Abstract
The most important prognostic factor in oral squamous cell carcinoma (OSCC) is neck metastasis, which is treated by neck dissection. Although selective neck dissection (SND) is a useful tool for clinically node-negative OSCC, its efficacy for neck node-positive OSCC has not been established. Sixty-eight OSCC patients with pN1–3 disease who were treated with curative surgery using SND and/or modified-radical/radical neck dissection (MRND/RND) were retrospectively reviewed. The neck control rate was 94% for pN1–3 patients who underwent SND. The five-year overall survival (OS) and disease-specific survival (DSS) in pN1-3 OSCC patients were 62% and 71%, respectively. The multivariate analysis of clinical and pathological variables identified the number of positive nodes as an independent predictor of SND outcome (OS, hazard ratio (HR) = 4.98, 95% confidence interval (CI): 1.48–16.72, p < 0.01; DSS, HR = 6.44, 95% CI: 1.76–23.50, p < 0.01). The results of this retrospective study showed that only SND for neck node-positive OSCC was appropriate for those with up to 2 lymph nodes that had a largest diameter ≤3 cm without extranodal extension (ENE) of the neck and adjuvant radiotherapy. However, the availability of postoperative therapeutic options for high-risk OSCC, including ENE and/or multiple positive lymph nodes, needs to be further investigated.
Keywords: oral squamous cell carcinoma, selective neck dissection, survival, metastatic nodal parameters, pathologically positive nodes
1. Introduction
Oral squamous cell carcinoma (OSCC) constitutes a broad range of tumors with diverse etiologies that are classified by region. The estimated age-standardized rate is relatively large at 2.7 per 100,000. This rate is 3.7 among men and 1.8 among women, with an estimated 202,000 patients newly diagnosed with oral cancer in 2012 [1]. It is widely accepted that OSCC metastasizes, which usually occurs through the lymphatic system to the cervical lymph nodes, with the most important prognostic factor being the presence of neck metastasis [2,3,4,5]. Therefore, ablation surgery of the primary OSCC with appropriate neck dissection is considered to be the standard treatment modality. Indeed, some authors have shown that the failure pattern among OSCC patients is approximately 30%, which is typically due to regional metastases [6,7]. Thus, pathologically proven lymph node metastases (pN+) are recognized as an adverse prognostic factor in OSCC.
Most surgeons support comprehensive neck dissection, such as modified radical neck dissection (MRND) or radical neck dissection (RND), for the basic management of regional disease in patients with clinically positive node (cN+) involvement [8,9]. On the other hand, selective neck dissection (SND) removes lymph node groups at designated anatomic levels. Therefore, SND results in improved quality of life and a lower likelihood of orofacial or shoulder dysfunction compared to comprehensive neck dissection [10,11]. In OSCC, SND (of levels I–III) is generally accepted as a regional treatment option because OSCC mainly drains into neck levels I, II and III [6,9,12]. Therefore, for the management of regional lymph nodes in OSCC, SND (I–III) has become the standard elective procedure for clinically node-negative (cN0) patients or those with microscopic disease [13,14]. With respect to the management of cN+ OSCC, some authors agree that SND (I–III) may be considered together with adequate removal of the gross tumor with or without adjuvant radiotherapy [15,16,17]. However, whether therapeutic SND (I–III) is appropriate for cN+ disease in the neck remains unclear because the objective measures for patient selection have not been clearly defined [17].
The aim of this retrospective study was to evaluate the efficacy and outcomes of SND (I–III) for pN+ OSCC. In addition, we examined the prognostic significance of node-related factors in pN+ OSCC in order to evaluate SND (I–III) for pN+ OSCC.
2. Results
2.1. Outcomes and 5-Year Survival in Patients Who Underwent Neck Dissection
Recurrences at primary, regional and distant sites were demonstrated in 37 (28%), 11 (8%) and 3 (2%) of 131 patients who underwent neck dissection, respectively. The five-year overall survival (OS) was 67% for 131 patients: 80% for cN0, 68% for cN1 and 54% for cN2. Furthermore, the five-year OS was 77% for patients with pN0 and 55% (p = 0.01) for patients with pN+ during the follow-up interval, which ranged from 28 to 154 months with a median follow-up time of 77 months. Similarly, the five-year disease-specific survival (DSS) was 88% for patients with pN0 and 61% for patients with pN+ (p < 0.01).
Of the 131 patients who received neck dissection as the definitive surgery, the pathologic examination of the neck dissection specimens revealed metastatic lymph nodes in 68 patients (52%). Ipsilateral, bilateral and contralateral metastases were found in 54 patients, 13 patients and 1 patient, respectively (Table 1). With a minimum follow-up duration of 42 months for survivors in 68 patients with pN+, 26 patients (38%) died of OSCC and 7 (10%) died from other causes.
Table 1.
Ipsilateral and bilateral or contralateral neck dissection according to type of neck dissection in 68 patients with pathologically node-positive oral squamous cell carcinoma.
| Ipsilateral and Bilateral or Contralateral Neck Dissection | Type of Neck Dissection | |||
|---|---|---|---|---|
| Selective Neck Dissection | Modified Radical Neck Dissection | Radical Neck Dissection | ||
| Ipsilateral neck dissection | (n = 54) | 31 | 19 | 4 |
| Bi-or contralateral neck dissection | (n = 14) | 4 | 9 | 1 |
2.2. Regional Control and Prognostic Factors in 35 Node-Positive OSCC Patients Underwent SND (I–III)
Among the 68 patients with pN+ disease, 35 patients (51%) underwent SND (I–III), 28 patients underwent MRND and 5 patients underwent RND. The distribution of ipsilateral and contralateral metastasis according to the extent of neck dissection is shown in Table 2. The frozen section diagnoses of level III lymph nodes did not detect micrometastasis in 5 necks.
Table 2.
Level of lymph node involvement in 68 patients with pN+ and 35 pN+ who underwent SND.
| Neck Side | Lymph Node Level | Total Number of Positive Necks (81 Necks a) | SND (39 Necks a) |
|---|---|---|---|
| Ipsilateral | I | 28 | 23 |
| I + II | 6 | 3 | |
| I + II + III | 3 | 0 | |
| I + II + III + IV | 1 | 0 | |
| I + II + III + V | 1 | 0 | |
| I + II + III + IV + V | 1 | 0 | |
| I + III | 4 | 0 | |
| I + III + IV | 1 | 0 | |
| II | 12 | 6 | |
| II + III | 3 | 0 | |
| III | 7 | 4 | |
| Contralateral | I | 9 | 2 |
| I + II | 1 | 0 | |
| I + II + III + IV | 2 | 0 | |
| II + III | 1 | 0 | |
| III | 1 | 1 |
pN+, pathologically node-positive; SND, selective neck dissection; a, number of positive necks.
A total of 10 patients developed regional recurrence: 4 of these had undergone selective neck dissection (4/35, 11%), 5 had undergone MRND (5/28, 18%) and 1 had undergone RND (1/5, 20%). Regional recurrences were well controlled as this occurred only in two patients who underwent SND (Table 3). The five-year OS and DSS of the 35 pN+ OSCC patients who underwent SND were 62% and 71%, respectively (Table 4).
Table 3.
Clinical variables in patients with node-positive oral squamous cell carcinoma.
| Variable | Total Number of Patients with pN+ (%) | SND | |
|---|---|---|---|
| No. of patients | 68 | 35 | |
| Sex | Male | 40 (59) | 24 |
| Female | 28 (19) | 11 | |
| Age (years) | ≤69 | 36 (53) | 22 |
| >69 | 32 (47) | 13 | |
| Site | Oral tongue | 28 (41) | 8 |
| Floor of mouth | 11 (16) | 8 | |
| Upper gum | 4 (6) | 2 | |
| Lower gum | 15 (22) | 10 | |
| Buccal mucosa | 10 (15) | 7 | |
| Treatment | Surgery | 38 (56) | 18 |
| Neoadjuvant chemotherapy and/or radiotherapy plus surgery | 30 (44) | 17 | |
| cT classification | cT1 | 12 (18) | 7 |
| cT2 | 32 (47) | 18 | |
| cT3 | 6 (9) | 2 | |
| cT4 | 18 (26) | 8 | |
| cN classification | cN0 | 27 (40) | 15 |
| cN1 | 10 (15) | 7 | |
| cN2 | 31 (45) | 13 | |
| cTNM stage | I | 9 (13) | 5 |
| II | 16 (24) | 9 | |
| III | 7 (10) | 4 | |
| IV | 36 (53) | 17 | |
| Type of neck dissection | Elective | 6 (9) | 5 |
| Therapeutic | 62 (91) | 30 | |
| Adjuvant radiotherapy | No | 56 (82) | 31 |
| Yes | 12 (18) | 4 | |
| Local recurrence | No | 48 (71) | 24 |
| Yes | 20 (29) | 11 | |
| Regional recurrence | No | 58 (85) | 31 |
| Yes | 10 (15) | 4 | |
| Regional control | No | 8 (12) | 2 |
| Yes | 60 (88) | 33 | |
pN+, pathologically node-positive; SND, selective neck dissection.
Table 4.
Treatment, pathologic variables and five-year survival in 35 pN+ OSCC patients who underwent SND (I–III).
| Variable | No. of Patients | Five-Year Survival | ||||
|---|---|---|---|---|---|---|
| OS (%) | p-Value a | DSS (%) | p-Value a | |||
| Total | 35 | 62 | - | 71 | - | |
| Treatment | Surgery | 18 | 78 | 0.08 | 83 | 0.13 |
| Neoadjuvant chemotherapy and/or radiotherapy plus surgery | 17 | 46 | 58 | |||
| Type of neck dissection | Elective | 5 | 40 | 0.35 | 53 | 0.63 |
| Therapeutic | 30 | 66 | 73 | |||
| cN classification | cN0 | 15 | 73 | 0.41 | 86 | 0.15 |
| cN1 | 7 | 54 | 71 | |||
| cN2 | 13 | 54 | 54 | |||
| Tumor grade | Grade 1 | 17 | 76 | 0.19 | 88 | 0.03 |
| Grade 2 | 16 | 50 | 50 | |||
| Grade 3 | 2 | 50 | 100 | |||
| pN classification | pN1 | 18 | 77 | 0.12 | 82 | 0.16 |
| pN2 | 13 | 43 | 54 | |||
| pN3 | 4 | 50 | 75 | |||
| Highest positive anatomic level | I | 20 | 75 | 0.16 | 85 | 0.11 |
| II | 10 | 40 | 50 | |||
| III | 5 | 60 | 60 | |||
| Number of positive nodes | ≤2 | 30 | 69 | <0.01 | 79 | <0.01 |
| >2 | 5 | 20 | 20 | |||
| Microscopic ENE | Absent | 31 | 64 | 0.52 | 71 | 0.98 |
| Present | 4 | 50 | 75 | |||
| Mean number of dissected lymph nodes | ≤18 | 22 | 58 | 0.73 | 68 | 0.74 |
| >18 | 13 | 69 | 77 | |||
| LND | ≤0.11 | 27 | 70 | 0.06 | 77 | 0.10 |
| >0.11 | 8 | 33 | 50 | |||
| Lymphovascular emboli | No | 30 | 62 | 0.86 | 73 | 0.58 |
| Yes | 5 | 60 | 60 | |||
| Perineural invasion | No | 32 | 62 | 0.93 | 71 | 0.88 |
| Yes | 3 | 67 | 67 | |||
| Surgical margin status | Negative | 33 | 66 | <0.01 | 75 | <0.01 |
| Positive | 2 | 0 | 0 | |||
| Tumor budding | <5 | 14 | 79 | 0.68 | 79 | 0.25 |
| 5–10 | 16 | 69 | 56 | |||
| ≥10 | 5 | 60 | 40 | |||
| CD8+ T-cell density | ≥64 cells | 6 | 50 | 0.63 | 83 | 0.54 |
| <64 cells | 27 | 66 | 70 | |||
| Mode of invasion | Grade 1 + 2 + 3 | 25 | 66 | 0.40 | 79 | 0.12 |
| Grade 4C | 6 | 50 | 50 | |||
| Grade 4D | 4 | 50 | 50 | |||
| Worst pattern of invasion (WPOI) | WPOI-1 + 2 + 3 + 4 | 33 | 62 | 0.61 | 72 | 0.44 |
| WPOI-5 | 2 | 50 | 50 | |||
| Adjuvant radiotherapy | No | 31 | 60 | 0.55 | 67 | 0.21 |
| Yes | 4 | 75 | 100 | |||
SND, selective neck dissection; OS, overall survival; DSS, disease-specific survival; ENE, extranodal extension; LND, lymph node density; pN+, pathologically node-positive. a, Log-rank test.
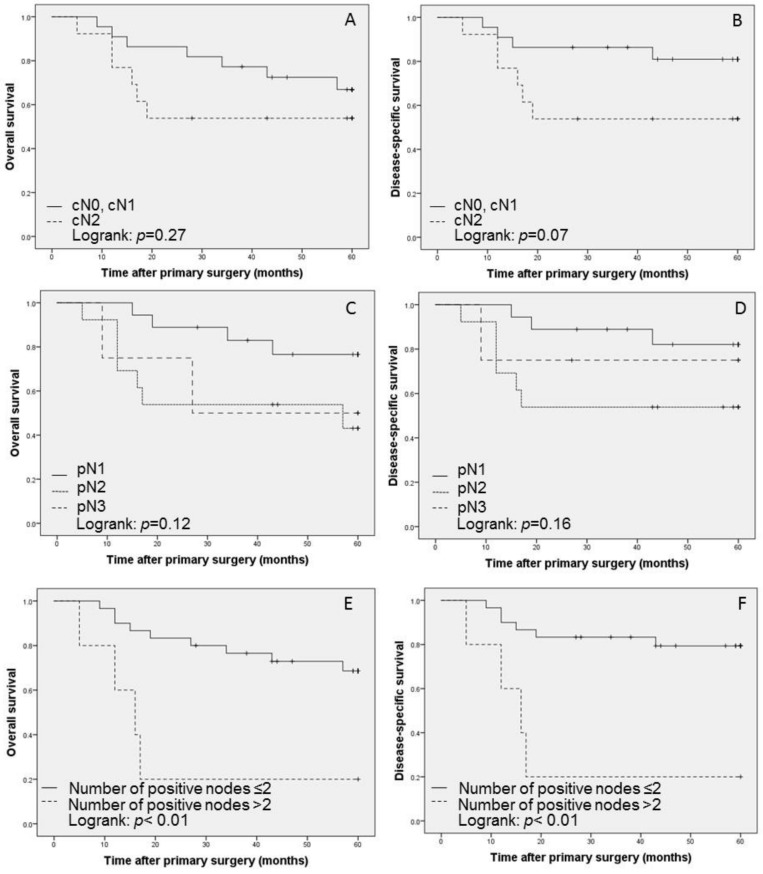
The number of lymph nodes resected ranged from 6 to 42 (mean, 18) and the number of positive lymph nodes was 1–5 (mean, 2). When the cutoff point for metastatic lymph nodes was set at 2, there were 30 patients with ≤2 and 5 patients with >2. The number of positive lymph nodes significantly affected OS and DSS (p < 0.01, Figure 1). Microscopic extranodal extension (ENE) was present in 4 patients, with no significant effect on OS and DSS in the univariate analysis (p = 0.52 and p = 0.98, respectively). The total number of excised lymph nodes was neither associated with OS nor DSS. The lymph node density (LND) was calculated as the ratio of positive lymph nodes to the total number of lymph nodes removed. The mean LND was 0.11 (range 0.01–0.33). When the cutoff value for high and low LND was set at 0.11, based upon the mean LND, a high LND was also not correlated with low OS and DSS (p = 0.06 and p = 0.10, respectively) in the univariate analysis.
Figure 1.
The five-year Kaplan–Meier survival estimates by extent of neck dissection for overall survival (A, C and E) and disease-specific survival (B, D and F); A and B show the survival curves of cN0, cN1 versus cN2. C and D show the survival curves of pN1 versus pN2 versus pN3. According to the number of positive lymph nodes (divided into ≤2: E, F and >2: E, F).
In 35 pN+ patients who underwent SND (I–III), the number of positive nodes and surgical margin status were associated with lower survival rates for both OS and DSS in the univariate analysis. The final stepwise selection in the Cox proportional hazards regression model revealed that the number of positive nodes was an independent predictor of outcome for patients who received SND (I–III) (hazard ratio (HR) = 4.98, 95% confidence interval (CI): 1.48–16.72, p < 0.01 for OS; HR = 6.44, 95% CI: 1.76–23.50, p < 0.01 for DSS) (Table 5).
Table 5.
Multivariate Cox hazards regression model for the factors influencing overall survival and disease-specific survival in patients with node-positive squamous cell carcinoma who underwent selective neck dissection.
| Variable | Factors | Overall Survival | ||
|---|---|---|---|---|
| HR | 95% CI | p-Value | ||
| Before stepwise selection | ||||
| Surgical margin status | Positive | 1.98 | 0.26–14.92 | 0.50 |
| Number of positive nodes | >2 | 3.82 | 0.81–17.86 | 0.08 |
| After stepwise selection | ||||
| Number of positive nodes | >2 | 4.98 | 1.48–16.72 | <0.01 |
| Variable | Factors | Disease-Specific Survival | ||
| HR | 95% CI | p-Value | ||
| Before stepwise selection | ||||
| Tumor grade | Grade 2 + 3 | 1.98 | 0.69–5.72 | 0.20 |
| Surgical margin status | Positive | 1.08 | 0.14–8.30 | 0.93 |
| Number of positive nodes | >2 | 6.17 | 1.17–32.38 | 0.03 |
| After stepwise selection | ||||
| Number of positive nodes | >2 | 6.44 | 1.76–23.50 | <0.01 |
CI: confidence interval; HR: hazard ratio.
3. Discussion
The current retrospective comparative study that examined SND (I–III) and MRND/RND confirmed that only SND (I–III) with (4 patients) or without (31 patients) adjuvant radiotherapy for OSCC with pN+ that were limited to levels I and II was appropriate for patients with up to 2 tumor-positive lymph nodes with a largest tumor diameter of ≤3 cm rather than the immunohistochemical invasive tumor patterns or density of tumor–infiltrating CD8+ T cells. Some authors have suggested that SND (I–III) combined with adjuvant radiotherapy is a management strategy with high efficacy and minor morbidity for selecting pN+ OSCC patients [16,17,18]. However, most of these conclusions were not based on a comparison of SND (I–III) and MRND/RND. In addition, the selected patients were not appropriately defined. In a meta-analysis comparing SND with MRND/RND in OSCC patients with cN+ disease, Liang et al. [19] also suggested that cN+ OSCC patients treated with SND (I, I–III or I–IV) that was followed by adjuvant therapy had comparable clinical outcomes to MRND/RND because no significant difference was found for regional recurrence, OS or DSS between any of the dissection treatment types. However, the extent and selection of the SND levels differed between studies rather than being limited to the dissected fields of I–II. Moreover, the ipsilateral neck recurrence rates ranged from 8–15% for the SND group and from 3–16% for the MRND/RND group. Similar ipsilateral neck recurrence rates were found in the current study (11% for the SND group; 14% for the MRND/RND group), with regional control rates of 94% for the SND (I–III) group and 86% for the MRND/RND group. These results indicate that SND (I–III) could achieve good regional control and had a favorable prognosis for pN+ OSCC in the present cohort. For head and neck squamous cell carcinoma, including OSCC, Schmitz et al. [20] suggested that postoperative irradiation is not justified for pN1 neck disease without microscopic ENE.
Nodal fixation and gross ENE are considered as contraindications for SND as highlighted by Rodrigo et al. [21]. Thus, ENE is a predictor for worse prognosis of OSCC, while ENE does not serve as an independent prognostic factor [17], as shown in the present study. In particular, microscopic ENE is generally not easily detected by either physical examination or various imaging techniques.
In a series of 400 OSCC patients with primary surgery combined with neck dissection, Rogers et al. [22] reported that OS and DSS among 175 patients with pN+ disease had rates of 36% and 52%, respectively, compared to 67% and 87% among 314 patients with pN0 OSCC (p < 0.01 and p < 0.01, respectively). The outcomes for the 63 pN+ OSCC patients in the current study, with five-year OS of 57% and DSS of 63%, are comparable with the aforementioned cohorts. The major reason for the good survival of pN+ OSCC patients in the current study was the favorable outcomes for those with delayed neck development. It is well known that the adverse outcomes associated with delayed neck dissection can partly be explained by the fact that patients developing delayed cervical lymph node metastasis have a more advanced nodal stage. In our previous publications, we also postulated that the mode of invasion was associated with poor prognosis in patients with OSCC and with delayed cervical lymph node metastasis in patients with cN0 OSCC [23,24,25]. Therefore, after these results were obtained, we adopted a follow-up strategy of watchful waiting, especially for patients having grades 4C and 4D modes of invasion with node-negative OSCC, who were followed up carefully at short intervals in order to detect and treat delayed cervical lymph node metastasis as early as possible. By doing this, we could achieve favorable survival for patients with pN+ OSCC. Moreover, lymph nodes are vital immunological organs as they are essentially information marketplaces where antigen-presenting cells, the body’s scouts, come to display information that they have gathered regarding antigens that they have encountered in the field and patrolling lymphocytes find that specific antigens have entered the body [26]. Based on these anatomic physiological aspects, we chose a treatment policy for the avoidance of routine elective neck dissection and SND (I–III) was adopted mainly as a therapeutic procedure rather than an elective modality of management for cN0.
The current study revealed that the number of positive nodes was an independent predictor for both OS and DSS in the SND (I–III) group.
Givi et al. [27] also reported that the number of positive nodes (≤2 vs. >2) was a predictor of poorer two-year disease-specific survival in head and neck cancer.
Although confirming the results of previous studies [28,29,30] and supporting the widely held belief that the number of tumor-positive lymph nodes is associated with the outcome, this observation does not help in treatment planning before definitive surgery. Six of the 17 patients with 3 or more positive lymph nodes developed ipsilateral regional recurrence and died of OSCC. Five of these patients had not received postoperative radiotherapy. Although the long-term follow-up results from the RTOG 9501/Intergroup Phase III Trial suggested that head and neck cancer patients with 2 or more positive cervical lymph nodes did not benefit from adjuvant chemoradiotherapy [31], the availability of postoperative therapeutic options for high-risk OSCC, including multiple positive lymph nodes, needs to be further investigated.
Recent advances in cancer immunology have validated the concept that immune cells have potential key roles for effective cancer treatment [32]. Several chemotherapeutic agents and radiotherapy can induce immunogenic modulation [33]. Based on this information, combined adjuvant therapies using chemoradiation and/or immunotherapies, for which there is already evidence of efficacy for head and neck cancer, including OSCC, such as peptide vaccines [34,35] and the anti-programmed death 1 monoclonal antibody [36], may improve the prognosis of OSCC patients with multiple cervical positive lymph nodes.
4. Materials and Methods
4.1. Patients
From January 2004 through December 2014, inpatients who underwent definitive surgery with neck dissection, including SND (I–III) or MRND/RND, at the Department of Oral Surgery, University Hospital, Sapporo Medical University for either cN+ or cN0 OSCC were screened for this retrospective study. Although the neck dissection performed was dependent upon the site, size and extent of the primary tumor and nodal disease, which was diagnosed by clinical signs, including physical examination, and imaging techniques, such as computed tomography (CT) scanning, magnetic resonance imaging, ultrasonography (US), positron-emission tomography (PET)-CT and serum tumor markers, the extent of neck dissection was decided based on the following criteria. According to the results of our previous study [25], OSCC patients having up to 2 positive nodes limited to levels I and II, in addition to cN0 OSCC with delayed nodal development, underwent SND (I–III). MRND was indicated for OSCC with cN+ at levels III, IV and V. RND was indicated for OSCC with clinical ENE. Postoperative adjuvant chemotherapy and/or radiotherapy were performed for OSCC for those with at least 3 positive nodes and/or ENE, except for patients who refused additional treatment.
Of 221 OSCC patients who had surgical treatment, 131 patients received a neck dissection (93 ipsilateral, 37 bilateral and 1 contralateral), with 108 patients receiving this procedure at the same time as the initial surgery while the remaining 23 patients had delayed neck dissection without recurrence of the primary tumor. The types of ipsilateral neck dissection administered were: SND (I–III), 82 necks; MRND, 43 necks; and RND, 5 necks. The following procedures were used to treat the contralateral neck: SND (I–III) in 32 necks; and MRND in 6 necks. When a level III positive node was confirmed under the frozen section diagnosis during SND (I–III), the neck dissection was converted to MRND. Finally, the types of neck dissection performed were: SND (I–III), 114 necks; MRND, 49 necks; and RND, 5 necks.
None of the patients received previous treatment, except for neoadjuvant chemotherapy or chemoradiotherapy. Patients were excluded from the current study if they had received any form of neck dissection with resection of a recurrent primary OSCC. The tumor extent and the histopathological grading were classified according to the American Joint Committee on Cancer/International Union against Cancer (AJCC/UICC)-TNM staging system [37,38]. Follow-up evaluations were carried out with physical examination and imaging studies as mentioned above. The follow-up rate was 94.7% and data from patients lost to follow-up were censored.
This retrospective study was conducted according to the principles stated in the 1964 Declaration of Helsinki and its subsequent revisions, which was approved by the Institutional Review Board of our university on 12 September 2017 (no. 292-1116). Informed consent or an acceptable substitute was obtained from all patients before study inclusion.
4.2. Immunohistopathologic Analysis
Immunohistochemistry was employed to detect multi-cytokeratins, identify the tumor cells and determine CD8+ T-cell density. Briefly, 4 μm serial sections from paraffin-embedded samples deparaffinized in xylene were soaked in 10 mM citrate buffer (pH 8.0) and placed in an autoclave at 121 °C for 10 min for antigen retrieval. Endogenous peroxidase was blocked by incubation with 0.3% hydrogen peroxide in methanol for 30 min. After this, the sections were incubated with a primary monoclonal antibody targeting pancytokeratin (1:200, clone AE1/AE3, abcam, Cambridge, UK) and CD8 (Clone C8/144B, Code 413201, Nichirei Bioscience, Inc. Tokyo, Japan) at 4 °C overnight. Secondary antibodies were applied as indicated for the EnVision system (EnVision+; DAKO, Glostrup, Denmark). Staining was visualized with diaminobenzidine tetrachloride. The sections were counterstained with hematoxylin, dehydrated, cleared and mounted. Following this, serial sections from the paraffin-embedded samples were stained with hematoxylin and eosin for the assessment of the mode of invasion and the worst pattern of invasion (WPOI). The presence and absence of lymphovascular invasion and perineural invasion were tabulated according to the information from the routine histopathological reports.
Tumor budding was defined as the presence of isolated single tumor cells or a small group of fewer than five cells ahead of the deep invasive tumor parts. For the assessment of tumor budding, immunostained tumor specimens were initially scanned with a ×4 objective lens (and ×10 ocular one) to select the areas with the highest density of budding. Tumor budding in the selected areas was then counted using a ×20 objective lens and the highest count per slide was used as the number of buds. The intensity of tumor budding was arbitrarily categorized into low intensity (<5 buds/field), intermediate intensity (5–10 buds/field) and high intensity (≥10 buds/field), according to the International Tumor Budding Consensus Conference (ITBCC) 2016 recommendations [39].
CD8+ T-cell density was quantitatively assessed. After the CD8+ T-cells were identified in the tumor stroma at the periphery of the tumor at a low magnification, they were counted manually in the areas of highest CD8+ intensity under 400× magnification and the cell counts were averaged as previously described [40]. The histopathological evaluation of the mode of invasion at the invasive front of the tumor was conducted according to Yamamoto et al. [23]. WPOI was assessed according to previous descriptions [41].
4.3. Statistical Analysis
To assess the association of pathologic lymph node status and clinicopathologic variables, the chi-square test and Fisher’s exact test were performed. We used the Kaplan–Meier method to estimate OS and DSS, with the univariate difference in the survival rates being assessed by the log-rank test.
Two-tailed p values of <0.05 were considered to indicate statistical significance. The variables that had prognostic potential as suggested by univariate analysis were subjected to multivariate analysis with a Cox proportional hazards regression model. The model was simplified using a stepwise selection method by removing variables that were negatively associated with survival or had p value of greater than 0.05. Statistical analyses were performed using SPSS version 23.0 for Windows (IBM Inc., Armonk, NY, USA).
5. Conclusions
The results of this retrospective study show that SND (I–III) limited to the field of levels I and II for OSCC is an appropriate management technique for up to 2 pathologically positive neck lymph nodes that are no more than 3 cm in their longest diameter. Therefore, it appears unnecessary to routinely perform an MRND/RND for cN1 OSCC.
Acknowledgments
We thank Editage (www.editage.jp) for English language editing.
Author Contributions
S.S. (Shunichi Shimura) and K.O. contributed equally to this work and should be considered co-first authors. Conceptualization, A.M. (Akihiro Miyazaki), A.M. (Akira Miyakawa) and H.H.; methodology, A.M. (Akihiro Miyazaki), A.M. (Akira Miyakawa) and H.H.; formal analysis, T.S. and S.S. (Shota Shimizu); original draft preparation, S.S. (Shunichi Shimura) and K.O.; histopathological diagnosis, T.H.; patient care and data curation, T.K., J.K. and T.I.; final review of article, A.M. (Akihiro Miyazaki) and H.H. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Funding
This study was supported by the Grant-inAid for Challenging Exploratory Research and Scientific Research (C) from the Japan Society for Promotion of Science (JSPS KAKENHI 26670872, K.O.; 16K11729, A.M.; 16K15827, H.H.).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Shield K.D., Ferlay J., Jemal A., Sankaranarayanan R., Chaturvedi A.K., Bray F., Soerjomataram I. The global incidence of lip oral cavity and pharyngeal cancers by subsite in 2012. CA Cancer J. Clin. 2017;67:51–64. doi: 10.3322/caac.21384. [DOI] [PubMed] [Google Scholar]
- 2.Huang S.F., Kang C.J., Lin C.Y., Fan K.H., Yen T.C., Wang H.M., Chen I.H., Liao C.T., Cheng A.J., Chang J.T. Neck treatment of patients with early stage oral tongue cancer: Comparison between observation, supraomohyoid dissection and extended dissection. Cancer. 2008;112:1066–1075. doi: 10.1002/cncr.23278. [DOI] [PubMed] [Google Scholar]
- 3.Ganly I., Patel S., Shah J. Early stage squamous cell cancer of the oral tongue–clinicopathologic features affecting outcome. Cancer. 2012;118:101–111. doi: 10.1002/cncr.26229. [DOI] [PubMed] [Google Scholar]
- 4.Amit M., Yen T.C., Liao C.T., Binenbaum Y., Chaturvedi P., Agarwal J.P., Kowalski L.P., Ebrahimi A., Clark J.R., Cernea C.R., et al. International Consortium for Outcome Research (ICOR) in Head and Neck Cancer. Clinical nodal stage is a significant predictor of outcome in patients with oral cavity squamous cell carcinoma and pathologically negative neck metastases: Results of the International Consortium for Outcome Research. Ann. Surg. Oncol. 2013;20:3575–3581. doi: 10.1245/s10434-013-3044-0. [DOI] [PubMed] [Google Scholar]
- 5.D’Cruz A.K., Vaish R., Kapre N., Dandekar M., Gupta S., Hawaldar R., Agarwal J.P., Pantvaidya G., Chaukar D., Deshmukh A., et al. Elective versus therapeutic neck dissection in node–negative oral cancer. N. Engl. J. Med. 2015;373:521–529. doi: 10.1056/NEJMoa1506007. [DOI] [PubMed] [Google Scholar]
- 6.Shah J.P., Candela F.C., Poddar A.K. The patterns of cervical lymph node metastases from squamous carcinoma of the oral cavity. Cancer. 1990;66:109–113. doi: 10.1002/1097-0142(19900701)66:1<109::AID-CNCR2820660120>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 7.Woolgar J.A. Detailed topography of cervical lymph-node metastases from oral squamous cell carcinoma. Int. J. Oral Maxillofac. Surg. 1997;26:3–9. doi: 10.1016/S0901-5027(97)80837-5. [DOI] [PubMed] [Google Scholar]
- 8.Ferlito A., Rinaldo A. Is radical neck dissection a current option for neck disease? Laryngoscope. 2008;118:1717–1718. doi: 10.1097/MLG.0b013e31817d9cd5. [DOI] [PubMed] [Google Scholar]
- 9.Pantvaidya G.H., Pal P., Vaidya A.D., Pai P.S., D’Cruz A.K. Prospective study of 583 neck dissections in oral cancers: Implications for clinical practice. Head Neck. 2014;36:1503–1507. doi: 10.1002/hed.23494. [DOI] [PubMed] [Google Scholar]
- 10.Chepeha D.B., Taylor R.J., Chepeha J.C., Teknos T.N., Bradford C.R., Sharma P.K., Terrell J.E., Wolf G.T. Functional assessment using Constant’s shoulder scale after modified radical and selective neck dissection. Head Neck. 2002;24:432–436. doi: 10.1002/hed.10067. [DOI] [PubMed] [Google Scholar]
- 11.Spalthoff S., Zimmerer R., Jehn P., Gellrich N.C., Handschel J., Krüskemper G. Neck dissection’s burden on the patient: Functional and psychosocial aspects in 1652 patients with oral squamous cell carcinomas. J. Oral Maxillofac. Surg. 2017;75:839–849. doi: 10.1016/j.joms.2016.09.037. [DOI] [PubMed] [Google Scholar]
- 12.Byers R.M., Wolf P.F., Ballantyne A.J. Rationale for elective modified neck dissection. Head Neck Surg. 1991;10:160–167. doi: 10.1002/hed.2890100304. [DOI] [PubMed] [Google Scholar]
- 13.Manni J.J., van den Hoogen F.J.A. Supraomohyoid neck dissection with frozen section biopsy as a staging procedure in the clinically node-negative neck in carcinoma of the oral cavity. Am. J. Surg. 1991;162:373–376. doi: 10.1016/0002-9610(91)90151-3. [DOI] [PubMed] [Google Scholar]
- 14.Brazillian Head and Neck Cancer Study Group Results of a prospective trial on elective modified radical classical versus supraomohyoid neck dissection in the management of oral squamous carcinoma. Am. J. Surg. 1998;176:422–427. doi: 10.1016/S0002-9610(98)00230-X. [DOI] [PubMed] [Google Scholar]
- 15.Kowalski L.P., Carvalho A.L. Feasibility of supraomohyoid neck dissection in N1 and N2a oral cancer patients. Head Neck. 2002;24:921–924. doi: 10.1002/hed.10127. [DOI] [PubMed] [Google Scholar]
- 16.Shin Y.S., Koh Y.W., Kim S.H., Choi E.C. Selective neck dissection for clinically node-positive oral cavity squamous cell carcinoma. Yonsei Med. J. 2013;54:139–144. doi: 10.3349/ymj.2013.54.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feng Z., Gao Y., Niu L.X., Peng X., Guo C.B. Selective versus comprehensive neck dissection in the treatment of patients with a pathologically node-positive neck with or without microscopic extracapsular spread in oral squamous cell carcinoma. Int. J. Oral Maxillofac. Surg. 2014;43:1182–1188. doi: 10.1016/j.ijom.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 18.Schiff B.A., Roberts D.B., El-Naggar A., Garden A.S., Myers J.N. Selective vs modified radical neck dissection and postoperative radiotherapy vs observation in the treatment of squamous cell carcinoma of the oral tongue. Arch. Otolaryngol. Head Neck Surg. 2005;131:874–878. doi: 10.1001/archotol.131.10.874. [DOI] [PubMed] [Google Scholar]
- 19.Liang L., Zhang T., Kong Q., Liang J., Liao G. A meta-analysis on selective versus comprehensive neck dissection in oral squamous cell carcinoma patients with clinically node-positive neck. Oral Oncol. 2015;51:1076–1081. doi: 10.1016/j.oraloncology.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Schmitz S., Machiels J.P., Weynand B., Gregoire V., Hamoir M. Results of selective neck dissection in the primary management of head and neck squamous cell carcinoma. Eur. Arch. Otorhinolaryngol. 2009;266:437–443. doi: 10.1007/s00405-008-0767-9. [DOI] [PubMed] [Google Scholar]
- 21.Rodrigo J.P., Grilli G., Shah J.P., Medina J.E., Robbins K.T., Takes R.P., Hamoir M., Kowalski L.P., Suárez C., López F., et al. Selective neck dissection in surgically treated head and neck squamous cell carcinoma patients with a clinically positive neck: Systematic review. Eur. J. Surg. Oncol. 2018;44:395–403. doi: 10.1016/j.ejso.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 22.Rogers S.N., Brown J.S., Woolgar J.A., Lowe D., Magennis P., Shaw R.J., Sutton D., Errington D., Vaughan D. Survival following primary surgery for oral cancer. Oral Oncol. 2009;45:201–211. doi: 10.1016/j.oraloncology.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 23.Yamamoto Y., Kohama G., Sunakawa E., Iwai M., Hiratsuka H. Mode of invasion, bleomycin sensitivity and clinical course in squamous cell carcinoma of the oral cavity. Cancer. 1983;51:2175–2180. doi: 10.1002/1097-0142(19830615)51:12<2175::AID-CNCR2820511205>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 24.Yamamoto E., Miyakawa A., Kohama G. Mode of invasion and lymph node metastasis in squamous cell carcinoma of the oral cavity. Head Neck Surg. 1984;6:938–947. doi: 10.1002/hed.2890060508. [DOI] [PubMed] [Google Scholar]
- 25.Hiratsuka H., Miyakawa A., Nakamori K., Kido Y., Sunakawa H., Kohama G. Multivariate analysis of occult lymph node metastasis as a prognostic indicator for patients with squamous cell carcinoma of the oral cavity. Cancer. 1997;80:351–356. doi: 10.1002/(SICI)1097-0142(19970801)80:3<351::AID-CNCR1>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 26.Willard-Mack C. Normal structure, function and histology of lymph nodes. Toxicol. Pathol. 2006;34:409–424. doi: 10.1080/01926230600867727. [DOI] [PubMed] [Google Scholar]
- 27.Givi B., Linkov G., Ganly I., Patel S.G., Wong R.J., Singh B., Boyle J.O., Shaha A.R., Shah J.P., Kraus D.H. Selective neck dissection in node-positive squamous cell carcinoma of the head and neck. Otolaryngol. Head. Neck. Surg. 2012;147:707–715. doi: 10.1177/0194599812444852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Olsen K.D., Caruso M., Foote R.L., Stanley R.J., Lewis J.E., Buskirk S.J., Frassica D.A., DeSanto L.W., O’Fallon W.M., Hoverman V.R. Primary head and neck cancer. Histopathologic predictors of recurrence after neck dissection in patients with lymph node involvement. Arch. Otolaryngol. Head Neck Surg. 1994;120:1370–1374. doi: 10.1001/archotol.1994.01880360066012. [DOI] [PubMed] [Google Scholar]
- 29.Greenberg J.S., Fowler R., Gomez J., Mo V., Roberts D., El Naggar A.K., Myers J.N. Extent of extracapsular spread: A critical prognosticator in oral tongue cancer. Cancer. 2003;97:1464–1470. doi: 10.1002/cncr.11202. [DOI] [PubMed] [Google Scholar]
- 30.Sawar F.A., Irwin C.R., Gordon D.J., Leonard A.G., Stephenson M., Napier S.S. Invasive front grading: Reliability and usefulness in the management of oral squamous cell carcinoma. J. Oral Pathol. Med. 2003;32:1–9. doi: 10.1034/j.1600-0714.2003.00060.x. [DOI] [PubMed] [Google Scholar]
- 31.Cooper J.S., Zhang Q., Pajak T.F., Forastiere A.A., Jacobs J., Saxman S.B., Kish J.A., Kim H.E., Cmelak A.J., Rotman M., et al. Long-term follow-up of the RTOG 9501/intergroup phase III trial: Postoperative concurrent radiation therapy and chemotherapy in high-risk squamous cell carcinoma of the head and neck. Int. J. Radiat. Oncol. Biol. Phys. 2012;84:1198–1205. doi: 10.1016/j.ijrobp.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Topalian S.L., Weiner G.J., Pardoll D.M. Cancer immunotherapy comes of age. J. Clin. Oncol. 2011;29:4828–4836. doi: 10.1200/JCO.2011.38.0899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bauman J.E., Cohen E., Ferris R.L., Adelstein D.J., Brizel D.M., Ridge J.A., O’Sullivan B., Burtness B.A., Butterfield L.H., Carson W.E., et al. Immunotherapy of head and neck cancer: Emerging clinical trials from a National Cancer Institute Head and Neck Cancer Steering Committee Planning Meeting. Cancer. 2017;123:1259–1271. doi: 10.1002/cncr.30449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miyazaki A., Kobayashi J., Torigoe T., Hirohashi Y., Yamamoto T., Yamaguchi A., Asanuma H., Takahashi A., Michifuri Y., Nakamori K., et al. Phase I clinical trial of survivinderived peptide vaccine therapy for patients with advanced or recurrent oral cancer. Cancer Sci. 2011;102:324–329. doi: 10.1111/j.1349-7006.2010.01789.x. [DOI] [PubMed] [Google Scholar]
- 35.Yoshitake Y., Fukuma D., Yuno A., Hirayama M., Nakayama H., Tanaka T., Nagata M., Takamune Y., Kawahara K., Nakagawa Y., et al. Phase II clinical trial of multiple peptide vaccination for advanced head and neck cancer patients revealed induction of immune responses and improved OS. Clin. Cancer Res. 2015;21:312–321. doi: 10.1158/1078-0432.CCR-14-0202. [DOI] [PubMed] [Google Scholar]
- 36.Ferris R.L., Blumenschein G., Jr., Fayette J., Guigay J., Colevas A.D., Licitra L., Harrington K., Kasper S., Vokes E.E., Even C., et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 2016;375:1856–1867. doi: 10.1056/NEJMoa1602252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amin M.B., Edge S.B., Greene F.L., Byrd D.R., Brookland R.K., Washington M.K., Gershenwald J.E., Compton C.C., Hess K.R., Sullivan D.C., et al. American Joint Committee on Cancer Staging Manual. 8th ed. Springer International Publishing; New York, NY, USA: 2017. [Google Scholar]
- 38.Brierley J.D., Gospodarowicz M.K., Wittekind C. TNM Classification of Malignant Tumours. 8th ed. Wiley-Blackwell; Hoboken, NJ, USA: 2017. [Google Scholar]
- 39.Lugli A., Kirsch R., Ajioka Y., Bosman F., Cathomas G., Dawson H., El Zimaity H., Fléjou J.F., Hansen T.P., Hartmann A., et al. Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016. Mod. Pathol. 2017;30:1299–1311. doi: 10.1038/modpathol.2017.46. [DOI] [PubMed] [Google Scholar]
- 40.Shimizu S., Hiratsuka H., Koike K., Tsuchihashi K., Sonoda T., Ogi K., Miyakawa A., Kobayashi J., Kaneko T., Igarashi T., et al. Tumor-infiltrating CD8+ T-cell density is an independent prognostic marker for oral squamous cell carcinoma. Cancer. Med. 2019;8:80–93. doi: 10.1002/cam4.1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.BrandweinGensler M., Teixeira M.S., Lewis C.M., Lee B., Rolnitzky L., Hille J.J., Genden E., Urken M.L., Wang B.Y. Oral squamous cell carcinoma: Histologic risk assessment, but not margin status, is strongly predictive of local disease-free and overall survival. Am. J. Surg. Pathol. 2005;29:167–178. doi: 10.1097/01.pas.0000149687.90710.21. [DOI] [PubMed] [Google Scholar]