported location of a destabilizing force leading to a fall, accounting for 54% (49 of 90) of all reported falls (Figure 2). The proportion of participants (36.4%, 95% CI: 26.4–48.4) and the average number of falls per participant (.75, 95% CI: .63-.85) due to a disruption of the BoS were both significantly greater than those arising from a disruption of the CoM (proportion: 9.1%, 95% CI: 1.9–16.3; average number/participant: .18, 95% CI: .09-.28) or those with no apparent disruption to the BoS or the CoM (i.e., “other”) (proportion: 16.7%, 95% CI: 7.4–26.0; average number/participant: .32, 95% CI: .20-.43) (Table 2).
Table 2.
Proportion of participants who fell at least once, and average number of falls per participant due to various types of falls*
| Proportion of participants who fell | Number of falls per participant | ||||
|---|---|---|---|---|---|
| Estimated Proportion % (SE) | 95% CI | Estimated count n (SE) | 95% CI | ||
| Location of destabilizing force | |||||
| Base of support | 36.4% | (5.9) | 26.4–48.4 | .75 (.05) | .63-.85 |
| Center of mass | 9.1% | (3.5) | 1.9–16.3 | .18 (.05) | .09-.28 |
| Other | 16.7% | (4.6) | 7.4–26.0 | .32 (.06) | .20-.43 |
| Source of destabilizing force | |||||
| Extrinsic | 27.3% | (5.5) | 16.2–38.4 | .46 (.06) | .33-.58 |
| Intrinsic | 39.4% | (6.0) | 27.2–51.6 | .78 (.05) | .69-.89 |
| Fall pattern | |||||
| Slip | 18.2% | (4.7) | 8.6–27.8 | .35 (.06) | .23-.47 |
| Trip | 16.7% | (4.6) | 7.4–26.0 | .30 (.06) | .19-.42 |
| Inadequate weight shift | 9.1% | (3.5) | 1.9–16.3 | .18 (.05) | .09-.28 |
| Inadequate base of support | 7.6% | (3.3) | 0–14.2 | .09 (.04) | 0-.16 |
| Prosthetic factors | 15.2% | (4.4) | 6.2–24.1 | .30 (.06) | .19-.42 |
| Physiological factors | 1.5% | (1.5) | 0–4.6 | .02 (.02) | 0-.05 |
| Unknown | 10.6% | (3.8) | 2.9–18.3 | .12 (.04) | .04-.20 |
Estimated proportions and counts may not sum across fall types to 100% or 1.0 respectively because participants can belong to more than one fall type if they reported multiple falls.
Intrinsic versus extrinsic falls
Intrinsic (i.e. personal) factors were the most commonly reported source of destabilizing forces leading to a fall (Figure 2). Fifty-two of the ninety reported falls (58%) were attributed to intrinsic sources (e.g., missed step, poor foot clearance), while 30 of the reported falls (33%) were attributed to extrinsic sources (e.g., icy surface, cracked sidewalk, uneven terrain) (Figure 2). However, neither the proportion of participants reporting a fall nor the average number of falls per participant were significantly different between intrinsic and extrinsic sources (Table 2).
Fall patterns
Slips were the most commonly reported fall pattern, accounting for 23 of the 90 reported falls (26%). This was followed by trips and prosthetic factors, each accounting for 22% of all reported falls (Figure 2). The proportion of participants reporting slips (18.2%, 95% CI: 8.6–27.8) and trips (16.7%, 95%CI: 7.4–26.0), as well as the average number of slips (.35, 95% CI: .23-.47) and trips (.30, 95% CI: .19-.42) per participant were significantly greater than the proportion of participants reporting falls due to physiological factors (1.5%, 95% CI: 0–4.6) and the number of falls per participant due to physiological factors (.02, 95% CI: 0-.05) or an inadequate BoS (.09, 95% CI: 0-.16). No other significant differences in the proportion of participants falling or number of falls per participant were identified across fall patterns (Table 2).
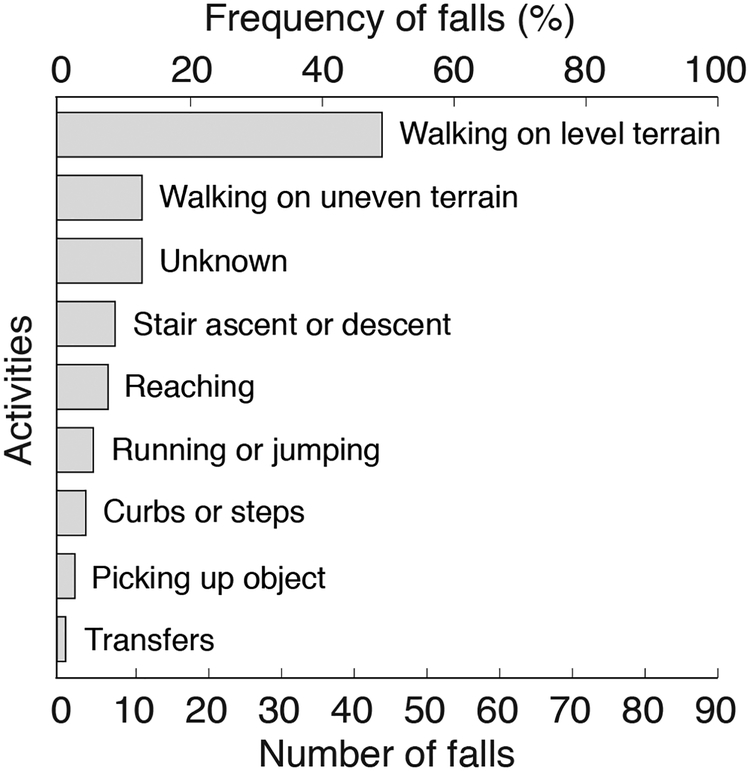
Activities performed at the time of a fall
Participants most commonly reported walking on level terrain when they experienced a fall. Falls that occurred while participants were walking on level terrain accounted for 45.6% (41 of 90) of all falls (Figure 3). The proportion of participants who reported falling while walking on level terrain (31.8%, 95% CI: 20.2–43.4), and the mean number of falls while walking per participant (.62, 95% CI: .50-.74) were both significantly greater than falls that occurred while participants’ were engaged in any other reported activity (e.g., walking on uneven terrain, stairs, transfers) (Table 3). There were thirteen (14%) falls that occurred during an “unknown” activity (Figure 3).
Figure 3.
Number and frequency of falls reported by lower limb prosthesis users based upon the activity at the time of a fall. Walking was the most commonly reported activity at the time of a fall. More falls occurred while walking on level versus uneven terrain.
Table 3.
Proportion of participants who fell at least once, and average number of falls per participant for activities reported at the time of a fall*
| Proportion of participants who fell | Number of falls per participant | |||
|---|---|---|---|---|
| Estimated Proportion % (SE) | 95% CI | Estimated count n (SE) | 95% CI | |
| Walking level terrain | 31.8% (5.7) | 20.2–43.4 | .62 (.06) | .50-.74 |
| Unknown | 12.1% (4.0) | 4.0–20.3 | .20 (.05) | .10-.30 |
| Stairs | 10.6% (3.8) | 2.9–18.3 | .11 (.04) | .03.18 |
| Walking uneven terrain | 9.1% (3.5) | 1.9–16.3 | .20 (.05) | .10-.30 |
| Running or jumping | 6.1% (2.9) | .1–12.0 | .06 (.03) | 0-.12 |
| Reaching | 6.1% (2.9) | 0–12.0 | .09 (.04) | .02-.16 |
| Curbs or steps | 3.0% (2.1) | 0–7.3 | .05 (.03) | 0-.10 |
| Picking up object | 1.5% (1.5) | 0–4.6 | .03 (.02) | 0-.07 |
| Transfers | 1.5% (1.5) | 0–4.6 | .02 (.02) | 0-.05 |
Estimated proportions and counts may not sum across activities to 100% of 1.0 respectively because participants can belong to more than one group if they reported multiple falls.
Discussion
This secondary analysis was conducted to provide an initial characterization of the circumstances of falls among ambulatory unilateral LLP users, and propose a fall type classification framework. The prevalence of falls among this sample of LLP users exceeded 50%. The majority of these falls arose from disruptions to the base-of-support, intrinsic destabilizing factors, and a diverse set of fall patterns (e.g., slips, trips, inadequate weight shift). While additional work is necessary to confirm and expand upon these results in a larger sample, the present findings represent an important first step in developing specific targets for clinical assessment and treatment, as wellas future research directions.
The proposed classification framework successfully categorized fall types reported by LLP users.
The proposed framework offers three advantages. First, both reviewers independently arrived at and agreed upon the fall categorizations, suggesting that the framework and accompanying taxonomy are reliable. Second, the taxonomy appears comprehensive. All reported falls were successfully categorized. Only eight (9%) of the reported falls were categorized as “unknown”, well below 19% among older adults [52]. Three fall patterns, “push, pull, or collision”, “loss of external support”, and “inadequate base-of-support” were not utilized. These fall patterns have been previously reported by LLP users [4] and older adults [26], as such their removal from the framework is not recommended until they can be assessed in a larger sample.
Falls remain frequent among LLP users.
Historically, over 50% of LLP users report falling at least once a year [1,2,4,5,25]. The results of this secondary analysis revealed that the prevalence of falls among community-living ambulatory LLP users remains high, at 57.6%. The prevalence of recurrent falls, 36.3%, also remains at or above historically reported values for LLP users (i.e., 23.4%−39.0%) [1,3,5]. The relevance of the elevated frequency of falls among LLP users should be judged not on its magnitude alone, but also on the severity and occurrence of adverse outcomes. Between 8.0% and 57.0% of LLP users report a fall-related injury [1,4,7,25,53], while 14.6% seek medical attention, and 7.3% require surgery [53] after a fall. Coupled with the importance LLP users place on balance [54], these consequences indicate that falls negatively impact the lives of a substantial portion of LLP users Research exploring new approaches guided by the types of falls experienced by LLP users may be needed to reduce falls in LLP.
LLP users are more susceptible to base-of-support than center-of-mass falls.
Base-of-support (BoS) falls are more common than center-of-mass (CoM) falls among LLP users. These findings are consistent with those among older adults without lower limb amputation, where BoS falls consistently outnumber CoM falls [27,31,36–38]. Environmental barriers and/or limitations in modern prosthetic components may contribute to the prevalence of BoS falls among LLP users. Environmental hazards that disrupt the BoS (e.g., cracks in the sidewalk) may be more common than those that disrupt the CoM (e.g., collisions in crowds). The lack of active ankle dorsiflexion in most contemporary prosthetic feet may limit the functional shortening of the prosthetic leg required during swing phase to achieve sufficient toe clearance, increasing the likelihood of a BoS disruption (i.e., trip) [13]. Minimum toe clearance of the prosthetic leg during swing phase is 50% lower among transtibial LLP users with a history of trip-related (i.e., BoS) falls than without [33]. LLP users may also be susceptible to BoS falls because of limited or ineffective responses to BoS disruptions. For example, when the prosthetic leg is obstructed during a trip, transfemoral LLP users only select the “lowering” strategy, ignoring the “elevating” strategy, even when the “elevating” strategy is more suitable [20]. Additionally, the “lowering” strategy is often unsuccessful in transfemoral prosthesis users due to excessive stance phase flexion (i.e., buckling) of the prosthetic knee [20,55]. New prosthetic designs with active powered control may therefore be necessary for LLP users to successfully utilize the full range of available balance response strategies [17]. Clinical balance tests that probe responses to BoS disruptions [27] may be needed to improve fall risk assessment among LLP users [30].
The prevalence of intrinsic falls among LLP users may explain the high rate of recurrent falls.
Consistent with prior research [1], the results of this secondary analysis confirmed that ambulatory LLP users experience more falls initiated by intrinsic personal factors than imposed by extrinsic environmental factors. A higher proportion of intrinsic falls are typically associated with advanced age (i.e., greater than 75 years old) [31,43,45,56]. However, the relatively low mean age of our sample, 50.4 years, suggests that the intrinsic falls are unlikely to be attributable to age. Instead, challenges and demands unique to prosthetic ambulation, such as controlling a prosthetic knee (i.e., “prosthetic factors”), and a reduction in strength [3,28,57] are more likely to be responsible for intrinsic falls. The prevalence of intrinsic falls, which are associated with systemic issues and multiple falls [47], may explain the high rate of recurrent falls (36.3%) that were observed in this analysis. Additionally, by placing greater emphasis and quickly identifying and treating intrinsic factors related to fall risk, clinicians may be able to reduce recurrent falls among LLP users. While both modifiable (e.g., pain, general health, mobility, strength) [3,53,57] as well as non-modifiable (e.g., level of amputation, cause of amputation, increasing age, altered somatosensation, and sex) [3,53,57] intrinsic personal factors have been associated with increased fall risk, a history of falls, and fall related injuries among LLP users, other important and modifiable intrinsic factors including prosthetic design, and reaction time [21,58] remain unexamined. How intrinsic factors change across the stages of recovery [59], and their synthesis into a clinical test for predicting susceptibility to intrinsic falls may improve fall risk assessment. A full characterization of intrinsic personal factors, and their association with falls among LLP users is warranted [60].
LLP users reported a variety of fall patterns.
Nearly three-quarters of the falls reported by LLP users were categorized as slips (26%), trips (22%), or prosthetic factors (22%). The prevalence of slips and trips corroborates the findings of Rosenblatt et al., (2016) who reported that among a small sample of transtibial LLP users, a quarter of the falls were trips and a quarter were slips. Kulkarni et al., (1996) reported that 12% of the falls in their sample of LLP users were attributed to prosthetic-related factors, about half of what our analysis revealed. These prosthetic-related falls in the prior study included “prosthetic failures” (e.g., foot breaking), and “prostheses not working as expected”. This suggests that LLP users may be attempting activities that their prostheses don’t well allow them to do, and that new components may increase patient safety. These results also expand upon the diversity of fall patterns previously identified. While previously reported among older adults [26,27], incorrect weight shifts and a small base of support, which accounted for 20% of all reported falls, had not previously been described among LLP users. Owing to this variety, neither assessment nor treatment of falls among LLP users can currently be prioritized based on the prevalence of a specific fall pattern.
Walking was the most common activity at the time of a fall.
Participants in this study were generally engaged in some form of locomotion, mainly on level terrain, at the time of a fall. This is consistent with a previous study of a small sample transtibial LLP users where most falls and stumbles occurred while walking, 83% of which were on level ground [33]. The prevalence of falls while walking is likely attributable to the prominence of walking in our lives, and the inherently unstable biomechanics of walking [61]. Falls in LLP users may be more common on level terrain due to opportunity (i.e., there is more level than uneven terrain), avoiding uneven terrain, or gait modifications made to preserve “stability” on uneven terrain. While challenging [62], when walking on uneven terrain LLP users adopt a cautious, conservative gait pattern (i.e., reduce speed, wider base of support, increased double support time, lowered center-of-mass, and increased upper extremity motion) [22,63–66]. While potentially imposing additional costs or demands (i.e., metabolic), these changes appear to mitigate additional risk associated with walking over uneven terrain [22,66].
Limitations
LLP users were asked to recall fall events over the past 12 months (i.e., self-report). This may have introduced recall bias, and led to an underestimation of the prevalence of falls [67,68]. There is currently no consensus regarding recall period when asking LLP users about falls. Additionally, commonly adopted definitions of a fall [1,3,5] do not contain prosthetic specific language (e.g., “a fall with or without your prosthesis”). Similar to guidelines proposed for older adults [69], future research may benefit from establishing the time window over which LLP users can accurately recall fall events and their related details, as well as a fall definition that is meaningful to LLP users.
The current analysis is limited by our understanding of the situation in which falls occurred, as well as the role if any of prosthetic componentry on fall type. For example, the mental (e.g., distraction, urgency) or physical state (e.g., fatigue) of LLP users at the time of a fall remains unknown. Additional research characterizing these situations may clarify why falls while walking on level terrain were prevalent. Future research would benefit from a clearer separation of activity and physical environment, as well as additional details characterizing the physical environment at the time of a fall (e.g., lighting, time of day, indoors/outdoor). Likewise, the role of prosthetic componentry in contributing to or reducing certain fall types remains to be determined. A comprehensive analysis of the physical, social, economic, and psychological consequences of falls among LLP users is needed to better determine the impact of falls among LLP users. Characterizing fall consequences may also provide a more robust approach to prioritizing clinical and research directions with respect to specific fall patterns.
Conclusion
The primary objective of this secondary analysis was to provide an initial characterization of the circumstances surrounding falls among ambulatory unilateral LLP users. The results of this secondary analysis suggest that falls remain frequent among ambulatory LLP users, and that clinicians and researchers may wish to prioritize falls owing to disruptions of BoS that occur while walking. The secondary objective was to propose and evaluate a LLP user-specific fall type classification framework and taxonomy. The proposed fall type classification framework successfully classified all self-reported falls, suggesting that it is comprehensive. Future falls research among LLP users may wish to use a similar taxonomy and framework. With the frequency of falls remaining above 50%, and the rate of amputation expected to rise [70], falls among LLP user are likely to be a substantial burden on the U.S. health care system. An understanding of the circumstances and consequences associated with falls may lead to previously unidentified targets for assessing and treating fall risk.
Acknowledgments
Funding Support:
Research reported in this publication was supported by the Department of Defense (DoD) under award number W81XWH-17-1-0547 (JK, BH, AS), the National Institutes of Health (NIH) under award number K12HD073945 (AS), the Orthotics and Prosthetics Education and Research Foundation, Inc. (OPERF) under grant number OPERF-SGA-2016–1 (AS, BH), and the US Department of Veterans Affairs under award number IK2 RX001322 (MM). The content is solely the responsibility of the authors and does not necessarily represent the official views of the DoD, NIH, OPERF, or the VA.
Abbreviations:
- BoS
base of support
- CI
confidence interval
- CoM
center of mass
- LLP
lower limb prosthesis
- TF
transfemoral
- TT
transtibial
Definition of fall related terms
Fall: an unplanned, unexpected, or unintentional event that occurred during standing, walking or changing posture and resulted in the contact of a body part, other than the feet, coming to rest on the ground or a lower level, other than as a consequence of a loss of consciousness, violent blow, stroke, or epileptic seizure [34,1,68].
Intrinsic cause: precipitating factors initiating a fall that are attributed to the individual [29,31] (e.g. muscle weakness).
Extrinsic cause: precipitating factors initiating a fall that are attributed to the environment [29,31] (e.g. icy driveway, uneven terrain).
Note: if both intrinsic and extrinsic causes are involved in the precipitating incident leading to a fall, the primary cause will be interpreted as intrinsic (e.g. tripping over an object due to poor muscle weakness that limited ability to adequately lift the leg [31]).
Base-of-support fall: fall initiated by a perturbation (i.e. force) applied to the base-of-support that prevents the base-of-support from remaining beneath the center of mass [27].
Intrinsic base-of-support falls
Trip/stumble: fall initiated by obstructing the trajectory of one’s foot or leg on an unchanging or unobstructed surface, an assistive device, or one’s own body [26–27] (e.g. walking on level surface but catching toe because of inadequate foot clearance).
Inadequate base-of-support: fall initiated by an error in foot placement that results in a step or stance width that is too small or provides insufficient contact with the support surface (e.g. foot is in partial contact with a stair/step, or foot placement reduces step width or length).
Extrinsic base-of-support falls
Trip/stumble: fall initiated by catching foot or leg on uneven surface, obstacle, step, or terrain transition [26–27] (e.g. catching toe on a crack in the sidewalk).
Slip: fall initiated by inadequate friction between the foot and the ground arising from environmental conditions [26–27] (e.g. slipping on an icy sidewalk).
Inadequate base-of-support: fall initiated by surface that is too small and/or provides inadequate contact beneath the foot (e.g. losing balance on a narrow step stool).
Center-of-mass fall: fall initiated by a perturbation (i.e. force) applied to the center of mass/trunk that acts to displace the center of mass beyond the existing base of support [27].
Intrinsic center-of-mass falls
Incorrect weight shift: fall due to self-induced shifting of body weight beyond the base-of-support [26] (e.g. reaching, turning, transfers).
Extrinsic center-of-mass falls
Push: fall initiated by the application of a force directed towards the center-of-mass by another person or object (e.g. being pushed by someone while standing still).
Pull: fall initiated by the application of a force directed away from the center-of-mass by another person or object (e.g. being pulled by someone when rising from a chair).
Collision: fall initiated by an impact with someone or something while moving (e.g. bumping into someone while walking in a crowded street). Note: Bump will be included in this definition
Other types of falls
Intrinsic
Prosthetic factors: fall initiated by prosthetic behavior that does not align with user intent or expectations, as well as any component of the prosthesis that mal-functions, breaks, fits poorly, or is misaligned [1] (e.g. prosthetic knee buckling).
Physiological: fall in the absence of a physical perturbation, caused by a transient physiological event [26–27,31] (e.g. syncope, seizure, or a sudden loss of muscle tone or head movement, vertigo).
Extrinsic
Loss of external support: fall initiated by a support structure moving unexpectedly [26,31](e.g. chair moves unexpectedly during sit-to-stand).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Publisher's Disclaimer: Prior Publication:
The work described in this manuscript has not been previously published or presented, nor is it under consideration for publication elsewhere.
Financial Disclosure:
The authors declare no competing interest.
Institutional Review:
All study procedures were reviewed and approved by Institutional Review Boards (IRBs) at the University of xref.
References
- 1.Kulkarni J, Wright S, Toole C, Morris J, Hirons R. Falls in patients with lower limb amputations: prevalence and contributing factors. Physiotherapy. 1996;82:130–6. [Google Scholar]
- 2.Gauthier-Gagnon C, Grisé MC, Potvin D. Enabling factors related to prosthetic use by people with transtibial and transfemoral amputation. Arch of Phys Med Rehabil. 1999;80:706–13. [DOI] [PubMed] [Google Scholar]
- 3.Miller WC, Speechley M, Deathe B. The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Arch of Phys Med Rehabil. 2001;82:1031–7. [DOI] [PubMed] [Google Scholar]
- 4.Ülger Ö, Topuz S, Bayramlar K, Erbahçeci F, Sener G. Risk factors, frequency, and causes of falling in geriatric persons who has had a limb removed by amputation. Top Geriatr Rehabil. 2010;26:156–63. [Google Scholar]
- 5.Wong CK, Chen CC, Blackwell WM, Rahal RT, Benoy SA. Balance ability measured with the Berg balance scale: a determinant of fall history in community-dwelling adults with leg amputation. J Rehabil Med. 2015;47:80–6. [DOI] [PubMed] [Google Scholar]
- 6.McWhinnie DL, Gordon AC, Collin J. Rehabilitation outcome 5 years after 100 lower-limb amputations. Br J of Surg. 1994;1596–9. [DOI] [PubMed] [Google Scholar]
- 7.Pauley T, Devlin M, Heslin K. Falls sustained during inpatient rehabilitation after lower limb amputation: prevalence and predictors. Am J Phys Med Rehabil. 2006;85:521–32. [DOI] [PubMed] [Google Scholar]
- 8.Schoppen T, Boonstra A, Groothoff JW, de Vries J, Goeken L, Eisma WH. The Timed “Up and Go” test: reliability and validity in persons with unilateral lower limb amputation. Arch of Phys Med Rehabil. 1999;80:825–8. [DOI] [PubMed] [Google Scholar]
- 9.Miller WC, Deathe AB, Speechley M. Psychometric properties of the Activities-specific Balance Confidence scale among individuals with a lower-limb amputation. Arch of Phys Med Rehabil. 2003;84:656–61. [DOI] [PubMed] [Google Scholar]
- 10.Dite W, Connor HJ, Curtis HC. Clinical identification of multiple fall risk early after unilateral transtibial amputation. Arch of Phys Med Rehabil. 2007;88:109–14. [DOI] [PubMed] [Google Scholar]
- 11.Major MJ, Fatone S, Roth EJ. Validity and reliability of the Berg Balance Scale for community-dwelling persons with lower-limb amputation. Arch of Phys Med Rehabil. 2013;94:2194–202. [DOI] [PubMed] [Google Scholar]
- 12.Sawers A, Hafner BJ. A study to assess whether fixed-width beam walking provides sufficient challenge to assess balance ability across lower limb prosthesis users. Clin Rehabil. 2018;32:483–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenblatt NJ, Bauer A, CPO, Rotter D, CPO, Grabiner MD. Active dorsiflexing prostheses may reduce trip-related fall risk in people with transtibial amputation. JRRD. 2014;51:1229–42. [DOI] [PubMed] [Google Scholar]
- 14.Hafner BJ, Willingham LL, Buell NC, Allyn KJ, Smith DG. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch of Phys Med Rehabil. 2007;88:207–17. [DOI] [PubMed] [Google Scholar]
- 15.Hafner BJ, Smith DG. Differences in function and safety between Medicare Functional Classification Level-2 and −3 transfemoral amputees and influence of prosthetic knee joint control. JRRD. 2009;46:417–34. [PubMed] [Google Scholar]
- 16.Kahle JT, Highsmith MJ, Hubbard SL. Comparison of nonmicroprocessor knee mechanism versus C-Leg on Prosthesis Evaluation Questionnaire, stumbles, falls, walking tests, stair descent, and knee preference. JRRD. 2008;45:1–14. [DOI] [PubMed] [Google Scholar]
- 17.Shirota C, Simon AM, Kuiken TA. Transfemoral amputee recovery strategies following trips to their sound and prosthesis sides throughout swing phase. J NeuroEng Rehabil. 2015:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Segal AD, Klute GK. Lower-limb amputee recovery response to an imposed error in mediolateral foot placement. J Biomech. 2014;47:2911–8. [DOI] [PubMed] [Google Scholar]
- 19.Bolger D, Ting LH, Sawers A. Individuals with transtibial limb loss use interlimb force asymmetries to maintain multi-directional reactive balance control. Clin Biomech 2014;29:1039–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crenshaw JR, Kaufman KR, Grabiner MD. Trip recoveries of people with unilateral, transfemoral or knee disarticulation amputations: Initial findings. Gait Posture. 2013;38:534–6. [DOI] [PubMed] [Google Scholar]
- 21.Curtze C, Hof AL, Otten B, Postema K. Balance recovery after an evoked forward fall in unilateral transtibial amputees. Gait Posture. 2010;32:336–41. [DOI] [PubMed] [Google Scholar]
- 22.Curtze C, Hof AL, Postema K, Otten B. The relative contributions of the prosthetic and sound limb to balance control in unilateral transtibial amputees. Gait Posture. 2012;36:276–81. [DOI] [PubMed] [Google Scholar]
- 23.Yang J, Jin D, Ji L, Wang R, Zhang J, Fang X, et al. The reaction strategy of lower extremity muscles when slips occur to individuals with trans-femoral amputation. J Electromyogr Kinesiol. 2007;17:228–40. [DOI] [PubMed] [Google Scholar]
- 24.Vanicek N, Strike S, McNaughton L, Polman R. Gait patterns in transtibial amputee fallers vs. non-fallers: Biomechanical differences during level walking. Gait Posture. 2009;29:415–20. [DOI] [PubMed] [Google Scholar]
- 25.Miller WC, Deathe AB, Speechley M, Koval J. The influence of falling, fear of falling, and balance confidence on prosthetic mobility and social activity among individuals with a lower extremity amputation. Arch of Phys Med Rehabil. 2001;82:1238–44. [DOI] [PubMed] [Google Scholar]
- 26.Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, et al. Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. The Lancet. 2013;381:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Topper AK, Maki BE, Holliday PJ. Are activity-based assessments of balance and gait in the elderly predictive of risk of falling and/or type of fall? J Am Geriatr Soc. 1993;41:479–87. [DOI] [PubMed] [Google Scholar]
- 28.Vlahov D, Myers AH, Al-ibrahim MS. Epidemiology of falls among patients in a rehabilitation hospital. Arch of Phys Med Rehabil. 1990:8–12. [PubMed] [Google Scholar]
- 29.Wild D, Nayak US, Isaacs B. Description, classification and prevention of falls in old people at home. Rheumatol Rehabil. 1981;20:153–9. [DOI] [PubMed] [Google Scholar]
- 30.Hart-Hughes S, Latlief GA, Phillips S, Groer S, Highsmith MJ. A review of clinical outcome assessment instruments for gait, balance, and fall risk in persons with lower extremity amputation. Top Geriatr Rehabil. 2014;30:70–6. [Google Scholar]
- 31.Lach HW, Reed AT, Arfken CL, Miller JP, Paige GD, Birge SJ, et al. Falls in the elderly: reliability of a classification system. J Am Geriatr Soc. 1991;39:197–202. [DOI] [PubMed] [Google Scholar]
- 32.Bleijlevens MHC, Diederiks JPM, Hendriks MRC, van Haastregt JCM, Crebolder HFJM, van Eijk JTM. Relationship between location and activity in injurious falls: an exploratory study. BMC Geriatr. 2010;10:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rosenblatt NJ, Bauer A, Grabiner MD. Relating minimum toe clearance to prospective, self-reported, trip-related stumbles in the community. Prosthet Orthot Int. 2016;41:387–92. [DOI] [PubMed] [Google Scholar]
- 34.Askham J, Glucksman E, Owens P, Swift C, Tinker A, Yu G. Home and leisure accident research: a review of research on falls among elderly people. London, UK: Age Concern Institute of Gerontology, King’s College London, and Department of Trade and Industry; 1990. [Google Scholar]
- 35.Haga H, Shibata H, Shichita K, Matsuzaki T, Hatano S. Falls in the institutionalized elderly in Japan. Arch Gerontol Geriatr. 1986;5:1–9. [DOI] [PubMed] [Google Scholar]
- 36.Berg WP, Alessio HM, Mills EM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing. 1997;26:261–8. [DOI] [PubMed] [Google Scholar]
- 37.Hill K, Schwarz J, Flicker L, Carroll S. Falls among healthy, community-dwelling, older women: a prospective study of frequency, circumstances, consequences and prediction accuracy. Aust N Z J Public Health. 1999;23:41–8. [DOI] [PubMed] [Google Scholar]
- 38.Crenshaw JR, Bernhardt KA, Achenbach SJ, Atkinson EJ, Khosla S, Kaufman KR, et al. The circumstances, orientations, and impact locations of falls in community-dwelling older women. Arch Gerontol Geriatr. 2017;73:240–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.MacKinnon CD, Winter DA. Control of whole-body balance in the frontal plane during human walking. J Biomech. 1993;26:633–44. [DOI] [PubMed] [Google Scholar]
- 40.Eng JJ, Winter DA. Kinetic analysis of the lower limbs during walking: what information can be gained from a three-dimensional model? J Biomech. 1995:753–8. [DOI] [PubMed] [Google Scholar]
- 41.Hof AL, Gazendam MGJ, Sinke WE. The condition for dynamic stability. J Biomech. 2005;38:1–8. [DOI] [PubMed] [Google Scholar]
- 42.Carpenter R, Reddi B. The control of posture 5th ed Neurophysiology. CRC Press; 2012, 215–24 [Google Scholar]
- 43.Niino N, Tsuzuku S, Ando F, Shimokata H. Frequencies and circumstances of falls in the National Institute for Longevity Sciences, Longitudinal Study of Aging (NILS-LSA). J Epidemiol. 2000;10:S90–4. [DOI] [PubMed] [Google Scholar]
- 44.Wolf-Klein GP, Silverstone FA, Basavarajo N, Foley CJ, Pascara A, Ma PH. Prevention of falls in the elderly population. Arch of Phys Med Rehabil. 1988;69:689–91. [PubMed] [Google Scholar]
- 45.Morfitt JM. Falls in old people at home: intrinsic versus environmental factors in causation. Public Health. 1983;97:115–20. [DOI] [PubMed] [Google Scholar]
- 46.Clark AN. Factors in fracture of the female femur. A clinical study of the environmental, physical, medical and preventive aspects of this injury. Gerontol Clin (Basel). 1968;10:257–70. [DOI] [PubMed] [Google Scholar]
- 47.Campbell AJ, Reinken J, Allan BC, Martinez GS. Falls in old age: a study of frequency and related clinical factors. Age Ageing. 1981;10:264–70. [DOI] [PubMed] [Google Scholar]
- 48.Grabiner MD, Bareither ML, Gatts S, Marone J, Troy KL. Task-specific training reduces trip-related fall risk in women. Med Sci Sports Exerc. 2012;44:2410–4. [DOI] [PubMed] [Google Scholar]
- 49.Oddsson LI, Karlsson R, Konrad J, Ince S, Williams SR, Zemkova E. A rehabilitation tool for functional balance using altered gravity and virtual reality. J NeuroEng Rehabil. 2007;4:25–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Giboin L-S, Gruber M, Kramer A. Task-specificity of balance training. Hum Mov Sci. 2015;44:22–31. [DOI] [PubMed] [Google Scholar]
- 51.Kaufman KR, Wyatt MP, Sessoms PH, Grabiner MD. Task-specific fall prevention training is effective for warfighters with transtibial amputations. Clin Orthop Relat Res. 2014;472:3076–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blake AJ, Morgan K, Bendall MJ, Dallosso H, Ebrahim SB, Arie TH, et al. Falls by elderly people at home: prevalence and associated factors. Age Ageing. 1988;17:365–72. [DOI] [PubMed] [Google Scholar]
- 53.Wong C, Chihuri S, Li G. Risk of fall-related injury in people with lower limb amputations: A prospective cohort study. J Rehabil Med. 2016;48:80–5. [DOI] [PubMed] [Google Scholar]
- 54.Legro MW, Reiber G, del Aguila M, Ajax MJ, Boone DA, Larsen JA, et al. Issues of importance reported by persons with lower limb amputations and prostheses. JRRD. 1999;36:155–63. [PubMed] [Google Scholar]
- 55.Bellmann M, Schmalz T, Blumentritt S. Comparative biomechanical analysis of current microprocessor-controlled prosthetic knee joints. Arch of Phys Med Rehabil. 2010;91:644–52. [DOI] [PubMed] [Google Scholar]
- 56.Nickens H Intrinsic factors in falling among the elderly. Arch. Intern. Med 1985;145:1089–93. [PubMed] [Google Scholar]
- 57.Quai TM, Brauer SG, Nitz JC. Somatosensation, circulation and stance balance in elderly dysvascular transtibial amputees. Clin Rehabil. 2005;19:668–76. [DOI] [PubMed] [Google Scholar]
- 58.Richardson JK, Eckner JT, Allet L, Kim H, Ashton-Miller JA. Complex and simple clinical reaction times are associated with gait, balance, and major fall injury in older subjects with diabetic peripheral neuropathy. Am J Phys Med Rehabil. 2017;96:8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Steinberg N, Gottlieb A, Siev-Ner I, Plotnik M. Fall incidence and associated risk factors among people with a lower limb amputation during various stages of recovery - a systematic review. Disabil Rehabil. 2018;16:1–10. [DOI] [PubMed] [Google Scholar]
- 60.Hunter SW, Batchelor F, Hill KD, Hill A-M, Mackintosh S, Payne M. Risk factors for falls in people with a lower limb amputation: a systematic review. PM R; 2016:1–12. [DOI] [PubMed] [Google Scholar]
- 61.Winter DA. Biomechanics and Motor Control of Human Movement. 4 ed John Wiley & Sons; 2009. [Google Scholar]
- 62.Viton JM, Mouchnino L, Mille ML, Cincera M, Delarque A, Pedotti A, et al. Equilibrium and movement control strategies in trans-tibial amputees. Prosthet Orthot Int. 2000;24:108–16. [DOI] [PubMed] [Google Scholar]
- 63.Paysant J, Beyaert C, Dati A-M, Martinet N, Andr J-M. Influence of terrain on metabolic and temporal gait characteristics of unilateral transtibial amputees. JRRD. 2006;43:153–10. [PubMed] [Google Scholar]
- 64.Kendell C, Lemaire ED, Dudek NL, Kofman J. Indicators of dynamic stability in transtibial prosthesis users. Gait Posture. 2010;31:375–9. [DOI] [PubMed] [Google Scholar]
- 65.Gates DH, Dingwell JB, Scott SJ, Sinitski EH, Wilken JM. Gait characteristics of individuals with transtibial amputations walking on a destabilizing rock surface. Gait Posture. 2012;36:33–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gates DH, Scott SJ, Wilken JM, Dingwell JB. Frontal plane dynamic margins of stability in individuals with and without transtibial amputation walking on a loose rock surface. Gait Posture. 2013;38:570–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mackenzie L, Byles J. Validation of self-reported fall events in intervention studies. Clin Rehabil. 2006;20:331–9. [DOI] [PubMed] [Google Scholar]
- 68.Jenkins P, Earle-Richardson G, Slingerland DT, May J. Time dependent memory decay. Am. J. Ind. Med 2002;41:98–101. [DOI] [PubMed] [Google Scholar]
- 69.Lamb SE, Jørstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network europe consensus. JAGS. 2005;53:1618–22. [DOI] [PubMed] [Google Scholar]
- 70.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch of Phys Med Rehabil. 2008;89:422–9. [DOI] [PubMed] [Google Scholar]