Abstract
Background
With increasing survival rates among patients with myocardial infarction (MI), more demands are placed on secondary prevention. While physical activity (PA) efforts to obtain a sufficient PA level are part of secondary preventive recommendations, it is still underutilized. Importantly, the effect of changes in PA after MI is largely unknown. Therefore, we sought to investigate the effect on survival from changes in PA level, post‐MI.
Methods and Results
Data from Swedish national registries were combined, totaling 22 227 patients with MI. PA level was self‐reported at 6 to 10 weeks post‐MI and 10 to 12 months post‐MI. Patients were classified as constantly inactive, increased activity, reduced activity, and constantly active. Proportional hazard ratios were calculated. During 100 502 person‐years of follow‐up (mean follow‐up time 4.2 years), a total of 1087 deaths were recorded. Controlling for important confounders (including left ventricular function, type of MI, medication, smoking, participation in cardiac rehabilitation program, quality of life, and estimated kidney function), we found lower mortality rates among constantly active (hazard ratio: 0.29, 95% confidence interval: 0.21–0.41), those with increased activity (0.41, 95% confidence interval: 0.31–0.55), and those with reduced activity (hazard ratio: 0.56, 95% confidence interval: 0.45–0.69) during the first year post‐MI, compared with those being constantly inactive. Stratified analyses indicated strong effect of PA level among both sexes, across age, MI type, kidney function, medication, and smoking status.
Conclusions
The present article shows that increasing the PA level, compared with staying inactive the first year post‐MI, was related to reduced mortality.
Keywords: mortality, physical exercise, registry
Subject Categories: Cardiovascular Disease, Exercise, Secondary Prevention
Clinical Perspective
What Is New?
Patients who remained physically active over the first year post‐myocardial infarction (MI) had the lowest risk of mortality, over a 4.2‐year follow‐up period.
However, changes in physical activity level the first‐year post‐MI is important, lowering the risk of mortality in patients increasing their activity and increasing risk in those with decreased activity.
It seems not to be too late to start being active post‐MI, since the group with increased activity post‐MI did not differ in survival from the constantly active group.
What Are the Clinical Implications?
The shown relation to survival, in patients who maintain or increase their level of physical activity post‐MI, reinforces the importance of the present guidelines and highlights the need for their implementation in secondary prevention.
Being active post‐MI seems to be equally important for different subgroups.
Introduction
Myocardial infarction (MI) remains one of the most feared complications of cardiovascular disease (CVD), being associated with substantial morbidity and mortality. However, because of the advancements in emergency care, including the widespread use of cardiac interventions as well as antithrombotic, antihypertensive, and dyslipidemia treatment, a larger proportion of patients now survive their first MI.1, 2 This positive development has resulted in more focus being put on secondary prevention.
Physical activity (PA) is a well‐recognized factor in the primary prevention of CVD.3, 4 Also in patients with established CVD, structured physical activity (PA)5 as well as increases in PA6, 7 have been shown to be associated with reduced cardiovascular mortality. These effects rest on multiple positive effects on traditional risk factors for CVD, including hypertension, dyslipidemia, obesity, and diabetes mellitus as well as on possible effects on atherosclerotic progression, endothelial dysfunction, autonomic control, and subsequent arrhythmia risk.8, 9 Thus, a sufficiently high PA level is recommended as first‐line treatment in primary and secondary prevention guidelines10 globally. However, the adherence to these PA recommendations, and the use of exercise as part of regular treatment in health care, vary to a great extent.11
Atherosclerosis is a progressing disease, and the disease itself, and its consequences, may affect the ability of the individual to be sufficiently physically active both before and after a cardiac event. One limitation of earlier studies on the association between the level of PA and survival post‐MI is the risk of selection bias (ie, that the individuals with the most advanced disease are also the least active because of their functional status). Therefore, changes in PA level during the period following the event, rather than a single measure of PA, may provide more information when assessing the effect of rehabilitation interventions. The effect of lifestyle‐focused cardiac rehabilitation has been investigated, showing reduced risk of readmissions and decreased cardiovascular mortality, while inconsistent findings for total mortality exist.12, 13 Cardiac rehabilitation focusing on risk reduction has also been shown to reduce mortality.14 However, many patients are not offered cardiac rehabilitation for various reasons. Also, cardiac rehabilitation is multifactorial in its nature, and the isolated effect from exercise may be difficult to identify.15
Little is known about the long‐term effects on mortality from changes in PA levels in patients with MI. In a pioneer article, Steffen‐Batey et al16 reported considerably lowered mortality in patients who increased their activity (Relative risk (RR)=0.11), compared with those who remained physically inactive, in a cohort of 406 male and female MI patients. Recently, another study on 856 women in the Women's Health Initiative‐Observational study, showed similar results.7 However, additional and larger studies are needed, to be able to study these relations in important strata, related to the severity of the MI, comorbidities, or consequences, such as kidney function, quality of life, and the degree of tolerated medication. Such comparisons would be of clinical importance, directly influencing the treatment post‐MI.
Therefore, the aim of this study was to assess the long‐term survival among patients with MI in relation to changes in self‐reported PA in a large nationwide cohort of Swedish patients with MI. Furthermore, we aimed to assess any moderating effects from known risk factors on this relationship.
Methods
Data, analytical methods, and study materials will not be made available to other researchers by the authors for purpose of reproducing the results or replicating the procedure. The authors are not authorized to share SWEDEHEART data.
We obtained data from the national SWEDEHEART registry (Swedish Web‐system for Enhancement and Development of Evidence‐based care in Heart disease Evaluated According to Recommended Therapies17 including the initial care [subregistry RIKS‐HIA] and all subsequent MI‐related care [subregistry SEPHIA]). SWEDEHEART has an uptake of >90% of all cardiology units in Sweden, and the cohort can be regarded as representative of the Swedish patients with MI. The SWEDEHEART subregistry SEPHIA (Secondary Prevention after Heart Intensive Care Admissions)18 provided information from 2 follow‐up visits, at 6 to 10 weeks and 12 months post‐MI, which included data on secondary prevention treatments, lifestyle, and prevalence of risk factors. The primary outcome was mortality, which was obtained from the Swedish Census registry. Mortality data were extracted on October 7, 2014. Mean follow‐up time (ie, between date for MI and date of death or end of study) was 1635 days or 4.2 years.
We included all patients (n=22 227) between ages 18 and 75 years who were diagnosed with their first MI (International Classification of Diseases, Tenth revision [ICD‐10] code I.21) between December 28, 2004 and October 25, 2013 and who provided complete data in the SWEDEHEART registry (Figure 1).
Figure 1.
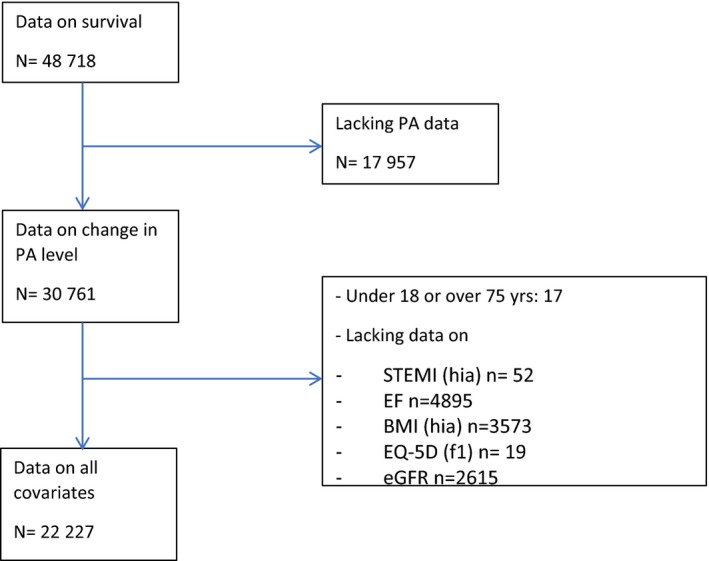
Flow chart for inclusion in analyses. BMI indicates body mass index; EF, ejection fraction; eGFR, estimated glomerular filtration rate; EQ‐5D, EuroQol‐5 dimensions; PA, physical activity; STEMI, ST‐segment–elevation myocardial infarction.
From the SWEDEHEART registry, age, body mass index, serum creatinine, height, sex, type of MI, and left ventricular function were obtained. Type of MI was based on a clinical assessment and patients were classified as having had a ST‐segment‐elevation MI (STEMI), or a non‐ST‐segment‐elevation MI (NSTEMI). Left ventricular function was expressed as ejection fraction (EF) in percent, and was further divided into >50%, 49% to 40%, or ≤40%. The use of percutaneous cardiac interventions during treatment was also recorded in the SWEDEHEART and coded as yes or no. Estimated glomerular filtration rate (eGFR) was based on plasma creatinine values calculated according to the Cockcroft‐Gault formula [eGFR=(1.23×(140−age)×body mass)/serum creatinine and eGFR=(1.04×(140−age)×body mass)/serum creatinine, for men and women, respectively], which has previously been used in analyses of the SWEDEHEART registry.19 eGFR was dichotomized at 60 mL/min per 1.73 m2, to identify normal or mildly decreased GFR from moderately decreased or more pronouncedly decreased GFR.
PA was reported in the SEPHIA subregistry at both follow‐up visits as self‐reported number of PA sessions, 30 minutes or longer, during the last 7 days. Values between zero and 7 were accepted in the registry. Patients were classified as “inactive” if they reported none or 1 session of PA per week, only. Patients reporting 2 or more sessions per week were classified as “active.” Patients were further classified according to changes in activity level between the 2 secondary prevention visits (at 6–10 weeks and 12 months, respectively), as constantly being inactive, having reduced activity, increased activity, or being constantly active. Full pharmacological treatment was identified as being treated with angiotensin‐converting enzyme inhibitors, β‐blocking agent, statins, or other lipid‐lowering agents and antithrombogenic agents (coded as yes or no). Smoking status (never‐smoker, ex‐smoker since >1 month or smoker) was recorded at the first rehabilitation visit, 6 to 10 weeks after discharge from the hospital. When data were missing on smoking (n=32), additional data were obtained from the second visit. Data on participation in exercise‐based cardiac rehabilitation during the year following MI was obtained from the second rehabilitation visit. Data from the Euro‐Qol 5 dimensions (EQ‐5D) from the first visit was used to estimate health‐related quality of life.20 The Regional Ethics Board in Stockholm, Sweden approved this study (2013/2067‐31). No informed consent was required. The corresponding author had full access to all the data in the study and takes responsibility for its integrity and the data analysis.
Statistics
Descriptive demographic and clinical characteristics were analyzed using means (SDs) and percentage. Differences between survivors and fatal cases were tested using the t test and χ2 test. Hazard ratios (HRs) and their 95% confidence interval were computed using Cox proportional hazard ratios using the SPSS Cox regression with time‐dependent covariate module. Hazard ratios for the 4 PA strata (constantly active, reduced activity, increased activity, or constantly inactive) were computed unadjusted and controlled for potential confounders. In the fully adjusted models, age, sex, date for MI, body mass index, EQ‐5D, EF, type of MI, the use of percutaneous cardiac interventions, eGFR, smoking, pharmacological treatment, and participation in cardiac rehabilitation training were included. We checked the proportionality assumption using scaled Schönfelts residuals. All variables were checked for proportionality, including the separate measures from the first and second PA assessment. A weak and borderline significance was noted only for PA strata. Because of this, we included an interaction term for time × PA strata in all analyses. Formal interaction analyses for HRs between PA strata were performed as proposed by Bland and Altman.21 HRs was considered to be statistically significant if the 95% confidence interval did not include the value of 1. All statistics were performed in IBM SPSS (version 21).
Results
Subject inclusion is described in Figure 1. The included and nonincluded patients differ in some aspects. Those with PA data, compared with those without, were less likely to be smokers (11.0% versus 13.6%), and have a low eGFR (8.2% versus 10.1%). Also their survival was lower (90.0% versus 94.2%). When comparing those included with PA data and those with PA data but lacking other variables, the latter group was less likely to have full medication (64.2% versus 69.6%), have had a STEMI (37.7% versus 41.1%), and more likely to be female (28.7% versus 26.1%). Also their survival was lower (92.0% versus 95.1%).
Subject characteristics, for the 22 227 included MI patients, are given in Table 1. All the examined variables differed across PA strata, except for pharmacological treatment, where no difference could be seen between PA groups. Some differences were small, albeit statistically significant (age, body mass index). Women and current smokers were overrepresented in the constantly inactive strata, as were patients with NSTEMI. Constantly active participants also participated in exercise‐based cardiac rehabilitation to a higher degree (40.9% versus 21.6%) compared with the constantly inactive group.
Table 1.
Subject Description
| Constantly Inactive (n=2361) | Reduced Activity (n=3418) | Increased Activity (n=1998) | Constantly Active (n=14 450) | |
|---|---|---|---|---|
| Number of deaths (total 1087) | 291 | 198 | 103 | 495 |
| Person‐y at risk (total 100 502 person‐y) | 10 213 | 15 593 | 8932 | 65 764 |
| n (%) | n (%) | n (%) | n (%) | P Value | |
|---|---|---|---|---|---|
| Sex | |||||
| Female | 785 (33.2) | 892 (26.1) | 587 (29.4) | 3542 (24.5) | <0.001 |
| Male | 1576 (66.8) | 2526 (73.9) | 1411 (70.6) | 10 908 (75.5) | |
| STEMI | 874 (37.0) | 1459 (42.7) | 818 (40.9) | 6284 (43.5) | <0.001 |
| Ejection fraction | |||||
| >50 | 1434 (60.7) | 2189 (64.0) | 1295 (64.8) | 9955 (68.9) | <0.001 |
| 40–49 | 528 (22.4) | 732 (21.4) | 416 (20.8) | 2818 (19.5) | |
| <39 | 399 (16.9) | 497 (14.5) | 287 (14.4) | 1677 (11.6) | |
| Participation in cardiac rehabilitation training (@12 mo) | 510 (21.6) | 1258 (36.8) | 611 (30.6) | 5909 (40.9) | <0.001 |
| PCI during treatment | 1782 (75.5) | 2707 (79.2) | 1547 (77.4) | 11 683 (80.9) | <0.001 |
| Smoking status (@6–10 wks) | |||||
| Never‐smoker | 541 (22.9) | 943 (27.6) | 616 (30.8) | 5180 (35.8) | <0.001 |
| Ex‐smoker | 1347 (57.1) | 2010 (58.8) | 1101 (55.1) | 8075 (55.9) | |
| Smoker | 473 (20.0) | 465 (13.6) | 281 (14.1) | 1195 (8.3) | |
| eGFR <60 mL/min per 1.73 m2 | 336 (14.2) | 243 (7.1) | 197 (9.9) | 1011 (7.0) | <0.001 |
| Full pharmacological treatment | 1648 (69.8) | 2417 (70.7) | 1369 (68.5) | 10 045 (69.5) | 0.36 |
| Age, y | |||||
| Mean (SD) | 62.8 (9.1) | 60.8 (9.0) | 62.0 (8.9) | 61.9 (8.4) | <0.001 |
| Age distribution | |||||
| Under 40 y, n | 43 | 64 | 38 | 202 | |
| 40–49, n | 209 | 419 | 196 | 1376 | |
| 50–59, n | 602 | 1060 | 511 | 4017 | |
| 60–69, n | 973 | 1326 | 902 | 6627 | |
| ≥70, n | 534 | 549 | 351 | 2228 | |
| EQ‐5D score (SD) | 0.69 (0.3) | 0.81 (0.22) | 0.77 (0.25) | 0.86 (0.18) | <0.001 |
| BMI, kg/m2 (SD) | 28.3 (5.5) | 28.3 (0.22) | 27.6 (4.44) | 27.1 (5.3) | <0.001 |
BMI indicates body mass index; eGFR, estimated glomerular filtration rate; EQ‐5D, EuroQol‐5 dimensions; PCI, percutaneous coronary intervention; STEMI, ST‐segment‐elevation myocardial infarction.
Patients reporting being active at both 6 to 10 weeks, and 1‐year post‐MI, had higher EQ‐5D, less prevalence of low eGFR, more often underwent percutaneous cardiac interventions, and had a higher EF post‐MI (Table 1).
In uncontrolled analyses, mortality (cases per 1000 person‐years with 95% confidence interval) in the 4 PA strata was 28.5 (25.3–32.0) among the constantly inactive, 12.7 (11.0–14.6) among those who reduced their activity, 11.5 (9.4–14.0) among those who increased their activity, and 7.5 (6.9–8.2) among the constantly active patients. In the fully controlled model, HRs for mortality were lower for those being constantly active, and for those with increased and decreased activity strata compared with those in the constantly inactive strata. However, HR for patients who increased and patients who decreased their PA did not differ. Constantly active patients had lower HR compared with individuals decreasing their PA level. HR for patients who increased their PA level did not differ from those being constantly active (Table 2, Figure 2).
Table 2.
HR (95% CI) for the PA Strata in Age‐ and Sex‐Adjusted and Fully Adjusted Models
| Constantly Inactive | Reduced Activity | Increased Activity | Constantly Active | ||
|---|---|---|---|---|---|
|
Full sample 1087 deaths 100 502 person‐y |
Age‐sex | 1 (ref) |
0.43 (0.35–0.53) 1 (ref) |
0.32 (0.24–0.43) 0.83 (0.62–1.12) 1 (ref) |
0.19 (0.14–0.26) 0.54 (0.37–0.80) 0.82 (0.49–1.37) |
|
1087 deaths 100 502 person‐y |
Fully adjusted | 1 (ref) |
0.56 (0.45–0.69) 1 (ref) |
0.41 (0.31–0.55) 0.82 (0.61–1.10) 1 (ref) |
0.29 (0.21–0.41) 0.64 (0.43–0.94) 0.95 (0.57–1.61) |
Fully adjusted for age, sex, date of myocardial infarction, body mass index, estimated glomerular filtration rate, EuroQol‐5 dimensions, ejection fraction, ST‐elevation myocardial infarction, percutaneous coronary intervention, smoking status, pharmacological treatment, participation in cardiac rehabilitation training, and an interaction term for time × physical activity strata. CI indicates confidence interval; HR, hazard ratio; PA, physical activity.
Figure 2.
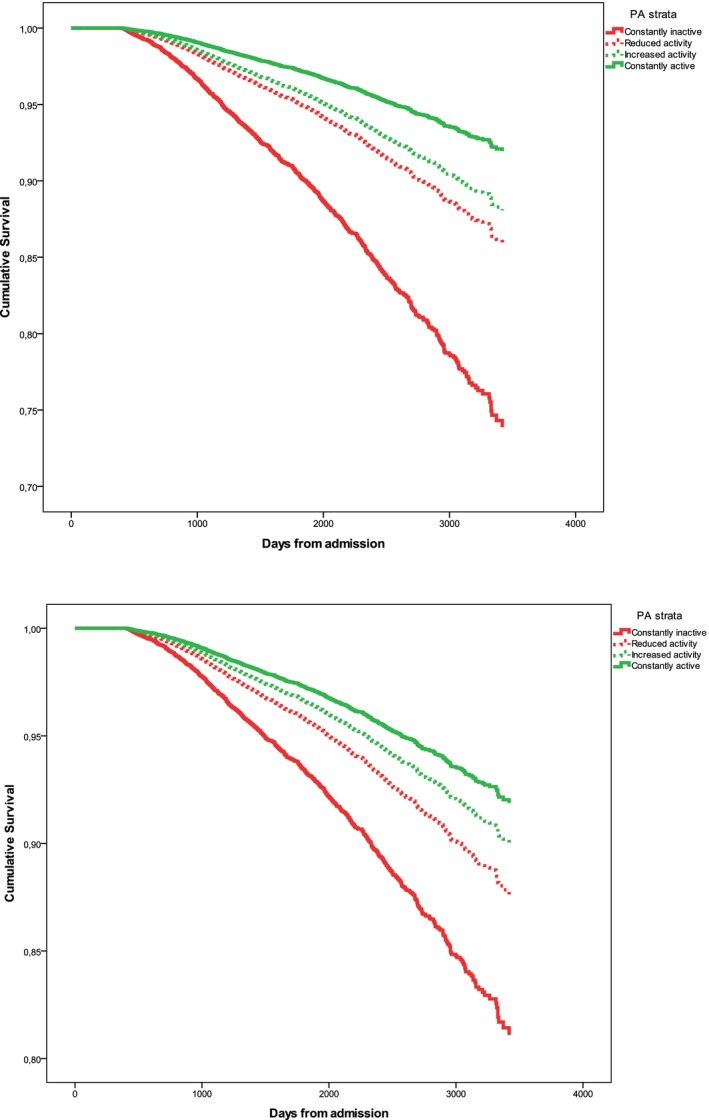
All‐cause mortality age and sex adjusted (upper) and fully adjusted (lower) among individuals with different physical activity (PA) strata. Fully adjusted for age, sex, date of myocardial infarction, body mass index, estimated glomerular filtration rate, EuroQol‐5 dimensions, ejection fraction, ST‐elevation myocardial infarction, percutaneous coronary intervention, smoking status, pharmacological treatment, participation in cardiac rehabilitation training, and an interaction term for time × PA strata.
No interactions were found for any of the variables in the full model, indicating similar differences between PA strata and mortality between age, sex, STT changes, the use of percutaneous cardiac interventions, Eq‐5D, eGFR, cardiac rehabilitation, smoking status, and pharmacological treatment. The exception was EF, where HRs in the reduced PA strata were 0.42 (0.27–0.67) and 0.63 (0.42–0.93) for EF 40% to 50% and EF <40%, respectively. For the increased PA strata, corresponding values were 0.56 (0.30–1.10) and 0.20 (0.10–0.41) and for the constantly active strata 0.39 (0.19–0.79) and 0.20 (0.10–0.41).
We also related mortality to activity levels at the 2 assessments separately. In age‐ and sex‐controlled analyses, active patients had lower mortality at both assessments, with HR (95% confidence interval=0.42 [0.38–0.48] and 0.41 [0.36–0.46]) for the first and second assessment, respectively. In fully controlled analyses, corresponding values were 0.58 (0.51–0.67) and 0.53 (0.47–0.60), for the first and second assessment, respectively.
Discussion
The main result of this study, based on a national registry of unselected patients with MI, is that the mortality among inactive patients, who increase their PA level during the first year following a MI, was much lower, over a 4.2‐year follow‐up period, compared with those who remained inactive. The lowest risk was seen in patients who remained physically active over the first year, post‐MI. Results for the group increasing their PA level is interesting, since the results indicate that patients who were initially inactive (which previous single‐assessment‐based studies have indicated to be at high risk) can reduce the risk by increasing activity. HRs in the group with increasing activity post‐MI did not differ from the constantly active group at follow‐up. The previous studies have also concluded that this group may be more affected by unmeasured factors or residual confounding, which in turn worsen the prognosis. Although this might well be present in this study, results from the group increasing their activity level post‐MI clearly show that mortality is lower in this group compared with the constantly inactive group, controlled for a large number of covariates.
Similarly, results from the group decreasing their PA level indicate that those who were active 6 to 10 weeks after MI but reduced PA have a worse prognosis, as compared with those remaining physically active. Again, even if unmeasured and uncontrolled factors may differ between active and inactive patients at 6 to 10 weeks after MI, changes in PA level over 1 year were still related to mortality. Patients potentially having a more severe disease still benefit from PA increase to a similar extent as those with less severe disease. The exception was between patients with EF between 40% and 50% and EF <40%, where HRs differed between PA strata. Results indicated that patients with a low EF (<40%), compared with a moderately reduced EF 40% to 50%, showed an even stronger risk reduction among constantly active patients and patients increasing their PA level.
When analyzing the 2 assessments separately, we found smaller risk reductions among active patients as compared with those being constantly active. One possible explanation for this is that the inactive group at a single assessment will include participants with either a more active future or being more active in the past, which would dilute the contrast. This stresses the importance of studying PA level at more than 1 time point. Also, these results add to previous studies, by showing that these relations seem independent of cardiac rehabilitation participation in major subgroups post‐MI. Also, the similarity of the HRs found at the 2 assessments (6–10 weeks and 10–20 months post‐MI) when analyzed separately can be taken as an argument against a possible competing hypothesis that the type or intensity of the PA performed at the 2 time points differ.
Presently, the association between higher levels of PA and lower risk of events in those with cardiovascular disease22 is well established. We were able to confirm this association and also expand on the previous findings by Stefen‐Batey16 and Gorczyca7 by identifying a lower risk in those patients with MI who increased their activity and an increased risk in those decreasing their activity, during the first year post‐MI. The present study, however, includes >22 000 patients with MI, and allowed for adjusting for multiple possible confounders, which was not possible in the previous studies. We could also show that this was true for several important subgroups, including older patients, those having heart failure, those with decreased kidney function, smokers, and for both sexes.
Importantly, our study included the sum of all self‐reported PA and exercise, and not only exercise‐based cardiac rehabilitation, which has earlier been found be related to lower mortality post‐MI.12, 13 Indeed, our results were independent of participation or nonparticipation in cardiac rehabilitation. Exercise‐based cardiac rehabilitation performed at home or at the hospital have both been related to CVD reduction in patients with MI.23 However, far from all patients are offered cardiac rehabilitation for different reasons, often related to severity of the MI or other health‐related factors, including older age. Of those offered hospital‐based cardiac rehabilitation, not all choose to participate, perhaps because of practical reasons (such as living a long distance from the hospital or lack of interest). Thus, those investigated in studies of hospital or home‐based cardiac rehabilitation may constitute a selected subgroup. In addition, when entering a physical training program, such as cardiac rehabilitation, other parts of the activity pattern, such as everyday activity or hobbies, may be compensatorily decreased, leading to a status quo regarding total PA.24 Similarly, sedentary activity may increase again after the end of cardiac rehabilitation.25 Unfortunately, Hansen et al showed that the cardiovascular disease risk profile worsened significantly during long‐term follow‐up after cardiac rehabilitation.26 Therefore, focusing on all PA, regardless of context, may offer an important target for improved clinical secondary prevention post‐MI.
The relative intensity of the performed activities in the present study is unknown. The intensity of the PA performed may be of importance, since aerobic fitness has been shown to be an important predictor of survival, also post‐MI,27 and cardiac rehabilitation has been shown to increase aerobic fitness.28 However, both high‐intensity exercise and less‐intense continuous exercise have been shown to reduce CVD risk in cardiac patients,29 while Williams et al showed that walking had equal CVD‐risk‐reducing effects as running did in patients at high cardiac risk.22 Regarding frequency of PA, we showed that two 30‐minute sessions/wk of physical exercise, or an increase to that level within the first year post‐MI, were related to lowered mortality post‐MI, while 0 to 1 sessions/wk seems be too little. The lowered mortality related to activity may be even smaller, as self‐reported PA generally is higher than the levels found by more objective measures, such as accelerometry.30 Interestingly, these findings are consistent with the findings of Hansen et al, showing that a smaller exercise volume during phase II rehabilitation generated equal long‐term clinical benefits, compared with a greater exercise volume.26 Such findings may be associated with a lower compliance of greater exercise volumes and higher‐intensity activity.
Thus, the findings of the present study may have important clinical implications, since although universally recommended,10 PA is still underutilized as part of preventive and treatment strategies in health care. This is troublesome, since other commonly used components in secondary prevention, such as patient education, have been shown to be less efficient.15 The shown relation to survival, in patients who maintain or increase their level of PA post‐MI, reinforces the importance of the present guidelines and highlights the need for improved secondary prevention including the implementation of PA advice as part of regular postinfarction treatment. At present not enough is known regarding how to design effective counseling for increased PA among MI survivors, despite many studies. Promising initiatives and methods, such as PA on prescription (PAP) and Exercise is medicine (EiM), have been shown to increase the level of PA,31, 32 and may receive a large boost, as a result of the present findings, but need to be investigated further in patients with MI before it can be suggested to be an alternative to exercise‐based rehabilitation. Other interventions include different forms of automated feedback from wearable electronic devices. One such system has been tested in a randomized clinical trial study, reporting important changes in activity levels,33 although contradicting data have been published.34 Patients should receive counseling on PA after having an MI, and this could be offered as a continuation of, or as an alternative to, cardiac rehabilitation, when this is not available.
An obvious strength of the present study is the large sample size, and its representativeness of the whole Swedish MI population over 10 years. The large sample size allows us to perform subgroup analyses on important subgroups, as described above. In addition, the study took place in the 2000s, confirming the role of changes in PA for secondary prevention in the modern era of MI treatment, including a high rate of invasive treatment and effective medication for secondary prevention.
The mean follow‐up time is relatively short, possibly making the results sensitive to reverse causation. To investigate this, we undertook analyses with patients with a shorter follow‐up time than 2 years after admission is excluded (n=3424, 151 deaths). The main analyses were repeated and only limited and nonsignificant differences were noted, when applying formal testing.21 This indicated that the effect of reverse causation might be limited.
A limitation of the study is the exposure measure. The criterion‐related validity of the PA assessment in patients with MI is unknown. Furthermore, it does not include measures of sedentary behaviors and variations in intensity of the PA, which would have added to the study. However, the predictive validity of the question is strong, as shown by the present article. Another limitation is the possibility of residual confounding (ie, although measures were taken to control for important factors, there is a possibility that some variation was unmeasured). Also, we lack data on potential important socioeconomic variables. Yet another limitation is the absence of nutritional information. This was not included in the SWEDEHEART registry at the time of this study and therefore could not be accounted for.
Included and nonincluded patients differ in several aspects, as noted in the Results section. Included patients were generally less often smokers, had better eGFR, were less likely to have had a STEMI, and had a higher survival. Investigating a cohort biased to be healthier may lead to an underestimation of the effect of changes in PA. However, the absences of interaction between the variables in the full model and PA strata indicates that findings are generally robust across strata (ie, similar results among those with high/low eGFR, STEMI/NSTEMI, etc), with the exception of EF. Therefore, it is assumed that this bias is limited. As mentioned in the Results, PA strata differ in several aspects. It is possible that, despite both controlling for these differences and performing stratified analyses, being inactive serves as a proxy for MI severity or other ongoing illness. However, the similarities in the stratified analyses can be taken as an argument against this.
Three categories for exposure to smoking were used. A more precise measure, such as pack‐years, may have reduced possible residual confounding regarding this variable.
In conclusion, increased PA in the first year post‐MI is associated with a lower risk of subsequent death. This is the largest study to assess the effects of changes in PA post‐MI in the modern era of MI treatment, in a nationwide representative cohort. The results of the present study will have great clinical impact, highlighting the use of PA as part of regular secondary preventive measures after MI. Hopefully, we now have no excuses not to improve the adherence to existing guidelines on secondary prevention.
Sources of Funding
Ekblom and Ek were funded by ICA Sweden. There was no other specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
Disclosures
None.
Acknowledgments
This work was performed at the Swedish School of Sport and Health Sciences.
(J Am Heart Assoc. 2018;7:e010108 DOI: 10.1161/JAHA.118.010108.)
References
- 1. The National Board of Health and Welfare . Statistics on myocardial infarctions 2015. 2017.
- 2. Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord. 2017;17:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wijndaele K, Sharp SJ, Wareham NJ, Brage S. Mortality risk reductions from substituting screen time by discretionary activities. Med Sci Sports Exerc. 2017;49:1111–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Li J, Siegrist J. Physical activity and risk of cardiovascular disease—a meta‐analysis of prospective cohort studies. Int J Environ Res Public Health. 2012;9:391–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Miura Y, Fukumoto Y, Miura T, Shimada K, Asakura M, Kadokami T, Ando S, Miyata S, Sakata Y, Daida H, Matsuzaki M, Yasuda S, Kitakaze M, Shimokawa H. Impact of physical activity on cardiovascular events in patients with chronic heart failure. A multicenter prospective cohort study. Circ J. 2013;77:2963–2972. [DOI] [PubMed] [Google Scholar]
- 6. Yates T, Haffner SM, Schulte PJ, Thomas L, Huffman KM, Bales CW, Califf RM, Holman RR, McMurray JJ, Bethel MA, Tuomilehto J, Davies MJ, Kraus WE. Association between change in daily ambulatory activity and cardiovascular events in people with impaired glucose tolerance (NAVIGATOR trial): a cohort analysis. Lancet. 2014;383:1059–1066. [DOI] [PubMed] [Google Scholar]
- 7. Gorczyca AM, Eaton CB, LaMonte MJ, Manson JE, Johnston JD, Bidulescu A, Waring ME, Manini T, Martin LW, Stefanick ML, He K, Chomistek AK. Change in physical activity and sitting time after myocardial infarction and mortality among postmenopausal women in the Women's Health Initiative‐Observational Study. J Am Heart Assoc. 2017;6:e005354 DOI: 10.1161/JAHA.116.005354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Palmefors H, DuttaRoy S, Rundqvist B, Borjesson M. The effect of physical activity or exercise on key biomarkers in atherosclerosis—a systematic review. Atherosclerosis. 2014;235:150–161. [DOI] [PubMed] [Google Scholar]
- 9. Martinez DG, Nicolau JC, Lage RL, Toschi‐Dias E, de Matos LD, Alves MJ, Trombetta IC, Dias da Silva VJ, Middlekauff HR, Negrao CE, Rondon MU. Effects of long‐term exercise training on autonomic control in myocardial infarction patients. Hypertension. 2011;58:1049–1056. [DOI] [PubMed] [Google Scholar]
- 10. Piepoli MF, Hoes AW, Brotons C, Hobbs RFD, Corra U; Task Force for the guidelines on cardiovascular disease prevention in clinical p . Main messages for primary care from the 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur J Gen Pract. 2018;24:51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hansen D, Rovelo Ruiz G, Doherty P, Iliou MC, Vromen T, Hinton S, Frederix I, Wilhelm M, Schmid JP, Abreu A, Ambrosetti M, Garcia‐Porrero E, Coninx K, Dendale P; Group EEw . Do clinicians prescribe exercise similarly in patients with different cardiovascular diseases? Findings from the EAPC EXPERT working group survey. Eur J Prev Cardiol. 2018;25:682–691. DOI: 10.1177/2047487318760888. [DOI] [PubMed] [Google Scholar]
- 12. Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise‐based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta‐analysis. J Am Coll Cardiol. 2016;67:1–12. [DOI] [PubMed] [Google Scholar]
- 13. Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise‐based cardiac rehabilitation post‐myocardial infarction: a systematic review and meta‐analysis of randomized controlled trials. Am Heart J. 2011;162(571–584):e2. [DOI] [PubMed] [Google Scholar]
- 14. van Halewijn G, Deckers J, Tay HY, van Domburg R, Kotseva K, Wood D. Lessons from contemporary trials of cardiovascular prevention and rehabilitation: a systematic review and meta‐analysis. Int J Cardiol. 2017;232:294–303. [DOI] [PubMed] [Google Scholar]
- 15. Anderson L, Brown JP, Clark AM, Dalal H, Rossau HK, Bridges C, Taylor RS. Patient education in the management of coronary heart disease. Cochrane Database Syst Rev. 2017;6:CD008895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Steffen‐Batey L, Nichaman MZ, Goff DC Jr, Frankowski RF, Hanis CL, Ramsey DJ, Labarthe DR. Change in level of physical activity and risk of all‐cause mortality or reinfarction: the Corpus Christi Heart Project. Circulation. 2000;102:2204–2209. [DOI] [PubMed] [Google Scholar]
- 17. Jernberg T, Attebring MF, Hambraeus K, Ivert T, James S, Jeppsson A, Lagerqvist B, Lindahl B, Stenestrand U, Wallentin L. The Swedish Web‐system for enhancement and development of evidence‐based care in heart disease evaluated according to recommended therapies (SWEDEHEART). Heart. 2010;96:1617–1621. [DOI] [PubMed] [Google Scholar]
- 18. Hambraeus K, Tyden P, Lindahl B. Time trends and gender differences in prevention guideline adherence and outcome after myocardial infarction: data from the SWEDEHEART registry. Eur J Prev Cardiol. 2016;23:340–348. [DOI] [PubMed] [Google Scholar]
- 19. Sederholm Lawesson S, Alfredsson J, Szummer K, Fredrikson M, Swahn E. Prevalence and prognostic impact of chronic kidney disease in STEMI from a gender perspective: data from the SWEDEHEART register, a large Swedish prospective cohort. BMJ Open. 2015;5:e008188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, Swinburn P, Busschbach J. Measurement properties of the EQ‐5D‐5L compared to the EQ‐5D‐3L across eight patient groups: a multi‐country study. Qual Life Res. 2013;22:1717–1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Williams PT, Thompson PD. Increased cardiovascular disease mortality associated with excessive exercise in heart attack survivors. Mayo Clin Proc. 2014;89:1187–1194. [DOI] [PubMed] [Google Scholar]
- 23. Anderson L, Sharp GA, Norton RJ, Dalal H, Dean SG, Jolly K, Cowie A, Zawada A, Taylor RS. Home‐based versus centre‐based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6:CD007130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gomersall SR, Rowlands AV, English C, Maher C, Olds TS. The ActivityStat hypothesis: the concept, the evidence and the methodologies. Sports Med. 2013;43:135–149. [DOI] [PubMed] [Google Scholar]
- 25. Ter Hoeve N, Sunamura M, van Geffen ME, Fanchamps MH, Horemans HL, Bussmann JB, Stam HJ, van Domburg RT, van den Berg‐Emons RJ. Changes in physical activity and sedentary behavior during cardiac rehabilitation. Arch Phys Med Rehabil. 2017;98:2378–2384. [DOI] [PubMed] [Google Scholar]
- 26. Hansen D, Dendale P, Raskin A, Schoonis A, Berger J, Vlassak I, Meeusen R. Long‐term effect of rehabilitation in coronary artery disease patients: randomized clinical trial of the impact of exercise volume. Clin Rehabil. 2010;24:319–327. [DOI] [PubMed] [Google Scholar]
- 27. Barons MJ, Turner S, Parsons N, Griffiths F, Bethell H, Weich S, Thorogood M. Fitness predicts long‐term survival after a cardiovascular event: a prospective cohort study. BMJ Open. 2015;5:e007772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hannan AL, Hing W, Simas V, Climstein M, Coombes JS, Jayasinghe R, Byrnes J, Furness J. High‐intensity interval training versus moderate‐intensity continuous training within cardiac rehabilitation: a systematic review and meta‐analysis. Open Access J Sports Med. 2018;9:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Elliott AD, Rajopadhyaya K, Bentley DJ, Beltrame JF, Aromataris EC. Interval training versus continuous exercise in patients with coronary artery disease: a meta‐analysis. Heart Lung Circ. 2015;24:149–157. [DOI] [PubMed] [Google Scholar]
- 30. Ekblom O, Ekblom‐Bak E, Bolam KA, Ekblom B, Schmidt C, Soderberg S, Bergstrom G, Borjesson M. Concurrent and predictive validity of physical activity measurement items commonly used in clinical settings—data from SCAPIS pilot study. BMC Public Health. 2015;15:978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rodjer L, H Jonsdottir I, Borjesson M. Physical activity on prescription (PAP): self‐reported physical activity and quality of life in a Swedish primary care population, 2‐year follow‐up. Scand J Prim Health Care. 2016;34:443–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Börjesson M, Arvidsson D, Blomqvist Å, Daxberg E‐L, Jonsdottir IH, Lundqvist S, Mellén A, Onerup A, Perrson J, Sjögren P, Svanberg T, Jivegård L. Efficacy of the Swedish model for physical activity on prescription. Regional activity based HTA 2018. [DOI] [PubMed]
- 33. Martin SS, Feldman DI, Blumenthal RS, Jones SR, Post WS, McKibben RA, Michos ED, Ndumele CE, Ratchford EV, Coresh J, Blaha MJ. mActive: a randomized clinical trial of an automated mHealth intervention for physical activity promotion. J Am Heart Assoc. 2015;4:e002239 DOI: 10.1161/JAHA.115.002239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Maddison R, Pfaeffli L, Whittaker R, Stewart R, Kerr A, Jiang Y, Kira G, Leung W, Dalleck L, Carter K, Rawstorn J. A mobile phone intervention increases physical activity in people with cardiovascular disease: results from the HEART randomized controlled trial. Eur J Prev Cardiol. 2015;22:701–709. [DOI] [PubMed] [Google Scholar]


