Abstract
Background/Aims
Few studies have addressed whether there are differences in clinical efficacy between intravenous methylprednisolone (methyl-Pd) and intravenous immunoglobulin (IVIg) use.
Methods
We retrospectively compared platelet responses and toxicities associated with these two treatments in adult patients with immune thrombocytopenia. Patients received intravenous methyl-Pd therapy followed by oral prednisolone (Pd) from 1993 to 2002 and IVIg together with oral Pd from 2003 to 2008.
Results
Early response and maintenance of the response were assessed at 7 days and 6 months after treatment, respectively. Of the 87 patients enrolled, 77 (88.5%) were eligible for analysis. Early responses occurred in 30 of 39 patients (76.9%) receiving methyl-Pd versus 33 of 38 patients (86.6%) receiving IVIg (p = 0.187). The response was maintained in 28 patients (71.8%) in the methyl-Pd arm and in 23 patients (60.5%) in the IVIg arm (p = 0.187). The time to a complete response in the IVIg arm (6 days; range, 1 to 35) was shorter than that in the methyl-Pd arm (13.5 days; range, 2 to 29) (p = 0.002). Side effects were mild and tolerable in both arms. Five years after initiating treatment, 7 of 18 patients (38.9%) and five of 14 patients (35.7%) were still maintaining a response in the methyl-Pd and IVIg arms, respectively.
Conclusions
These results indicate that neither the early response rate nor the long-term outcome differed between the methyl-Pd and IVIg treatments. However, IVIg induced a complete response more rapidly than did methyl-Pd.
Keywords: Immune thrombocytopenia, Methylprednisolone, Intravenous immunoglobulins
INTRODUCTION
Primary immune thrombocytopenia (ITP) is an acquired immune-mediated disorder characterized by isolated thrombocytopenia, defined as a peripheral blood platelet count of less than 100 × 109/L, and depending upon the degree of thrombocytopenia, an increased risk of bleeding [1]. Standard initial treatments for newly diagnosed patients requiring emergency therapy (such as a platelet count of less than 20 × 109/L, or platelet counts of 20 to 50 × 109/L with bleeding tendency) include the use of corticosteroids and intravenous immunoglobulin (IVIg) [2]. Corticosteroids have as high as 50% to 80% response rates, and a small percentage of patients exhibit a sustained response. IVIg also produces initial response rates comparable to those of corticosteroids, albeit transiently [3]. About a decade ago, Godeau et al. [4] compared IVIg with high-dose methylprednisolone (methyl-Pd) in untreated adults with primary ITP and assessed the efficacy of subsequent oral steroids compared with a placebo. In their study, the treatment strategy for oral steroid maintenance to increase the sustained response rate was feasible. However, the response criteria in their study differed from those used now. Few studies have compared methyl-Pd with steroid maintenance therapy versus IVIg with steroid maintenance therapy according to response criteria set by the 2009 International Working Group on ITP [1]. Thus, this study investigated response rates, toxicities and long-term follow-up data between these two treatment strategies by the new criteria.
METHODS
Patient characteristics
This was a single-center retrospective study with analysis by review of medical records. Patients diagnosed with ITP requiring treatment and then followed for at least 6 months at Chungnam National University Hospital (Daejeon, Korea) between January 1993 and December 2008 were enrolled in this study. ITP was diagnosed according to the practice guidelines of the American Society of Hematology and recommendations of the 2010 International Consensus Report on ITP [2,3]. All patients had either a platelet count of less than 20 × 109/L, or clinically significant mucosal bleeding and a platelet count of less than 50 × 109/L. Patients with comorbidities including uncontrolled hypertension, diabetes mellitus, liver and kidney function impairment (e.g., alanine transaminase, aspartate transaminase > 2-fold the upper normal limit, and creatinine > 1.8 mg/dL, respectively), hepatitic C virus, human immunodeficiency virus, surface antigen of the hepatitis B virus seropositive status or active infection, and those who were pregnant or had treatment with corticosteroids during the previous 6 months were excluded.
Treatment protocol
Adult patients newly diagnosed with ITP between 1993 and 2002 received initial therapy of intravenous methyl-Pd therapy (10 mg/kg/day for 3 days) followed by oral prednisone (Pd; 1 mg/kg/day). Patients between 2003 and 2008 received IVIg (400 mg/kg/day for 5 days or 1,000 mg/kg/day for 2 days) together with oral Pd (1 mg/kg/day). Oral Pd was maintained at a dose of 1 mg/kg for 4 to 6 weeks, before tapering according to platelet count.
Response evaluation
The criteria for response were defined according to the standardization of the 2009 International Working Group on ITP [1]. Complete response (CR) was defined as a platelet count ≥ 100 × 109/L and an absence of bleeding. Response (R) was defined as a platelet count ≥ 30 × 109/L and at least a two-fold increase in the baseline platelet count and an absence of bleeding. No response was defined as a platelet count ≤ 30 × 109/L or a less than 2-fold increase in the baseline platelet count or bleeding. Initial response was defined as response by day 7 after initiation of treatment. A sustained response was defined as a platelet count that remained above 50 × 109/L after 6 months of follow-up. Loss of CR or R was defined as a platelet count < 100 × 109/L or bleeding (from CR), and < 30 × 109/L or a less than two-fold increase of the baseline platelet count or bleeding (from R).
Statistical analysis
The primary end point of this study was the initial response rate while secondary end points were sustained response rate, time to response, durability of response, and side effects of each treatment. Continuous variables were compared using Student t test for independent samples, and the chi-square test was used to assess differences in the distribution of categorical data. A p < 0.05 indicated a statistical significance and all reported p values were two-tailed. All other values were reported as means ± standard deviation unless otherwise indicated.
Ethics statement
The study protocol was approved by the Institutional Review Board of Chungnam National University Hospital (IRB No. 2014-06-014). Informed consent was waived due to the retrospective nature of the analysis.
RESULTS
Patient characteristics
Between January 1993 and December 2002, 59 patients were diagnosed with ITP and treated with intravenous methyl-Pd followed by oral Pd at Chungnam National University Hospital. Thirteen patients met the criteria for exclusion and another seven patients without 6-month follow-up data were also excluded, leaving 39 patients enrolled and eligible for analysis. Between January 2003 and December 2008, 52 patients were diagnosed with ITP and treated with IVIg together with oral Pd. Ten patients met the exclusion criteria; therefore, 38 patients with 6-month follow-up data remained eligible for analysis (Fig. 1).
Figure 1.
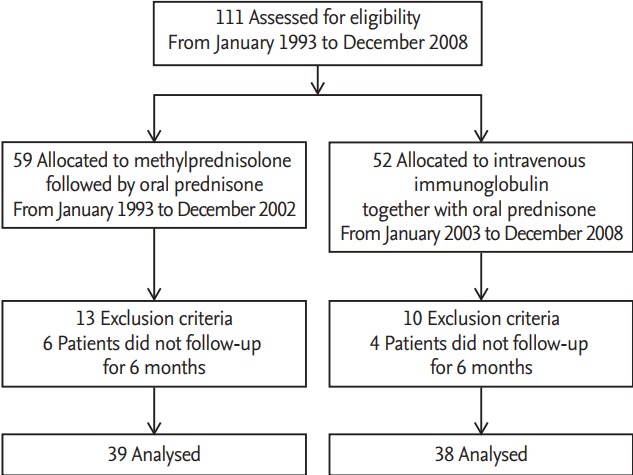
Disposition of patients in each arm.
The median age of patients in the methyl-Pd and IVIg treatment groups was 41 years (range, 16 to 83) and 44.5 years (range, 17 to 81), respectively. In the methyl-Pd treatment group seven patients (17.9%) were male, and 32 patients (82.1%) were female. In the IVIg treatment group 15 patients (39.5%) were male, and 23 (60.5%) were female. The median duration of follow-up was 121 months (range, 12 to 254) in the methyl-Pd group and 63 months (range, 6 to 109) in the IVIg group. Pre-treatment platelet counts were 4.846 ± 4.788 × 109/L in the methyl-Pd group and 4.268 ± 3.773 × 109/L in the IVIg group (Table 1).
Table 1.
Baseline characteristics of patients
| Characteristic | Methyl-Pd arm (n = 39) | IVIg arm (n = 38) | p value |
|---|---|---|---|
| Age, yr | 41.0 (16–83) | 44.5 (17–81) | 0.229 |
| Sex | 0.037 | ||
| Male | 7 (17.9) | 15 (39.5) | |
| Female | 32 (81.2) | 23 (60.5) | |
| Follow-up duration, mon | 121 (12–254) | 63 (6–109) | 0.002 |
| Pretreatment platelet count, /µL | 4,846 ± 4,788 | 4,368 ± 3,773 | 0.629 |
Values are presented as median (range), number (%), or mean ± SD.
Methyl-Pd, methylprednisolone; IVIg, intravenous immune globulin.
Response to therapy
The mean platelet count at day 7 was 98.592 ± 89.478 × 109/L in the methyl-Pd group and 92.925 ± 78.577 × 109/L in IVIg group, revealing no statistically significant difference between treatments (p = 0.806). The mean platelet count at 6 months was 145.711 ± 96.473 × 109/L in the methyl-Pd group and 153.111 ± 70.910 × 109/L in the IVIg group (p = 0.754) (Table 2).
Table 2.
Changes in platelet count (× 109/L)
| Variable | Methyl-Pd (n = 39) | IVIg (n = 38) | p value |
|---|---|---|---|
| 2 Days | 31.638 ± 35.119 | 31.236 ± 31.750 | 0.959 |
| 4 Days | 49.894 ± 50.410 | 70.078 ± 58.166 | 0.110 |
| 7 Days | 98.592 ± 89.478 | 92.925 ± 78.577 | 0.806 |
| 14 Days | 142.969 ± 113.370 | 118.827 ± 85.657 | 0.353 |
| 28 Days | 152.540 ± 98.999 | 147.026 ± 77.258 | 0.788 |
| 3 Months | 183.527 ± 87.100 | 147.026 ± 77.258 | 0.109 |
| 6 Months | 145.771 ± 96.473 | 153.111 ± 70.910 | 0.754 |
Values are presented as mean ± SD.
Methyl-Pd, methylprednisolone; IVIg, intravenous immune globulin.
The initial response rate at day 7 was 76.9% in the methyl-Pd group and 86.8% in the IVIg group, revealing no significant difference (p = 0.259). The complete response rate at day 7 was 30.8% in the methyl-Pd group and 50.0% in the IVIg group (p = 0.085). The 6-month maintenance response rate was 71.8% in the methyl-Pd group and 60.5% in the IVIg group (p = 0.296) and the complete response rate at 6 months was 56.4% in the methyl-Pd group and 52.6% in the IVIg group (p = 0.739) (Table 3). No significant differences in the number of patients and dose of platelet transfusion were observed between the two groups (Supplementary Table 1).
Table 3.
Response rate to each therapy
| Variable | Methyl-Pd (n = 39) | IVIg (n = 38) | p value |
|---|---|---|---|
| Initial response | |||
| Complete response | 12 (30.8) | 19 (50.0) | 0.085 |
| Response | 30 (76.9) | 33 (86.8) | 0.259 |
| Response maintenance | |||
| Complete response | 22 (56.4) | 20 (52.6) | 0.739 |
| Response | 28 (71.8) | 23 (60.5) | 0.296 |
Values are presented as number (%).
Methyl-Pd, methylprednisolone; IVIg, intravenous immune globulin.
The median time to response was 4 days (range, 1 to 5) in the methyl-Pd group and 3 days (range, 1 to 21) in the IVIg group, with no statistically significant difference between treatment groups (p = 0.146). The median time to complete response was 13.5 days (range, 2 to 26) in the methyl-Pd group and 6.0 days (range, 1 to 35) in the IVIg group, revealing a significantly more rapid complete response after IVIg treatment (p = 0.002). The median time to peak response was 53 days (range, 7 to 182) for the methyl-Pd treatment group and 22 days (range, 3 to 138) for the IVIg treatment group (p = 0.353) (Table 4).
Table 4.
Time to response
| Variable | Methyl–Pd (n = 39) | IVIg (n = 38) | p value |
|---|---|---|---|
| Time to response, day | 4.0 (1–15) | 3.0 (1–21) | 0.146 |
| Time to complete response, day | 13.5 (2–69) | 6.0 (1–35) | 0.002 |
| Time to peak response, day | 53.0 (7–182) | 22.0 (3–138) | 0.353 |
Values are presented as median (range).
Methyl-Pd, methylprednisolone; IVIg, intravenous immune globulin.
The median duration of steroid maintenance was 3.0 months (range, 1.5 to 120) for methyl-Pd treatment and 3.0 months (range, 1 to 32) for IVIg treatment, and the number of patients requiring steroids for > 2 months was 35 (89.7%) and 33 (86.8%), respectively (p = 0.692).
Long-term follow-up data
One year after treatment initiation, 14 of 30 patients (46.7%) maintained response in the methyl-Pd treatment group as did 15 of 29 patients (51.7%) in the IVIg group (p = 0.698). Two years after treatment initiation, 10 of 28 patients (35.7%) maintained response in the methyl-Pd group as did 12 of 26 patients (46.2%) in the IVIg group (p = 0.435). Five years after treatment initiation, seven of 18 patients (38.7%) maintained response in the methyl-Pd treatment group as did five of 14 patients (35.7%) in the IVIg group (p = 0.854). At 5 years after treatment initiation, three (16.7%) and two patients (14.3%) were refractory in the methyl-Pd and IVIg groups, respectively (p = 0.854). During the follow-up period, 22 of 30 patients (73.3%) and 18 of 33 patients (55.5%) had lost their response in the methyl-Pd and IVIg groups, respectively (p = 0.326); and 19 (50.0%) and 18 patients (46.2%) required one or more salvage treatments in the methyl-Pd and IVIg groups, respectively (p = 0.736) (Tables 5 and 6).
Table 5.
Long-term follow-up data
| Variable | Methyl-Pd (n = 39) | IVIg (n = 38) | p value |
|---|---|---|---|
| Maintenance of response at 1 year | 14/30 (46.7) | 15/29 (51.7) | 0.698 |
| Refractory state at 1 year | 2/30 (6.7) | 1/29 (3.4) | 0.574 |
| Maintenance of response at 2 years | 10/28 (35.7) | 12/26 (46.2) | 0.435 |
| Refractory state at 2 years | 2/28 (7.1) | 1/26 (3.8) | 0.597 |
| Maintenance of response at 5 years | 7/18 (38.9) | 5/14 (35.7) | 0.854 |
| Refractory state at 5 years | 3/18 (16.7) | 2/14 (14.3) | 0.854 |
| Loss of CR or R | 20/30 (66.7) | 18/33 (54.5) | 0.326 |
| Time to loss of CR or R, mon | 6.5 (2–72) | 3.5 (0.5–44) | 0.243 |
| Salvage therapy | 19 (50.0) | 18 (46.2) | 0.736 |
Values are presented as number (%) or median (range).
Methyl-Pd, methylprednisolone; IVIg, intravenous immune globulin; CR, complete response; R, response.
Table 6.
Salvage therapy
| Variable | Methyl-Pd (n = 39) | IVIg (n = 38) | p value |
|---|---|---|---|
| Switch to each other | 17 | 14 | - |
| Danazol | 5 | 1 | - |
| Azathioprine | 6 | 6 | - |
| Rituximab | 1 | 0 | - |
| TPO-R agonist | 0 | 1 | - |
| Splenectomy | 2 | 4 | - |
| Others | 4 | 2 | - |
| Total no. (%) | 19 (48.7) | 18 (47.4) | 0.906 |
Methyl-Pd, methylprednisolone; IVIg, intravenous immune globulin; TPO-R, thrombopoietin receptor.
Adverse events
During the first 6 months after initiation of treatment, six patients (15.4%) gained weight, three patients (7.7%) had hyperglycemia, and one patient (2.5%) had a urinary tract infection in the methyl-Pd treatment group. In the IVIg group, two patients (5.3%) had weight gain, four patients (10.5%) had hyperglycemia, and one patient (2.6%) had a urinary tract infection. There was no bleedingrelated mortality during the first 6 months. However, in the methyl-PD treatment group, one patient who achieved complete response after initial treatment died from relapsed disease by intracranial hemorrhage after 8 years of treatment (Table 7).
Table 7.
Adverse events
| Variable | Methyl-Pd (n = 39) | IVIg (n = 38) | p value |
|---|---|---|---|
| Weight gain | 6/39 (15.4) | 2/38 (5.3) | 0.146 |
| Hyperglycemia | 3/39 (7.7) | 4/39 (10.5) | 0.665 |
| Infection (UTI) | 1/39 (2.6) | 1/38 (2.6) | 0.985 |
| Bleeding related-death | 0/39 (0.0) | 0/38 (0.0) | - |
| Total | 10/39 (25.6) | 7/38 (18.4) | 0.445 |
Values are presented as number (%).
Methyl-Pd, methylprednisolone; IVIg, intravenous immune globulin; UTI, urinary tract infection.
DISCUSSION
This study demonstrated that ITP treatment with either intravenous methyl-Pd followed by oral Pd, or intravenous IVIg together with oral Pd, had similar efficacies in terms of the initial response and sustained response. A limited number of randomized controlled trials (RCT) for the treatment of ITP have been conducted. A RCT conducted by Godeau et al. [4] demonstrated that administration of IVIg with oral Pd had superior efficacy to intravenous methyl-Pd with oral Pd in front-line treatment of adult ITP; however, the primary outcome of their study was the number of days with a platelet count greater than 50 × 109/L and the response assessment time points differed from those used in this study. While most recent studies [5,6] assessed response rates between days 7 to 10, Godeau et al. [4] assessed response rate at days 2 and 5 after treatment initiation. This is considered an early time point for response rate measurement because IVIg more rapidly increases platelet count than methyl-Pd. Thus, IVIg with oral Pd appeared to produce a better response than methyl-Pd treatment in their study. In addition, Godeau et al. [4] used response criteria that differed from the standardized criteria of the International Working Group on ITP. To our knowledge, this study is the first to compare these two treatment strategies in previously untreated adult ITP patients, according to the standardized criteria of the International Working Group on ITP.
Favorable maintenance response rates of ≤ 60% at 6 months after treatment initiation were demonstrated for both treatments, comparable to the outcomes of recent studies on rituximab treatment [7,8]. Zaja et al. [7] reported that front-line therapy using dexamethasone with rituximab in newly diagnosed ITP patients had a sustained response rate of 63% at 6 months after treatment initiation; however, ≤ 10% of patients experienced serious adverse events caused by rituximab. In our study, the side effects of the treatment regimen were transient and no serious adverse events were reported. The favorable results of maintenance response observed in this study were likely attributed to the effects of oral Pd, administered for a median of 3 months. Similarly, Godeau et al. [4] reported that treatment with methyl-Pd or IVIg in combination with oral Pd had a longer median time to failure than treatment without oral Pd and the adverse effects of oral steroid treatment were tolerable.
In this study, the IVIg treatment group achieved a complete response more rapidly than the methyl-Pd treatment group. Since its initial use approximately 30 years ago, it has been well established that the response to IVIg is rapid but transient, and platelet counts drift back to pretreatment levels 3 to 4 weeks following IVIg treatment [3,9]. This IVIg response pattern is considered to be caused by the mechanism of action of IVIg, which blocks and modulates the macrophage activating Fc receptors in the reticuloendothelial system [10,11]. Thus, IVIg is considered more effective in situations requiring a rapid increase in platelet count, such as serious bleeding or urgent surgery. However, IVIg is much more expensive than methyl-Pd in Korea. The cost of IVIg (IVGlobulin SN 2.5 g, Green Cross Corp., Yongin, Korea) treatment is about 2 million Korean won and the cost of methyl-pd (PREDISOL INJ, Reyon Pharm Corp., Seongnam, Korea) treatment is only 10 thousand Korean won. Thus, in view of cost-effectiveness, methyl-Pd is beneficial to patients with a low risk of bleeding.
A large percentage of patients were followed up for a long time in our study; approximately 70% by year 2 and 40% by year 5. This long-term follow-up data revealed that loss of response increased over time. It is well known that ITP in adults is a chronic disease in most cases [12,13]. However, most patients who were in chronic- phase ITP showed a response to salvage therapy; just ≤ 15% of patients were in a refractory state. Certainly, the patients who lost CR or R did not all undergo salvage therapy in this study, because the ITP treatment objective was for patients to live free from bleeding risk, providing increased quality of life [2,14]. In this study, few patients used rituximab and thrombopoietin receptor agonists as a salvage therapy due to their cost in Korea. A greater number of patients who lost CR or R were in the methyl-Pd treatment group rather than the IVIg group. Time to loss of CR or R was also longer in the methyl-Pd treatment group compared to the IVIg group, likely due to the longer follow-up period of the methyl-Pd treatment regimen. The bleeding-related mortality rate in this study was 1.1% during the follow-up period, which is comparable to that reported previously. A recent reports by Norgaard et al. [13] demonstrated a 1.4% rate of intracranial bleeding and 2.3 rate ratios of 5-year allcause mortality. In this study, the methyl-Pd treatment group had more female patients than those in the IVIg group. This limitation was due to the retrospective nature of this study, but no differences in clinical outcome or response to treatment were observed between genders in patients with ITP [15].
In conclusion, the early and maintenance response rates of methyl-Pd and IVIg treatment regimens for ITP are similar. However, in special situations such as active bleeding or urgent surgery, IVIg is to be preferred for its rapid response.
KEY MESSAGE
1. The early and maintenance response rates of methylprednisolone and intravenous immune globulin (IVIg) treatment regimens for immune thrombocytopenia are similar.
2. IVIg is to be preferred for its rapid response in special situations such as active bleeding or urgent surgery.
Footnotes
No potential conflict of interest relevant to this article was reported.
Supplementary Materials
Number of patients and dose of platelet transfusion in the initial treatment
REFERENCES
- 1.Rodeghiero F, Stasi R, Gernsheimer T, et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood. 2009;113:2386–2393. doi: 10.1182/blood-2008-07-162503. [DOI] [PubMed] [Google Scholar]
- 2.Neunert C, Lim W, Crowther M, et al. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117:4190–4207. doi: 10.1182/blood-2010-08-302984. [DOI] [PubMed] [Google Scholar]
- 3.Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115:168–186. doi: 10.1182/blood-2009-06-225565. [DOI] [PubMed] [Google Scholar]
- 4.Godeau B, Chevret S, Varet B, et al. Intravenous immunoglobulin or high-dose methylprednisolone, with or without oral prednisone, for adults with untreated severe autoimmune thrombocytopenic purpura: a randomised, multicentre trial. Lancet. 2002;359:23–29. doi: 10.1016/S0140-6736(02)07275-6. [DOI] [PubMed] [Google Scholar]
- 5.Cheng Y, Wong RS, Soo YO, et al. Initial treatment of immune thrombocytopenic purpura with high-dose dexamethasone. N Engl J Med. 2003;349:831–836. doi: 10.1056/NEJMoa030254. [DOI] [PubMed] [Google Scholar]
- 6.Mazzucconi MG, Fazi P, Bernasconi S, et al. Therapy with high-dose dexamethasone (HD-DXM) in previously untreated patients affected by idiopathic thrombocytopenic purpura: a GIMEMA experience. Blood. 2007;109:1401–1407. doi: 10.1182/blood-2005-12-015222. [DOI] [PubMed] [Google Scholar]
- 7.Zaja F, Baccarani M, Mazza P, et al. Dexamethasone plus rituximab yields higher sustained response rates than dexamethasone monotherapy in adults with primary immune thrombocytopenia. Blood. 2010;115:2755–2762. doi: 10.1182/blood-2009-07-229815. [DOI] [PubMed] [Google Scholar]
- 8.Gudbrandsdottir S, Birgens HS, Frederiksen H, et al. Rituximab and dexamethasone vs dexamethasone monotherapy in newly diagnosed patients with primary immune thrombocytopenia. Blood. 2013;121:1976–1981. doi: 10.1182/blood-2012-09-455691. [DOI] [PubMed] [Google Scholar]
- 9.Newland AC, Treleaven JG, Minchinton RM, Waters AH. High-dose intravenous IgG in adults with autoimmune thrombocytopenia. Lancet. 1983;1:84–87. doi: 10.1016/s0140-6736(83)91738-5. [DOI] [PubMed] [Google Scholar]
- 10.Gelfand EW. Intravenous immune globulin in autoimmune and inflammatory diseases. N Engl J Med. 2012;367:2015–2025. doi: 10.1056/NEJMra1009433. [DOI] [PubMed] [Google Scholar]
- 11.Siragam V, Crow AR, Brinc D, Song S, Freedman J, Lazarus AH. Intravenous immunoglobulin ameliorates ITP via activating Fc gamma receptors on dendritic cells. Nat Med. 2006;12:688–692. doi: 10.1038/nm1416. [DOI] [PubMed] [Google Scholar]
- 12.Schoonen WM, Kucera G, Coalson J, et al. Epidemiology of immune thrombocytopenic purpura in the General Practice Research Database. Br J Haematol. 2009;145:235–244. doi: 10.1111/j.1365-2141.2009.07615.x. [DOI] [PubMed] [Google Scholar]
- 13.Norgaard M, Jensen AO, Engebjerg MC, et al. Long-term clinical outcomes of patients with primary chronic immune thrombocytopenia: a Danish population-based cohort study. Blood. 2011;117:3514–3520. doi: 10.1182/blood-2010-10-312819. [DOI] [PubMed] [Google Scholar]
- 14.Cines DB, Bussel JB. How I treat idiopathic thrombocytopenic purpura (ITP) Blood. 2005;106:2244–2251. doi: 10.1182/blood-2004-12-4598. [DOI] [PubMed] [Google Scholar]
- 15.Andres E, Mecili M, Fothergill H, Zimmer J, Vogel T, Maloisel F. Gender-related analysis of the clinical presentation, treatment response and outcome in patients with immune thrombocytopenia. Presse Med. 2012;41:e426. doi: 10.1016/j.lpm.2012.02.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Number of patients and dose of platelet transfusion in the initial treatment


