Abstract
Background
Longer transport adversely affects outcomes in out-of-hospital cardiac arrest (OHCA) patients who do not return to spontaneous circulation (ROSC). The aim of this study was to determine the association between the transport time interval (TTI) and neurological outcomes in OHCA patients without ROSC.
Methods
We analyzed adult OHCA patients with presumed cardiac etiology and without prehospital ROSC from 2012 to 2015. The study population was divided into 2 groups according to STI (short STI [1–5 minutes] and long STI [≥ 6 minutes]). The primary exposure was TTI, which was categorized as short (1–5 minutes), intermediate (6–10 minutes), or long (≥ 11 minutes). The primary outcome was a good neurological recovery at discharge. Multiple logistic regression analysis was used in each STI group.
Results
Among 57,822 patients, 23,043 (40%), 20,985 (36%), and 13,794 (24%) were classified as short, intermediate, and long TTI group. A good neurological recovery occurred in 1.0%, 0.6%, and 0.3% of the patients in the short, intermediate and long TTI group, respectively. Among 12,652 patients with short STI, a good neurological recovery occurred in 2.2%, 1.0%, and 0.4% of the patients in the short, intermediate and long TTI group, respectively. Among 45,570 patients with long STI, a good neurological recovery occurred in 0.7%, 0.5%, and 0.3% of the patients in the short, intermediate and long TTI group, respectively. When short TTI was used as a reference, the adjusted odds ratios (AOR) of TTI for good neurological recovery was different between short STI group and long STI group (AOR [95% confidence interval, 0.46 [0.32–0.67] vs. 0.72 [0.59–0.89], respectively, for intermediate TTI and 0.31 [0.17–0.55] vs. 0.49 [0.37–0.65], respectively, for long TTI).
Conclusion
A longer TTI adversely affected the likelihood of a good neurological recovery in OHCA patients without prehospital ROSC. This negative effect was more prominent in short STI group.
Keywords: Out-of-Hospital Cardiac Arrests, Outcomes, Emergency Medical Service
Graphical Abstract
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) is a significant public health problem worldwide.1 The disease burden of OHCA leads to low survival and is frequently associated with neurological damage among survivors.2 The outcomes of OHCA are extremely time-sensitive and are influenced by the quality of prehospital resuscitation.3,4 Emergency medical service (EMS) plays an important role in the management of OHCA patients. EMS is involved in several links of the ‘chain of survival’ in terms of rapid response, immediate high-quality CPR, early defibrillation and basic and advanced prehospital management.5
EMS oversees the transport of patients to the emergency department (ED), where advanced life support and post-arrest care begin. For patients without a return of spontaneous circulation (ROSC), resuscitative efforts during transport is another critical role that EMS plays in the management of OHCA.6,7 In previous studies, a longer transport time interval (TTI) was not associated with the survival of OHCA patients.8,9,10,11 However, several studies have indicated that the quality of CPR during the transport of OHCA patients is likely to be poor,12,13,14 and CPR quality might have differential effects on survival and neurological outcomes in these patients.15,16 Thus, for OHCA patients without prehospital ROSC, a longer TTI could adversely affect their neurological outcome. In addition, negative effects might be aggravated if resuscitation is insufficient in the field because those patients are affected by transport in the early phase of cardiac arrest which is a critical period in the management of OHCA.17,18 Therefore, the effect of TTI on the outcomes of OHCA patients without prehospital ROSC might differ based on the scene time interval (STI).
The aim of this study was to determine the association between TTI and the neurologic outcomes of OHCA patients without prehospital ROSC. We also examined whether the effect of TTI on the neurologic outcomes of OHCA patients without prehospital ROSC differed based on the STI. We hypothesized that a longer TTI adversely affects the neurologic outcomes of OHCA patients without prehospital ROSC and that those negative effects could be aggravated if the STI was short.
METHODS
Study design and setting
This was a cross-sectional study that used a nationwide prospective EMS out-of-hospital cardiac arrest registry in Korea. Since 2006, the National Fire Agency and the Korea Centers for Disease Control (CDC) and Prevention have collaborated to construct a nationwide EMS-assessed OHCA registry as part of the Cardiovascular Disease Surveillance (CAVAS) project. All EMS-assessed OHCA cases were identified from electronically stored patient care records, and a follow-up investigation was performed via a medical record review by an expert from the Korean CDC who visited hospitals to complete an Utstein-style structured survey form. Detailed information and data quality management processes for the registry have been described previously.19,20
Korea established a single-tiered, fire-based public EMS in 1995. The Korean EMS provides basic-to-intermediate ambulance services and supports a population of approximately 50 million.21 An EMS provider can administer CPR at the scene and during transport with automatic external defibrillation and advanced airway management under direct medical control. Advanced cardiac life support is very limited in most areas of the country.21 An EMS provider cannot declare death at the scene or terminate CPR unless there is ROSC. Therefore, all OHCA victims are transported to the ED. The decision to depart from the scene is decided by the EMS provider. Although transfer to the nearest ED is recommended for OHCA patients in the field emergency protocol in Korea, it is not mandatory, and EMS providers can choose an ED according to a family's wishes, the patient's condition, expected transport interval, etc.
Study population
Data were extracted from January 2012 to December 2015. All adults who were older than 18 years and treated by EMS for OHCAs with a presumed cardiac etiology were included. Patients were excluded if the arrest was witnessed by EMS or if prehospital ROSC was achieved. Patients whose time data were ineligible (TTI less than 0 or STI less than 0) or whose TTI was over 30 minutes were also excluded. Patients with missing information on prehospital ROSC, TTI, STI or outcomes at discharge were also excluded.
Outcome measure
The primary outcome was good neurologic recovery (cerebral performance 1 or 2) at discharge,22 and the secondary outcome was survival to hospital discharge. The CPC score was assessed by medical record reviewers based on discharge summary abstracts or documentation in the medical records.
Methods of measurement
The information for TTI (the elapsed time interval from EMS's departure from the scene to arrival at the ED) and STI (the elapsed time interval from EMS's arrival on the scene to its departure from the scene) was obtained from EMS patient care records. TTI was categorized into three groups: short TTI for 1–5 minutes, intermediate TTI for 6–10 minutes, and long TTI for 11 minutes and longer. STI was categorized into two groups: short STI for 1–5 minutes and long STI for 6 minutes and longer. We collected demographic and prehospital variables, including age, gender, medical insurance status (medical aid vs. non-medical aid), location of the arrest (public vs. other), witness status, bystander CPR, initial electrocardiogram (ECG) rhythm (shockable vs. asystole vs. pulseless electrical activity), prehospital defibrillation, prehospital advanced airway placement, prehospital mechanical CPR, response time interval (elapsed time interval from call to EMS arrival on the scene), and prehospital ROSC status (any ROSC before arrival at hospital). Data for in-hospital variables, such as the provision of therapeutic hypothermia (TH), extracorporeal membrane oxygenation (ECMO) and cardiac reperfusion therapy, were also collected. Additionally, we collected the following variables: comorbidities, including hypertension, diabetes mellitus, stroke and heart disease (myocardial infarction and angina pectoris), and community urbanization (metropolitan vs. non-metropolitan) based on a population of one million to adjust for geographical variations in community performance and resources. We divided the EDs into two groups according to the number of OHCA cases they received. EDs with an average of more than 40 OHCA cases per year were defined as high-volume centers, and the others were designated as low-volume centers. This cut-off value of 40 is suggested by the Resuscitation Outcome Consortium (ROC).23
Statistical analysis
The study population was divided into 2 groups according to STI. Demographic findings and outcomes based on STI and TTI are described. Continuous variables were compared via Student’s T-test or the Wilcoxon rank sum test, and categorical variables were compared using the χ2 test or Fischer's exact test. The significance of the trends in TTI was evaluated with the Cochran-Armitage test for dichotomous variables and the Jonckheere-Terpstra test for continuous variables.
Multivariable logistic regression was conducted to analyze the effect of TTI on the outcome and to calculate the adjusted odds ratios (ORs) with 95% confidence intervals (CI) after adjusting for co-variables. The variables included in the model were age, gender, medical insurance status, location of arrest, witness status, bystander CPR, initial ECG rhythm, prehospital defibrillation, prehospital advanced airway,24,25 prehospital mechanical CPR, response time interval, urbanization level, and the volume of center.23,26 We tested multicollinearity between co-variables in the model, and we did not find it in our analysis.
Because we hypothesized that longer TTI would worsen outcomes of patients without prehospital ROSC, we visually assessed if those worsening effects might be offset by visiting a high volume center. Adjusted probabilities of good neurological recovery and survival to discharge were calculated and plotted on the basis of a logistic regression analysis.
Two-sided tests were conducted, and P < 0.05 was considered significant. STATA 13.0 (StataCorp, College Station, TX, USA) and R, version 3.32 (Available at http://www.r-project.org), were used for all analyses.
Ethics statement
This study was performed in compliance with the Declaration of Helsinki. The protocol was approved with by the Institutional Review Board (IRB) of Seoul National University Hospital, who provided a waiver for informed consent (IRB No. 1103-153-357).
RESULTS
Characteristics of study subjects
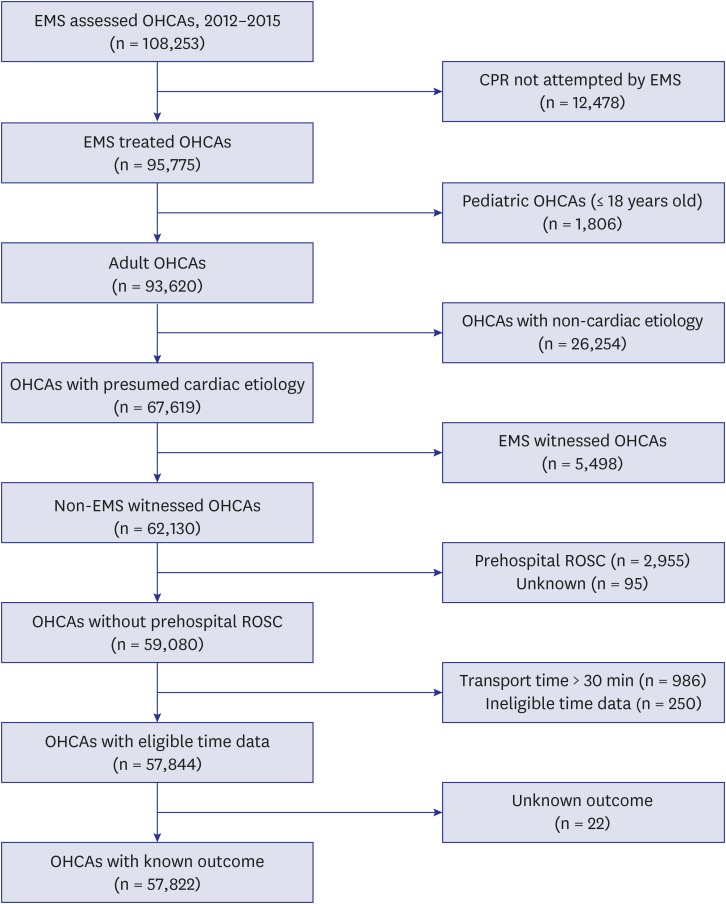
Among the 108,253 EMS-assessed OHCA patients evaluated during the study period, the 57,822 (53%) with a presumed cardiac etiology underlying an arrest that was not witnessed by EMS who did not achieve ROSC prior to hospitalization were analyzed (Fig. 1). This included 12,652 patients in the short STI (21.9%) group and 45,170 (78.1%) in the long STI group.
Fig. 1. Patient flow.
EMS = emergency medical service, OHCA = out-of-hospital cardiac arrest, CPR = cardiopulmonary resuscitation, ROSC = return of spontaneous circulation.
The characteristics of the study population are described according to TTI in Table 1. A total of 23,043 (40%) patients were categorized into the short TTI group, 20,985 (36%) into the intermediate TTI group, and 13,794 (24%) into the long TTI group. TTI was associated with significant increases in EMS response time and decreases in the proportion of patients with a shockable rhythm and urbanization level. Survival to discharge and good neurological recovery were higher in the short TTI group (3.4% and 1.0%, respectively) than in the intermediate TTI group (2.4% and 0.6%, respectively) and the long TTI group (1.3% and 0.3%, respectively; P < 0.001 for both trends).
Table 1. Characteristics of the study population based on transport time interval.
| Characteristics | Transport time interval | P value | P for trend | |||
|---|---|---|---|---|---|---|
| 1–5 min (n = 23,043) | 6–10 min (n = 20,985) | > 10 min (n = 13,794) | ||||
| Age, yr, mean (SD) | 69.3 (15.3) | 70.0 (15.2) | 71.0 (14.7) | < 0.001 | < 0.001 | |
| Men, No. (%) | 14,602 (63.4) | 12,968 (61.8) | 8,674 (62.9) | 0.003 | 0.151 | |
| Past medical history | ||||||
| Diabetes mellitus | 4,933 (21.4) | 4,538 (21.6) | 2,634 (19.1) | < 0.001 | < 0.001 | |
| Hypertension | 7,330 (31.8) | 6,844 (32.6) | 4,063 (29.5) | < 0.001 | < 0.001 | |
| Heart disease | 3,180 (13.8) | 2,957 (14.1) | 1,804 (13.1) | 0.025 | 0.102 | |
| Stroke | 2,008 (8.7) | 1,967 (9.4) | 1,214 (8.8) | 0.039 | 0.503 | |
| Medical aid, No. (%) | 2,050 (8.9) | 1,846 (8.8) | 1,141 (8.3) | 0.103 | 0.051 | |
| Community urbanization, No. (%) | < 0.001 | < 0.001 | ||||
| Metropolitan | 11,367 (49.3) | 10,151 (48.4) | 3,336 (24.2) | |||
| Initial ECG, No. (%) | < 0.001 | < 0.001a | ||||
| Asystole | 17,558 (76.2) | 16,098 (76.7) | 11,042 (80.0) | |||
| PEA | 2,502 (10.9) | 2,337 (11.1) | 1,123 (8.1) | |||
| Shockable rhythm | 2,983 (12.9) | 2,550 (12.2) | 1,629 (11.8) | |||
| Circumstance of arrest, No. (%) | ||||||
| Public location | 4,127 (17.9) | 3,128 (14.9) | 2,189 (15.9) | < 0.001 | < 0.001 | |
| Witnessed | 9,589 (41.6) | 9,027 (43.0) | 5,926 (43.0) | 0.004 | 0.006 | |
| Bystander CPR | 10,790 (46.8) | 9,980 (47.6) | 6,436 (46.7) | 0.175 | 0.981 | |
| Prehospital management, No. (%) | ||||||
| Defibrillation | 4,218 (18.3) | 4,068 (19.4) | 2,937 (21.3) | < 0.001 | < 0.001 | |
| Advanced airway management | 3,272 (14.2) | 3,145 (15.0) | 1,722 (12.5) | < 0.001 | < 0.001 | |
| Mechanical CPR | 83 (0.4) | 93 (0.4) | 73 (0.5) | 0.053 | 0.015 | |
| Elapsed time, median (IQR), min | ||||||
| EMS response time | 6.0 (5.0–8.0) | 7.0 (5.0–10.0) | 9.0 (6.0–14.0) | < 0.001 | < 0.001 | |
| Scene time | 9.0 (6.0–12.0) | 9.0 (6.0–12.0) | 8.0 (5.0–11.0) | < 0.001 | < 0.001 | |
| Transport time | 4.0 (3.0–5.0) | 8.0 (6.0–9.0) | 15.0 (12.0–19.0) | < 0.001 | < 0.001 | |
| Volume of centre, No. (%) | < 0.001 | < 0.001 | ||||
| High volume (≥ 40 cases) | 16,352 (71.0) | 15,917 (75.8) | 9,322 (67.6) | |||
| Post resuscitation care, No. (%) | ||||||
| Reperfusion | 319 (1.4) | 241 (1.1) | 85 (0.6) | < 0.001 | < 0.001 | |
| Hypothermia | 533 (2.3) | 500 (2.4) | 182 (1.3) | < 0.001 | < 0.001 | |
| ECMO | 196 (0.9) | 158 (0.8) | 58 (0.4) | < 0.001 | < 0.001 | |
| Outcome, No. (%) | ||||||
| Survival to discharge | 792 (3.4) | 508 (2.4) | 183 (1.3) | < 0.001 | < 0.001 | |
| Good neurological recovery | 232 (1.0) | 124 (0.6) | 42 (0.3) | < 0.001 | < 0.001 | |
SD = standard deviation, ECG = electrocardiogram, PEA = Pulseless electrical activity, CPR = cardiopulmonary resuscitation, IQR = interquartile range, EMS = emergency medical service, ECMO = extracorporeal membrane oxygenation.
aTo calculate the p for trend, the initial ECG category was collapsed into shockable vs. non-shockable.
The characteristics of the study population are shown according to STI in Table 2. Compared to the short STI group, the subjects in the long STI group were less often found in public places, more likely to receive prehospital defibrillation and prehospital advanced airway placement and more likely to be transferred to a high-volume center. The survival to discharge and good neurological recovery rates were higher in the short STI group than in the long STI group (4.1% vs. 2.1%, respectively, for survival to discharge and 1.2% vs. 0.5%, respectively, for good neurological recovery; both P values < 0.001).
Table 2. Characteristics of study population by scene time interval.
| Characteristics | Scene time interval | P value | ||
|---|---|---|---|---|
| 1–5 min (n = 12,652) | > 5 min (n = 45,170) | |||
| Age, yr, mean (SD) | 69.9 (15.0) | 70.0 (15.2) | 0.319 | |
| Men, No. (%) | 7,784 (61.5) | 28,460 (63.0) | 0.002 | |
| Past medical history, No. (%) | ||||
| Diabetes mellitus | 2,459 (19.4) | 9,646 (21.4) | < 0.001 | |
| Hypertension | 3,852 (30.4) | 14,385 (31.8) | 0.003 | |
| Heart disease | 1,690 (13.4) | 6,251 (13.8) | 0.169 | |
| Stroke | 1,005 (7.9) | 4,184 (9.3) | < 0.001 | |
| Medical aid, No. (%) | 1,137 (9.0) | 3,900 (8.6) | 0.220 | |
| Community urbanization, No. (%) | < 0.001 | |||
| Metropolitan | 5,118 (40.5) | 19,736 (43.7) | ||
| Circumstance of arrest, No. (%) | ||||
| Public location | 3,082 (24.4) | 6,362 (14.1) | < 0.001 | |
| Witnessed | 5,318 (42.0) | 19,224 (42.6) | 0.294 | |
| Bystander CPR | 5,118 (40.5) | 22,088 (48.9) | < 0.001 | |
| Initial ECG, No. (%) | 0.023 | |||
| Asystole | 9,888 (78.2) | 34,810 (77.1) | ||
| PEA | 1,277 (10.1) | 4,685 (10.4) | ||
| Shockable rhythm | 1,487 (11.8) | 5,675 (12.6) | ||
| Prehospital management, No. (%) | ||||
| Defibrillation | 2,225 (17.6) | 8,998 (19.9) | < 0.001 | |
| Advanced airway management | 1,054 (8.3) | 7,085 (15.7) | < 0.001 | |
| Mechanical CPR | 48 (0.4) | 201 (0.4) | 0.358 | |
| Elapsed time, median (IQR), min | ||||
| EMS response time | 7.0 (5.0–10.0) | 7.0 (5.0–10.0) | 0.656 | |
| Scene time | 4.0 (3.0–5.0) | 10.0 (8.0–13.0) | < 0.001 | |
| Transport time | 7.0 (5.0–12.0) | 6.0 (4.0–10.0) | < 0.001 | |
| Volume of center, No. (%) | < 0.001 | |||
| High volume (≥ 40 cases) | 8,884 (70.2) | 32,707 (72.4) | ||
| Post resuscitation care, No. (%) | ||||
| Reperfusion | 200 (1.6) | 445 (1.0) | < 0.001 | |
| Hypothermia | 357 (2.8) | 858 (1.9) | < 0.001 | |
| ECMO | 95 (0.8) | 317 (0.7) | 0.603 | |
| Outcome, No. (%) | ||||
| Survival to discharge | 516 (4.1) | 967 (2.1) | < 0.001 | |
| Good neurologic recovery | 158 (1.2) | 240 (0.5) | < 0.001 | |
SD = standard deviation, ECG = electrocardiogram, PEA = Pulseless electrical activity, CPR = cardiopulmonary resuscitation, IQR = interquartile range, EMS = emergency medical service, ECMO = extracorporeal membrane oxygenation.
Baseline characteristics according to TTI in each STI group are shown in Table 3. TTI was associated with significant increase in response time and decrease in the proportion of urbanization level in both STI group. In short STI group, survival to discharge and good neurological recovery were higher in short TTI group (5.9% and 2.2%, respectively) than in the intermediate TTI group (4.2% and 1.0%, respectively) and the long TTI group (1.9%, and 0.4% respectively; P < 0.001 for both trends). In long STI group, survival to discharge and good neurological recovery were higher in short TTI group (2.9% and 0.7%, respectively) than in the intermediate TTI group (2.0% and 0.5%, respectively) and the long TTI group (1.1%, and 0.3% respectively; P < 0.001 for both trends).
Table 3. Characteristics of the study population by transport time interval according to scene time interval.
| Characteristics | Transport time interval | ||||||
|---|---|---|---|---|---|---|---|
| Scene time interval: 0–5 min | Scene time interval: > 5 min | ||||||
| 1–5 min (n = 4,445) | 6–10 min (n = 4,479) | > 10 min (n = 3,728) | 1–5 min (n = 18,598) | 6–10 min (n = 16,506) | > 10 min (n = 10,066) | ||
| Age, years, mean (SD) | 69.0 (15.2) | 69.7 (15.1) | 71.1 (14.7)a,b | 69.4 (15.4) | 70.1 (15.2) | 71.0 (14.6)a,b | |
| Men, No. (%) | 2,796 (62.9) | 2,704 (60.4) | 2,284 (61.3)c | 11,806 (63.5) | 10,264 (62.2) | 6,390 (63.5)c | |
| Past medical history, No. (%) | |||||||
| Diabetes mellitus | 903 (20.3) | 896 (20.0) | 660 (17.7)a | 4,030 (21.7) | 3,642 (22.1) | 1,974 (19.6)a | |
| Hypertension | 1,387 (31.2) | 1,416 (31.6) | 1,049 (28.1)a,b | 5,943 (32.0) | 5,428 (32.9) | 3,014 (29.9)a,d | |
| Heart disease | 637 (14.3) | 606 (13.5) | 447 (12.0)a,b | 2,543 (13.7) | 2,351 (14.2) | 1,357 (13.5) | |
| Stroke | 362 (8.1) | 355 (7.9) | 288 (7.7) | 1,646 (8.9) | 1,612 (9.8) | 926 (9.2)c | |
| Medical aid, No. (%) | 420 (9.4) | 409 (9.1) | 308 (8.3)a | 1,630 (8.8) | 1,437 (8.7) | 833 (8.3)a | |
| Community urbanization, No. (%) | |||||||
| Metropolitan | 2,194 (49.4) | 2,065 (46.1) | 859 (23.0)a,b | 9,173 (49.3) | 8,086 (49.0) | 2,477 (24.6)a,b | |
| Circumstance of arrest, No. (%) | |||||||
| Public location | 1,288 (29.0) | 1,051 (23.5) | 743 (19.9) | 2,839 (15.3) | 2,077 (12.6) | 1,446 (14.4)a,b | |
| Witnessed status | 1,852 (41.7) | 1,909 (42.6) | 1,557 (41.8) | 7,737 (41.6) | 7,118 (43.1) | 4,369 (43.4) | |
| Bystander CPR | 1,779 (40.0) | 1,853 (41.4) | 1,486 (39.9) | 9,011 (48.5) | 8,127 (49.2) | 4,950 (49.2) | |
| Initial ECG, No. (%) | |||||||
| Asystole | 3,374 (75.9) | 3,440 (76.8) | 3,074 (82.5) | 14,184 (76.3) | 12,658 (76.7) | 7,968 (79.2) | |
| PEA | 512 (11.5) | 487 (10.9) | 278 (7.5) | 1,990 (10.7) | 1,850 (11.2) | 845 (8.4) | |
| Shockable rhythm | 559 (12.6) | 552 (12.3) | 376 (10.1)a,b | 2,424 (13.0) | 1,998 (12.1) | 1,253 (12.4)a | |
| Prehospital management, No. (%) | |||||||
| Defibrillation | 692 (15.6) | 838 (18.7) | 695 (18.6)a,b | 3,526 (19.0) | 3,230 (19.6) | 2,242 (22.3)a,b | |
| Advanced airway management | 308 (6.9) | 400 (8.9) | 346 (9.3)a,b | 2,964 (15.9) | 2,745 (16.6) | 1,376 (13.7)a,b | |
| Mechanical CPR | 15 (0.3) | 17 (0.4) | 16 (0.4) | 68 (0.4) | 76 (0.5) | 57 (0.6)c,d | |
| Elapsed time, median (IQR), min | |||||||
| EMS response time | 6.0 (5.0–8.0) | 7.0 (5.0–10.0) | 9.0 (6.0–14.0)a,b | 6.0 (5.0–8.0) | 7.0 (6.0–10.0) | 9.0 (6.0–14.0)b,d | |
| Scene time | 4.0 (3.0–5.0) | 4.0 (3.0–5.0) | 4.0 (3.0–5.0)a,b | 10.0 (8.0–13.0) | 10.0 (8.0–13.0) | 10.0 (7.0–13.0)b,d | |
| Transport time | 4.0 (3.0–5.0) | 8.0 (7.0–9.0) | 15.0 (13.0–19.0)a,b | 4.0 (3.0–5.0) | 7.0 (6.0–9.0) | 15.0 (12.0–19.0)b,d | |
| Volume of center, No. (%) | |||||||
| High volume (≥ 40 cases) | 3,109 (69.9) | 3,351 (74.8) | 2,424 (65.0)a,b | 13,243 (71.2) | 12,566 (76.1) | 6,898 (68.5)a,d | |
| Post resuscitation care, No. (%) | |||||||
| Reperfusion | 95 (2.1) | 76 (1.7) | 29 (0.8)a,b | 224 (1.2) | 165 (1.0) | 56 (0.6)a,b | |
| Hypothermia | 143 (3.2) | 156 (3.5) | 58 (1.6)a,b | 390 (2.1) | 344 (2.1) | 124 (1.2)a,b | |
| ECMO | 43 (1.0) | 37 (0.8) | 15 (0.4)b,c | 153 (0.8) | 121 (0.7) | 43 (0.4)a,b | |
| Outcome, No. (%) | |||||||
| Survival to discharge | 261 (5.9) | 186 (4.2) | 69 (1.9)a,b | 531 (2.9) | 322 (2.0) | 114 (1.1)a,b | |
| Good neurologic recovery | 98 (2.2) | 46 (1.0) | 14 (0.4)a,b | 134 (0.7) | 78 (0.5) | 28 (0.3)a,b | |
SD = standard deviation, ECG = electrocardiogram, PEA = Pulseless electrical activity, CPR = cardiopulmonary resuscitation, IQR = interquartile range, EMS = emergency medical service, ECMO = extracorporeal membrane oxygenation. aP < 0.01; bP for trend < 0.01; cP < 0.05; dP for trend < 0.05.
Main results
Overall, intermediate and long TTIs were significantly less likely to have a good neurological recovery (aOR for a good neurological recovery [95% CI], 0.58 (0.47–0.73) for intermediate TTI and 0.30 [0.21–0.41] for long TTI) and had lower survival rates (aOR for survival to discharge [95% CI], 0.57 [0.45–0.73] for intermediate TTI and 0.48 [0.34–0.68] for long TTI) than was observed in the short TTI group.
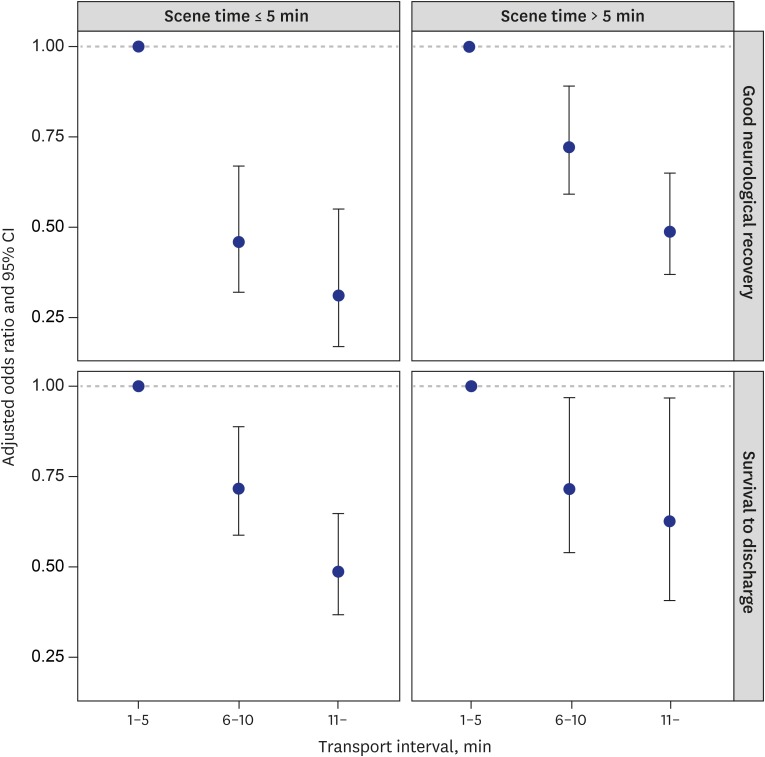
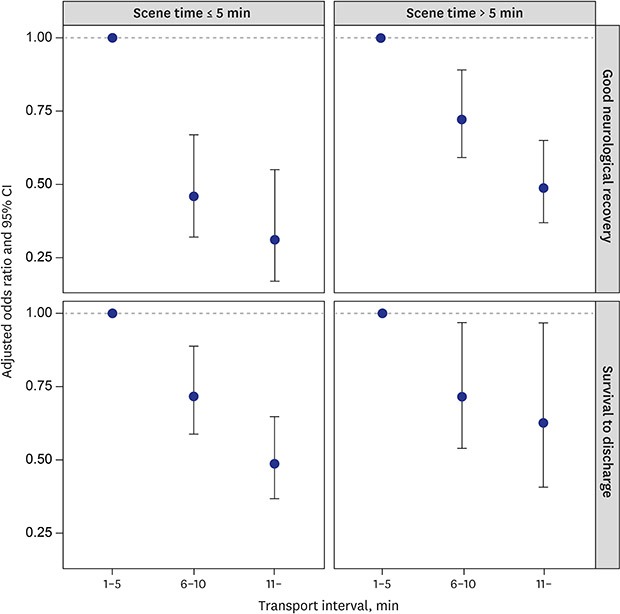
The aORs of TTI for good neurological recovery according to the STI group are shown in Table 4. In short STI group, intermediate and long TTIS were significantly less likely to have a good neurological recovery (AOR for good neurological recovery [95% CI], 0.46 [0.32–0.67] for intermediate TTI and 0.31 [0.17–0.55] for long TTI) and had lower survival rates (AOR for survival to discharge [95% CI], 0.72 [0.59–0.89] for intermediate TTI and 0.49 [0.37–0.65] for long TTI) than was observed in the short TTI group. In long STI group, intermediate and long TTIS were significantly less likely to have a good neurological recovery (AOR for good neurological recovery [95% CI], 0.72 [0.59–0.89] for intermediate TTI and 0.49 [0.37–0.65] for long TTI) and had lower survival rates (AOR for survival to discharge [95% CI], 0.72 [0.54–0.97] for intermediate TTI and 0.63 [0.41–0.97] for long TTI) than was observed in the short TTI group (Table 4 and Fig. 2).
Table 4. Effects of transport time interval on clinical outcomes according to the scene time interval.
| Variables | Scene time interval: 0–5 min | Scene time interval: > 5 min | |||
|---|---|---|---|---|---|
| No. of outcome/No. (%) | AORa (95% CI) | No. of outcome/No. (%) | AORa (95% CI) | ||
| Good neurological recovery, min | |||||
| 1–5 | 98/4,445 (2.2) | Reference | 134/18,598 (0.7) | Reference | |
| 6–10 | 46/4,479 (1.0) | 0.46 (0.32–0.67) | 78/16,506 (0.5) | 0.72 (0.59–0.89) | |
| ≥ 11 | 14/3,728 (0.4) | 0.31 (0.17–0.55) | 28/10,066 (0.3) | 0.49 (0.37–0.65) | |
| Survival to discharge | |||||
| 1–5 | 261/4,445 (5.9) | Reference | 531/18,598 (2.9) | Reference | |
| 6–10 | 186/4,479 (4.2) | 0.72 (0.59–0.89) | 322/16,506 (2.0) | 0.72 (0.54–0.97) | |
| ≥ 11 | 69/3,728 (1.9) | 0.49 (0.37–0.65) | 114/10,066 (1.1) | 0.63 (0.41–0.97) | |
AOR = Adjusted odds ratio, CI = confidence interval, CPR = cardiopulmonary resuscitation. aAdjusted for age, gender, medical insurance status, location of arrest, witness status, bystander CPR, response time interval, initial electrocardiogram rhythm, prehospital defibrillation, prehospital advanced airway, prehospital mechanical CPR, urbanization level, and volume of center.
Fig. 2. Clinical outcomes of patients according to transport time and scene time. (A) The good neurological recovery rate and (B) survival to discharge rate.
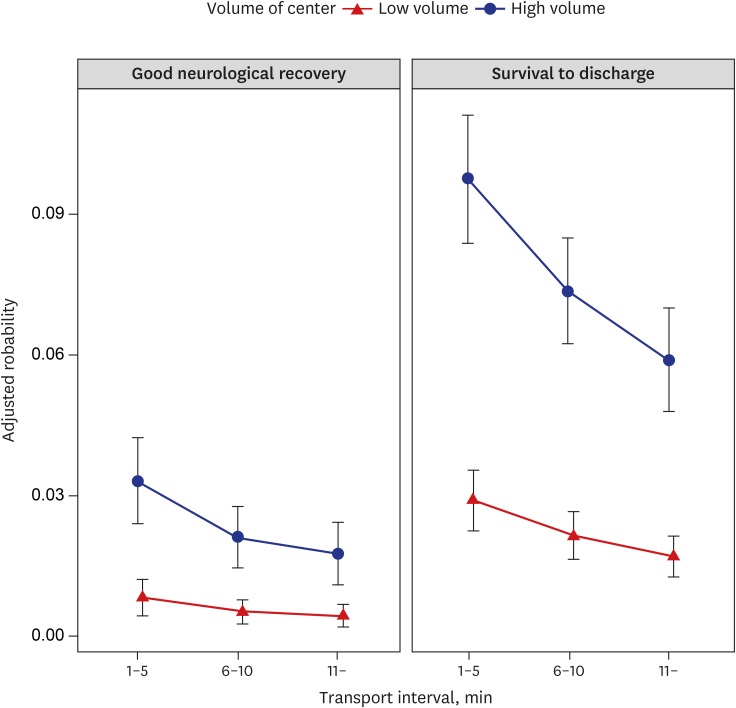
Fig. 3 showed the adjusted probability for the good neurological recovery and survival to discharge by TTI according to the volume of center. Adjusted probabilities for outcomes of high volume center visitors were higher than those of low volume center visitors. Adjusted probability for good neurological recovery and survival to discharge in the long TTI group who visited high volume center was higher than that in the short TTI group who visited low volume center (0.018 [95% CI, 0.011–0.024] vs. 0.008 [95% CI, 0.004–0.012], respectively, for good neurological recovery and 0.059 [95% CI, 0.048–0.070] vs. 0.017 [95% CI, 0.013–0.021], respectively).
Fig. 3. Adjusted probability and 95% confidence intervals for good neurological recovery and survival to discharge according to transport time and volume of center. Adjusted factors include age, gender, medical insurance status, location of arrest, witness status, bystander CPR, response time interval, initial electrocardiogram rhythm, prehospital defibrillation, prehospital advanced airway, prehospital mechanical CPR and urbanization level.
CPR = cardiopulmonary resuscitation.
DISCUSSION
By analyzing the national OHCA registry, this study found that TTI had a negative effect on neurologic outcome in OHCA patients without prehospital ROSC both short STI group and long STI group. The harmful effects of a longer TTI on neurologic outcome were more prominent for the short STI group than the long STI group (Table 4). These results emphasize that when EMS providers choose the hospital to which OHCA patients without prehospital ROSC will be transported, STI and TTI should be considered because the negative effect of a longer TTI might be intensified when an STI is short.
Although we demonstrated the negative effect of TTI on neurologic outcomes of OHCA patients without ROSC, our finding does not mean that the bypass of OHCA patients without ROSC is always harmful. For patients who received sufficient resuscitation efforts at the scene, the negative effect of a longer TTI might be attenuated. We found that a long STI group received significantly more prehospital defibrillation and prehospital advanced airway management than a short STI group (Table 2). Rhythm analysis and defibrillation in the early period of CPR may be inappropriate in the short STI group because rhythm analysis in a moving ambulance can be inaccurate due to multiple reasons.27 An advanced airway management prior to transfer may contribute to reduce hypoxic events during transport. In addition, the interruption of chest compression in the early period of CPR may be worse for clinical outcomes than that in the late period of CPR.28 Therefore, if EMS providers provide sufficient resuscitation to a patient in the field and transport the patient to the high volume center, the risk of extended transport time by bypassing the nearest low volume center could be attenuated.
Comprehensive post-arrest care is an independent predictor of good neurological recovery in OHCA patients.29,30,31,32,33,34 We also found that adjusted probability for outcomes of high volume center visitor with long TTI was higher than that of low volume center visitor with short TTI (Fig. 3). Because the negative effect of longer TTI might be offset by better post-arrest care, it is important for EMS providers to have access to information about hospitals that can treat OHCA. Designating cardiac receiving centers and reporting their outcomes could be very helpful for EMS providers choosing a hospital to which OHCA patients will be transported.33 The risk of transporting OHCA patients and the quality of hospital care should be considered when developing transportation protocols for OHCA patients. In addition, the different risks associated with transporting subgroups of OHCA patients should be considered. An outcome-based investigation is needed to identify the factors that confer a transfer risk in OHCA patients and develop effective transportation protocols to prevent or avoid such risks.
We categorized transport time into three groups. The 5-minute and 10-minute cutoffs were approximately defined by the distribution of a transport time in our study population (1st quantile of TTI, 4 minutes; 3rd quantile of TTI, 10 minutes). We categorized scene time into two groups because Korean national prehospital care protocols for OHCA patients recommends a minimum of 5 minutes of on-scene resuscitation before transport to the hospital.35 Therefore, our findings would be different in other communities with different transport time distributions and scene time protocols.
Several studies, including one meta-analysis, have reported that a longer TTI is not associated with decreased survival.6,8,9,10,11 Most of those studies analysed the effect of TTI on survival in all OHCA patients, including patients with prehospital ROSC. However, poor-quality CPR during transport could critically affect patients without ROSC. Therefore, the negative effect of TTI on the outcomes of OHCA patients might be diluted when all OHCA patients are included in analyses. In addition, the degradation of CPR quality during transport may be further strengthened in our setting than in most Western countries. Because the highest service level of emergency medical technician (EMT) is limited to the level of intermediate EMT in the US, CPR performance may be inadequate compared to Western countries with high service level.36 In addition, feedback CPR devices that can be used to maintain the quality of CPR during transport are not widely used in Korea.37 Therefore, quality control of compression during transport is also limited in Korea. These aspects can contribute to further degrading the quality of CPR during transport in our setting. Moreover, most of the studies investigating TTI were conducted in Western countries, where sufficient resuscitation efforts can be attempted in prehospital areas. Spaite et al. reported that median STI for OHCA patients were 18 minutes.9 However, we found that median STI was 10 minutes even in long STI group (Table 2). Because the negative effect of TTI was attenuated in the long STI group, it might be difficult to assess the negative association between TTI and clinical outcomes of OHCA patients in a community where scene time is long enough in most patients. In addition, compared with the effect of a longer TTI on good neurologic recovery, its effect on a poor outcome was attenuated by survival to discharge in our study (Table 4). This finding indicates that the effect of poor-quality CPR during transport might be more prominent for neurologic outcome than for survival. The different effects of CPR quality on survival and neurologic outcome after arrest have also been reported in a few studies.15,16 The relatively small sample sizes of previous studies also contributed to the negative results.
Because high-quality CPR during transport is difficult to achieve,12,13,14 various efforts to achieve high-quality CPR during transport are needed because the transport of patients without ROSC is inevitable, even when advanced life support is available and the termination of prehospital resuscitation are allowed.9,33,38 Although mechanical CPR is not associated with better outcomes in the prehospital setting,39,40 mechanical CPR during transport might be an alternative for maintaining quality CPR during transport.17 CPR feedback devices could also maintain the quality of CPR during transport.37 Further investigations that develop various methods to maintain CPR quality during transport and evaluate the effects of those methods are needed.
This study has several limitations. First, although we assumed that the quality of CPR was poor during transport, it was not directly measured. However, several studies have indicated that the quality of CPR during transport is poor.12,13,14 Second, we excluded patients whose TTI was over 30 minutes because we could not find a reason for such long transport times in our database. However, those cases accounted for only 1.7% of the study population. Third, this study was conducted in Korea. Therefore, the generalizability of the results to other countries is not clear. Fourth, this study was not a randomized controlled trial to explore the effects of TTI on OHCA outcomes. Although we adjusted for potential risk confounders using Utstein elements, our ability to adjust for these risks may have been limited.
In conclusion, we found that a longer TTI adversely affected neurologic recovery in OHCA patients without prehospital ROSC and that this negative effect was intensified in patients who received insufficient resuscitation at the scene. This finding emphasizes that EMS providers should carefully consider TTI and STI when choosing the hospital to which OHCA patients without prehospital ROSC will be transported. Weighing the risk of transporting OHCA patients without prehospital ROSC and the potential benefits of better post-cardiac arrest care at a distant hospital is important when considering the creation of a regionalized system for OHCA patients.
Footnotes
Funding: This study was financially supported by the Korea Centers for Disease Control and Prevention (CDC) (2012-2015, fund code 2012-E33010-00, 2013-E33010-00, 2014-E33010-00, 2014-E33010-00, and 2015-E33010-00).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim YJ, Shin SD.
- Data curation: Park JH, Ro YS, Shin SD.
- Formal analysis: Park JH, Ro YS, Kim S.
- Investigation: Park JH, Kim YJ, Cha WC.
- Methodology: Park JH, Ro YS, Kim S, Cha WC.
- Software: Park JH, RO YS.
- Validation: Park JH, Ro YS, Kim YJ.
- Writing - original draft: Park JH, Kim YJ.
- Writing - review & editing: Cha WC, Shin SD.
References
- 1.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Yang HJ, Kim GW, Kim H, Cho JS, Rho TH, Yoon HD, et al. Epidemiology and outcomes in out-of-hospital cardiac arrest: a report from the NEDIS-based cardiac arrest registry in Korea. J Korean Med Sci. 2015;30(1):95–103. doi: 10.3346/jkms.2015.30.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120(13):1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lyon RM, Clarke S, Gowens P, Egan G, Clegg GR. Resuscitation quality assurance for out-of-hospital cardiac arrest--setting-up an ambulance defibrillator telemetry network. Resuscitation. 2010;81(12):1726–1728. doi: 10.1016/j.resuscitation.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Kronick SL, Kurz MC, Lin S, Edelson DP, Berg RA, Billi JE, et al. Part 4: systems of care and continuous quality improvement: 2015 American Heart Association Guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18) Suppl 2:S397–S413. doi: 10.1161/CIR.0000000000000258. [DOI] [PubMed] [Google Scholar]
- 6.Davis DP, Fisher R, Aguilar S, Metz M, Ochs G, McCallum-Brown L, et al. The feasibility of a regional cardiac arrest receiving system. Resuscitation. 2007;74(1):44–51. doi: 10.1016/j.resuscitation.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Herlitz J, Ekström L, Axelsson A, Bång A, Wennerblom B, Waagstein L, et al. Continuation of CPR on admission to emergency department after out-of-hospital cardiac arrest. Occurrence, characteristics and outcome. Resuscitation. 1997;33(3):223–231. doi: 10.1016/s0300-9572(96)01014-3. [DOI] [PubMed] [Google Scholar]
- 8.Cha WC, Lee SC, Shin SD, Song KJ, Sung AJ, Hwang SS. Regionalisation of out-of-hospital cardiac arrest care for patients without prehospital return of spontaneous circulation. Resuscitation. 2012;83(11):1338–1342. doi: 10.1016/j.resuscitation.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Spaite DW, Bobrow BJ, Vadeboncoeur TF, Chikani V, Clark L, Mullins T, et al. The impact of prehospital transport interval on survival in out-of-hospital cardiac arrest: implications for regionalization of post-resuscitation care. Resuscitation. 2008;79(1):61–66. doi: 10.1016/j.resuscitation.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 10.Spaite DW, Stiell IG, Bobrow BJ, de Boer M, Maloney J, Denninghoff K, et al. Effect of transport interval on out-of-hospital cardiac arrest survival in the OPALS study: implications for triaging patients to specialized cardiac arrest centers. Ann Emerg Med. 2009;54(2):248–255. doi: 10.1016/j.annemergmed.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 11.Geri G, Gilgan J, Wu W, Vijendira S, Ziegler C, Drennan IR, et al. Does transport time of out-of-hospital cardiac arrest patients matter? A systematic review and meta-analysis. Resuscitation. 2017;115:96–101. doi: 10.1016/j.resuscitation.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Havel C, Schreiber W, Riedmuller E, Haugk M, Richling N, Trimmel H, et al. Quality of closed chest compression in ambulance vehicles, flying helicopters and at the scene. Resuscitation. 2007;73(2):264–270. doi: 10.1016/j.resuscitation.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Kurz MC, Dante SA, Puckett BJ. Estimating the impact of off-balancing forces upon cardiopulmonary resuscitation during ambulance transport. Resuscitation. 2012;83(9):1085–1089. doi: 10.1016/j.resuscitation.2012.01.033. [DOI] [PubMed] [Google Scholar]
- 14.Skogvoll E, Eftestøl T, Gundersen K, Kvaløy JT, Kramer-Johansen J, Olasveengen TM, et al. Dynamics and state transitions during resuscitation in out-of-hospital cardiac arrest. Resuscitation. 2008;78(1):30–37. doi: 10.1016/j.resuscitation.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 15.Sanders AB, Kern KB, Berg RA, Hilwig RW, Heidenrich J, Ewy GA. Survival and neurologic outcome after cardiopulmonary resuscitation with four different chest compression-ventilation ratios. Ann Emerg Med. 2002;40(6):553–562. doi: 10.1067/mem.2002.129507. [DOI] [PubMed] [Google Scholar]
- 16.Yang CL, Wen J, Li YP, Shi YK. Cardiocerebral resuscitation vs cardiopulmonary resuscitation for cardiac arrest: a systematic review. Am J Emerg Med. 2012;30(5):784–793. doi: 10.1016/j.ajem.2011.02.035. [DOI] [PubMed] [Google Scholar]
- 17.Shin SD, Kitamura T, Hwang SS, Kajino K, Song KJ, Ro YS, et al. Association between resuscitation time interval at the scene and neurological outcome after out-of-hospital cardiac arrest in two Asian cities. Resuscitation. 2014;85(2):203–210. doi: 10.1016/j.resuscitation.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 18.Kim TH, Shin SD, Kim YJ, Kim CH, Kim JE. The scene time interval and basic life support termination of resuscitation rule in adult out-of-hospital cardiac arrest. J Korean Med Sci. 2015;30(1):104–109. doi: 10.3346/jkms.2015.30.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee YJ, Hwang SS, Shin SD, Lee SC, Song KJ. Effect of national implementation of telephone CPR program to improve outcomes from out-of-hospital cardiac arrest: an interrupted time-series analysis. J Korean Med Sci. 2018;33(51):e328. doi: 10.3346/jkms.2018.33.e328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ro YS, Shin SD, Lee YJ, Lee SC, Song KJ, Ryoo HW, et al. Effect of dispatcher-assisted cardiopulmonary resuscitation program and location of out-of-hospital cardiac arrest on survival and neurologic outcome. Ann Emerg Med. 2017;69(1):52–61.e1. doi: 10.1016/j.annemergmed.2016.07.028. [DOI] [PubMed] [Google Scholar]
- 21.Ro YS, Shin SD, Song KJ, Lee EJ, Kim JY, Ahn KO, et al. A trend in epidemiology and outcomes of out-of-hospital cardiac arrest by urbanization level: a nationwide observational study from 2006 to 2010 in South Korea. Resuscitation. 2013;84(5):547–557. doi: 10.1016/j.resuscitation.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 22.Edgren E, Hedstrand U, Kelsey S, Sutton-Tyrrell K, Safar P BRCT I Study Group. Assessment of neurological prognosis in comatose survivors of cardiac arrest. Lancet. 1994;343(8905):1055–1059. doi: 10.1016/s0140-6736(94)90179-1. [DOI] [PubMed] [Google Scholar]
- 23.Callaway CW, Schmicker R, Kampmeyer M, Powell J, Rea TD, Daya MR, et al. Receiving hospital characteristics associated with survival after out-of-hospital cardiac arrest. Resuscitation. 2010;81(5):524–529. doi: 10.1016/j.resuscitation.2009.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hasegawa K, Hiraide A, Chang Y, Brown DF. Association of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA. 2013;309(3):257–266. doi: 10.1001/jama.2012.187612. [DOI] [PubMed] [Google Scholar]
- 25.Shin SD, Ahn KO, Song KJ, Park CB, Lee EJ. Out-of-hospital airway management and cardiac arrest outcomes: a propensity score matched analysis. Resuscitation. 2012;83(3):313–319. doi: 10.1016/j.resuscitation.2011.10.028. [DOI] [PubMed] [Google Scholar]
- 26.Ro YS, Shin SD, Song KJ, Park CB, Lee EJ, Ahn KO, et al. A comparison of outcomes of out-of-hospital cardiac arrest with non-cardiac etiology between emergency departments with low- and high-resuscitation case volume. Resuscitation. 2012;83(7):855–861. doi: 10.1016/j.resuscitation.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Calle PA, De Paepe P, Van Sassenbroeck D, Monsieurs KG. External artifacts by advanced life support providers misleading automated external defibrillators. Resuscitation. 2008;79(3):482–489. doi: 10.1016/j.resuscitation.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 28.Bobrow BJ, Clark LL, Ewy GA, Chikani V, Sanders AB, Berg RA, et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299(10):1158–1165. doi: 10.1001/jama.299.10.1158. [DOI] [PubMed] [Google Scholar]
- 29.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346(8):557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 30.Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 31.Langhelle A, Tyvold SS, Lexow K, Hapnes SA, Sunde K, Steen PA. In-hospital factors associated with improved outcome after out-of-hospital cardiac arrest. A comparison between four regions in Norway. Resuscitation. 2003;56(3):247–263. doi: 10.1016/s0300-9572(02)00409-4. [DOI] [PubMed] [Google Scholar]
- 32.Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013;369(23):2197–2206. doi: 10.1056/NEJMoa1310519. [DOI] [PubMed] [Google Scholar]
- 33.Spaite DW, Bobrow BJ, Stolz U, Berg RA, Sanders AB, Kern KB, et al. Statewide regionalization of postarrest care for out-of-hospital cardiac arrest: association with survival and neurologic outcome. Ann Emerg Med. 2014;64(5):496–506.e1. doi: 10.1016/j.annemergmed.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 34.Sunde K, Pytte M, Jacobsen D, Mangschau A, Jensen LP, Smedsrud C, et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73(1):29–39. doi: 10.1016/j.resuscitation.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 35.Kim TH, Lee EJ, Shin SD, Ro YS, Kim YJ, Ahn KO, et al. Neurological favorable outcomes associated with EMS compliance and on-scene resuscitation time protocol. Prehosp Emerg Care. 2018;22(2):214–221. doi: 10.1080/10903127.2017.1367443. [DOI] [PubMed] [Google Scholar]
- 36.Shin SD, Ong ME, Tanaka H, Ma MH, Nishiuchi T, Alsakaf O, et al. Comparison of emergency medical services systems across Pan-Asian countries: a Web-based survey. Prehosp Emerg Care. 2012;16(4):477–496. doi: 10.3109/10903127.2012.695433. [DOI] [PubMed] [Google Scholar]
- 37.Cheskes S, Byers A, Zhan C, Verbeek PR, Ko D, Drennan IR, et al. CPR quality during out-of-hospital cardiac arrest transport. Resuscitation. 2017;114:34–39. doi: 10.1016/j.resuscitation.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 38.Xiong Y, Zhan H, Lu Y, Guan K, Okoro N, Mitchell D, et al. Out-of-hospital cardiac arrest without return of spontaneous circulation in the field: who are the survivors? Resuscitation. 2017;112:28–33. doi: 10.1016/j.resuscitation.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 39.Bonnes JL, Brouwer MA, Navarese EP, Verhaert DV, Verheugt FW, Smeets JL, et al. Manual cardiopulmonary resuscitation versus CPR including a mechanical chest compression device in out-of-hospital cardiac arrest: a comprehensive meta-analysis from randomized and observational studies. Ann Emerg Med. 2016;67(3):349–360.e3. doi: 10.1016/j.annemergmed.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 40.Rubertsson S, Lindgren E, Smekal D, Östlund O, Silfverstolpe J, Lichtveld RA, et al. Mechanical chest compressions and simultaneous defibrillation vs conventional cardiopulmonary resuscitation in out-of-hospital cardiac arrest: the LINC randomized trial. JAMA. 2014;311(1):53–61. doi: 10.1001/jama.2013.282538. [DOI] [PubMed] [Google Scholar]