Abstract
Background
We aimed to determine the change in treatment strategies and times to treatment over the first 5 years of the Mission: Lifeline program.
Methods and Results
We assessed pre‐ and in‐hospital care and outcomes from 2008 to 2012 for patients with ST‐segment–elevation myocardial infarction at US hospitals, using data from the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network Registry—Get With The Guidelines Registry. In‐hospital adjusted mortality was calculated including and excluding cardiac arrest as a reason for primary percutaneous coronary intervention delay. A total of 147 466 patients from 485 hospitals were analyzed. There was a decrease in the proportion of eligible patients not treated with reperfusion (6.2% versus 3.3%) and treated with fibrinolytic therapy (13.4% versus 7.0%). Median time from symptom onset to first medical contact was unchanged (≈50 minutes). Use of prehospital ECGs increased (45% versus 71%). All major reperfusion times improved: median first medical contact‐to‐device for emergency medical systems transport to percutaneous coronary intervention–capable hospitals (93 to 84 minutes), first door‐to‐device for transfers for primary percutaneous coronary intervention (130 to 112 minutes), and door‐in–door‐out at non–percutaneous coronary intervention–capable hospitals (76 to 62 minutes) (all P<0.001 over 5 years). Rates of cardiogenic shock and cardiac arrest, and overall in‐hospital mortality increased (5.7% to 6.3%). Adjusted mortality excluding patients with known cardiac arrest decreased by 14% at 3 years and 25% at 5 years (P<0.001).
Conclusions
Quality of care for patients with ST‐segment–elevation myocardial infarction improved over time in Mission: Lifeline, including increased use of reperfusion therapy and faster times‐to‐treatment. In‐hospital mortality improved for patients without cardiac arrest but did not appear to improve overall as the number of these high‐risk patients increased.
Keywords: fibrinolytic therapy, primary percutaneous coronary intervention, reperfusion, ST‐segment elevation myocardial infarction
Subject Categories: Percutaneous Coronary Intervention, Quality and Outcomes
Clinical Perspective
What Is New?
This report from the American Heart Association's Mission: Lifeline program shows that a national campaign, including a total of 485 US hospitals, to improve regional systems of care for ST‐elevation–myocardial infarction can substantially improve time from first medical contact to primary percutaneous coronary intervention.
The program included optimizing and coordinating the roles of emergency medical services and non–percutaneous coronary intervention–capable and percutaneous coronary intervention–capable hospitals.
Along with improved timely reperfusion, after adjusting for other factors including cardiac arrest, there was a 25% improvement in hospital survival.
What Are the Clinical Implications?
This analysis strongly supports the value of regional systems, including data collection and feedback across regions, to improve the care and outcomes of patients with ST‐segment–elevation myocardial infarction.
This experience reinforces the recommendations in US and European clinical practice guidelines to establish regional systems of care for patients with ST‐segment–elevation myocardial infarction.
Introduction
The most important intervention to improve early survival for patients with ST‐segment–elevation myocardial infarction (STEMI) presenting within 12 hours of symptom onset is prompt myocardial reperfusion, with a 20% to 25% relative risk reduction with fibrinolytic therapy1 and a 30% additional relative risk reduction with primary percutaneous coronary intervention (PCI).2 The additional benefit of modestly faster reperfusion times is debatable, but the fact that faster reperfusion results in smaller infarct size and lower mortality is not, particularly in the early hours after symptom onset. Because patients with STEMI have various points of entry into the healthcare system—emergency medical systems (EMS) versus self‐transportation, non–PCI‐capable hospitals versus PCI‐capable hospitals—the American Heart Association (AHA) organized a stakeholders meeting in 2006 that identified challenges and opportunities in improving regional systems of care.3 This provided the framework for the AHA Mission: Lifeline program, which aimed to promote ideal systems of STEMI care by bringing healthcare resources together into efficient, organized, coordinated systems at the community level.4, 5 The goals of Mission: Lifeline are supported by the 2013 American College of Cardiology Foundation/AHA Guideline for the Management of ST‐Elevation Myocardial Infarction, with a class I, level of evidence B recommendation that “all communities should create and maintain a regional system of STEMI care that includes assessment and continuous quality improvement of EMS and hospital‐based activities. Performance can be facilitated by participating in programs such as Mission: Lifeline and the Door‐to‐Balloon (D2B) Alliance.”6 Herein, we report the clinical results during the first 5 years of the Mission: Lifeline program.
Methods
All patients with STEMI admitted to hospitals registered with Mission: Lifeline from January 1, 2008 to December 31, 2012 were entered into the National Cardiovascular Data Registry ACTION‐GWTG (Acute Coronary Treatment and Intervention Outcomes Network Registry—Get With The Guidelines) and constitute the study population. Hospital participation in Mission: Lifeline is voluntary.
The ACTION‐GWTG Registry serves as a hospital data collection and evaluation mechanism for Mission: Lifeline and has been described previously.7 A diagnosis of STEMI was defined as persistent ST‐segment elevation ≥1 mm in ≥2 contiguous ECG leads or a STEMI equivalent such as a new or presumed new left bundle‐branch block or an isolated posterior myocardial infarction. All participating institutions were required to comply with local regulatory and privacy guidelines and, if required, to secure institutional review board approval. Because data were used primarily at the local site for quality improvement, sites were granted a waiver of informed consent under the common rule. The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
Objectives
Mission: Lifeline aims to improve application of guideline‐recommended care for STEMI through development and promotion of regional systems of care. Relevant class I recommendations from the 2013 American College of Cardiology Foundation/AHA STEMI guidelines include (1) a 12‐lead ECG by EMS personnel at the site of first medical contact (FMC) in patients with symptoms consistent with STEMI; (2) EMS transport directly to a PCI‐capable hospital for primary PCI with an ideal FMC‐to‐device time system goal of 90 minutes or less; (3) for patients initially presenting to a non–PCI‐capable hospital, immediate transfer to a PCI‐capable hospital for primary PCI, with a FMC‐to‐device time system goal of 120 minutes or less; and (4) in the absence of contraindications, fibrinolytic therapy for patients at non–PCI‐capable hospitals when the anticipated FMC‐to‐device time at a PCI‐capable hospital exceeds 120 minutes because of unavoidable delays.6
Intervention
Tools were provided on the Mission: Lifeline website for addressing each of the points of entry (EMS, non–PCI‐capable hospitals, PCI‐capable hospitals, and the system) and for coordinating them, including protocols, clear lines of communication, and measurement and timely feedback. Regular (monthly) meetings of interdisciplinary teams are recommended, including EMS, nursing, emergency medicine and cardiology physicians, quality improvement experts, and hospital administrators. Regular webinars were provided. Reports were provided to each hospital, and regional reports that included groups of hospitals in specified regions were available to assess performance and progress. These regional activities were supported by local leaders and AHA staff. The Mission: Lifeline program was led by an Advisory Working Group with EMS, research, and publications committees.
Statistical Analysis
Descriptive statistics were summarized as medians with 25th and 75th percentiles for continuous variables and percentages for categorical variables. Differences between groups were compared using Cochran‐Mantel‐Haenszel nonzero correlation tests for continuous variables and Cochran‐Mantel‐Haenszel row mean score tests for categorical variables.
In‐hospital mortality was adjusted for patient baseline factors with the multivariable model developed from the ACTION‐GTWG Registry data.8 Adjustment variables were: age, sex, race, weight, heart failure at presentation (heart failure only, shock only, or shock with heart failure versus none), heart rate (linear spline with knot at 70), systolic blood pressure, hypertension, diabetes mellitus, peripheral artery disease, current/recent smoker, dyslipidemia, prior myocardial infarction, prior PCI, prior coronary artery bypass graft surgery, prior heart failure, stroke, baseline hemoglobin, baseline serum creatinine, baseline troponin, and insurance status. All regression models used generalized estimating equations with an exchangeable working correlation matrix to adjust for clustering within hospitals.
Because cardiac arrest is often fatal, and because an increasing proportion of patients with STEMI and cardiac arrest are taken for primary PCI (a class I recommendation in the STEMI guidelines), analyses were also conducted removing patients with known cardiac arrest. Cardiac arrest “as a reason for PCI delay” has been collected since 2008, and the presence or absence of prehospital cardiac arrest has been collected since 2011.
Proportions of missing values were less than 0.6% across all variables. Missing categorical variables were imputed to the most frequent value; weight, baseline hemoglobin, and baseline serum creatinine were imputed to the sex‐specific median of the nonmissing values, and other missing continuous variables were imputed to the median of the nonmissing values. The results are presented as odds ratios with 95% confidence intervals. P<0.05 was considered significant, although these results need to be interpreted in the context of multiple testing and plausibility. All statistical analyses were performed at the Duke Clinical Research Institute using SAS software (version 9.2, SAS Institute, Cary, NC).
Results
Between January 1, 2008 and December 31, 2012, 147 466 patients with STEMI were admitted to a total of 485 US hospitals, from 46 states, representing 656 systems (Figure 1) registered with Mission: Lifeline and entered into the ACTION‐GWTG Registry. The number of participating hospitals increased from 179 in 2008 to 445 in 2012.
Figure 1.
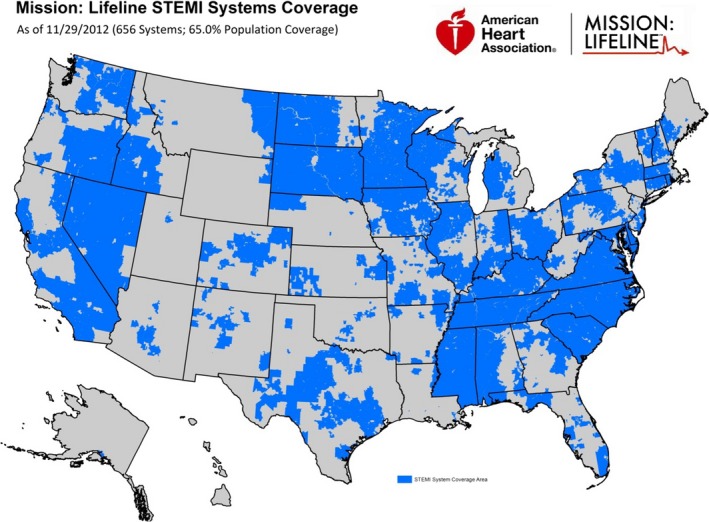
Mission: Lifeline STEMI systems United States national coverage as of November 29, 2012. STEMI indicates ST‐segment–elevation myocardial infarction.
Baseline patient characteristics of the population by year are shown in Table 1. The median age was 60 years, and 30% were women. Median time from symptom onset to FMC was ≈50 minutes. The population had generally similar baseline characteristics over the 5 years with the exception of Killip class IV patients, who increased from 6.8% to 7.7% (P<0.001), and recorded cardiac arrest increased from 1.7% to 9.9% (P<0.001).
Table 1.
Baseline Characteristics and Reperfusion Strategy by Year
| Variable | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|
| Hospitals (n) | 179 | 224 | 334 | 383 | 445 |
| Patients (n) | 18 583 | 21 670 | 29 886 | 35 683 | 41 644 |
| Baseline characteristics | |||||
| Age, median (25th, 75th), y | 60 (52, 71) | 60 (52, 71) | 60 (52, 71) | 61 (52, 71) | 61 (52, 70) |
| Male, (%) | 69.8 | 70.4 | 70.0 | 70.2 | 70.3 |
| Female, (%) | 30.2 | 29.5 | 30.0 | 29.8 | 29.7 |
| SBP on admission, median (25th, 75th), mm Hg | 138 (118, 158) | 140 (119, 161) | 140 (119, 160) | 140 (119, 162) | 140 (119, 162) |
| Heart rate on admission, median (25th, 75th), bpm | 78 (65, 92) | 78 (65, 93) | 79 (66, 93) | 79 (66, 94) | 79 (66, 94) |
| Killip class, (%) | |||||
| I | 85.2 | 84.4 | 85.2 | 86.2 | 86.8 |
| II to III | 7.7 | 7.0 | 6.2 | 5.8 | 5.5 |
| IV | 6.8 | 8.4 | 8.4 | 7.9 | 7.7 |
| Cardiac arrest, % | 1.72 | 4.10 | 4.56 | 8.02 | 9.85 |
| Time from symptom onset to FMC, median (25th, 75th), min | 50 (21, 120) | 50 (23, 120) | 50 (23, 120) | 52 (24, 120) | 49 (23, 115) |
| Transfer strategy | |||||
| Direct presenting to PCI‐capable hospital via EMS, % | 38.4 | 40.9 | 42.0 | 41.9 | 43.0 |
| Direct presenting to PCI‐capable hospital via private vehicle, % | 12.6 | 24.9 | 25.1 | 25.6 | 26.1 |
| Transfer from non–PCI‐capable to PCI‐capable hospital, % | 36.8 | 34.2 | 32.9 | 32.5 | 30.9 |
| Reperfusion strategy | |||||
| PPCI among direct presenters, % | |||||
| No | 6.48 | 7.35 | 7.14 | 3.80 | 2.39 |
| Yes | 93.0 | 92.3 | 92.6 | 96.1 | 97.5 |
| PPCI among transfer in, % | |||||
| No | 37.7 | 31.8 | 27.3 | 14.9 | 9.90 |
| Yes | 61.7 | 68.0 | 72.3 | 84.9 | 89.9 |
| Fibrinolytic therapy, % | |||||
| No | 82.6 | 88.3 | 90.6 | 92.3 | 92.8 |
| Yes | 13.4 | 11.2 | 9.03 | 7.39 | 7.02 |
| Fibrinolytics followed by PCI within first 24 h among fibrinolytic‐treated patients, % | |||||
| No | 93.5 | 91.6 | 90.9 | 92.2 | 92.1 |
| Yes | 6.21 | 8.35 | 9.06 | 7.72 | 7.81 |
| Treated with neither PPCI nor fibrinolytics (excluding contraindications), % | |||||
| No reperfusion | 6.16 | 6.20 | 6.21 | 4.39 | 3.26 |
| Reperfusion | 93.6 | 93.7 | 93.7 | 95.5 | 96.7 |
EMS indicates emergency medical systems; FMC, first medical contact; PCI, percutaneous coronary intervention; PPCI, primary percutaneous coronary intervention; SBP, systolic blood pressure.
Mode of Presentation, Use of Prehospital ECGs, and Reperfusion Strategies
Approximately two‐thirds of the population presented directly to PCI‐capable hospitals, and one‐third presented to non–PCI‐capable hospitals, with nearly all of these patients being transferred to PCI‐capable hospitals. For patients presenting directly to PCI‐capable hospitals, 62% presented by EMS, and this percentage remained constant over 5 years (Table 1). Use of prehospital ECGs increased from 45% to 71%. Over the 5 years, the proportion of patients presenting to PCI‐capable hospitals who received primary PCI (excluding patients with contraindications) increased from 93% to 98%. Primary PCI among transfer patients increased from 62% to 90%. Use of fibrinolytic therapy decreased from 13.4% to 7.0%, and fibrinolytic therapy followed by PCI within 24 hours (a class IIa, level of evidence B recommendation) increased from 6.2% to 7.8%. The total proportion of patients (without contraindications) not treated with reperfusion therapy decreased from 6.2% to 3.3% (P<0.001).
Times to Treatment
For patients brought directly to PCI‐capable hospitals by EMS, FMC‐to‐device times consistently decreased over 5 years from 93 to 84 minutes (P<0.001), with 75% treated within 102 minutes in 2012 (Table 2). For transfer patients, first door‐to‐device time decreased from 130 to 112 minutes (P<0.001). Median door‐in–door‐out times at non–PCI‐capable hospitals decreased from 76 to 62 minutes (P<0.001).
Table 2.
Prehospital ECGs and Treatment Times
| Variable | 2008 | 2009 | 2010 | 2011 | 2012 | P Valuea |
|---|---|---|---|---|---|---|
| Prehospital ECGs among EMS transport to PCI centers, % | 45.3 | 57.7 | 61.1 | 65.9 | 71.3 | <0.001 |
| Door‐to‐device time (all direct presenters), min | 68 (52, 86) | 63 (48, 80) | 61 (47, 78) | 60 (44, 76) | 59 (43, 75) | <0.001 |
| FMC‐to‐device time (EMS+direct presenters at PCI centers), min | 93 (77, 112) | 90 (74, 108) | 89 (72, 107) | 86 (70, 104) | 84 (68, 102) | <0.001 |
| First door–to‐device time (transfers), min | 130 (101, 181) | 122 (98, 164) | 119 (93, 161) | 114 (90, 153) | 112 (89, 151) | <0.001 |
| Door‐in–door‐out (transfers), min | 76 (48, 125) | 71 (46, 115) | 66 (42, 107) | 64 (40, 105) | 62 (39, 101) | <0.001 |
| STEMI performance composite score, %b | 100 (87.5, 100) | 100 (88.9, 100) | 100 (88.9, 100) | 100 (100, 100) | 100 (100, 100) | <0.001 |
All data presented as median (25th, 75th), indicating percentiles, unless otherwise indicated. ACE indicates angiotensin‐converting enzyme; EMS, emergency medical system; FMC, first medical contact; PCI, percutaneous coronary intervention; STEMI, ST‐segment–elevation myocardial infarction.
P value for trend test across the 5 years.
Performance composite score includes use of aspirin, β‐blockers, ACE inhibitors, reperfusion therapy, door‐to‐balloon time ≤90 minutes, statins, ejection fraction evaluation, smoking cessation, rehabilitation referral.
In‐Hospital Clinical Outcomes
Cardiogenic shock and cardiac arrest steadily increased over the 5 years as a reason for PCI delay (cardiogenic shock from 6.1% in 2008 to 6.8% in 2012; cardiac arrest from 1.7% in 2008 to 5.3% in 2012; P<0.001 across 5 years). Mortality increased from 5.7% to 6.3% (P=0.001) (Figure 2). However, when patients with known cardiac arrest were excluded and baseline differences were adjusted, mortality steadily decreased over the 5 years (Figure 3). The odds ratios (compared with year 1) were 0.90 in year 2 and 0.86 in year 3, representing a statistically significant 14% relative risk reduction in mortality. In a sensitivity analysis that removed patients with prehospital cardiac arrest as collected in years 4 and 5, the odds ratios decreased to 0.78 in year 4 and 0.75 in year 5 compared with year 1 (P<0.001).
Figure 2.
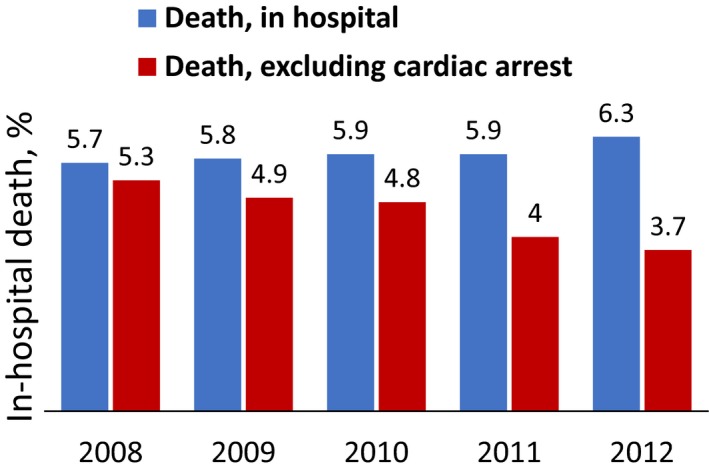
Yearly in‐hospital mortality, crude and excluding reported cardiac arrest, 2008‐2012.
Figure 3.
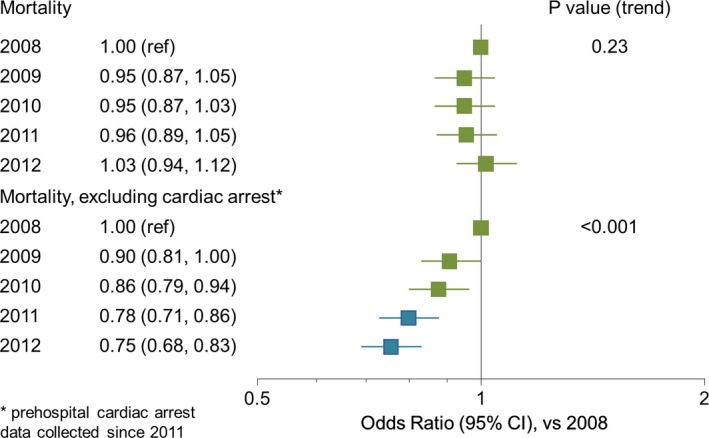
In‐hospital mortality, yearly adjusted odds ratio vs 2008. CI indicates confidence interval; ref, reference value.
Discussion
We have demonstrated that there were substantial improvements in care for patients with STEMI during the first 5 years of the Mission: Lifeline program across the entire system of care. There was a 26% absolute increase in the use of prehospital ECGs by EMS. There was an increase in the use of primary PCI, including a 28% absolute increase in primary PCI among patients transferred from non–PCI‐capable hospitals. There was nearly a 50% reduction in patients not treated with reperfusion therapy. At the same time, times to reperfusion were shortened, particularly times that reflect the performance of the system: median FMC‐to‐device time for patients directly transported by EMS dropped from 93 to 84 minutes, and first door‐to‐device time for transfer patients dropped from 130 to 112 minutes.
Prehospital/Emergency Medical Services
An important focus of Mission: Lifeline has been on prehospital care, where a major portion of system delay occurs.9 This includes earliest diagnosis (with prehospital ECGs), transporting the patient to the nearest PCI‐capable hospital (even if further than a closer non–PCI‐capable center), and activation of the catheterization laboratory team as early as possible, each of which has been shown to improve time to reperfusion.9, 10, 11 The increase in prehospital ECGs from 46% to 71% over 5 years represents a substantial success. This is also reflected in the 9‐minute improvement in FMC‐to‐device time, although the fact that one‐quarter of patients still exceeded 102 minutes shows the need for further improvement.
Non–PCI‐Capable Hospitals
A major shortcoming in STEMI systems has been long delays in transfer of patients for primary PCI.12 A large part of these delays has been the door‐in–door‐out time at the referring hospital,13 which is related to clinical outcomes.10 Fibrinolytic therapy is used in a minority of patients even when transportation time exceeds 45 minutes or when only about 40% of patients are treated within 120 minutes.14 Mission: Lifeline has seen a substantial improvement in door‐in–door‐out time, from 76 to 62 minutes, although this still does not approach the recommended goal of 30 minutes.6 Overall first door–to‐device time has substantially improved from 130 to 112 minutes; however, 25% of patients experience times exceeding 151 minutes with a well‐described association of longer delays with higher mortality.15
PCI‐Capable Hospitals and System
Median door‐to‐device time for all patients presenting to PCI‐capable hospitals improved from 68 to 59 minutes, with 75% achieving door‐to‐device times within 75 minutes. Thus, for patients presenting to PCI‐capable hospitals in the Mission: Lifeline program, the problem of delays in door‐to‐device time has been solved. By 2012, three‐quarters of PCI‐capable hospitals reported that a composite score of 100% was achieved including use of aspirin, β‐blockers, statins, ACE inhibitors, reperfusion therapy (for eligible patients), door‐to‐balloon time ≤90 minutes, left ventricular ejection fraction evaluation, smoking cessation, and cardiac rehabilitation referral. The challenge of optimizing STEMI care has now moved to regional issues, where there are still many opportunities for improvement.
In‐Hospital Outcomes
Whereas the specific goals of Mission: Lifeline have been focused on improving treatment of all eligible patients with timely reperfusion, with primary PCI when possible, the ultimate goal is to improve clinical outcomes including survival. Despite improved door‐to‐device times in this report, raw unadjusted mortality rates did not decline, as previously observed in a population‐level analysis using the National Cardiovascular Data Registry CathPCI Registry.16 However, using the same data set, Nallamothu et al demonstrated that shorter patient‐specific door‐to‐balloon times were consistently associated at the individual level with lower in‐hospital and 6‐month mortality rates.17 The discordance in the 2 analyses is explained by an increasing mortality risk in the growing and changing primary PCI population that has resulted in the recent absence of association between annual door‐to‐balloon time and changes in mortality at the population level, despite the consistent association between door‐to‐balloon time and mortality at the patient level. Similarly, we observed an increase in patients with Killip class IV and with cardiac arrest over time.18 Adjusting for this, we see a 14% lower mortality at 3 years and as much as a 25% lower mortality at 5 years compared with mortality rates from 2008. These results support ongoing efforts to sustain and expand the adoption and the impact of Mission: Lifeline, which is ongoing.19
Strengths and Limitations
Mission: Lifeline has been one of the largest quality improvement efforts in STEMI ever attempted, with nearly 500 hospitals and 148 000 unselected patients included, and thus is more representative of care in the United States than smaller studies. Yet, these hospitals are selected by nature of their voluntary participation in this quality improvement program, which may limit the generalizability of these findings. Moreover, because the participating hospitals shifted over time, changes may reflect the differing hospital population as well as changes in patient care over time. In addition, these finding are from more than 5 years ago, and there has likely been further change since then. Imputation of missing variables may distort associations. Although we saw substantial improvements in processes of care as reflected by established performance measures,20 we cannot be sure that these improvements resulted from participation in the Mission: Lifeline program because we do not have a relevant control group that did not participate. Whereas we see substantial improvement in survival when patients with known cardiac arrest are excluded, this creates selection bias in that such patients were not excluded before 2011. However, policy statements in 201021 and guideline recommendations reflecting an evolving consensus6 to perform primary PCI for patients with cardiac arrest and ST elevation on the presenting ECG (class I, level of evidence B) can be expected to have resulted in a higher proportion of these patients undergoing PCI each year. Definitive data on changes in the proportion of patients with cardiac arrest undergoing primary PCI, however, are lacking. Nevertheless, this changing consensus on primary PCI for patients with out‐of‐hospital cardiac arrest justifies an analysis removing this group of patients with a very high (50%) mortality, at least as a sensitivity analysis.
Conclusions
Quality of care for patients with STEMI improved over time in Mission: Lifeline, including increased use of reperfusion therapy and faster times to treatment. In‐hospital mortality improved for patients without cardiac arrest but did not appear to improve overall as the number of these high‐risk patients increased.
This highlights the need for improving system‐level care for out‐of‐hospital cardiac arrest, an ongoing objective of Mission: Lifeline.
Sources of Funding
Mission: Lifeline is an initiative of the American Heart Association. ACTION‐GWTG Registry is a registry led and supported by the American College of Cardiology Foundation and the American Heart Association, with partnering support from the Society of Chest Pain Centers, the Society of Hospital Medicine, and the American College of Emergency Physicians. The registry is sponsored by Bristol‐Myers Squibb/Sanofi Pharmaceuticals.
Disclosures
Dr Granger has a working relationship (ie, consulting, research, and educational services) with the following companies: American College of Cardiology Foundation, AstraZeneca, Boehringer Ingelheim, Bristol‐Myers Squibb, Elsevier, GlaxoSmithKline, Hoffman LaRoche (Roche Holding), McGraw‐Hill Publishing, Medtronic Inc, Pfizer Inc, Sanofi‐Aventis, UpToDate, Inc, and WebMD. All conflicts of interest are listed at www.dcri.org. Dr Jollis has a working relationship (ie, consulting, research, and educational services) with the following companies: Blue Cross Blue Shield North Carolina, Medtronic Foundation, Sanofi‐Aventis, and United Healthcare. The remaining authors have no disclosures to report.
Acknowledgments
We thank Elizabeth Cook for editorial assistance with this manuscript. We acknowledge the contributions of Chris Bjerke, RN, and Lori Hollowell, RN, for their contributions to Mission: Lifeline.
(J Am Heart Assoc. 2019;8:e008096 DOI: 10.1161/JAHA.118.008096)
References
- 1. Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group . Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet. 1994;343:311–322. [PubMed] [Google Scholar]
- 2. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. [DOI] [PubMed] [Google Scholar]
- 3. Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of systems of care for ST‐elevation myocardial infarction patients: executive summary. Circulation. 2007;116:217–230. [DOI] [PubMed] [Google Scholar]
- 4. Jollis JG, Granger CB, Henry TD, Antman EM, Berger PB, Moyer PH, Pratt FD, Rokos IC, Acuña AR, Roettig ML, Jacobs AK. Systems of care for ST‐segment‐elevation myocardial infarction: a report from the American Heart Association's Mission: Lifeline. Circ Cardiovasc Qual Outcomes. 2012;5:423–428. [DOI] [PubMed] [Google Scholar]
- 5. American Heart Association . Mission: Lifeline website. Available at: http://www.heart.org/HEARTORG/HealthcareResearch/MissionLifelineHomePage/Mission-Lifeline-Home-Page_UCM_305495_SubHomePage.jsp. Accessed April 4, 2017.
- 6. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis‐Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX. 2013 ACCF/AHA Guideline for the Management of ST‐elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–e425. [DOI] [PubMed] [Google Scholar]
- 7. Peterson ED, Roe MT, Rumsfeld JS, Shaw RE, Brindis RG, Fonarow GC, Cannon CP. A call to ACTION (Acute Coronary Treatment and Intervention Outcomes Network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:491–499. [DOI] [PubMed] [Google Scholar]
- 8. Chin CT, Chen AY, Wang TY, Alexander KP, Mathews R, Rumsfeld JS, Cannon CP, Fonarow GC, Peterson ED, Roe MT. Risk adjustment for in‐hospital mortality of contemporary patients with acute myocardial infarction: the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) registry‐Get With the Guidelines (GWTG) acute myocardial infarction mortality model and risk score. Am Heart J. 2011;161:113–122.e2. [DOI] [PubMed] [Google Scholar]
- 9. O'Connor RE, Nichol G, Gonzales L, Manoukian SV, Moyer PH, Rokos I, Sayre MR, Solomon RC, Wingrove GL, Brady WJ, McBride S, Lorden AL, Roettig ML, Acuna A, Jacobs AK. Emergency medical services management of ST‐segment elevation myocardial infarction in the United States—a report from the American Heart Association Mission: Lifeline Program. Am J Emerg Med. 2014;32:856–863. [DOI] [PubMed] [Google Scholar]
- 10. Wang TY, Nallamothu BK, Krumholz HM, Li S, Roe MT, Jollis JG, Jacobs AK, Holmes DR, Peterson ED, Ting HH. Association of door‐in to door‐out time with reperfusion delays and outcomes among patients transferred for primary percutaneous coronary intervention. JAMA. 2011;305:2540–2547. [DOI] [PubMed] [Google Scholar]
- 11. Fosbol EL, Granger CB, Jollis JG, Monk L, Lin L, Lytle BL, Xian Y, Garvey JL, Mears G, Corbett CC, Peterson ED, Glickman SW. The impact of a statewide pre‐hospital STEMI strategy to bypass hospitals without percutaneous coronary intervention capability on treatment times. Circulation. 2013;127:604–612. [DOI] [PubMed] [Google Scholar]
- 12. Jollis JG, Al‐Khalidi HR, Monk L, Roettig ML, Garvey JL, Aluko AO, Wilson BH, Applegate RJ, Mears G, Corbett CC, Granger CB. Expansion of a regional ST‐segment‐elevation myocardial infarction system to an entire state. Circulation. 2012;126:189–195. [DOI] [PubMed] [Google Scholar]
- 13. Dauerman HL, Bates ER, Kontos MC, Li S, Garvey JL, Henry TD, Manoukian SV, Roe MT. Nationwide analysis of patients with ST‐segment‐elevation myocardial infarction transferred for primary percutaneous intervention: findings from the American Heart Association Mission: Lifeline Program. Circ Cardiovasc Interv. 2015;8:e002450. [DOI] [PubMed] [Google Scholar]
- 14. Vora AN, Holmes DN, Rokos I, Roe MT, Granger CB, French WJ, Antman E, Henry TD, Thomas L, Bates ER, Wang TY. Fibrinolysis use among patients requiring interhospital transfer for ST‐segment elevation myocardial infarction care: a report from the US National Cardiovascular Data Registry. JAMA Intern Med. 2015;175:207–215. [DOI] [PubMed] [Google Scholar]
- 15. Miedema MD, Newell MC, Duval S, Garberich R, Handran C, Larson DM, Mulder S, Wang YL, Lips D, Henry TD. Causes of delay and associated mortality in patients transferred with ST‐elevation myocardial infarction. Circulation. 2011;124:1636–1644. [DOI] [PubMed] [Google Scholar]
- 16. Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS. Door‐to‐balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901–909. [DOI] [PubMed] [Google Scholar]
- 17. Nallamothu BK, Normand SL, Wang Y, Hofer TP, Brush JE Jr, Messenger JC, Bradley EH, Rumsfeld JS, Krumholz HM. Relation between door‐to‐balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;385:1114–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Swaminathan RV, Wang TY, Kaltenbach LA, Kim LK, Minutello RM, Bergman G, Wong SC, Feldman DN. Nonsystem reasons for delay in door‐to‐balloon time and associated in‐hospital mortality: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2013;61:1688–1695. [DOI] [PubMed] [Google Scholar]
- 19. Jollis JG, Al‐Khalidi HR, Roettig ML, Berger PB, Corbett CC, Dauerman HL, Fordyce CB, Fox K, Garvey JL, Gregory T, Henry TD, Rokos IC, Sherwood MW, Suter RE, Wilson BH, Granger CB. Regional systems of care demonstration project: American Heart Association Mission: Lifeline STEMI Systems Accelerator. Circulation. 2016;134:365–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jneid H, Addison D, Bhatt DL, Fonarow GC, Gokak S, Grady KL, Green LA, Heidenreich PA, Ho PM, Jurgens CY, King ML, Kumbhani DJ, Pancholy S. AHA/ACC clinical performance and quality measures for adults with ST‐elevation and non‐ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2017;2017:10. [DOI] [PubMed] [Google Scholar]
- 21. Nichol G, Aufderheide TP, Eigel B, Neumar RW, Lurie KG, Bufalino VJ, Callaway CW, Menon V, Bass RR, Abella BS, Sayre M, Dougherty CM, Racht EM, Kleinman ME, O'Connor RE, Reilly JP, Ossmann EW, Peterson E. Regional systems of care for out‐of‐hospital cardiac arrest: a policy statement from the American Heart Association. Circulation. 2010;121:709–729. [DOI] [PubMed] [Google Scholar]


