Abstract
Background
While prior studies have linked the neighborhood environment and development of subclinical atherosclerosis, it is unknown whether living in neighborhoods with greater availability of “unhealthy” food outlets (fast‐food chain restaurants and convenience stores) is associated with risk of developing coronary artery calcification (CAC).
Methods and Results
We included 2706 CARDIA study (Coronary Artery Risk Development in Young Adults) participants who underwent CAC measurement during follow‐up years 15 (2000–2001), 20 (2005–2006), and 25 (2010–2011). Neighborhood features examined included percentage of all food outlets that were convenience stores and fast‐food chain restaurants within a 3‐km Euclidean buffer distance from each participant's residence. Econometric fixed effects models, which by design control for all time‐invariant covariates, were used to model the longitudinal association between simultaneous within‐person change in percentage food outlet and change in CAC. At baseline (year 15), 9.7% of participants had prevalent CAC. During 10 years of follow‐up, 21.1% of participants developed CAC. Each 1‐SD increase in percentage of convenience stores was associated with a 1.34 higher odds of developing CAC (95% CI: 1.04, 1.72) after adjusting for individual‐ and neighborhood‐level covariates; however, there was no significant association between increased percentage of fast‐food chain restaurants and developing CAC (odds ratio=1.15; 95% CI: 0.96, 1.38). There were no significant associations between increases in either food outlet percentage and progression of CAC.
Conclusions
Our findings suggest that increases in the relative availability of convenience stores in participants' neighborhoods is related to the development of CAC over time.
Keywords: atherosclerosis, coronary artery calcification, neighborhood
Subject Categories: Epidemiology
Clinical Perspective
What Is New?
This article investigates whether neighborhood fast‐food chain restaurants and convenience stores are associated with development of subclinical atherosclerosis in the CARDIA (Coronary Artery Risk Development in Young Adults) study.
Fixed effects models are used to determine how changes in concentration of these outlets influences the development of coronary artery calcification.
What Are the Clinical Implications?
A better understanding of the relationships between neighborhood environments and cardiovascular disease risk will help physicians address the root causes underlying poor health outcomes in their patients.
The findings supports public health efforts to establish multilevel policies to prevent cardiovascular disease.
Introduction
Previous studies have reported that neighborhood socioeconomic deprivation is associated with the development of subclinical atherosclerosis.1, 2, 3, 4, 5 Some research suggests the neighborhood food environment could account for these relationships by limiting access to healthy foods.6 The neighborhood food environment could also be an indicator of economic investment in a neighborhood.7 Previous research suggests that more socioeconomically disadvantaged neighborhoods have a greater density of convenient food outlet options than more affluent neighborhoods,6, 8 and thus the food environment could serve as a proxy for a variety of factors related to neighborhood disadvantage and atherosclerosis independent of diet including employment, crime, and political capital.7, 9, 10, 11 However, few studies have examined relationships of the neighborhood food environment with subclinical atherosclerosis.12
Another limitation of the existing literature is that most studies have measured features of the neighborhood food environment at a single point in time.4, 5, 13 A recent study found that improvements in access to neighborhood healthy food stores are related to decreases in subclinical atherosclerosis, as measured by coronary artery calcification (CAC).12 However, the impact of greater access to neighborhood stores that sell unhealthy food and other substances on development of CAC has yet to be studied. Previous research suggests reducing access to unhealthy foods, such as those sold in fast food outlets and convenience stores, may have a greater impact on reducing obesity than focusing solely on increasing access to healthy food options.14, 15, 16 Assessing the role of obesogenic neighborhood food environments in the development of atherosclerosis will help improve our understanding of the mechanisms through which place influences cardiovascular disease risk.
In this study, we investigated whether 2 “unhealthy” features of the neighborhood food environment, fast‐food chain restaurants and convenience stores, were related to the development of CAC independent of neighborhood poverty in participants of the CARDIA (Coronary Artery Risk Development in Young Adults) Study over a 10‐year period from 2000 to 2001 to 2010 to 2011. Fast‐food outlet and convenience store density have been previously hypothesized to be linked to higher cardiovascular risk.17 Using fixed effects models, we separately investigated whether within‐person increases in the percentage of all food outlets that were convenience stores and fast food chain restaurants were associated with the development of CAC and increases in CAC levels over time. Understanding whether changes in the relative availability of fast‐food chain restaurants and convenience stores are related to the development of subclinical atherosclerosis has important implications for policy‐level interventions designed to reduce health disparities by improving access to health‐promoting resources.
Methods
The data, analytic methods, and study materials are available to other researchers for purposes of reproducing the results or replicating the procedure from the CARDIA Coordinating Center.18 CARDIA complies with data‐sharing requirements of the National Institutes of Health by providing limited‐access data sets from various CARDIA examinations to the National Heart, Lung and Blood Institute bioLINCC.19
Study Population and Study Variables
The CARDIA Study is a prospective, multicenter, cohort study investigating predictors of the development of coronary heart disease risk factors in young adults.20 At the initial examination in 1985 to 1986, the cohort consisted of 5115 black and white men and women aged 18 to 30 years recruited from 4 field centers in the following US urban areas: Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California. In each area, the recruitment goal was to enroll adults in approximately equal numbers of women and men, blacks and whites, people aged <25 years and ≥25 years, as well as people with a high school education or less and people with more than a high school education. Follow‐up examinations took place 2, 5, 7, 10, 15, 20, 25, and 30 years later. CARDIA participants provided written informed consent at each examination, and the study was approved by institutional review boards at each of the study centers.
We restricted our analysis to the time period between examination year 15 (baseline) and the following 2 examination years, when the primary outcome CAC was measured in CARDIA. For this analysis, we included CARDIA participants who had a CAC scan at baseline and either/both of the 5‐ and 10‐year follow‐up examinations and who did not have a history of cardiovascular disease (n=2753). We excluded 47 participants who were missing geocoded food environment information. In total, 2706 participants (52.9% of CARDIA participants) met the study criteria for the analysis.
Exposures
CARDIA participant residential addresses at the time of each examination were geocoded. Data on food resources at the time of each examination were obtained from Dun and Bradstreet, a commercial data set of US businesses, according to 8‐digit Standard Industrial Classification (SIC) codes. Business establishments are assigned 4‐digit SIC codes by the US government to designate the primary line of business of the establishment; private data companies such as Dun and Bradstreet assign them 8‐digit SIC codes to further classify industries. Based on previous research, the total count of food resources, overall and by type, were calculated within a 3‐km Euclidean buffer distance from each participant's residential location.21, 22
We focused on 2 commonly studied “unhealthy” food outlets: fast‐food chain restaurants (eg, McDonald's or Pizza Hut and convenience stores including gasoline stations with convenience stores eg, 7‐Eleven or Mobil Mart). Within the 3‐km radius, we calculated separately the percentage of fast‐food chain restaurants and convenience stores relative to all food outlet options. This provided a measure of the prevalence of fast‐food chain restaurants and convenience stores relative to the larger neighborhood retail food environment, contextualizing absolute number of fast‐food chain stores and convenience stores within the total number of available options. Table 1 shows the SIC codes included in this study. Fast‐food chain stores and convenience stores were classified using the more specific 8‐digit SIC codes. The total set of food outlet options mainly comprises the more general 4‐digit SIC codes, as well as two 8‐digit SIC codes: country general stores within the category of miscellaneous general merchandise stores (4‐digit SIC code 5399) and food cooperatives within the category of membership organizations not elsewhere classified (SIC code 8699).
Table 1.
Detailed Food Store and Restaurant Types Based on 4‐ or 8‐Digit SIC Codes
| Food Resource Type | Description | SIC |
|---|---|---|
| Fast‐food chain restaurant | Fast‐food restaurant, chain | 58120307 |
| Pizzeria, chain | 58120601 | |
| Convenience stores | Variety stores | 53310000 |
| Convenience stores | 54110200 | |
| Convenience stores, chain | 54110201 | |
| Convenience stores, independent | 54110202 | |
| Gasoline service stations | 55410000 | |
| Gasoline service stations, not elsewhere classified | 55419900 | |
| Filling stations, gasoline | 55419901 | |
| All food outlet options | Retail, grocery stores | 5411 |
| Retail, food stores | 5400 | |
| Eating places | 5812 | |
| Retail bakeries | 5461 | |
| Miscellaneous food stores | 5499 | |
| Dairy products stores | 5451 | |
| Candy, nut, and confectionary stores | 5441 | |
| Fruit and vegetable markets | 5431 | |
| Meat and fish (seafood) markets | 5421 | |
| Country general stores | 53999903 | |
| Food cooperatives | 86999907 |
SIC indicates Standard Industrial Classification.
Outcome
CAC was measured at examination years 15, 20, and 25 using a standardized protocol.23 At examination years 15 and 20, CAC was measured in the coronary arteries (left main, left circumflex, left anterior descending, and right) using 2 computed tomography (CT) scans taken 1 to 2 minutes apart, using either electron‐beam CT or multidetector CT scanners. At examination year 25, given the high reproducibility at previous examinations, a single CT scan was performed using only multidetector scanners. For all examinations, CT images were transmitted to a central reading center where CAC was quantified in 2.5‐ to 3.0‐mm‐thick images by experienced, highly trained technicians and discordant scan pairs were adjudicated by an expert cardiovascular radiologist.24 A total CAC score in Agatston units was calculated by summing the scores of all lesions within the coronary arteries. We defined presence of CAC (yes/no) as a total Agatston score >0, and also assessed CAC as a continuous variable based on the total Agatston score. Because CAC score distribution is highly skewed, we log‐transformed the nonzero CAC scores to model progression of CAC as approximately normally distributed.
Covariates
Race was self‐reported as black or white. Highest level of educational attainment was categorized as ≤12 years (representing ≤high school degree), 13 to 16 years (representing college degree, associate's degree, or some college), and ≥17 years (representing>college degree, such as MD, JD, PhD, MSc). Annual household income was categorized as <$16 000, $16 000 to 34 999, $35 000 to 49 999, $50 000 to 74 999, $75 000 to 99 999, and ≥$100 000. Sex was self‐reported as male or female.
We included 4 self‐reported measures of health behavior: weekly fast‐food consumption ≥2 times per week (yes/no), current cigarette smoking (yes/no), alcohol consumption (never/moderate/heavy), and physical activity, converted to standardized exercise units based on frequency and intensity of participation in 13 categories of moderate and vigorous recreational sports, exercise, leisure, and occupational activities.24 We also included 4 self‐reported measures of cardiovascular disease risk factors: hypertension (yes/no), hypercholesterolemia (yes/no), diabetes mellitus (yes/no), and body mass index (kg/m2) derived from measured height and weight. Resting systolic and diastolic blood pressure were measured at three 1‐minute intervals using random zero sphygmomanometers and reported as the average of the second and third measurements. Hypertension was determined by either use of antihypertensive medication or measured systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg.25 Participants also underwent a venipuncture blood draw after a minimum fast of 8 hours. Hypercholesterolemia was determined by use of cholesterol medication or fasting plasma cholesterol concentration ≥240 mg/dL.26 Participants were considered diabetic if they reported taking diabetes mellitus medication or had a fasting glucose concentration ≥126 mg/dL.27 Body mass index was derived from weight and height (kg/m2), measured by certified technicians.
Three neighborhood‐level covariates were included in models. Neighborhood poverty was calculated as the proportion of the population within the participant's census tract living in poverty. Population density of the participant's census tract (total people per square mile) was categorized into approximate tertiles: <2500, 2500 to 7500, and >7500. Total food resource count within a 3‐km Euclidean distance was categorized into approximate tertiles: <75 resources, 75 to 200 resources, and >200 resources.
Statistical Methods
We first compared baseline characteristics between those who had prevalent CAC, those who developed CAC during follow‐up, and those who did not develop CAC. We then used fixed effects models to model the associations of within‐person change in percentage of convenience stores and fast‐food chain stores with the development of CAC in those without CAC at baseline. We also used fixed effects models to relate changes in percentage of convenience stores and fast‐food chain stores to change in level of CAC among those with prevalent CAC at baseline. Fixed effect models examine within‐person change, adjusting by design for all measured and unmeasured time‐invariant confounding. We modeled change in percentage of convenience stores and fast‐food chain stores as SD change (10% and 3%, respectively). We used logistic regression to determine the odds ratio of within‐person CAC development, and linear regression to model within‐person changes in the log‐transformed CAC score. We used a sequential covariate adjustment strategy for both outcomes, first adjusting for baseline sociodemographic characteristics, population density, total food resource density, and neighborhood poverty (model 1), then incorporating health behaviors (model 2), and finally adjusting for cardiovascular disease risk factors (model 3). We also tested for interactions of percentage food outlet with CARDIA field center to determine whether associations varied by site. Missing covariate data were multiply imputed (10 times) by chained equations. Table 2 shows the number of participants missing data on each study covariate. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
Table 2.
Number of Participants Missing Data on Each Study Covariate
| Characteristic | Baseline | 5‐Year Follow‐Up | 10‐Year Follow‐Up |
|---|---|---|---|
| Education | 2 | 140 | 190 |
| Annual household income | 29 | 167 | 212 |
| Fast‐food consumption | 272 | 754 | 208 |
| Cigarette smoking | 6 | 150 | 215 |
| Alcohol consumption | 2 | 186 | 204 |
| Physical activity | 4 | 142 | 200 |
| Body mass index | 6 | 135 | 188 |
| Hypertension | 4 | 132 | 188 |
| Hypercholesterolemia | 32 | 148 | 192 |
| Diabetes mellitus | 187 | 303 | 258 |
Results
The mean age of participants with prevalent CAC at baseline was 41.8 years (Table 3). Participants with prevalent CAC were more likely to be men (69.8%) and white (64.9%). These individuals had lower levels of education and income than those without prevalent CAC and were more likely to have hypertension, hypercholesterolemia, and diabetes mellitus.
Table 3.
Characteristics of CARDIA Study Participants by Timing of CAC Development, 2000/2001
| Characteristic | Prevalent CAC at Baseline (Year 15) (n=262) | Developed CAC During Follow‐Up (Year 20/Year 25) (n=570) | Did Not Develop CAC During Follow‐Up (n=1874) | |||
|---|---|---|---|---|---|---|
| Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | |
| Age, y | 41.8 (0.2) | 40.8 (0.1) | 40.0 (0.08) | |||
| Sex | ||||||
| Male | 69.8 | 61.0 | 36.0 | |||
| Female | 30.2 | 39.0 | 64.0 | |||
| Race | ||||||
| Black | 35.1 | 43.9 | 45.6 | |||
| White | 64.9 | 56.1 | 54.4 | |||
| Field center | ||||||
| Birmingham, AL | 22.1 | 23.0 | 23.1 | |||
| Chicago, IL | 23.3 | 26.5 | 24.4 | |||
| Minneapolis, MN | 29.0 | 25.8 | 24.1 | |||
| Oakland, CA | 25.6 | 24.7 | 28.4 | |||
| Education | ||||||
| High school or less | 29.0 | 21.6 | 19.3 | |||
| Some college/college | 51.9 | 58.5 | 57.7 | |||
| Graduate school | 19.1 | 19.9 | 23.0 | |||
| Annual household income ($) | ||||||
| <16 000 | 10.5 | 7.4 | 7.7 | |||
| 16 000 to 34 999 | 15.4 | 15.4 | 14.7 | |||
| 35 000 to 49 999 | 19.3 | 16.9 | 15.5 | |||
| 50 000 to 74 999 | 18.3 | 20.2 | 23.2 | |||
| 75 000 to 99 999 | 16.5 | 15.3 | 15.1 | |||
| ≥100 000 | 20.0 | 24.8 | 23.8 | |||
| Fast‐food consumption ≥2 times per wk | 35.2 | 45.7 | 36.2 | |||
| Current cigarette smoker | 32.1 | 26.0 | 16.8 | |||
| Alcohol consumption | ||||||
| Never | 19.7 | 22.1 | 20.0 | |||
| Moderate | 70.8 | 73.3 | 75.6 | |||
| Heavy | 9.5 | 4.6 | 4.4 | |||
| Physical activity | 402.6 (18.9) | 352.6 (11.5) | 345.3 (6.4) | |||
| Body mass index, kg/m2 | 29.3 (0.4) | 30.0 (0.3) | 27.9 (0.1) | |||
| Hypertension | 28.0 | 21.4 | 11.1 | |||
| Hypercholesterolemia | 20.2 | 11.0 | 5.3 | |||
| Diabetes mellitus | 7.8 | 5.1 | 2.2 | |||
CAC was measured using the Agatston score. Any score >0 indicates presence of CAC. CAC indicates coronary artery calcium; CARDIA, Coronary Artery Risk Development in Young Adults Study.
Over follow‐up more men than women, participants with lower levels of education, and smokers developed CAC. More participants with hypertension, hypercholesterolemia, and diabetes mellitus than those without these cardiovascular disease risk factors developed CAC. There was no age difference between those who did and did not develop CAC.
There were no differences in levels of neighborhood poverty, total food resource density, or population density by development of CAC (Table 4). There was a larger percentage of neighborhood convenience stores among those who developed CAC (16.4% mean percentage convenience store in those who developed CAC versus 15.8% in those who did not develop CAC). However, the mean percentage of fast‐food chain restaurants in a given neighborhood was the same for those who did and did not develop CAC (4.2%).
Table 4.
Baseline Measures of the Neighborhood Environment of CARDIA Study Participants by Timing of CAC Development, 2000/2001
| Characteristic | Prevalent CAC at Baseline (Year 15) (n=262) | Developed CAC During Follow‐up (n=570) | Did Not Develop CAC During Follow‐up (n=1874) | |||
|---|---|---|---|---|---|---|
| Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | |
| Neighborhood povertya | 12.2 (0.7) | 11.9 (0.5) | 12.3 (0.3) | |||
| Population density | ||||||
| <2500 people per sq mi | 26.3 | 28.4 | 31.0 | |||
| 2500 to 7500 people per sq mi | 36.7 | 35.6 | 33.9 | |||
| >7500 people per sq mi | 37.0 | 36.0 | 35.1 | |||
| Total food outlet count within 3 kmb | ||||||
| <75 resources | 25.2 | 30.7 | 32.0 | |||
| 75–200 resources | 40.1 | 34.3 | 33.6 | |||
| >200 resources | 34.7 | 35.0 | 34.4 | |||
| Food outlet percentagec | ||||||
| Convenience stores | 14.6 (0.5) | 16.4 (0.5) | 15.8 (0.2) | |||
| Fast‐food chain restaurants | 3.8 (0.2) | 4.2 (0.1) | 4.2 (0.08) | |||
CAC was measured using the Agatston score. Any score >0 indicates presence of CAC. CAC indicates coronary artery calcium; CARDIA, Coronary Artery Risk Development in Young Adults Study.
Neighborhood poverty measured as percent of individuals living under 100% of the federal poverty level within the participant's census tract of residence.
Total food outlet count includes fast‐food chain restaurants, sit‐down restaurants, supermarkets, and convenience stores.
Measured as the percentage of a specific food resource count relative to the total food resource count in a 3‐km Euclidean distance from the participant's residence.
Overall percentage of convenience stores was similar at baseline and 5‐year follow‐up, but declined over the next 5‐year follow‐up period (mean difference −1.9%, 95% CI: −1.5%, −2.2%; Figure). Overall percentage of fast‐food chain restaurants increased from baseline to the first 5‐year follow‐up (mean difference 2.3%, 95% CI: 2.2%, 2.5%), but remained similar over the next follow‐up period. About 55% of the sample moved to a different neighborhood at least once during follow‐up, but the changes in total number of food outlets were similar in those who did or did not move.
Figure 1.
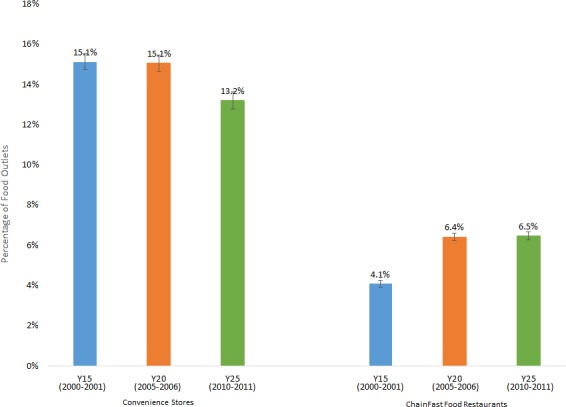
Percentage of all food outlets that are convenience stores and fast‐food chain restaurants by year and outlet type.
In the fixed effects model adjusting for time‐varying sociodemographic and geographic covariates, each SD increase in percentage convenience store participants were exposed to over follow‐up was associated with a 1.34 higher within‐person odds of developing CAC (Table 5; 95% CI: 1.04–1.73). Each SD increase in the percentage of fast‐food chain restaurants was associated with a 1.13 higher odds of developing CAC (95% CI: 0.94–1.36). These associations remained similar in magnitude after additional adjustment for health behaviors and cardiovascular disease risk factors. These associations did not vary significantly by site (P for interaction >0.4).
Table 5.
Within‐Person Odds of Developing CAC Associated With a 1‐SD Within‐Person Increase in Percentage of All Food Outlets That Are Convenience Stores or Fast‐Food Chain Restaurantsa
| Model 1b | Model 2c | Model 3d | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P value | OR (95% CI) | P Value | |
| Food outlet percentagee | ||||||
| Convenience stores | 1.34 (1.04–1.73) | 0.02 | 1.32 (1.03–1.71) | 0.03 | 1.34 (1.04–1.72) | 0.02 |
| Fast‐food chain restaurants | 1.13 (0.94–1.36) | 0.18 | 1.13 (0.94–1.36) | 0.18 | 1.15 (0.96–1.38) | 0.14 |
CAC indicates coronary artery calcium; OR, odds ratio.
All estimates are derived from fixed effects models. Each food resource type is investigated in a separate model. CAC was measured using the Agatston score. Any score >0 indicates presence of CAC.
Model 1: adjusted for age, age×race, and age×sex, income, population density, total food outlet density, and neighborhood poverty.
Model 2: adjusted as in model 1 plus physical activity, cigarette smoking status, alcohol consumption, and weekly fast‐food consumption.
Model 3: adjusted as in model 2 plus body mass index, hypertension, hypercholesterolemia, and diabetes mellitus.
Measured as the percentage of a specific food outlet count relative to the total food outlet count in a 3‐km Euclidean distance from the participant residence. Higher scores represent more unhealthy outlets: 1 SD of percentage of convenience stores=0.10, and 1 SD of percentage of fast‐food chain restaurants=0.03.
Among people with nonzero levels of CAC, a 1 SD increase in percentage of convenience stores and fast‐food chain restaurants did not significantly change the within‐person CAC score progression. In models fully adjusted for sociodemographics, geographic characteristics, health behaviors, and cardiovascular disease risk factors, each SD increase in percentage convenience store resulted in a 3.0% decrease in within‐person CAC (Table 6; −0.15 to 0.089), and each SD increase in percentage fast‐food chain restaurants resulted in a 3.2% decrease in within‐person CAC (−0.1 to 0.037). These associations did not vary significantly by site (P for interaction >0.3).
Table 6.
Mean Within‐Person Differences in CAC Associated With a 1‐SD Within‐Person Increase in Percentage of All Food Outlets That Are Convenience Stores or Fast‐Food Chain Restaurants, Among People with Measurable CACa
| Model 1b | Model 2c | Model 3d | ||||
|---|---|---|---|---|---|---|
| B (95% CI) | P Value | B (95% CI) | P Value | B (95% CI) | P Value | |
| Unhealthy food outlet percentagee | ||||||
| Convenience stores | −0.026 (−0.139 to 0.087) | 0.65 | −0.027 (−0.146 to 0.091) | 0.64 | −0.030 (−0.150 to 0.089) | 0.61 |
| Fast‐food chain restaurant | −0.033 (−0.097 to 0.032) | 0.32 | −0.033 (−0.101 to 0.035) | 0.33 | −0.032 (−0.100 to 0.037) | 0.35 |
CAC indicates coronary artery calcium.
All estimates are derived from fixed effects models. Each food resource type is investigated in a separate model. CAC was measured using the Agatston score. Any score >0 indicates presence of CAC.
Model 1: adjusted for age, age×race, and age×sex, income, population density, total food outlet density, and neighborhood poverty.
Model 2: adjusted as in model 1 plus physical activity, cigarette smoking status, alcohol consumption, and weekly fast‐food consumption.
Model 3: adjusted as in model 2 plus body mass index, hypertension, hypercholesterolemia, and diabetes mellitus.
Measured as the specific unhealthy food outlet count relative to the total food outlet count in a 3‐km Euclidean distance from the participant residence. Higher scores represent more unhealthy outlets: 1 SD of percentage of convenience stores=0.10, and 1 SD of percentage of fast‐food chain restaurants=0.03.
Discussion
In this study, we found that increases in the percentage of convenience stores were related to increases in CAC after adjustment for several individual‐ and neighborhood‐level covariates including neighborhood poverty. The direction of the association was the same for percentage of fast‐food chain restaurants, but the association was smaller in magnitude and not statistically significant. Although a number of studies have linked neighborhood characteristics to the development of subclinical atherosclerosis,1, 2, 3, 4, 5, 12 we are aware of no studies that have investigated longitudinal associations of fast‐food chain restaurants and convenience stores with the development of CAC.
The differential findings for fast‐food chain restaurants and convenience stores suggest the pathways through which food outlets influence CAC are broader than food availability. Previous research has shown that less nutritious snacks were more widely advertised, had better placement in stores, and were provided in a more consistent and extensive selection than healthy foods in convenience stores.28 However, findings relating fast‐food chain restaurants and convenience stores to diet and body mass index are mixed.6, 29, 30, 31, 32 In addition, there is growing evidence suggesting that unhealthy food is ubiquitous and that consumption is not limited to unhealthy food outlets.33, 34 This may explain why changes in fast‐food chain restaurants were not associated with CAC. This also suggests that unhealthy food availability is not the sole pathway linking convenience store outlets to CAC development.
There are other pathways through which convenience store concentration could impact CAC development. One is through the unhealthy nonfood items sold in convenience stores that are also associated with CAC, including cigarettes and alcohol. It is possible that higher availability of these items, rather than or in addition to unhealthy foods and sugar‐sweetened beverages, may be driving this association. Our findings persisted with adjustment for within‐person changes in a variety of health behaviors including smoking, alcohol use, and fast‐food consumption, suggesting that further work is needed to better understand whether and how the increased presence of these stores influences individual health behaviors.
A relative increase in convenience stores over time could also be an indicator of economic disinvestment, which could influence CAC development by increasing unemployment and crime, and by decreasing social cohesion.7, 9, 10, 11 Previous research in CARDIA has shown that lower‐income neighborhoods are more likely to gain convenience stores over time than higher‐income neighborhoods.35 Our findings for convenience stores persisted with adjustment for neighborhood poverty, but there are other, harder to measure, social and economic forces that influence where different types of retail stores will open such as gentrification, crime, or social capital.
A major strength of this study is that our use of fixed effects models allowed us to investigate whether a within‐person change in neighborhood food environment was related to a within‐person change in CAC while tightly adjusting for time‐invariant confounders, even those that were not measured in this study. Additionally, we adjusted for several time‐varying individual‐ and neighborhood‐level confounders. Another strength is that we included a diverse sample of participants living across the United States.
Our study is not without limitations. Although fixed effects models account for any unmeasured time‐invariant confounding, they do not account for unmeasured time‐varying confounding. Thus, we cannot account for factors such as changing preferences that may influence residential relocation and CAC risk. Additionally, electronic business record data (eg, Dun and Bradstreet) are susceptible to geospatial inaccuracy and misclassification.36 Furthermore, since data are lacking on the contents sold at convenience stores, another limitation is that we assume the types of products that are available are consistent over the follow‐up period.
Overall, the results from this longitudinal study provide new evidence that greater access to neighborhood convenience stores may contribute to the development of subclinical atherosclerosis in middle‐aged adults. This supports the notion that cardiovascular health depends not only on the behavioral and biological characteristics of individuals but also on the environments where people live. However, further work is needed to determine the mechanisms linking increases in convenience store concentration to CAC development (ie, whether they are a proxy for other adverse changes in neighborhood conditions or indicative of unhealthy changes in individual‐level behaviors associated) in order to better facilitate the development of effective multilevel policies to prevent cardiovascular disease.
Sources of Funding
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute (NHLBI), the Intramural Research Program of the National Institute on Aging (NIA), and an intra‐agency agreement between NIA and NHLBI (AG0005). The development of neighborhood measures used in this research was supported by grants R01HL104580 & R01HL114091.
Disclosures
None.
(J Am Heart Assoc. 2019;8:e010586 DOI: 10.1161/JAHA.118.010586.)
References
- 1. Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. [DOI] [PubMed] [Google Scholar]
- 2. Winkleby M, Sundquist K, Cubbin C. Inequities in CHD incidence and case fatality by neighborhood deprivation. Am J Prev Med. 2007;32:97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Murray ET, Diez Roux AV, Carnethon M, Lutsey PL, Ni H, O'Meara ES. Trajectories of neighborhood poverty and associations with subclinical atherosclerosis and associated risk factors: the multi‐ethnic study of atherosclerosis. Am J Epidemiol. 2010;171:1099–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dragano N, Hoffmann B, Stang A, Moebus S, Verde PE, Weyers S, Mohlenkamp S, Schmermund A, Mann K, Jockel KH, Erbel R, Siegrist J. Subclinical coronary atherosclerosis and neighbourhood deprivation in an urban region. Eur J Epidemiol. 2009;24:25–35. [DOI] [PubMed] [Google Scholar]
- 5. Kim D, Diez Roux AV, Kiefe CI, Kawachi I, Liu K. Do neighborhood socioeconomic deprivation and low social cohesion predict coronary calcification?: the CARDIA study. Am J Epidemiol. 2010;172:288–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rummo PE, Meyer KA, Boone‐Heinonen J, Jacobs DR Jr, Kiefe CI, Lewis CE, Steffen LM, Gordon‐Larsen P. Neighborhood availability of convenience stores and diet quality: findings from 20 years of follow‐up in the Coronary Artery Risk Development in Young Adults study. Am J Public Health. 2015;105:e65–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bader MD, Schwartz‐Soicher O, Jack D, Weiss CC, Richards CA, Quinn JW, Lovasi GS, Neckerman KM, Rundle AG. More neighborhood retail associated with lower obesity among New York City public high school students. Health Place. 2013;23:104–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lamichhane AP, Warren JL, Peterson M, Rummo P, Gordon‐Larsen P. Spatial‐temporal modeling of neighborhood sociodemographic characteristics and food stores. Am J Epidemiol. 2015;181:137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wilson WJ. When Work Disappears: The World of the New Urban Poor. New York: Knopf: Distributed by Random House, Inc.; 1996. [Google Scholar]
- 10. Jacobs J. The Death and Life of Great American Cities. New York: Random House; 1961. [Google Scholar]
- 11. LaVeist TA. The political empowerment and health status of African‐Americans: mapping a new territory. Am J Sociol. 1992;97:1080–1095. [Google Scholar]
- 12. Wing JJ, August E, Adar SD, Dannenberg AL, Hajat A, Sanchez BN, Stein JH, Tattersall MC, Diez Roux AV. Change in neighborhood characteristics and change in coronary artery calcium: a longitudinal investigation in the MESA (Multi‐Ethnic Study of Atherosclerosis) cohort. Circulation. 2016;134:504–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sundquist K, Theobald H, Yang M, Li X, Johansson SE, Sundquist J. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Soc Sci Med. 2006;62:2061–2071. [DOI] [PubMed] [Google Scholar]
- 14. Cooksey‐Stowers K, Schwartz MB, Brownell KD. Food swamps predict obesity rates better than food deserts in the United States. Int J Environ Res Public Health.2017;14:E1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cohen DA, Sturm R, Scott M, Farley TA, Bluthenthal R. Not enough fruit and vegetables or too many cookies, candies, salty snacks, and soft drinks? Public Health Rep. 2010;125:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mayne SL, Auchincloss AH, Michael YL. Impact of policy and built environment changes on obesity‐related outcomes: a systematic review of naturally occurring experiments. Obes Rev. 2015;16:362–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80:569–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. University of Alabama at Birmingham . CARDIA Study contact information. Available at: http://www.cardia.dopm.uab.edu/contact-cardia. Accessed January 3, 2019.
- 19. National Institutes of Health . NHLBI Biologic Specimen and Data Repository Information Coordinating Center. Available at: https://biolincc.nhlbi.nih.gov/home/. Accessed January 3, 2019.
- 20. Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. [DOI] [PubMed] [Google Scholar]
- 21. Boone‐Heinonen J, Gordon‐Larsen P, Kiefe CI, Shikany JM, Lewis CE, Popkin BM. Fast food restaurants and food stores: longitudinal associations with diet in young to middle‐aged adults: the CARDIA study. Arch Intern Med. 2011;171:1162–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Richardson AS, Meyer KA, Howard AG, Boone‐Heinonen J, Popkin BM, Evenson KR, Kiefe CI, Lewis CE, Gordon‐Larsen P. Neighborhood socioeconomic status and food environment: a 20‐year longitudinal latent class analysis among CARDIA participants. Health Place. 2014;30:145–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carr JJ, Nelson JC, Wong ND, McNitt‐Gray M, Arad Y, Jacobs DR Jr, Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac ct in population‐based studies: standardized protocol of Multi‐Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. [DOI] [PubMed] [Google Scholar]
- 24. Jacobs DR Jr, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and reliability of short physical activity history: CARDIA and the Minnesota Heart Health Program. J Cardiopulm Rehabil. 1989;9:448–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 26. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) . Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 27. American Diabetes Association . Standards of medical care in diabetes–2013. Diabetes Care. 2013;36(suppl 1):S11–S66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gebauer H, Laska MN. Convenience stores surrounding urban schools: an assessment of healthy food availability, advertising, and product placement. J Urban Health. 2011;88:616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rummo PE, Guilkey DK, Ng SW, Meyer KA, Popkin BM, Reis JP, Shikany JM, Gordon‐Larsen P. Understanding bias in relationships between the food environment and diet quality: the Coronary Artery Risk Development in Young Adults (CARDIA) study. J Epidemiol Community Health. 2017;71:1185–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rummo PE, Guilkey DK, Ng SW, Meyer KA, Popkin BM, Reis JP, Shikany JM, Gordon‐Larsen P. Does unmeasured confounding influence associations between the retail food environment and body mass index over time? The Coronary Artery Risk Development in Young Adults (CARDIA) study. Int J Epidemiol. 2017;46:1456–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zenk SN, Tarlov E, Wing C, Matthews SA, Jones K, Tong H, Powell LM. Geographic accessibility of food outlets not associated with body mass index change among veterans, 2009–14. Health Aff (Millwood). 2017;36:1433–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18:1172–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vaughan CA. Where do food desert residents buy most of their junk food? Supermarkets Public Health Nutr. 2017;20:2608–2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. An R, Maurer G. Consumption of sugar‐sweetened beverages and discretionary foods among US adults by purchase location. Eur J Clin Nutr. 2016;70:1396–1400. [DOI] [PubMed] [Google Scholar]
- 35. Rummo PE, Guilkey DK, Ng SW, Popkin BM, Evenson KR, Gordon‐Larsen P. Beyond supermarkets: food outlet location selection in four U.S. Cities over time. Am J Prev Med. 2017;52:300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bader MD, Ailshire JA, Morenoff JD, House JS. Measurement of the local food environment: a comparison of existing data sources. Am J Epidemiol. 2010;171:609–617. [DOI] [PMC free article] [PubMed] [Google Scholar]


