Abstract
Background and aims
Several studies have documented that consumption of legumes including soybean is inversely associated with systemic inflammation and oxidative stress. This study was done to assess the effects of soy beans or non-soy legumes consumption on C-reactive protein (CRP) and malondialdehyde (MDA) among Patients with Type 2 Diabetes (T2D).
Methods
75 persons with T2D participated in this randomized controlled clinical trial. Participants were randomized to one of the following 3 groups for 8 weeks: soy bean group (taking a cup of cooked soy beans three days a week), legumes group (taking a cup of cooked non-soy legumes three days a week) and control group (taking two servings of red meat three days a week). Anthropometric indices, dietary intakes, and serum MDA and CRP were measured at baseline and after intervention.
Results
A Significant decrease was observed in serum CRP of soy bean group (P = 0.01) which was significantly more than the controls (p = 0.001), while no significant changes of CRP was observed in legume group. Serum MDA changed significantly in none of the 3 groups.
Conclusions
In conclusion, we found that substitution of red meat with soybean but not non- soy legumes may reduce inflammatory factors with no effects on oxidative stress in diabetic patients.
Keywords: Diabetes, Soybean, Legumes, Inflammation, Oxidative stress
Introduction
Accompanied by a parallel rise in cardiovascular diseases (CVDs), prevalence of type 2 diabetes mellitus (T2DM) has significantly increased during the last decades. Global prevalence of T2DM has been estimated to be 8.3%, and many of these patients are unaware of their disease [1, 2]. Body of evidence indicates that the control of inflammatory factors (IF), and oxidative stress (OS) markers are useful to reduce the cardiovascular and microvascular complications in patients with T2DM [3, 4]. Yet, different studies have shown that such secondary prevention strategies in diabetic patients are not fixed perfectly [5–7].
Several studies have reported that more legumes (Soybean and Non-Soy) consumption is associated with better cardio-metabolic outcomes and postulated beneficial effect of legumes consumption on diabetes complications [8–13].
Different studies have shown that legumes including soy beans have some functional phytochemicals which are not nutritive but encompass health benefits [8, 9]. These nutraceutical components possess special features in human health by acting as antioxidant and anti-inflammatory agents; therefore they may have protective functions on pathological conditions which are triggered by oxidative stress including cardiovascular problems [11].
Besides, soy bean is a major source of isoflavones due to having an eccentric concentration of these components, particularly genistein and daidzein. These natural polyphenols have the ability to remove free radicals, activate antioxidant enzymes, and chelate metal catalysts therefore can inhibit oxidases [11, 14].
Results of some studies indicated that higher red meat consumption is associated with greater incidence of T2DM and CVD due to unfavorable inflammatory plasma biomarkers, so it is concluded that red meat substitution with another protein food source would be related to healthier inflammatory profile [15, 16]. To the best of our knowledge there is just few studies which assessed red meat substitution with soy nuts and there is no clinical trial which compared the effects of red meat with other plant based proteins on inflammation and oxidative stress. Besides this is the first study which compared red meat, soy bean and non-soy legumes at the same time in one study. The aim of our study was assessing the effects of red meat replacement with non-soy legumes or soy bean on inflammatory factors and oxidative stress markers in patients with T2DM.
Material and methods
Patients
This study was carried out from December 2016 to April 2017. Participants were recruited from society of diabetes members in Shahid Motahhari endocrinology clinic of Shiraz-Iran via invitation. Inclusion criteria were as follows: at least 6 months since diagnosed as diabetic, age range of 40 to 65 years, middle or high socioeconomic status (ability to buy meat, beans or Soybean), and ability to understand and sign informed consent. Individuals who needed insulin injection or lipid lowering drugs, any diagnose of thyroid disorders, kidney, liver, and cardiovascular diseases, use of any medication or nutritional supplements, being allergic to legumes or soy bean, participation in other studies during the last 6 months, smoking, alcohol consumption, pregnancy and lactation were excluded from participation.
Study design
This study was a single center, parallel group, randomized clinical trial (RCT). Study protocol was approved by ethics Committee of Shiraz University of Medical Sciences, and registered at IRCT with ID number of IRCT2015112925276N1. All procedures followed were in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Based on previous studies [17], sample size was computed as 20 persons per group for an “α” value equal to 0.05 and a power of 80%. This number was increased to 25 persons per group to accommodate dropout rate. After two weeks of run-in period, using a block randomization method eligible participants were randomly assigned to 1 of the following 3 groups in a 1:1:1 ratio for 8 weeks: 1) Control Group: Taking two servings of red meat three days a week and avoiding consumption of legumes and soy beans. 2) Soy Bean Group: Taking a cup of cooked soy beans three days a week and avoiding consumption of legumes and red meat. 3) Legume Group: Taking a cup of cooked non-soy legumes three days a week and avoiding consumption of soybean and red meat.
Based on the Estimated Energy Requirement (EER) equation [18], all diets were designed as balanced macronutrient diets (55% of energy from carbohydrates, 15% of energy from proteins and 30% of energy from fats) for each participant. All participants received the exchange list of foods and were instructed how to use it. Three groups’ diets were identical, but two servings of red meat in control group was replaced by soy beans/legumes three days a week in other groups. Half a cup of cooked legumes/soy bean was considered as one serving of red meat.
Measurements
Clinical and physical examinations were performed at baseline and after 8 weeks. All data were collected by trained nutritionists and all participants were given clear instructions. Body weight was measured using a scale (Seca, Germany), without shoes and in light clothing to the nearest 100 g. Height was measured barefoot by a mounted tape to the nearest 0.1 cm. Then, body mass index was calculated as weight (kg)/height2 (m).Waist circumference (WC) was measured at the level of the iliac crest at the end of normal expiration to the nearest 0.1 cm using a non-stretchable measuring tape. Physical activity was estimated using the international physical activity questionnaire (IPAQ) at baseline, week 4 and week 8. Levels of physical activity were expressed as metabolic equivalent hours per week (METh/w).
Blood samples (7-cc venous blood) were collected at baseline and at the end of the study, and were distributed among tubes containing K2EDTA then centrifuged to separate the serums which were stored at −72 °C for further biochemical analysis.
Serum malondialdehyde (MDA), was measured using standard kit by Elisa method (Zellbio Inc., Germany, intra C.V. = 5.8% and inter C.V. = 7.6%). Plasma CRP concentration was measured by a high sensitivity latex-enhanced immunonephelometric assay on a BN II analyzer (IBL kit, Germany, intra C.V. = 6.8% and inter C.V. = 11.6%).
Three 24-houre food records were taken at the baseline, week 4 and week 8 (each included two weekdays and one weekend). Also compliance to consumption of red meat, soy bean and legumes were assessed using a check list. Energy and nutrients contents of foods were calculated using NUTRITIONIST IV software.
Data analysis
SPSS version 16 was used for statistical analyses. One sample Kolmogorov-Smirnov was used to check the normal distribution of variables. One-way ANOVA was used to compare baseline values of dietary intakes and serum MDA and CRP also to compare the mean changes of serum MDA and CRP after intervention among the three groups. Then Tukey posthoc test was used for two by two comparisons. Effect of intervention in each group was assessed using Paired sample t-test. P values less than 0.05 were considered statistically significant.
Results
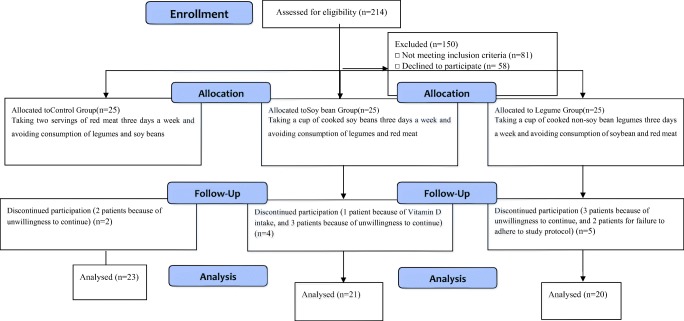
Of 75 persons meeting general eligibility criteria, 64 ones completed the study. Two participants in control group (due to unwillingness to continue the cooperation), four participants in soy bean group (due to intake of vitamin D supplement, and unwillingness to continue the cooperation), and five participants in legume group (due to protocol violation and unwillingness to continue the cooperation) dropped out the study (Fig. 1). No participants reported any adverse effects during the study.
Fig. 1.
Participant flow diagram throughout the study
General characteristics of participants are shown in Table 1. There were no significant differences in sex, age, education, diabetes duration, family history of diabetes, weight, BMI, and WC of participants among 3 groups.
Table 1.
General characteristics and anthropometric indices of participants at Baseline (N = 64)
| Control group (n = 23) |
Soy bean group (n = 21) |
Legume group (n = 20) |
p | |
|---|---|---|---|---|
| Sex (Female/Male) | (19/4) | (14/7) | (13/7) | 0.11** |
| Age (year) | 56 ± 7.3 | 57 ± 7.3 | 59 ± 5.9 | 0.16* |
| Education | 0.48** | |||
| Lower than diploma | 17 (71.9) | 8 (42.1) | 11 (55.0) | |
| Diploma | 5 (20.8) | 6 (31.6) | 6 (30.0) | |
| Academic education | 2 (8.3) | 5 (26.4) | 3 (15.0) | |
| Diabetes duration (years) | 11.29 ± 6.63 | 7.13 ± 5.95 | 8.34 ± 5.67 | 0.08* |
| Family history of diabetes | 0.74** | |||
| Yes | 17 (70.8) | 13 (76.5) | 13 (65.0) | |
| No | 7 (29.2) | 4 (23.5) | 7 (35.0) | |
| Weight (kg) | 67.8 ± 11.3 | 69.2 ± 11.2 | 69.9 ± 10.5 | 0.28* |
| BMI (kg/m2) | 26.7 ± 2.9 | 25.6 ± 3.9 | 27.2 ± 3.4 | 0.37* |
| WC (cm) | 98.3 ± 8.8 | 96.4 ± 9 | 97.4 ± 9.1 | 0.29* |
Except for sex, education and family history of diabetes all values are presented as mean ± standard deviation
BMI body mass index, WC waist circumference
*One-way ANOVA
**K-square test
Comparison of dietary intakes at baseline and during the study, among the 3 groups is shown in Table 2. Results of Paired samples T-test indicated that after 8 weeks of intervention, intake of fiber was significantly more in soy group (p = 0.03) and legume group (p = 0.02) also a significant decrease in cholesterol intake was observed in soy group (p = 0.01) in comparison with baseline values. Results of one-way ANOVA showed statistically significant differences in fiber (P = 0.001) and cholesterol (P = 0.02) intake among intervention and control groups during the study. Tukey post hoc test showed that reduction of cholesterol intake was significantly higher in soy groups (P = 0.01) and the elevated intake of fiber was significantly higher in soy and legume group (P = 0.01) compared to the controls. Intake of energy, Carbohydrate, fat and protein remained unchanged in all groups.
Table 2.
Dietary intakes and physical activity of participants before and during the intervention (N = 64)
| Nutrients | Control group (n = 23) |
Soy bean group (n = 21) |
Legume group (n = 20) |
p** | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before | During | p* | Before | During | p* | Before | During | p* | ||
| Energy(Kcal) | 1865 ± 207.9 | 1874 ± 149.4 | 0.76 | 1870 ± 217.1 | 1794 ± 149.4 | 0.2 | 1849 ± 197.1 | 1901 ± 100.1 | 0.38 | 0.29 |
| Carbohydrate(g) | 255 ± 40.2 | 254 ± 26 | 0.91 | 249 ± 37.1 | 260 ± 32.1 | 0.12 | 257 ± 39.8 | 261 ± 28.9 | 0.67 | 0.37 |
| Fat(g) | 61.6 ± 7.8 | 62 ± 8.1 | 0.63 | 63.3 ± 8.3 | 62.3 ± 9.2 | 0.84 | 60.3 ± 7.2 | 61.3 ± 7.1 | 0.32 | 0.72 |
| Protein(g) | 75.8 ± 11.3 | 79 ± 9.6 | 0.19 | 76.2 ± 11.9 | 78.8 ± 14.9 | 0.38 | 77.4 ± 13.6 | 73 ± 11.2 | 0.43 | 0.67 |
| Fiber(g) | 7/4 ± 4.2 | 8/5 ± 3.6 | 0.17 | 8/1 ± 3/5 | 15.4 ± 6.8a | 0.03 | 7/7 ± 3/8 | 14.4 ± 7.1a | 0.02 | 0.001 |
| Vitamin E(mg) | 143 ± 61 | 139 ± 57 | 0.61 | 170 ± 101 | 185 ± 121 | 0.11 | 155 ± 65 | 151 ± 73 | 0.13 | 0.28 |
| Vitamin C(mg) | 143 ± 61 | 139 ± 57 | 0.61 | 170 ± 101 | 185 ± 121 | 0.11 | 155 ± 65 | 151 ± 73 | 0.13 | 0.28 |
| Cholesterol(mg) | 181/8 ± 32/8 | 187/1 ± 4 | 0.42 | 192/3 ± 40/8 | 110 ± 22.1a | 0.01 | 190/2 ± 33 | 168 ± 42.4 | 0.06 | 0.02 |
| Physical activity (METs) | 35.2 ± 3.9 | 34.1 ± 3.5 | 0.23 | 33 ± 4.1 | 33.2 ± 3.1 | 0.51 | 33 ± 4.3 | 32.2 ± 3.4 | 0.27 | 0.46 |
All Data are presented as mean ± Standard deviation, *Paired t-test, **One-way ANOVA, a:Tukey post hoc test showed significant differences compared to Control Group (p = 0.01)
Effects of 8 weeks intervention on biochemical factors are presented in Table 3. A significant decrease was observed in CRP of soy bean group (P = 0.01) in comparison with baseline values. Also compared to the controls a significant decline was seen in CRP values of soy bean group (P = 0.04). Serum MDA changed significantly in none of the 3 groups.
Table 3.
Comparison of biochemical parameters’ changes among three groups (N = 64)
| Control group (N = 23) |
Soy bean group (N = 21) |
Legume group (N = 20) |
p** | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | p* | Before | After | p* | Before | After | p* | ||
| MDA (mmol/l) | 4.3 ± 0.6 | 4.1 ± 0.5 | 0.11 | 4.1 ± 0.5 | 4.2 ± 0.4 | 0.39 | 4.2 ± 0.6 | 4.1 ± 0.7 | 0.43 | 0.38 |
| CRP (μg/ml) | 1.2 ± 0.2 | 1.3 ± 0.2 | 0.21 | 1.2 ± 0.2 | 1 ± 0.3a | 0.01 | 1.2 ± 0.2 | 1.2 ± 0.1 | 0.17 | 0.04 |
All data are presented as mean ± Standard deviation, *Paired t-test, ** One-way ANOVA, a: Tukey post hoc test showed significant change
Compared to Control Group (p = 0.001)
CRP C-reactive protein, MDA malondialdehyde
Discussion
This study explored the effects of red meat substitution with soybean or non- soy legumes on inflammatory markers and oxidative stress in adults with T2D. In the current study, beneficial effect on CRP level was observed following a diet rich in soybean. Azadbakht et al. also found this effect. They performed an 8 week intervention in which red meat was substituted with soy nut or soy proteins and found that inflammatory markers including CRP improved just in soy nut group [19]. In contrast with our findings Hanson et al. did not find any influence on CRP concentration following soy consumption [20] besides Bakhtiari et al. found a non-significant reduction in CRP in soy group [21]. Although Soy contains fiber, phytoestrogens (such as isoflavones) and polyunsaturated fats which each of them individually has regressive effects on markers of inflammation and cause its beneficial effects, these controversies might be justified by different baseline CRP of participants in the studies. Results of a meta-analysis on effect of soy isoflavones on circulating CRP showed that baseline CRP would have modifier effect on CRP lowering action of soy consumption and soy isoflavones exert a significant CRP reduction just among participants with elevated CRP [22].
Polyunsaturated Fatty Acid content of diet specially appropriate combination of ω3 and ω6 fatty acids has substantial role in adjusting pro-inflammatory conditions; hence as mentioned above, some inflammatory protection properties of soy can be attributed to its fatty acids content which consists of both ω3 and ω6 fatty acids [19, 23].
While the result of our study did not demonstrate any significant changes in CRP level in legumes group, prior studies have shown that legumes consumption can improve some cardio metabolic risk factors such as some inflammatory markers in diabetic patients. There are some reports, indicating that greater consumption of plant based protein food versus red meat may reduce the progression of T2D and CVDs [24, 25], also an inverse association between legumes consumption and CRP level has been reported [11, 12, 26].
While the present study resulted in no significant changes in MDA; there are various results about soy bean and/or legumes consumption effects on oxidative stress in different trials; Jamilian et al. conducted a 6 week RCT among women with gestational diabetes mellitus. They compared a diet containing 0.8 g/kg protein as control group with a diet containing the same amount of protein consisted of 35% soy protein; and observed a significant improvement of biomarkers of oxidative stress in soy group [27]. Also in a crossover RCT which was conducted among healthy men and women, consumption of 2 g/kgBW soybean for one week resulted in an increase in total antioxidant capacity [28]. Crujeiras et al. [29] demonstrated that a balanced diet with moderate caloric restriction including 4 servings of legumes per week, could empower oxidative stress improvement, while Nestel et al. [22] found no effect on oxidative stress markers following consumption of 4 servings of legumes per week with no calorie restriction. These differences are probably related to different target population and/or study design, for instance in Crujeiras et al. study weight loss through calorie restriction may resulted in oxidative stress improvement, which was not applied in 2 other studies.
Overally higher consumption of food rich in complex carbohydrates and fiber such as soy and non-soy legumes, along with lower consumption of animal products and their fat can be great measure for better protection against many inflammatory and oxidative stress related diseases.
Conclusion
We concluded that, red meat substitution with soybean among patients with T2D can attenuate inflammation but non-soybean legumes do not exert the same effect. Subsequent results showed that substitution of red meat with none of the legumes or soy bean can improve oxidative stress status. Future studies by using higher doses of soy and legumes beside longer duration of intervention are needed to resolve previous controversies related to soy and legume effects on oxidative stress and inflammatory factors.
Acknowledgements
The authors would like to thank all participants for their kind cooperation. This article was extracted from an MSc thesis written by Zeinab Hemmatdar which was funded by Shiraz University of Medical Sciences with the grant No 94-01-84-9916.
Compliance with ethical standards
Conflict of interest
The authors declared that they have no conflict of interest.
References
- 1.Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–149. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Mannucci E, Dicembrini I, Lauria A, Pozzilli P. Is glucose control important for prevention of cardiovascular disease in diabetes? Diabetes Care. 2013;36(Suppl 2):S259–S263. doi: 10.2337/dcS13-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HAW. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 5.Committee PP, Classification A. Standards of medical care in diabetes-2010. Diabetes Care. 2010;33(Suppl 1):S11–61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jørgensen CH, Gislason GH, Ahlehoff O, Andersson C, Torp-Pedersen C, Hansen PR. Use of secondary prevention pharmacotherapy after first myocardial infarction in patients with diabetes mellitus. BMC Cardiovasc Disord. 2014;14:1–9. doi: 10.1186/1471-2261-14-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Classification I. Standards of medical care in diabetes-2009. Diabetes Care. 2009;32(Suppl 1). [DOI] [PMC free article] [PubMed]
- 8.Jayagopal V, Albertazzi P, Kilpatrick ES, Howarth EM, Jennings PE, Hepburn DA, et al. Beneficial effects of soy phytoestrogen intake in postmenopausal women with type 2 diabetes. Diabetes Care. 2002;25(10):1709–1714. doi: 10.2337/diacare.25.10.1709. [DOI] [PubMed] [Google Scholar]
- 9.Mateos-Aparicio I, Redondo Cuenca A, Villanueva-Suárez MJ, Zapata-Revilla MA. Soybean, a promising health source. Nutr Hosp. 2008;23(4):305–312. [PubMed] [Google Scholar]
- 10.Anderson JW, Smith BM, Washnock CS. Cardiovascular and renal benefits of dry bean and soybean intake. Am J Clin Nutr. 1999;70(3 Suppl):464–474. doi: 10.1093/ajcn/70.3.464s. [DOI] [PubMed] [Google Scholar]
- 11.Bouchenak M, Lamri-Senhadji M. Nutritional quality of legumes, and their role in Cardiometabolic risk prevention: a review. J Med Food. 2013;16(3):185–198. doi: 10.1089/jmf.2011.0238. [DOI] [PubMed] [Google Scholar]
- 12.Saraf-Bank S. Esmaillzadeh A, Faghihimani E, Azadbakht L. Effect of non-soy legume consumption on inflammation and serum adiponectin levels among first-degree relatives of patients with diabetes: a randomized, crossover study. Nutrition. 2015;31(3):459–465. doi: 10.1016/j.nut.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Marventano S, Izquierdo Pulido M, Sánchez-González C, Godos J, Speciani A, Galvano F, Grosso G. Legume consumption and CVD risk: a systematic review and meta-analysis. Public Health Nutr. 2017;20(2):245–254. doi: 10.1017/S1368980016002299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Acker SA, van Balen GP, van den Berg DJ, Bast A, van der Vijgh WJ. Influence of iron chelation on the antioxidant activity of flavonoids. Biochem Pharmacol. 1998;56(8):935–943. doi: 10.1016/S0006-2952(98)00102-6. [DOI] [PubMed] [Google Scholar]
- 15.Ley SH, Sun Q, Willett WC, Eliassen AH, Wu K, Pan A, et al. Associations between red meat intake and biomarkers of inflammation and glucose metabolism in women 1–3. Am J Clin Nutr. 2014;99(2):352–360. doi: 10.3945/ajcn.113.075663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bendinelli B, Palli D, Masala G, Sharp SJ, Schulze MB, Guevara M, et al. Association between dietary meat consumption and incident type 2 diabetes: the EPIC-InterAct study. Diabetologia. 2013;56(1):47–59. doi: 10.1007/s00125-012-2718-7. [DOI] [PubMed] [Google Scholar]
- 17.Safaeiyan A, Pourghassem-Gargari B, Zarrin R, Fereidooni J, Alizadeh M. Randomized controlled trial on the effects of legumes on cardiovascular risk factors in women with abdominal obesity. ARYA Atheroscler. 2015;11(2):117–125. [PMC free article] [PubMed] [Google Scholar]
- 18.Pearson D, Grace C. Appendix 10 estimated energy requirement ( EER ). 2012;
- 19.Azadbakht L, Kimiagar M, Mehrabi Y, Esmaillzadeh A, Hu FB, Willett WC. Soy consumption, markers of inflammation, and endothelial function: a cross-over study in postmenopausal women with the metabolic syndrome. Diabetes Care. 2007;30(4):967–973. doi: 10.2337/dc06-2126. [DOI] [PubMed] [Google Scholar]
- 20.Hanson LN, Engelman HM, Alekel DL, Schalinske KL, Kohut ML, Reddy MB. Effects of soy isoflavones and phytate on homocysteine , C-reactive protein, and iron status in postmenopausal women 1-3. 2006;(2):774–80. [DOI] [PubMed]
- 21.Bakhtiary A, Yassin Z, Hanachi P, Rahmat A, Ahmad Z, Jalali F. Effects of soy on metabolic biomarkers of cardiovascular disease in elderly women with metabolic syndrome. Arch Iran Med. 2012;15(8):462–468. [PubMed] [Google Scholar]
- 22.Dong J-Y, Wang P, He K, Qin L-Q. Effect of soy isoflavones on circulating C-reactive protein in postmenopausal women. Menopause. 2011;18(11):1256–1262. doi: 10.1097/gme.0b013e31821bfa24. [DOI] [PubMed] [Google Scholar]
- 23.Pischon T, Hankinson SE, Hotamisligil GS, Rifai N, Willett WC, Rimm EB. Habitual dietary intake of n-3 and n-6 fatty acids in relation to inflammatory markers among US men and women. Circulation. 2003;108(2):155–160. doi: 10.1161/01.CIR.0000079224.46084.C2. [DOI] [PubMed] [Google Scholar]
- 24.Montonen J, Boeing H, Fritsche A, Schleicher E, Joost HG, Schulze MB, Steffen A, Pischon T. Consumption of red meat and whole-grain bread in relation to biomarkers of obesity, inflammation, glucose metabolism and oxidative stress. Eur J Nutr. 2013;52(1):337–345. doi: 10.1007/s00394-012-0340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Micha R, Michas G, Mozaffarian D, Lauwers E, Kaluza J, Wolk A, et al. Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes – an updated review of the evidence. Clin Nutr. 2012;14(6):515–524. doi: 10.1007/s11883-012-0282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a Metaanalysis of population-based prospective studies. Eur J Cardiovasc Prev Rehabil. 1996;3(2):213–219. doi: 10.1177/174182679600300214. [DOI] [PubMed] [Google Scholar]
- 27.Jamilian M, Asemi Z. The effect of soy intake on metabolic profiles of women with gestational diabetes mellitus. J Clin Endocrinol Metab. 2015;100(12):4654–4661. doi: 10.1210/jc.2015-3454. [DOI] [PubMed] [Google Scholar]
- 28.Celec P, Hodosy J, Pálffy R, Gardlík R, Halčák L, Ostatníková D. The short-term effects of soybean intake on oxidative and carbonyl stress in men and women. Molecules. 2013;18(5):5190–5200. doi: 10.3390/molecules18055190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crujeiras AB, Parra D, Abete I, Martínez JA. A hypocaloric diet enriched in legumes specifically mitigates lipid peroxidation in obese subjects. Free Radic Res. 2007;41(4):498–506. doi: 10.1080/10715760601131935. [DOI] [PubMed] [Google Scholar]