Abstract
Background
Prior studies suggest that persistence with and adherence to statin therapy is low. Interventions to improve statin persistence and adherence have been developed over the past decade.
Methods and Results
This was a retrospective cohort study of adults aged ≥21 y with commercial or government health insurance in the MarketScan (Truven Health Analytics) and Medicare databases who initiated statins in 2007–2014 and (1) started treatment after a myocardial infarction (n=201 573), (2) had diabetes mellitus but without coronary heart disease (CHD; n=610 049), or (3) did not have CHD or diabetes mellitus (n=2 244 868). Persistence with (ie, not discontinuing treatment) and high adherence to statin therapy were assessed using pharmacy fills in the year following treatment initiation. In 2007 and 2014, the proportions of patients persistent with statin therapy were 78.1% and 79.1%, respectively, among those initiating treatment following myocardial infarction; 66.5% and 67.3%, respectively, for those with diabetes mellitus but without CHD; and 64.3% and 63.9%, respectively, for those without CHD or diabetes mellitus. Between 2007 and 2014, high adherence to statin therapy increased from 57.9% to 63.8% among patients initiating treatment following myocardial infarction and from 34.9% to 37.6% among those with diabetes mellitus but without CHD (each P trend<0.001). Among patients without CHD or diabetes mellitus, high adherence did not improve between 2007 (35.7%) and 2014 (36.8%; P trend=0.14). In 2014, statin adherence was lower among younger, black, and Hispanic patients versus white patients and those initiating a high‐intensity statin dosage. Statin adherence was higher among men and patients with cardiologist care following treatment initiation.
Conclusions
Persistence with and adherence to statin therapy remain low, particularly among those without CHD.
Keywords: medication adherence, statin therapy
Subject Categories: Epidemiology, Primary Prevention, Secondary Prevention
Clinical Perspective
What Is New?
Persistence with statin therapy remained similar from 2007 to 2014.
High adherence to statin therapy increased modestly among patients initiating treatment after a myocardial infarction or with diabetes mellitus between 2007 and 2014 but did not improve among those without a history of coronary heart disease or diabetes mellitus.
What Are the Clinical Implications?
This study highlights the need to improve persistence with and adherence to statin therapy if the cardiovascular risk‐reduction benefits of statins demonstrated in clinical trials are to be translated into clinical practice.
Healthcare providers should monitor statin use following initiation of treatment and work with patients to identify barriers to taking this medication with high adherence.
Patient characteristics associated with lower persistence with and adherence to statin therapy identified in this study could be used to guide interventions aiming to increase statin persistence and adherence.
Introduction
Clinical trials have shown that statins are effective in reducing the risk of coronary heart disease (CHD) events.1, 2 Based on this evidence, the 2013 American College of Cardiology (ACC) and American Heart Association (AHA) “Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults” recommended that adults with CHD take a statin.3 Statin therapy is also recommended for adults with other forms of atherosclerotic cardiovascular disease or LDL (low‐density lipoprotein) cholesterol ≥190 mg/dL and those aged 40 to 75 years who have LDL cholesterol of 70 to 189 mg/dL in addition to diabetes mellitus or a 10‐year predicted risk of atherosclerotic cardiovascular disease ≥7.5%.3
Adults who have low adherence or who discontinue statin therapy have an increased risk of CHD events compared with their counterparts with high adherence to statins.4, 5 Observational studies have suggested that a high proportion of adults initiating statins have low adherence or discontinue treatment.6, 7, 8, 9 However, most large studies of statin adherence used data collected before 2005, and the use of statin therapy has increased markedly over the past 15 years.10, 11 In addition, randomized trials have demonstrated that health system, clinician, and patient‐centered approaches can improve statin adherence.12, 13, 14
The aim of this study was to analyze trends in persistence with (ie, nondiscontinuation) and high adherence to statins among adults aged ≥21 years who initiated this medication between 2007 and 2014. Patients initiating statin therapy following a myocardial infarction (MI), those with diabetes mellitus but without a history of CHD, and those without a history of CHD or diabetes mellitus were analyzed separately because these populations have different risks of CHD events, and we hypothesized that adherence would differ among them.15 We also determined patient characteristics associated with persistence with and high adherence to statin therapy in 2014.
Methods
We conducted a retrospective cohort study using administrative data from MarketScan (Truven Health Analytics, Ann Arbor, MI) and Medicare. The MarketScan database contains data from patients with commercial and Medicare supplemental health insurance in the United States. MarketScan data for 2006 through 2015 were obtained from Truven Health Analytics. Medicare is a government program that provides health insurance for US adults aged ≥65 years and adults aged <65 years with end‐stage renal disease or who are disabled. Medicare data, including a 100% sample of patients with an MI hospitalization between 2006 and 2015 and a 5% random sample of all beneficiaries between 2006 and 2015 were obtained from the Centers for Medicare and Medicaid Services (CMS) Chronic Conditions Warehouse. The institutional review board at the University of Alabama at Birmingham and the CMS approved the study and waived the requirement to obtain informed consent. Data used in the current study are available from the CMS. Other study information is available from the corresponding author.
Study Population
We identified patients in the MarketScan and Medicare databases with a statin prescription fill between January 1, 2007, and December 31, 2014. In each calendar year between 2007 and 2014, we identified the earliest statin prescription fill for each patient (ie, their index statin fill). From this population, we selected 3 mutually exclusive groups of patients in each calendar year: (1) patients whose index statin fill was within 30 days after hospital discharge for MI, (2) patients who had diabetes mellitus but no history of CHD, and (3) patients without a history of CHD or diabetes mellitus. MI hospitalizations and history of CHD and diabetes mellitus were defined based on previously validated algorithms and administrative claims in the year before the index statin fill, as described in Table 1.16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29 We used the 100% sample of Medicare beneficiaries with an MI to identify patients with government health insurance whose index statin fill was within 30 days following hospital discharge for MI. We used the 5% random sample of all Medicare beneficiaries to identify patients who had government health insurance with diabetes mellitus without a history of CHD and without a history of CHD or diabetes mellitus on the date of their index statin fill. All MarketScan claims were used to identify patients with commercial health insurance initiating statins following an MI, with diabetes mellitus without a history of CHD, and without a history of CHD or diabetes mellitus.
Table 1.
Definitions for Patient Characteristics
| Characteristics | Definition |
|---|---|
| Preindex statin fill characteristics* | |
| MI hospitalization16 | An inpatient claim with an ICD‐9‐CM code of 410.xx (except 410.x2, which represents a subsequent episode of care) in any discharge diagnosis position |
| History of CHD17, 18 | Any of the following:
|
| History of DM19 | Any of the following:
|
| History of stroke20 | Any of the following:
|
| History of peripheral artery disease21, 22 | Any of the following:
|
| History of HF23 | Any of the following:
|
| History of CKD24, 25 | Any of the following:
|
| History of dementia26 | Any of the following:
|
| Depression23, 27, 28 | Any of the following:
|
| Postindex statin fill characteristics† | |
| New diagnosis of CHD18, 29 | Any of the following among beneficiaries without a history of CHD:
|
| New diagnosis of DM19 | Any of the following among beneficiaries without a history of DM:
|
| New diagnosis of stroke20 | Any of the following among beneficiaries without a history of stroke:
|
| New diagnosis of HF23 | Any of the following among beneficiaries without a history of HF:
|
| New diagnosis of CKD24, 25 | Any of the following among beneficiaries without a history of CKD:
|
| New diagnosis of dementia26 | Any of the following among beneficiaries without a history of dementia:
|
| Cardiologist care | ≥1 physician evaluation and management visit with a specialty code 06 |
In Medicare, physician evaluation and management visits were defined by CPT code 99024, 99058, 99429, 99499, 99201–99215, 99241–99245, 99271–99275, 99301–99337, 99341–99355, 99385–99387, or 99395–99404, or 99281–99285. In MarketScan, physician evaluation and management visits were defined by an ambulatory visit, emergency department, or nursing home encounter type. CHD indicates coronary heart disease; CKD, chronic kidney disease; CPT, Current Procedure Terminology; DM, diabetes mellitus; HF, heart failure; ICD‐9‐CM, International Classification of Diseases, Ninth Revision, Clinical Modification; MI, myocardial infarction.
Defined using administrative data on or within 365 days before the date of the index statin fill.
Defined using administrative data within 182 days after the index statin fill.
To avoid including a patient twice in the same calendar year, we excluded patients aged ≥65 years on the date of their index statin fill in the MarketScan database because this population is eligible for Medicare health insurance. Because we required a 365‐day period before statin initiation to ensure that patients were not already taking a statin and to identify patient characteristics, we excluded patients aged <65 years 365 days before their index statin fill (ie, aged <66 years on their index statin fill) in the Medicare database. To ensure that the study population was composed of patients initiating statins, we excluded individuals who had a statin fill within 365 days before their index statin fill. We further restricted the analysis to patients living in the United States who had continuous inpatient, outpatient, and pharmacy coverage from 365 days before through 365 days after their index statin fill. Medicare Advantage provides managed care health insurance to Medicare beneficiaries without requiring claims to be filed for most services. Therefore, Medicare beneficiaries who had Medicare Advantage coverage at any time in the 365 days before or after their index statin fill were excluded. Patients in the Medicare databases were required to be alive 365 days after their index statin fill. This requirement was not applied to patients in MarketScan because mortality data are not available in that database. Table 2 shows a cascade of patients included in the current analysis.
Table 2.
Exclusion Cascade of Patients in MarketScan and Medicare Databases Included in the Current Analysis
| Exclusion Criteria | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Patients initiating a statin following a MI hospitalization | |||||||||
| First statin fill in the calendar year (ie, the index statin fill) within 30 d following hospital discharge for MI* | 41 426 | 48 587 | 49 097 | 49 542 | 52 482 | 54 649 | 55 181 | 57 126 | 408 090 |
| No statin fill in the 365 d before the index statin fill | 35 279 | 39 268 | 39 302 | 39 207 | 41 556 | 43 176 | 43 411 | 43 922 | 325 121 |
| Lived in the United States from 365 d before through 365 d after the index statin fill | 32 764 | 36 602 | 36 808 | 36 610 | 38 737 | 39 960 | 40 124 | 40 711 | 302 316 |
| Had continuous full health insurance coverage from 365 d before through 365 d after the index statin fill† | 20 816 | 24 125 | 24 495 | 25 456 | 26 556 | 26 310 | 26 378 | 27 437 | 201 573 |
| Patients initiating a statin with DM without a history of CHD | |||||||||
| Had DM without a history of CHD on the date of the first statin fill in the calendar year (ie, the index statin fill)* | 50 1283 | 70 7366 | 82 9836 | 84 9712 | 93 1119 | 95 3773 | 81 7412 | 85 0835 | 644 1336 |
| No statin fill in the 365 d before the index statin fill | 167 379 | 309 883 | 292 096 | 264 936 | 301 381 | 257 963 | 220 603 | 249 703 | 2 063 944 |
| Lived in the United States from 365 d before through 365 d after the index statin fill | 165 427 | 307 968 | 289 873 | 262 795 | 299 035 | 255 675 | 217 741 | 247 510 | 2 046 024 |
| Had continuous full health insurance coverage from 365 d before through 365 d after the index statin fill† | 61 134 | 67 636 | 83 808 | 84 985 | 90 929 | 79 979 | 73 522 | 68 056 | 610 049 |
| Patients initiating a statin without a history of CHD or DM | |||||||||
| No history of CHD or DM on the date of the first statin fill in the calendar year (ie, the index statin fill)* | 1 675 698 | 2 394 577 | 2 763 030 | 2 709 655 | 2 917 717 | 2 871 238 | 2 380 732 | 2 465 263 | 20 177 910 |
| No statin fill in the 365 d before the index statin fill | 685 900 | 1 270 626 | 1 237 209 | 1 066 309 | 1 199 621 | 1 000 980 | 831 252 | 933 944 | 8 225 841 |
| Lived in the United States from 365 d before through 365 d after the index statin fill | 681 854 | 1 266 549 | 1 232 417 | 1 061 690 | 1 194 748 | 996 171 | 824 863 | 929 125 | 8 187 417 |
| Had continuous full health insurance coverage from 365 d before through 365 d after the index statin fill† | 239 058 | 258 626 | 325 082 | 321 807 | 328 819 | 282 255 | 265 499 | 223 722 | 2 244 868 |
CHD indicates coronary heart disease; DM, diabetes mellitus; MI, myocardial infarction.
Patients in MarketScan were required to be 21 to <65 years of age and patients in Medicare were required to be ≥66 years of age on the date of their index statin fill.
Full health insurance coverage includes inpatient, outpatient and pharmacy coverage for patients in MarketScan. Full health insurance coverage includes Part A (inpatient), Part B (outpatient), and Part D (pharmacy) coverage without Medicare Advantage or Part C coverage (a program that provides managed care without the need of submitting claims for services that beneficiaries received). Beneficiaries in Medicare were also required to be alive 365 days after the index statin fill. This requirement was not applied to beneficiaries in MarketScan because mortality data are not available in this data set.
Statin Use, Persistence, and Adherence
Statin use was identified using claims for pharmacy fills and included atorvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin, and simvastatin. The intensity of the index statin fill was defined based on the 2013 ACC/AHA cholesterol treatment guideline (Table 3).3 Persistence with statin therapy was defined by having at least 1 day of statin supply available to take in the last 90 days of the year following the index statin fill (ie, in the 276–365 days following initiation). To assess adherence, we calculated the proportion of days covered (PDC; ie, the percentage of days on which the beneficiary had a statin available to take) in the 365 days after the index statin fill using the interval‐based method.30 Days spent in the hospital were excluded from the PDC calculation. High adherence to statin therapy was defined as PDC ≥80%.
Table 3.
Definition of High‐, Moderate‐ and Low‐Intensity Statins
| Statin Type | High Intensity (mg/d) | Moderate Intensity (mg/d) | Low Intensity (mg/d) |
|---|---|---|---|
| Atorvastatin | 40–80 | 10–20 | |
| Fluvastatin | 80 (or 40 mg twice daily) | 20–40 | |
| Lovastatin | 40–60 | 10–20 | |
| Pitavastatin | 2–4 | 1 | |
| Pravastatin | 40–80 | 10–20 | |
| Rosuvastatin | 20–40 | 5–10 | |
| Simvastatin | 80 | 20–40 | 5–10 |
Patient Characteristics
We used MarketScan and Medicare administrative data to determine patient age on the date of the index statin fill, sex, and race/ethnicity (which was available in Medicare only). Claims data in the 365 days before each patient's index statin fill (ie, the “look‐back” period) were used to define comorbid conditions including history of CHD, diabetes mellitus, stroke, peripheral artery disease, heart failure (HF), chronic kidney disease (CKD), dementia, and depression (see “Preindex statin fill characteristics” in Table 1). Use of antihypertensive medication and nonstatin lipid‐lowering medication was defined using claims for pharmacy fills in the look‐back period. A history of low adherence to antihypertensive medication has been predictive of statin discontinuation and low statin adherence among patients initiating statin therapy following MI.31 Consequently, we calculated the PDC for antihypertensive medication during the look‐back period, with low and high adherence being defined as PDC <80% and ≥80%, respectively. Claims in the 182 days after the index statin fill were used to identify patients with a new diagnosis of CHD, diabetes mellitus, stroke, HF, CKD, or dementia and those receiving cardiologist care (see “Postindex statin fill characteristics” in Table 1). Pharmacy claims in the 182 days following the index statin fill were used to determine the number of medications taken by each patient. A schematic showing the timeline used to identify patient characteristics and the assessment of statin adherence is provided in Figure 1.
Figure 1.
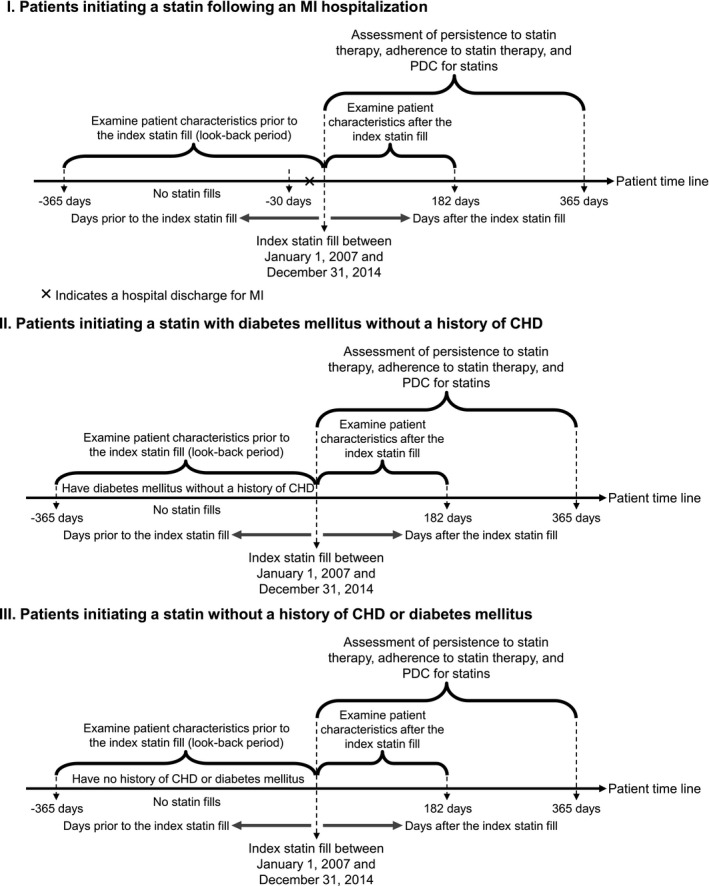
Schematic of the study design. CHD indicates coronary heart disease; MI, myocardial infarction; PDC, proportion of days covered.
Statistical Analysis
The following analyses were conducted separately in each population subgroup (ie, patients initiating statin therapy following an MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus). We calculated patient characteristics overall and by calendar year. For each calendar year, we calculated the proportion of patients with persistence with and high adherence to statin therapy. We used Poisson regression models with robust variance estimators to analyze linear trends in persistence with and high adherence to statin therapy, separately, between 2007 and 2014. We also calculated the mean PDC for statin therapy in each calendar year and used linear regression models to analyze trends in the mean PDC between 2007 and 2014. We pooled data from patients initiating a statin following an MI, with diabetes mellitus without a history of CHD, and without a history of CHD or diabetes mellitus, to compare trends in persistence with and high adherence to statin therapy and mean PDC for statins between 2007 and 2014 by population subgroups. To compare trends in persistence with and high adherence to statin therapy, we added interaction terms between calendar year and population subgroups (eg, calendar year × patients initiating a statin following an MI) to Poisson regression models with robust variance estimators that included main effects for calendar year and the population subgroups. To compare trends in mean PDC for statins, we added interaction terms between calendar year and population subgroups to a linear regression model including main effects for calendar year and population subgroups.
Using pooled data from patients initiating a statin following an MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus in 2014, we analyzed characteristics associated with persistence with statin therapy, high adherence to statin therapy, and mean PDC for statins. Characteristics analyzed included age, sex, race/ethnicity, statin intensity initiated, history of diabetes mellitus, stroke, peripheral artery disease, HF, CKD, dementia, depression, use of and adherence to antihypertensive medication, and use of nonstatin lipid‐lowering medication before the index statin fill. We also analyzed characteristics after the index statin fill, including a new diagnosis of CHD, diabetes mellitus, stroke, HF, CKD, or dementia; cardiologist care; and total number of medications taken. Poisson regression models with robust variance estimators were used to calculate relative risks and 95% CIs for persistence with and high adherence to statin therapy, separately, associated with patient characteristics.32 A linear regression model was used to calculate the difference in mean PDC associated with patient characteristics. Poisson and linear regression models included adjustment for the population group (ie, patients initiating a statin following an MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus) and all characteristics analyzed simultaneously. All analyses were conducted using SAS 9.4 (SAS Institute) and a 2‐sided level of significance <0.05.
Results
Patient Characteristics
Patients initiating a statin following an MI were older and more likely to have a history of stroke, peripheral artery disease, HF, CKD, and dementia and to be taking antihypertensive medication with high adherence before their index statin fill, compared with their counterparts with diabetes mellitus without a history of CHD and those without a history of CHD or diabetes mellitus (Table 4). Patients initiating a statin after an MI were also more likely to initiate a high‐intensity dosage; to have a new diagnosis of stroke, HF, CKD, or dementia; to receive cardiologist care; and to be taking more medications following their index statin fill. The proportions of patients initiating a statin following an MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus who initiated therapy on a high‐intensity dosage had a history of CKD and received cardiologist care following statin initiation increased between 2007 and 2014 (Tables 5, 6, 7). Use of nonstatin lipid‐lowering medication declined between 2007 and 2014 in all 3 groups.
Table 4.
Characteristics of Patients Initiating a Statin Between 2007 and 2014 in MarketScan and Medicare
| Initiating a Statin | |||
|---|---|---|---|
| Following an MI | DM Without a History of CHD | Without a History of CHD or DM | |
| n | 201 573 | 610 049 | 2 244 868 |
| Age, % | |||
| 21–44 y | 3.0 | 16.8 | 17.4 |
| 45–54 y | 9.2 | 32.3 | 35.0 |
| 55–64 y | 14.1 | 43.5 | 42.6 |
| 66–70 y | 17.7 | 2.6 | 1.7 |
| 71–75 y | 16.6 | 2.0 | 1.3 |
| 76–80 y | 14.3 | 1.4 | 0.9 |
| 81–85 y | 12.5 | 0.9 | 0.6 |
| ≥86 y | 12.6 | 0.5 | 0.4 |
| Male sex, % | 53.0 | 49.3 | 50.5 |
| Race/ethnicity, %* | |||
| White | 87.5 | 73.3 | 84.4 |
| Black | 6.9 | 14.1 | 7.3 |
| Asian American | 1.7 | 3.9 | 3.1 |
| Hispanic | 2.1 | 5.2 | 2.8 |
| Other | 1.9 | 3.5 | 2.4 |
| Initiation of high‐intensity statin, % | 34.1 | 11.1 | 8.8 |
| Preindex statin fill characteristics, % | |||
| History of CHD | 100.0 | 0.0 | 0.0 |
| History of DM | 27.6 | 100.0 | 0.0 |
| History of stroke | 2.1 | 1.4 | 1.1 |
| History of peripheral artery disease | 7.9 | 0.7 | 0.4 |
| History of HF | 26.2 | 1.2 | 0.4 |
| History of CKD | 23.3 | 4.7 | 1.4 |
| History of dementia | 6.1 | 0.5 | 0.3 |
| Depression | 20.8 | 23.0 | 23.2 |
| Taking antihypertensive medication | |||
| No | 35.3 | 35.0 | 57.2 |
| Yes, with low adherence | 13.8 | 20.6 | 12.8 |
| Yes, with high adherence | 50.8 | 44.4 | 30.0 |
| Taking nonstatin lipid‐lowering medication | 8.5 | 16.6 | 11.0 |
| Postindex statin fill characteristics, % | |||
| New diagnosis of CHD | 0.0 | 2.4 | 1.7 |
| New diagnosis of DM | 1.7 | 0.0 | 2.2 |
| New diagnosis of stroke | 1.3 | 0.4 | 0.2 |
| New diagnosis of HF | 5.7 | 0.6 | 0.2 |
| New diagnosis of CKD | 4.1 | 1.7 | 0.6 |
| New diagnosis of dementia | 1.6 | 0.1 | 0.1 |
| Cardiologist care | 76.6 | 8.1 | 8.3 |
| Number of medications taken | |||
| <5 | 11.2 | 24.4 | 54.6 |
| 5–9 | 45.6 | 47.1 | 34.2 |
| ≥10 | 43.3 | 28.5 | 11.2 |
Table 5.
Characteristics of Patients Initiating a Statin Following an MI Hospitalization in 2007–2014
| Calendar Year | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| n | 20 816 | 24 125 | 24 495 | 25 456 | 26 556 | 26 310 | 26 378 | 27 437 |
| Age, % | ||||||||
| 21–44 y | 2.7 | 2.8 | 3.1 | 3.5 | 3.3 | 3.1 | 3.0 | 2.2 |
| 45–54 y | 9.1 | 8.5 | 10.2 | 10.4 | 10.7 | 9.4 | 8.6 | 6.6 |
| 55–64 y | 13.8 | 12.5 | 14.7 | 16.2 | 16.2 | 14.6 | 13.4 | 11.1 |
| 66–70 y | 17.3 | 18.0 | 17.0 | 16.4 | 16.5 | 17.6 | 18.6 | 20.0 |
| 71–75 y | 15.8 | 16.6 | 15.7 | 15.6 | 15.8 | 16.7 | 17.4 | 18.7 |
| 76–80 y | 15.7 | 15.8 | 14.3 | 13.6 | 13.0 | 13.5 | 13.9 | 15.3 |
| 81–85 y | 13.4 | 13.6 | 12.5 | 12.0 | 12.0 | 12.4 | 12.1 | 12.6 |
| ≥86 y | 12.3 | 12.3 | 12.4 | 12.3 | 12.5 | 12.8 | 12.9 | 13.4 |
| Male sex, % | 51.9 | 51.8 | 52.7 | 53.8 | 53.8 | 53.1 | 53.7 | 52.9 |
| Race/ethnicity, %* | ||||||||
| White | 86.8 | 87.9 | 87.2 | 87.9 | 87.0 | 87.2 | 87.5 | 88.4 |
| Black | 7.1 | 6.8 | 7.0 | 6.5 | 7.2 | 7.0 | 6.8 | 6.6 |
| Asian American | 1.9 | 1.6 | 1.9 | 1.8 | 1.7 | 1.6 | 1.8 | 1.4 |
| Hispanic | 2.5 | 2.0 | 2.3 | 2.2 | 2.1 | 2.1 | 1.9 | 1.5 |
| Other | 1.7 | 1.7 | 1.6 | 1.6 | 2.0 | 2.1 | 2.0 | 2.2 |
| Initiation of high‐intensity statin, % | 27.7 | 27.6 | 28.6 | 28.2 | 27.4 | 35.3 | 41.8 | 53.2 |
| Preindex statin fill characteristics, % | ||||||||
| History of CHD | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| History of DM | 27.2 | 27.4 | 26.7 | 26.9 | 28.0 | 28.2 | 28.0 | 28.3 |
| History of stroke | 2.5 | 2.2 | 2.2 | 2.3 | 2.0 | 2.1 | 1.9 | 1.7 |
| History of peripheral artery disease | 7.4 | 7.4 | 7.2 | 6.8 | 8.7 | 8.8 | 8.4 | 8.6 |
| History of HF | 26.4 | 25.8 | 25.7 | 25.0 | 26.0 | 26.5 | 27.0 | 27.4 |
| History of CKD | 19.1 | 20.4 | 21.2 | 21.7 | 23.4 | 25.3 | 25.9 | 28.1 |
| History of dementia | 6.3 | 6.7 | 6.7 | 6.7 | 7.4 | 5.7 | 5.1 | 4.6 |
| Depression | 20.2 | 19.5 | 19.8 | 19.8 | 21.1 | 21.2 | 21.8 | 22.4 |
| Taking antihypertensive medication | ||||||||
| No | 33.8 | 34.6 | 35.7 | 36.2 | 35.9 | 35.9 | 35.7 | 34.6 |
| Yes, with low adherence | 14.8 | 14.6 | 14.2 | 14.0 | 14.1 | 13.9 | 13.0 | 12.5 |
| Yes, with high adherence | 51.4 | 50.8 | 50.1 | 49.8 | 50.0 | 50.2 | 51.3 | 52.9 |
| Taking nonstatin lipid‐lowering medication | 13.3 | 9.4 | 8.7 | 8.6 | 8.0 | 7.3 | 7.0 | 7.1 |
| Postindex statin fill characteristics, % | ||||||||
| New diagnosis of CHD | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| New diagnosis of DM | 2.0 | 1.9 | 1.8 | 1.7 | 1.6 | 1.4 | 1.5 | 1.5 |
| New diagnosis of stroke | 1.3 | 1.6 | 1.4 | 1.4 | 1.3 | 1.2 | 1.2 | 1.3 |
| New diagnosis of HF | 6.3 | 6.5 | 6.1 | 5.5 | 5.3 | 5.3 | 5.1 | 5.6 |
| New diagnosis of CKD | 4.1 | 4.0 | 4.3 | 4.2 | 3.9 | 4.0 | 4.1 | 4.3 |
| New diagnosis of dementia | 1.7 | 1.6 | 1.7 | 1.7 | 1.4 | 1.5 | 1.5 | 1.5 |
| Cardiologist care | 74.2 | 75.3 | 75.5 | 75.7 | 75.9 | 77.9 | 78.2 | 79.3 |
| Number of medications taken | ||||||||
| <5 | 9.8 | 10.8 | 11.2 | 11.8 | 11.8 | 11.4 | 11.4 | 10.8 |
| 5–9 | 45.6 | 45.3 | 46.4 | 46.1 | 45.9 | 45.8 | 44.7 | 44.8 |
| ≥10 | 44.6 | 43.9 | 42.4 | 42.1 | 42.4 | 42.9 | 43.9 | 44.5 |
CHD indicates coronary heart disease; CKD, chronic kidney disease: DM, diabetes mellitus; HF, heart failure; MI, myocardial infarction.
Limited to patients in Medicare.
Table 6.
Characteristics of Patients Initiating a Statin With DM Without a History of CHD in 2007–2014
| Calendar Year | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| n | 61 134 | 67 636 | 83 808 | 84 985 | 90 929 | 79 979 | 73 522 | 68 056 |
| Age, % | ||||||||
| 21–44 y | 15.7 | 16.0 | 17.5 | 18.1 | 17.7 | 17.0 | 16.5 | 15.2 |
| 45–54 y | 32.3 | 32.2 | 33.2 | 32.8 | 32.7 | 32.3 | 31.7 | 31.2 |
| 55–64 y | 43.5 | 43.4 | 42.5 | 42.9 | 43.6 | 43.9 | 44.0 | 44.5 |
| 66–70 y | 2.9 | 2.9 | 2.3 | 2.2 | 2.1 | 2.5 | 2.9 | 3.3 |
| 71–75 y | 2.3 | 2.3 | 1.9 | 1.8 | 1.7 | 1.9 | 2.1 | 2.6 |
| 76–80 y | 1.7 | 1.7 | 1.3 | 1.1 | 1.1 | 1.2 | 1.4 | 1.6 |
| 81–85 y | 1.0 | 1.0 | 0.9 | 0.8 | 0.7 | 0.7 | 0.8 | 1.0 |
| ≥86 y | 0.5 | 0.5 | 0.4 | 0.4 | 0.4 | 0.4 | 0.5 | 0.6 |
| Male sex, % | 48.3 | 48.1 | 48.7 | 49.8 | 49.5 | 49.6 | 49.9 | 49.8 |
| Race/ethnicity, %* | ||||||||
| White | 71.2 | 74.2 | 73.7 | 72.8 | 72.9 | 73.2 | 74.1 | 74.2 |
| Black | 16.0 | 14.2 | 14.1 | 14.2 | 13.9 | 13.4 | 13.5 | 13.9 |
| Asian American | 4.0 | 3.6 | 3.8 | 3.8 | 4.4 | 4.3 | 3.6 | 3.3 |
| Hispanic | 5.5 | 5.1 | 5.1 | 6.0 | 5.1 | 5.4 | 5.0 | 4.4 |
| Other | 3.3 | 3.0 | 3.3 | 3.2 | 3.7 | 3.7 | 3.7 | 4.1 |
| Initiation of high‐intensity statin, % | 9.1 | 10.2 | 10.2 | 9.8 | 10.3 | 12.1 | 12.0 | 15.5 |
| Preindex statin fill characteristics, % | ||||||||
| History of CHD | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| History of DM | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| History of stroke | 1.4 | 1.4 | 1.3 | 1.4 | 1.4 | 1.5 | 1.5 | 1.7 |
| History of peripheral artery disease | 0.7 | 0.7 | 0.7 | 0.7 | 0.7 | 0.7 | 0.8 | 0.9 |
| History of HF | 1.3 | 1.3 | 1.1 | 1.1 | 1.2 | 1.2 | 1.2 | 1.3 |
| History of CKD | 3.7 | 4.0 | 4.1 | 4.5 | 4.8 | 5.1 | 5.4 | 6.2 |
| History of dementia | 0.5 | 0.6 | 0.5 | 0.4 | 0.4 | 0.4 | 0.4 | 0.5 |
| Depression | 23.2 | 22.7 | 22.4 | 22.7 | 22.9 | 23.2 | 23.6 | 23.6 |
| Taking antihypertensive medication | ||||||||
| No | 32.5 | 34.2 | 34.5 | 36.4 | 35.9 | 36.3 | 35.3 | 34.2 |
| Yes, with low adherence | 20.3 | 20.6 | 21.7 | 21.2 | 20.9 | 20.3 | 19.7 | 19.4 |
| Yes, with high adherence | 47.1 | 45.3 | 43.8 | 42.5 | 43.2 | 43.4 | 45.0 | 46.4 |
| Taking nonstatin lipid‐lowering medication | 25.3 | 20.4 | 17.6 | 16.6 | 15.1 | 13.8 | 13.2 | 12.5 |
| Postindex statin fill characteristics, % | ||||||||
| New diagnosis of CHD | 2.6 | 2.7 | 2.5 | 2.3 | 2.4 | 2.2 | 2.4 | 2.4 |
| New diagnosis of DM | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| New diagnosis of stroke | 0.3 | 0.4 | 0.4 | 0.4 | 0.4 | 0.4 | 0.4 | 0.4 |
| New diagnosis of HF | 0.6 | 0.6 | 0.6 | 0.5 | 0.5 | 0.5 | 0.6 | 0.5 |
| New diagnosis of CKD | 1.3 | 1.6 | 1.6 | 1.6 | 1.7 | 1.8 | 1.9 | 2.0 |
| New diagnosis of dementia | 0.2 | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 |
| Cardiologist care | 7.7 | 8.1 | 7.7 | 7.6 | 7.8 | 8.2 | 8.9 | 9.3 |
| Number of medications taken | ||||||||
| <5 | 22.9 | 23.9 | 24.1 | 25.3 | 25.6 | 25.2 | 24.1 | 22.9 |
| 5–9 | 47.2 | 47.2 | 47.5 | 47.3 | 47.2 | 47.0 | 47.2 | 46.2 |
| ≥10 | 30.0 | 28.9 | 28.4 | 27.3 | 27.2 | 27.8 | 28.8 | 30.9 |
CHD indicates coronary heart disease; CKD, chronic kidney disease; DM, diabetes mellitus; HF, heart failure; MI, myocardial infarction.
Limited to patients in Medicare.
Table 7.
Characteristics of Patients Initiating a Statin Without a History of CHD or DM in 2007–2014
| Calendar Year | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| n | 239 058 | 258 626 | 325 082 | 321 807 | 328 819 | 282 255 | 265 499 | 223 722 |
| Age, % | ||||||||
| 21–44 y | 17.2 | 17.0 | 17.9 | 18.0 | 17.9 | 17.6 | 17.3 | 15.7 |
| 45–54 y | 35.8 | 35.6 | 35.9 | 35.7 | 35.5 | 34.6 | 34.1 | 32.1 |
| 55–64 y | 41.7 | 41.9 | 41.8 | 42.2 | 42.6 | 43.1 | 43.4 | 45.0 |
| 66–70 y | 1.8 | 1.9 | 1.5 | 1.4 | 1.4 | 1.7 | 1.9 | 2.6 |
| 71–75 y | 1.4 | 1.5 | 1.2 | 1.1 | 1.0 | 1.3 | 1.4 | 2.0 |
| 76–80 y | 1.1 | 1.1 | 0.8 | 0.7 | 0.7 | 0.8 | 0.9 | 1.2 |
| 81–85 y | 0.7 | 0.7 | 0.5 | 0.5 | 0.5 | 0.6 | 0.6 | 0.7 |
| ≥86 y | 0.4 | 0.4 | 0.3 | 0.3 | 0.3 | 0.4 | 0.4 | 0.5 |
| Male sex, % | 49.9 | 49.4 | 50.3 | 50.6 | 50.6 | 50.7 | 51.0 | 51.6 |
| Race/ethnicity, %* | ||||||||
| White | 83.0 | 84.3 | 84.6 | 83.9 | 84.2 | 84.8 | 85.2 | 85.0 |
| Black | 8.0 | 7.6 | 7.1 | 7.2 | 7.3 | 6.9 | 6.9 | 7.4 |
| Asian American | 3.5 | 3.1 | 3.1 | 3.4 | 3.3 | 3.0 | 2.8 | 2.6 |
| Hispanic | 3.2 | 2.9 | 2.9 | 3.0 | 3.1 | 2.8 | 2.6 | 1.8 |
| Other | 2.3 | 2.0 | 2.3 | 2.5 | 2.0 | 2.5 | 2.6 | 3.2 |
| Initiation of high‐intensity statin, % | 6.9 | 7.9 | 7.7 | 7.4 | 8.1 | 9.9 | 10.3 | 12.9 |
| Preindex statin fill characteristics, % | ||||||||
| History of CHD | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| History of DM | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| History of stroke | 0.9 | 0.9 | 0.9 | 1.0 | 1.2 | 1.2 | 1.2 | 1.3 |
| History of peripheral artery disease | 0.4 | 0.4 | 0.3 | 0.3 | 0.3 | 0.3 | 0.4 | 0.4 |
| History of HF | 0.4 | 0.4 | 0.4 | 0.4 | 0.4 | 0.4 | 0.5 | 0.5 |
| History of CKD | 1.0 | 1.2 | 1.2 | 1.4 | 1.5 | 1.6 | 1.7 | 2.0 |
| History of dementia | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 |
| Depression | 23.2 | 22.9 | 22.8 | 23.0 | 23.2 | 23.5 | 23.7 | 23.7 |
| Taking antihypertensive medication | ||||||||
| No | 55.6 | 55.9 | 57.2 | 57.9 | 58.2 | 58.0 | 57.6 | 56.0 |
| Yes, with low adherence | 12.8 | 13.0 | 13.1 | 12.9 | 12.8 | 12.6 | 12.3 | 12.8 |
| Yes, with high adherence | 31.6 | 31.1 | 29.7 | 29.2 | 29.0 | 29.4 | 30.1 | 31.2 |
| Taking nonstatin lipid‐lowering medication | 21.0 | 14.8 | 11.5 | 10.3 | 9.1 | 8.1 | 7.5 | 7.0 |
| Postindex statin fill characteristics, % | ||||||||
| New diagnosis of CHD | 1.8 | 1.8 | 1.7 | 1.7 | 1.6 | 1.7 | 1.8 | 2.0 |
| New diagnosis of DM | 2.1 | 2.0 | 2.1 | 2.1 | 2.2 | 2.2 | 2.4 | 2.7 |
| New diagnosis of stroke | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.3 | 0.3 |
| New diagnosis of HF | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.3 |
| New diagnosis of CKD | 0.4 | 0.5 | 0.5 | 0.5 | 0.5 | 0.6 | 0.7 | 0.8 |
| New diagnosis of dementia | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 |
| Cardiologist care | 7.7 | 8.0 | 7.8 | 7.8 | 7.8 | 8.7 | 9.3 | 10.2 |
| Number of medications taken | ||||||||
| <5 | 53.1 | 53.9 | 54.7 | 55.3 | 56.0 | 55.1 | 54.6 | 52.7 |
| 5–9 | 34.9 | 34.7 | 34.3 | 33.9 | 33.5 | 33.9 | 34.2 | 34.9 |
| ≥10 | 12.0 | 11.4 | 11.0 | 10.8 | 10.5 | 10.9 | 11.2 | 12.4 |
CHD indicates coronary heart disease; CKD, chronic kidney disease; DM, diabetes mellitus; HF, heart failure; MI, myocardial infarction.
Limited to patients in Medicare.
Trends in Persistence, Adherence, and PDC From 2007 Through 2014
Persistence with statin therapy was within 2 percentage points across calendar years among patients initiating a statin following an MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus (Figure 2). High adherence to statin therapy increased from 57.9% in 2007 to 63.8% in 2014 among patients who initiated a statin following an MI and from 34.9% in 2007 to 37.6% in 2014 among those with diabetes mellitus without a history of CHD, but there was no evidence of a change in high adherence (35.7% in 2007 and 36.8% in 2014) among patients without a history of CHD or diabetes mellitus (Figure 3). The mean PDC for statins increased between 2007 and 2014 among patients initiating treatment following an MI and with diabetes mellitus without a history of CHD but not among those without a history of CHD or diabetes mellitus (Figure 4).
Figure 2.
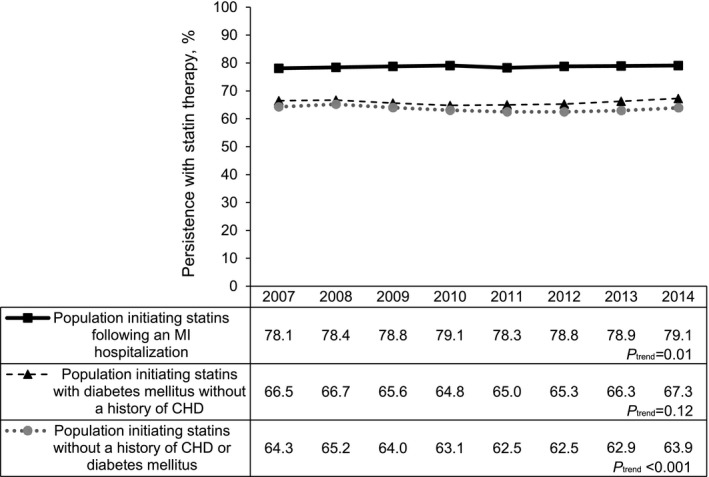
Persistence with statin therapy between 2007 and 2014. The P value comparing trends in persistence with statin therapy among patients initiating a statin following MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus was <0.001. CHD indicates coronary heart disease; MI, myocardial infarction.
Figure 3.
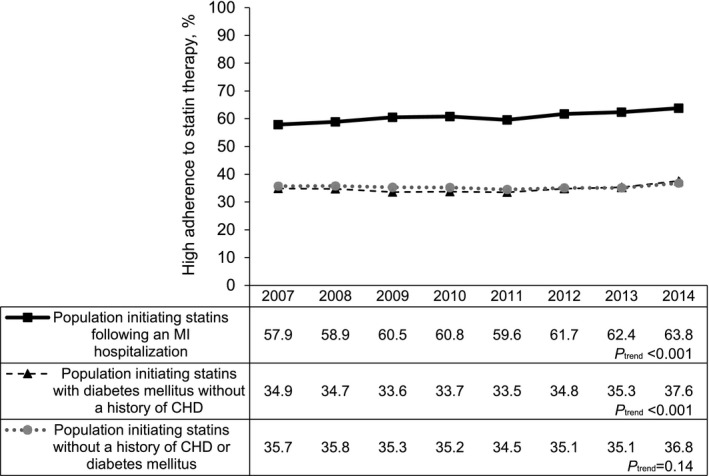
High adherence to statin therapy between 2007 and 2014. The P value comparing trends in high adherence to statin therapy among patients initiating a statin following MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus was <0.001. CHD indicates coronary heart disease; MI, myocardial infarction.
Figure 4.
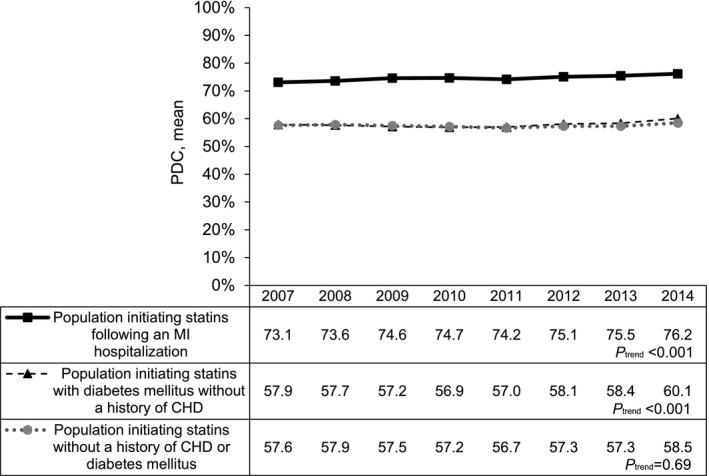
PDC for statins between 2007 and 2014. The P value comparing trends in mean PDC for statins among patients initiating a statin following MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus was <0.001. CHD indicates coronary heart disease; MI, myocardial infarction; PDC, proportion of days covered.
Factors Associated With High Statin Persistence, Adherence, and PDC in 2014
After multivariable adjustment, patients who initiated a statin following an MI were more likely to have high adherence, whereas patients with diabetes mellitus without CHD were less likely to have high adherence, each compared with their counterparts without a history of CHD or diabetes mellitus (Figure 5). In addition, male sex, a history of stroke and dementia, depression, nonstatin lipid‐lowering medication use before the index statin fill, a new diagnosis of CHD and diabetes mellitus, cardiologist care, and taking more medications after the index statin fill were each associated with higher likelihood of having high statin adherence. Black and Hispanic patients compared with white patients; patients initiating a high‐intensity dosage; those with a history of diabetes mellitus, peripheral artery disease, HF or CKD; and those with a new diagnosis of HF or CKD after their index statin fill were less likely to have high adherence to statin therapy. Patients aged 66 to 75 years were more likely to have high adherence to statins, whereas those aged 21 to 54 years were less likely to have high adherence, each compared with their counterparts aged 55 to 64 years. Patients taking antihypertensive medication with high adherence were more likely, whereas those taking antihypertensive medication with low adherence were less likely, to have high statin adherence compared with their counterparts not taking antihypertensive medication before their index statin fill. Patient characteristics associated with persistence with statin therapy and mean PDC for statins after multivariable adjustment are shown in Figures 6 and 7.
Figure 5.
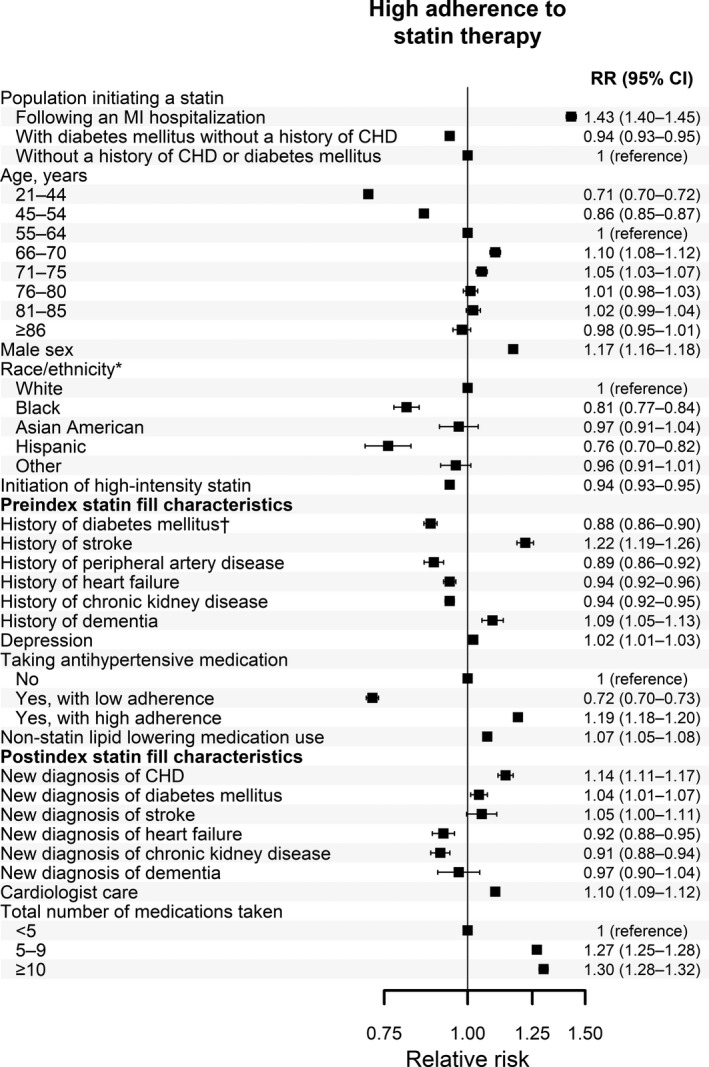
Patient characteristics associated with high adherence to statin therapy in 2014. *Limited to patients in Medicare. †Limited to patients initiating statin therapy following an MI hospitalization. RRs include adjustment for all variables in the figure simultaneously. CHD indicates coronary heart disease; MI, myocardial infarction; RR, relative risk.
Figure 6.
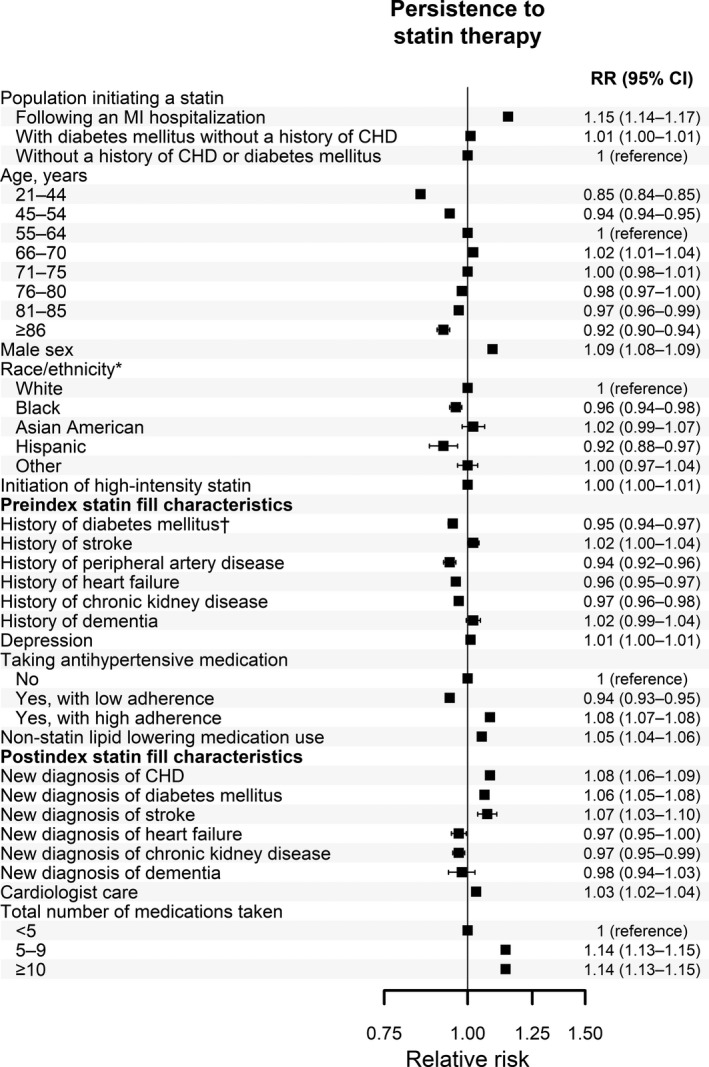
Patient characteristics associated with persistence with statin therapy in 2014. *Limited to patients in Medicare. †Limited to patients initiating statin therapy following an MI hospitalization. RRs for persistence with statin therapy include adjustment for all variables in the figure simultaneously. CHD indicates coronary heart disease; MI, myocardial infarction; RR, relative risk.
Figure 7.
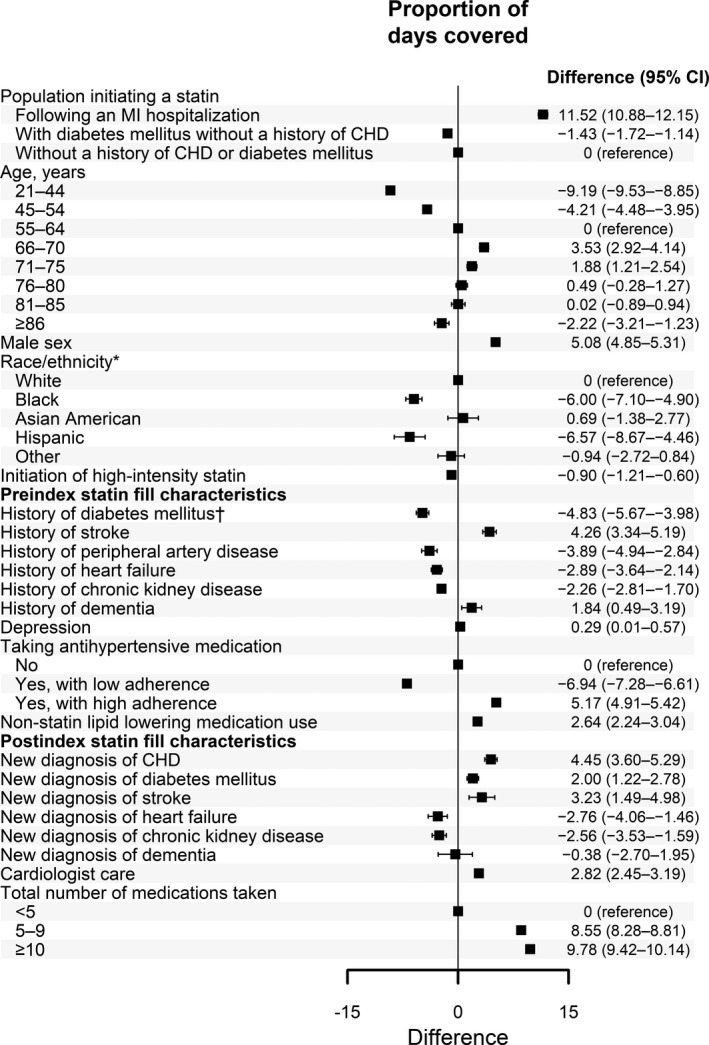
Patient characteristics associated with PDC for statins in 2014. *Limited to patients in Medicare. †Limited to patients initiating statin therapy following an MI hospitalization. Differences in PDC for statins include adjustment for all variables in the figure simultaneously. CHD indicates coronary heart disease; MI, myocardial infarction; PDC, proportion of days covered.
Discussion
Persistence with statin therapy remained similar between 2007 and 2014 among patients initiating treatment following an MI, patients with diabetes mellitus without a history of CHD, and patients without a history of CHD or diabetes mellitus. Between 2007 and 2014, high adherence to statin therapy and the mean PDC for statins increased among patients who initiated treatment following an MI and who had diabetes mellitus without a history of CHD but remained similar among patients without a history of CHD or diabetes mellitus. In 2014, only 63.8% of patients initiating a statin following an MI and <40% of those with diabetes mellitus without a history of CHD and those without a history of CHD or diabetes mellitus took this medication with high adherence. Initiating statin therapy following an MI, having a history of stroke, previously using antihypertensive medication with high adherence, and receiving cardiologist care were associated with higher statin adherence. Age <55 years, black and Hispanic versus white race/ethnicity, and prior use of antihypertensive medication with low adherence were associated with lower adherence to statin therapy following initiation.
Prior studies have suggested improvements in adherence to statin therapy following an MI over the past 25 years.33, 34 Choudhry et al reported that high adherence to statin therapy following an MI, defined by a PDC ≥80% within 365 days after discharge, increased from 38.6% in 1995 to 56.2% in 2003 among Medicare beneficiaries with low income in Pennsylvania and New Jersey.33 In a prior analysis, we reported an increase in adherence to high‐intensity statin therapy among Medicare beneficiaries who filled a high‐intensity statin dosage following an MI between 2007 and 2012.34 However, these 2 prior analyses included prevalent statin users, a subgroup of patients who have been shown to have higher adherence to statins compared with new users.35 In the current analysis of statin initiators, high adherence to statin therapy following an MI increased between 2007 and 2014. As we hypothesized, patients with diabetes mellitus without a history of CHD and patients without a history of CHD or diabetes mellitus initiating a statin had lower adherence compared with their counterparts who initiated this medication following MI. This finding may be explained by patients without a history of CHD perceiving that they have a low absolute risk for CHD events.
Results from the current analysis highlight the need to improve persistence with and adherence to statin therapy if the CHD risk reduction benefits of statins demonstrated in clinical trials are to be translated into clinical practice. In 2017, the European Society of Cardiology working group on cardiovascular pharmacotherapy published a position paper calling for comprehensive efforts to improve adherence to statin therapy in clinical practice.36 The working group called for personalized programs to empower patients to become informed medication consumers. These programs could include interventions that have been shown to increase statin adherence in clinical trials, including regular follow‐up visits, reward systems, and telephone or pharmacy reminders.12, 13, 14, 36 The working group also highlighted the need to strengthen efforts to accurately identify patients who have adverse statin side effects and the importance of stressing the benefits of statins to overcome media stories and misperception about the safety of statins among members of the public.
In the current study, several patient characteristics were associated with lower persistence with and adherence to statin therapy. These results could be used to identify patients who are more likely to benefit from interventions that can increase statin adherence. Regular follow‐up visits with healthcare professionals could improve persistence with and adherence to statin therapy because these provide an opportunity to identify reasons for low statin adherence or discontinuation, including side effects, perceived lack of benefit, and cost issues, and to reinforce the benefits of this medication for preventing CHD events.3, 36, 37, 38, 39 Prior studies have shown that many patients who discontinue statins due to side effects can be successfully re‐challenged and remain on treatment with high adherence.40, 41, 42 Other interventions, including nurse‐led cardiovascular risk factor counseling, drug‐regimen simplification, reminders, and phone calls, may also be effective for increasing statin adherence.43
Low adherence to antihypertensive medication was associated with lower persistence with and adherence to statin therapy in the current study. We analyzed adherence to antihypertensive medications because they are commonly used among US adults.31 However, having low adherence to other medications may also be a marker for low statin persistence and adherence. Reasons for low adherence that are common among different classes of medications include cost issues, cultural beliefs and perceived lack of need of treatment in general, and fear of toxicity or adverse effects.44 Therefore, clinicians should be aware that patients initiating statins who have low adherence to any other medication may be more likely to discontinue or to have low adherence to statin therapy.
Statin discontinuation may also result from medical reasons including contraindications.45, 46 In previous studies in the United States and Switzerland, the reason most frequently reported by patients for discontinuation of evidence‐based medications for CHD including statins was physician recommendation.47, 48 Using Medicare data, Schroeder et al reported that patients followed by cardiologists were more likely to fill a statin after an MI compared with those without cardiologist care.49 Consistent with this finding, patients in the current analysis who received cardiologist care in the 182 days following statin initiation were more likely to take this medication with high adherence compared with their counterparts who did not receive cardiologist care. These results suggest that physician characteristics, including specialty, may also play a role in persistence with and adherence to statin therapy among patients. Increasing physicians’ awareness and providing them with guidance and tools to identify and manage barriers to statin treatment, particularly among noncardiologists, may contribute to improvement of statin adherence and persistence in clinical practice.
The current analysis has several strengths. We used data from younger patients with commercial health insurance in MarketScan and older patients with Medicare coverage, thereby providing a high degree of generalizability to US adults initiating statin therapy. In addition, the large sample size provided adequate statistical power to investigate patient characteristics associated with statin adherence. The current study also has potential limitations. Misclassification of statin use in the current analysis is possible, given that pharmacy fills indicate only whether the patient filled a prescription, not whether they took it.50 Also, pharmacy fills in MarketScan and Medicare may not include all medications filled by patients. Therefore, the current analyses may underestimate persistence with and adherence to statin therapy if some patients paid for low‐cost generic statins using a discount drug program from a major retail pharmacy chain without submitting a pharmacy claim.51 However, we have previously reported that there is substantial agreement in lipid‐lowering medication use defined by Medicare pharmacy claims and self‐report or a medication inventory and that the agreement is similar for branded and generic statins.52 Reasons for statin initiation or discontinuation are not available in the MarketScan and Medicare databases. The observational study design prevents inferring a causal association between patient characteristics and statin adherence. Given the large sample size, clinical judgment is needed when interpreting the relevance of findings that were statistically significant in the current study.
In conclusion, results from the present study indicate that persistence with and adherence to statin therapy remain low, particularly among patients initiating treatment without a history of CHD. Low persistence with and adherence to statin therapy constitute major concerns because they are associated with substantial residual risk for CHD events. Healthcare providers should monitor statin use following initiation of treatment and work with patients to identify barriers to taking this medication with high adherence.
Sources of Funding
The design and conduct of the study, analysis, and interpretation of the data, and preparation of the article were supported through a research grant from Amgen Inc.
Disclosures
Rosenson, Farkouh, Safford, and Muntner receive research support from Amgen. Rosenson also receives research support from Akcea, AstraZeneca, Medicines Company, and Regeneron; provides advisory and consulting services for Amgen, C5, CVS Caremark, Regeneron, and Sanofi; receives honoraria from Akcea, Kowa, and Pfizer; receives royalties from UpToDate; and is a stockholder of MediMergent. Monda, Philip, and Mues are employed by and are stockholders of Amgen. The remaining authors have no disclosures to report.
Acknowledgments
The academic authors conducted all analyses and maintained the rights to publish this article.
(J Am Heart Assoc. 2019;8:e010376 DOI: 10.1161/JAHA.118.010376.)
References
- 1. Fulcher J, O'Connell R, Voysey M, Emberson J, Blackwell L, Mihaylova B, Simes J, Collins R, Kirby A, Colhoun H, Braunwald E, La Rosa J, Pedersen TR, Tonkin A, Davis B, Sleight P, Franzosi MG, Baigent C, Keech A. Efficacy and safety of LDL‐lowering therapy among men and women: meta‐analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015;385:1397–1405. [DOI] [PubMed] [Google Scholar]
- 2. Taylor F, Ward K, Moore TH, Burke M, Davey Smith G, Casas JP, Ebrahim S. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011;1:CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–S45. [DOI] [PubMed] [Google Scholar]
- 4. Gomez Sandoval YH, Braganza MV, Daskalopoulou SS. Statin discontinuation in high‐risk patients: a systematic review of the evidence. Curr Pharm Des. 2011;17:3669–3689. [DOI] [PubMed] [Google Scholar]
- 5. Bitton A, Choudhry NK, Matlin OS, Swanton K, Shrank WH. The impact of medication adherence on coronary artery disease costs and outcomes: a systematic review. Am J Med. 2013;126:357.e7–357.e27. [DOI] [PubMed] [Google Scholar]
- 6. Hirsh BJ, Smilowitz NR, Rosenson RS, Fuster V, Sperling LS. Utilization of and adherence to guideline‐recommended lipid‐lowering therapy after acute coronary syndrome: opportunities for improvement. J Am Coll Cardiol. 2015;66:184–192. [DOI] [PubMed] [Google Scholar]
- 7. Penning‐van Beest FJ, Termorshuizen F, Goettsch WG, Klungel OH, Kastelein JJ, Herings RM. Adherence to evidence‐based statin guidelines reduces the risk of hospitalizations for acute myocardial infarction by 40%: a cohort study. Eur Heart J. 2007;28:154–159. [DOI] [PubMed] [Google Scholar]
- 8. Schultz JS, O'Donnell JC, McDonough KL, Sasane R, Meyer J. Determinants of compliance with statin therapy and low‐density lipoprotein cholesterol goal attainment in a managed care population. Am J Manag Care. 2005;11:306–312. [PubMed] [Google Scholar]
- 9. Chan DC, Shrank WH, Cutler D, Jan S, Fischer MA, Liu J, Avorn J, Solomon D, Brookhart MA, Choudhry NK. Patient, physician, and payment predictors of statin adherence. Med Care. 2010;48:196–202. [DOI] [PubMed] [Google Scholar]
- 10. Salami JA, Warraich H, Valero‐Elizondo J, Spatz ES, Desai NR, Rana JS, Virani SS, Blankstein R, Khera A, Blaha MJ, Blumenthal RS, Lloyd‐Jones D, Nasir K. National Trends in Statin Use and Expenditures in the US Adult Population From 2002 to 2013: Insights From the Medical Expenditure Panel Survey. JAMA Cardiol. 2017;2:56–65. [DOI] [PubMed] [Google Scholar]
- 11. Bittner V, Deng L, Rosenson RS, Taylor B, Glasser SP, Kent ST, Farkouh ME, Muntner P. Trends in the Use of Nonstatin Lipid‐Lowering Therapy Among Patients With Coronary Heart Disease: A Retrospective Cohort Study in the Medicare Population 2007 to 2011. J Am Coll Cardiol. 2015;66:1864–1872. [DOI] [PubMed] [Google Scholar]
- 12. Stacy JN, Schwartz SM, Ershoff D, Shreve MS. Incorporating tailored interactive patient solutions using interactive voice response technology to improve statin adherence: results of a randomized clinical trial in a managed care setting. Popul Health Manag. 2009;12:241–254. [DOI] [PubMed] [Google Scholar]
- 13. Nieuwkerk PT, Nierman MC, Vissers MN, Locadia M, Greggers‐Peusch P, Knape LP, Kastelein JJ, Sprangers MA, de Haes HC, Stroes ES. Intervention to improve adherence to lipid‐lowering medication and lipid‐levels in patients with an increased cardiovascular risk. Am J Cardiol. 2012;110:666–672. [DOI] [PubMed] [Google Scholar]
- 14. Eussen SR, van der Elst ME, Klungel OH, Rompelberg CJ, Garssen J, Oosterveld MH, de Boer A, de Gier JJ, Bouvy ML. A pharmaceutical care program to improve adherence to statin therapy: a randomized controlled trial. Ann Pharmacother. 2010;44:1905–1913. [DOI] [PubMed] [Google Scholar]
- 15. Mondesir FL, Brown TM, Muntner P, Durant RW, Carson AP, Safford MM, Levitan EB. Diabetes, diabetes severity, and coronary heart disease risk equivalence: REasons for Geographic and Racial Differences in Stroke (REGARDS). Am Heart J. 2016;181:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Colantonio LD, Levitan EB, Yun H, Kilgore ML, Rhodes JD, Howard G, Safford MM, Muntner P. Use of Medicare claims data for the identification of myocardial infarction: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Med Care. 2018;56:1051–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kent ST, Safford MM, Zhao H, Levitan EB, Curtis JR, Kilpatrick RD, Kilgore ML, Muntner P. Optimal Use of Available Claims to Identify a Medicare Population Free of Coronary Heart Disease. Am J Epidemiol. 2015;182:808–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Culler SD, Kugelmass AD, Brown PP, Reynolds MR, Simon AW. Trends in coronary revascularization procedures among Medicare beneficiaries between 2008 and 2012. Circulation. 2015;131:362–370. [DOI] [PubMed] [Google Scholar]
- 19. Gandra SR, Lawrence LW, Parasuraman BM, Darin RM, Sherman JJ, Wall JL. Total and component health care costs in a non‐Medicare HMO population of patients with and without type 2 diabetes and with and without macrovascular disease. J Manag Care Pharm. 2006;12:546–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kumamaru H, Judd SE, Curtis JR, Ramachandran R, Hardy NC, Rhodes JD, Safford MM, Kissela BM, Howard G, Jalbert JJ, Brott TG, Setoguchi S. Validity of claims‐based stroke algorithms in contemporary Medicare data: REasons for Geographic And Racial Differences in Stroke (REGARDS) study linked with medicare claims. Circ Cardiovasc Qual Outcomes. 2014;7:611–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hirsch AT, Hartman L, Town RJ, Virnig BA. National health care costs of peripheral arterial disease in the Medicare population. Vasc Med. 2008;13:209–215. [DOI] [PubMed] [Google Scholar]
- 22. Harris TJ, Zafar AM, Murphy TP. Utilization of lower extremity arterial disease diagnostic and revascularization procedures in Medicare beneficiaries 2000‐2007. AJR Am J Roentgenol. 2011;197:W314–W317. [DOI] [PubMed] [Google Scholar]
- 23. Schneider KM, O'Donnell BE, Dean D. Prevalence of multiple chronic conditions in the United States’ Medicare population. Health Qual Life Outcomes. 2009;7:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Muntner P, Gutierrez OM, Zhao H, Fox CS, Wright NC, Curtis JR, McClellan W, Wang H, Kilgore M, Warnock DG, Bowling CB. Validation study of medicare claims to identify older US adults with CKD using the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Kidney Dis. 2015;65:249–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vlasschaert ME, Bejaimal SA, Hackam DG, Quinn R, Cuerden MS, Oliver MJ, Iansavichus A, Sultan N, Mills A, Garg AX. Validity of administrative database coding for kidney disease: a systematic review. Am J Kidney Dis. 2011;57:29–43. [DOI] [PubMed] [Google Scholar]
- 26. Taylor DH Jr, Ostbye T, Langa KM, Weir D, Plassman BL. The accuracy of Medicare claims as an epidemiological tool: the case of dementia revisited. J Alzheimers Dis. 2009;17:807–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hwang S, Jayadevappa R, Zee J, Zivin K, Bogner HR, Raue PJ, Bruce ML, Reynolds CF III, Gallo JJ. Concordance Between Clinical Diagnosis and Medicare Claims of Depression Among Older Primary Care Patients. Am J Geriatr Psychiatry. 2015;23:726–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Noyes K, Liu H, Lyness JM, Friedman B. Medicare beneficiaries with depression: comparing diagnoses in claims data with the results of screening. Psychiatr Serv. 2011;62:1159–1166. [DOI] [PubMed] [Google Scholar]
- 29. Cutrona SL, Toh S, Iyer A, Foy S, Cavagnaro E, Forrow S, Racoosin JA, Goldberg R, Gurwitz JH. Design for validation of acute myocardial infarction cases in Mini‐Sentinel. Pharmacoepidemiol Drug Saf. 2012;21(suppl 1):274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Choudhry NK, Shrank WH, Levin RL, Lee JL, Jan SA, Brookhart MA, Solomon DH. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15:457–464. [PMC free article] [PubMed] [Google Scholar]
- 31. Muntner P, Yun H, Sharma P, Delzell E, Kent ST, Kilgore ML, Farkouh ME, Vupputuri S, Bittner V, Rosenson RS, Levitan EB, Safford MM. Ability of low antihypertensive medication adherence to predict statin discontinuation and low statin adherence in patients initiating treatment after a coronary event. Am J Cardiol. 2014;114:826–831. [DOI] [PubMed] [Google Scholar]
- 32. Barros AJ, Hirakata VN. Alternatives for logistic regression in cross‐sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Choudhry NK, Setoguchi S, Levin R, Winkelmayer WC, Shrank WH. Trends in adherence to secondary prevention medications in elderly post‐myocardial infarction patients. Pharmacoepidemiol Drug Saf. 2008;17:1189–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Colantonio LD, Huang L, Monda KL, Bittner V, Serban MC, Taylor B, Brown TM, Glasser SP, Muntner P, Rosenson RS. Adherence to high‐intensity statins following a myocardial infarction hospitalization among medicare beneficiaries. JAMA Cardiol. 2017;2:890–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mann DM, Woodward M, Muntner P, Falzon L, Kronish I. Predictors of nonadherence to statins: a systematic review and meta‐analysis. Ann Pharmacother. 2010;44:1410–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vonbank A, Agewall S, Kjeldsen KP, Lewis BS, Torp‐Pedersen C, Ceconi C, Funck‐Brentano C, Kaski JC, Niessner A, Tamargo J, Walther T, Wassmann S, Rosano G, Schmidt H, Saely CH, Drexel H. Comprehensive efforts to increase adherence to statin therapy. Eur Heart J. 2017;38:2473–2479. [DOI] [PubMed] [Google Scholar]
- 37. Benner JS, Tierce JC, Ballantyne CM, Prasad C, Bullano MF, Willey VJ, Erbey J, Sugano DS. Follow‐up lipid tests and physician visits are associated with improved adherence to statin therapy. Pharmacoeconomics. 2004;22(suppl 3):13–23. [DOI] [PubMed] [Google Scholar]
- 38. Bruckert E, Hayem G, Dejager S, Yau C, Begaud B. Mild to moderate muscular symptoms with high‐dosage statin therapy in hyperlipidemic patients–the PRIMO study. Cardiovasc Drugs Ther. 2005;19:403–414. [DOI] [PubMed] [Google Scholar]
- 39. Wei MY, Ito MK, Cohen JD, Brinton EA, Jacobson TA. Predictors of statin adherence, switching, and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol. 2013;7:472–483. [DOI] [PubMed] [Google Scholar]
- 40. Mampuya WM, Frid D, Rocco M, Huang J, Brennan DM, Hazen SL, Cho L. Treatment strategies in patients with statin intolerance: the Cleveland Clinic experience. Am Heart J. 2013;166:597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zhang H, Plutzky J, Skentzos S, Morrison F, Mar P, Shubina M, Turchin A. Discontinuation of statins in routine care settings: a cohort study. Ann Intern Med. 2013;158:526–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Keating AJ, Campbell KB, Guyton JR. Intermittent nondaily dosing strategies in patients with previous statin‐induced myopathy. Ann Pharmacother. 2013;47:398–404. [DOI] [PubMed] [Google Scholar]
- 43. van Driel ML, Morledge MD, Ulep R, Shaffer JP, Davies P, Deichmann R. Interventions to improve adherence to lipid‐lowering medication. Cochrane Database Syst Rev. 2016;12:CD004371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Baroletti S, Dell'Orfano H. Medication adherence in cardiovascular disease. Circulation. 2010;121:1455–1458. [DOI] [PubMed] [Google Scholar]
- 45. Kottke TE, Ogwang Z, Smith JC. Reasons for not meeting coronary artery disease targets of care in ambulatory practice. Perm J. 2010;14:12–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cohen SM, Kataoka‐Yahiro M. Provider adherence to clinical guidelines related to lipid‐lowering medications. Mil Med. 2010;175:122–126. [DOI] [PubMed] [Google Scholar]
- 47. Sud A, Kline‐Rogers EM, Eagle KA, Fang J, Armstrong DF, Rangarajan K, Otten RF, Stafkey‐Mailey DR, Taylor SD, Erickson SR. Adherence to medications by patients after acute coronary syndromes. Ann Pharmacother. 2005;39:1792–1797. [DOI] [PubMed] [Google Scholar]
- 48. Gencer B, Rodondi N, Auer R, Raber L, Klingenberg R, Nanchen D, Carballo D, Vogt P, Carballo S, Meyer P, Matter CM, Windecker S, Luscher TF, Mach F. Reasons for discontinuation of recommended therapies according to the patients after acute coronary syndromes. Eur J Intern Med. 2015;26:56–62. [DOI] [PubMed] [Google Scholar]
- 49. Schroeder MC, Robinson JG, Chapman CG, Brooks JM. Use of statins by Medicare beneficiaries post myocardial infarction: poor physician quality or patient‐centered care? Inquiry. 2015;52:0046958015571131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Krousel‐Wood M, Holt E, Joyce C, Ruiz R, Dornelles A, Webber LS, Morisky DE, Frohlich ED, Re RN, He J, Whelton PK, Muntner P. Differences in cardiovascular disease risk when antihypertensive medication adherence is assessed by pharmacy fill versus self‐report: the Cohort Study of Medication Adherence among Older Adults (CoSMO). J Hypertens. 2015;33:412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Tungol A, Starner CI, Gunderson BW, Schafer JA, Qiu Y, Gleason PP. Generic drug discount programs: are prescriptions being submitted for pharmacy benefit adjudication? J Manag Care Pharm. 2012;18:690–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Colantonio LD, Kent ST, Kilgore ML, Delzell E, Curtis JR, Howard G, Safford MM, Muntner P. Agreement between Medicare pharmacy claims, self‐report, and medication inventory for assessing lipid‐lowering medication use. Pharmacoepidemiol Drug Saf. 2016;25:827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]


