Abstract
Purpose
To evaluate the changes in tear film osmolarity and Schirmer I test after cataract surgery.
Methods
This single-center, prospective study included patients with no subjective complaints about dry eye disease. Patients with the following conditions were excluded: contact lens wearers, patients with diabetes, pseudoexfoliation, pterygia, and eye drops users. The eye that had not undergone surgery was considered the control group. Tear osmolarity and Schirmer I test were evaluated before surgery and during the first postoperative month.
Results
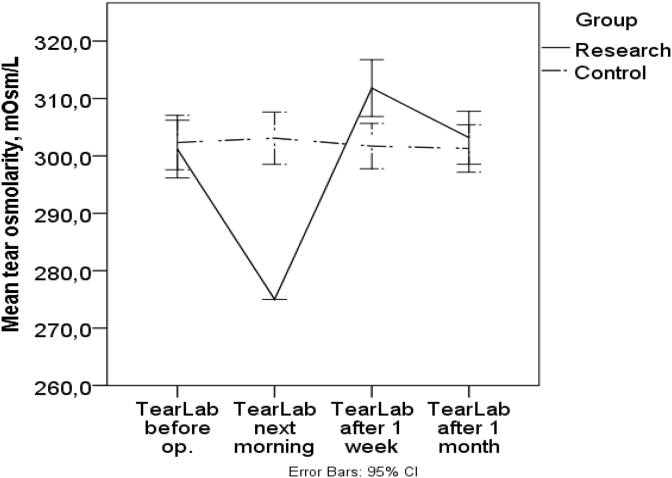
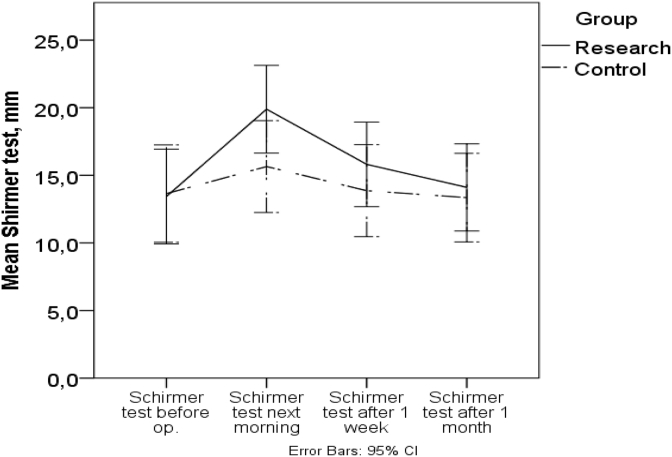
Thirty-seven patients were enrolled in the study. Before surgery, tear osmolarity was 301.2 ± 15.09 Osm/L in the study group and 302.3 ± 14.21 mOsm/L in the control group (P = 0.2), while Schirmer I test averaged 13.4 ± 10.50 mm in the study group and 13.7 ± 10.79 mm in the control group (P = 0.6). The next morning, the tear osmolarity decreased to <275 mOsm/L in the study group while in the control group, the value increased to 303.1 mOsm/L ± 13.68 (P = 0.008). The Schirmer I test in the same morning showed an increase up to 19.9 ± 9.73 mm in the study group and to 15.7 ± 10.19 mm in the control group (P = 0.01). One week later, the tear osmolarity increased to 311.8 ± 14.85 mOsm/L, while the control group averaged 301.7 ± 11.84 mOsm/L (P = 0.013). The Schirmer I test results decreased to 15.8 ± 9.37 mm in the study group and 13.9 ± 10.19 mm in the control group (P = 0.07) one week after the surgery. One month after surgery, tear osmolarity and Schirmer I test results in the study group decreased to the control group level (P > 0.05).
Conclusions
The tear osmolarity results increased to the dry eye disease level in the first postoperative week. Over the course of one month, the difference in tear osmolarity and Schirmer I test values for the study and control groups leveled off.
Keywords: Tear osmolarity, Cataract surgery, Schirmer I test, Postoperative period
Introduction
Almost every cataract surgeon has come up against a situation during the postoperative period when even though the primary goal – improvement of visual acuity – has been achieved, the patient feels frustrated because of a subjective discomfort in the operated eye. Sometimes this is a more important issue for the patient than a perfect visual outcome. Although it has been established that the ocular surface is affected during the postoperative period, there is still no generally accepted opinion about the changes in tear osmolarity after cataract surgery despite several studies dedicated to evaluation of these changes.1, 2 The present study was designed to evaluate the effect of cataract surgery on the characteristic features of ocular surface health, including tear film osmolarity and reflex tear flow in the early postoperative period.
Methods
This prospective study was conducted in the Pauls Stradins Clinical University Hospital Ophthalmology Department, Riga, Latvia, during the period from May 1 to May 31, 2017. The study excluded patients with the following dry eye symptoms: foreign body sensation, stinging, redness, burning, scratchy sensation, excessive tearing/watery eyes, stringy mucus in or around the eyes, sensitivity to light, and eye fatigue. Patients with diabetes, pseudoexfoliation syndrome, pterygia, contact lens wearers and any eye drop users were also excluded from the present study. The study was performed in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Review Board of Riga Stradins University (acceptance n. 29 decision date 30.03.2017). Informed consents were obtained.
Both eyes of the patients were examined for tear film osmolarity using the TearLab Osmolarity System (TearLab Corporation, San Diego, CA, USA) and reflex tear flow using the Schirmer test without anesthetic eye drops (Schirmer I test). The non-operated eyes of the same patients represented the control group. In order to avoid any external influence on the measurements, the tear osmolarity and Schirmer I tests were performed 2 h before surgery, before any anesthetic or mydriatic drops were used. Standard phacoemulsification surgery was performed under sub-Tenon anesthesia using lidocaine/bupivacaine solution. All surgeries were performed by the same surgeon with Infinity phaco machine (Alcon, Fort Worth, TX, USA). After the surgery, the patients received subconjunctival dexamethasone and gentamicin. In addition, all patients were treated with topical levofloxacin drops starting the day after surgery (Oftaquix, Santen, Japan). On day 1 of the postoperative care, before any eye drops were administered, the tear osmolarity and reflex tear flow were tested. Both tests were repeated 1 week and 1 month after the surgery. To avoid the influence of medical eye drops, the tests were performed at least 2 h after the last application of medication.
Statistical analyses were performed using IBM SPSS, version 22.0 (IBM Corporation, Endicott, New York, U.S.). The data is presented in the form of means and standard deviations (SD). Both groups were compared using paired t-test. The result changes in each group were evaluated by repeated measures analysis of variance (ANOVA). The P < 0.05 was chosen as statistically significant.
Results
The study included 37 patients, of which 16 (43.2%) were males and 21 (56.8%) were females. The average age was 73.1 ± 11.98 years. Preoperative tear osmolarity differed slightly, measuring 301.2 ± 15.09 mOsm/L in the study group and 302.3 ± 14.21 mOsm/L in the control group (P = 0.2). The mean preoperative Schirmer I test values were 13.4 ± 10.50 mm in the study group and 13.7 ± 10.79 mm in the control group (P = 0.6). On postoperative day 1, tear osmolarity was significantly below the reference range in all patients of the study group. The TearLab measurement range is linear ranging between 275 and 400 mOsm/L. Test results outside this range are reported as either “Below Range,” i.e., below 275 mOsm/L, or “Above Range,” i.e., above 400 mOsm/L.3 Due to the failure to obtain any reliable numerical values, because in the morning after the surgery all patients recorded a “Below range” result, the measurement of 275 mOsm/L, being the lowest value possible to register using TearLab, was used as the mean value for further statistical analysis to describe the test results of the study group. The mean tear osmolarity in the control group was slightly increased to 303.1 ± 13.68 mOsm/L on the postoperative day 1 (P = 0.008), compared to the preoperative results. The Schirmer I test results in the study group on the postoperative day 1 were increased by more than 6 mm to 19.9 ± 9.73 mm, with a 2-mm increase to 15.7 ± 10.19 mm in the control group (P = 0.01). Tear osmolarity 1 week after the surgery increased to 311.8 ± 14.85 mOsm/L in the study group, while the osmolarity in the control group remained unchanged at 301.7 ± 11.84 mOsm/L (P = 0.013). The Schirmer I test results also differed between the groups: 15.8 ± 9.37 mm in the study group and 13.9 ± 10.19 mm in the control group (P = 0.07). One month after the surgery, tear osmolarity results returned to preoperative levels of 303.2 ± 13.83 mOsm/L in the study group. The osmolarity in the control group remained almost the same as in the first postoperative week, at 301.3 ± 12.39 mOsm/L (P = 0.1). The same pattern was observed for Schirmer I test results. Measurements in the study group returned to the preoperative level of 14.1 ± 8.91 mm versus the control group at 13.4 ± 10.55 mm (P = 0.41) (Table 1; Fig. 1, Fig. 2).
Table 1.
TearLab and Schirmer test results before and during first postoperative month.
| Test | Groups | Before operation | Next morning | 1 week after | 1 month after | P-value | η2 |
|---|---|---|---|---|---|---|---|
| TearLab (mOsm/L) | Control group Mean ± SD; (min-max) | 302,32 ± 14,21; (276–337) | 303,08 ± 13,68; (280–346) | 301,70 ± 11,84; (280–333) | 301,29 ± 12,39; (276–329) | 0,20 | 0,04 |
| Research Mean ± SD; (min-max) | 301,19 ± 15,09; (276–333) | 37 patients Below Range <275,0; | 311,81 ±14,85 (281–351) | 303,16 ± 13,83 (280–332) | <0,001 | 0,79 | |
| Schirmer I test (mm) | Control group Mean ± SD; (min-max) | 13,65 ± 10,79; (2–35) | 15,65 ± 10,19; (5–35) | 13,87 ± 10,19; (3–35) | 13,47 ± 10,55; (3–35) | <0,001 | 0,19 |
| Research Mean ± SD; (min-max) | 13,43 ± 10,5; (2–35) | 19,89 ± 9,73; (6–35) | 15,81 ± 9,37; (4–35) | 14,12 ± 8,91 (3–35) | <0,001 | 0,44 |
SD: Standard deviation; min-max: Minimal – maximal; η2: Effect size.
Fig. 1.
Tear osmolarity before and after cataract surgery.
Fig. 2.
Schirmer test results before and after cataract surgery.
Comparison of the results in the study group before surgery, and 1 day, 1 week, and 1 month after the surgery showed statistically significant changes in tear osmolarity [P < 0.001, repeated measures ANOVA, effect size (η2) 0.79], while the osmolarity in the control group showed no statistically significant changes (P = 0.2, repeated measures ANOVA, η2 = 0.04). The Schirmer I test results demonstrated statistically significant changes in both groups during the first postoperative month (P < 0.001, repeated measures ANOVA); the effect size was 0.44 in the study group and 0.19 in the control group, accordingly. Comparison of the tear osmolarity changes between the study and control group revealed a significant difference at postoperative day 1 (P = 0.008, paired t-test) and week 1 after the surgery (P = 0.013, paired t-test), while the difference between the groups in the Schirmer I test results was significant only on postoperative day 1 (P = 0.01, paired t-test).
Discussion
To make the present study results more reliable and patients' tear film less affected, contact lens wearers were excluded, because the literature is divided over whether use of contact lenses increases4, 5, 6 or has no effect on tear osmolarity.7, 8, 9 The differences in the reported results are likely to be based on the wearers’ ability to maintain homeostasis of their tear film thus coping with the drying effect of the contact lenses.4 For the study to be more objective, all patients with diabetes were also excluded because diabetes has been found to increase tear osmolarity.10, 11 Different ocular conditions also seem to have different effects on tear film osmolarity. For instance, eyes with pseudoexfoliation syndrome, a condition that is thought to alter goblet cell activity and mucin production, reportedly show increased tear osmolarity when compared to the control group.12 Eyes of patients with pterygia, a predominantly inflammatory condition, also show increased tear osmolarity when compared with the control group.13 And finally, eye drops have shown various effects on tear osmolarity. Glaucoma medications increase tear osmolarity, which perhaps is due to the preservatives, while such medications did not have a significant effect on tear film breakup time or Schirmer test results.14 Artificial tears were noted by several studies to decrease tear osmolarity,15, 16, 17 but one study found no correlation between osmolarity and the use of artificial tears.18 This may be an important factor, because the type of eye drop can affect tear osmolarity.17 For instance, lower osmolarity eye drops have been associated with lower tear osmolarity.19, 20 The effect of anti-inflammatory medication on tear osmolarity is less clear, especially because the studies evaluating such effect were limited to a small sample size and the lack of a control group or randomization.21, 22, 23
A significant decrease in tear osmolarity on the postoperative day 1 and an increase one week later could be explained by the ocular surface response to significant irritation in the early postoperative period. The etiology of changes in tear film quality is multifactorial. Patient age plays a role, besides, every surgery – even minimally invasive cataract surgery – causes damage to tissue and elderly patients may take longer to recover from surgically-induced ocular trauma.24 Furthermore, tissue damage induces inflammation. In peer-reviewed literature over the last decade, increasing evidence has shown the role of inflammation in dry eye disease/ocular surface disease in both animal models and humans.25 Moreover, the influence of phacoemulsification thermal energy on corneal endothelial cells, as well as the irritant effect of bright light exposure during surgery, must be considered. Eye drops with preservatives used in the postoperative period also have an effect on tear film.21, 22, 23 In summary it can be said that dry eye disease is likely to occur in the early period after cataract surgery. As stated in the International Dry Eye WorkShop (DEWS) in 2007: “Dry eye disease is a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.”7
Another issue is the threshold value of tear osmolarity. TearLab guidelines define abnormal tear film osmolarity by the reading >300 mOsm/L, or when the inter-eye difference is >8 mOsm/L. These changes indicate a loss of homeostasis and instability of tear film.6 TearLab has also introduced the dry eye disease severity grading scale, on which 300–320 mOsm/L is ranked as mild, 320–340 mOsm/L is moderate, and any measurement >340 mOsm/L is considered severe. Evaluation of the diagnostic utility of tear osmolarity requires a cut-off value that would differentiate a healthy eye from an eye with loss of homeostasis as well as tear film instability; this is known as the threshold value. Reported tear osmolarity threshold values have varied from 305 mOsm/L to 316 mOsm/L. Currently, 308 mOsm/L is a widely accepted threshold. The tear osmolarity threshold of 308 mOsm/L was useful in correctly diagnosing dry eye and healthy ocular surface patients in 90.7% and 81.3% of the time, respectively; thus, this value appeared to be the most sensitive for differentiating between normal eyes and those demonstrating early stages of dry eye disease.26 According to the results obtained one week after cataract surgery, mean tear osmolarity in the study group increased from 301 mOsm/L to 311 mOsm/L, and the inter-eye difference increased to 10.1 mOsm/L. Therefore, 311 mOsm/L crosses the borderline normal range on the TearLab severity scale and the threshold used world-wide.
The definition of dry eye disease and significant tear osmolarity changes after cataract surgery indicate that dry eye disease is a temporary complication during the early postoperative period. Even if a significant increase in osmolarity and multifactorial etiology is registered, a closer inspection of cataract surgery as a process demonstrates that dry eye disease can only be a possibility because this research obtained no information about subjective symptomatology, which is the most important consideration in dry eye disease.
According to TearLab guidelines and generally accepted threshold values, the tear osmolarity rates and inter-eye differences in this study reached the dry eye disease level during the first week after surgery. During the first postoperative month, the TearLab and Schirmer I test differences between the study and control groups leveled off. Based on the definition from DEWS 2007, dry eye disease can be considered a temporary early complication after cataract surgery, but it has not been defined yet in terms of complexity. At the times when patient quality of life is becoming increasingly important, this study has obtained the results that will allow physicians to better understand early postoperative changes in ocular surface health after cataract surgery. This information is of value to patients as well as physicians. Tear film osmolarity and reflex tear flow changes can be used to explain temporary complications at an early stage in the postoperative period. The ability to anticipate and avoid unfavorable outcomes after cataract surgery would benefit both the patient and the surgeon.
This study has several limitations. The sample size was small, and there was no control group of dry eye patients. Also, patients with a variety of conditions predisposing eyes to postoperative dry eye, were excluded. In conclusion, this study shows significant tear film osmolarity changes in the study group the first day after cataract surgery and reaching dry eye disease level on postoperative week 1. Over the course of one month, the difference in tear osmolarity and Schirmer I test values for the study and control groups equalized. Larger studies with different categories of patients are recommended to elucidate our results.
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.González-Mesa A., Moreno-Arrones J.P., Ferrari D., Teus M.A. Role of tear osmolarity in dry eye symptoms after cataract surgery. Am J Ophthalmol. 2016;170:128–132. doi: 10.1016/j.ajo.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Oncel B., Pinarci E., Akova Y. The tear osmolarity changes after cataract surgery. Turk J Ophthalmol. 2012;42(1):35–37. [Google Scholar]
- 3.Erstad B.L. Osmolality and osmolarity: narrowing the terminology gap. Pharmacotherapy. 2003;23(9):1085–1086. doi: 10.1592/phco.23.10.1085.32751. [DOI] [PubMed] [Google Scholar]
- 4.Nichols J.J., Sinnott L.T. Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Invest Ophthalmol Vis Sci. 2006;47(4):1319–1328. doi: 10.1167/iovs.05-1392. [DOI] [PubMed] [Google Scholar]
- 5.Miller W.L., Doughty M.J., Narayanan S. A comparison of tear volume (by tear meniscus height and phenol red thread test) and tear fluid osmolality measures in non-lens wearers and in contact lens wearers. Eye Contact Lens. 2004;30(3):132–137. doi: 10.1097/01.icl.0000138714.96401.2b. [DOI] [PubMed] [Google Scholar]
- 6.Muselier-Mathieu A., Bron A.M., Mathieu B. Ocular surface assessment in soft contact lens wearers; the contribution of tear osmolarity among other tests. Acta Ophthalmol. 2014;92(4):364–369. doi: 10.1111/aos.12103. [DOI] [PubMed] [Google Scholar]
- 7.The Definition and Classification Subcommittee of the International Dry Eye WorkShop The definition and classification of dry eye disease: report of the definition and classification subcommittee of the international dry eye WorkShop. Ocul Surf. 2007;5(2):75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 8.Chen S.P., Massaro-Giordano G., Pistilli M., Schreiber C.A., Bunya V.Y. Tear osmolarity and dry eye symptoms in women using oral contraception and contact lenses. Cornea. 2013;32(4):423–428. doi: 10.1097/ICO.0b013e3182662390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alves M., Reinach P.S., Paula J.S. Comparison of diagnostic tests in distinct well-defined conditions related to dry eye disease. PLoS One. 2014;9(5) doi: 10.1371/journal.pone.0097921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sağdık H.M., Ugurbas S.H., Can M. Tear film osmolarity in patients with diabetes mellitus. Ophthalmic Res. 2013;50(1):1–5. doi: 10.1159/000345770. [DOI] [PubMed] [Google Scholar]
- 11.Oncel B.A., Pinarci E., Akova Y.A. Tear osmolarity in unilateral pseudoexfoliation syndrome. Clin Exp Optom. 2012;95(5):506–509. doi: 10.1111/j.1444-0938.2011.00683.x. [DOI] [PubMed] [Google Scholar]
- 12.Julio G., Lluch S., Pujol P., Alonso S., Merindano D. Tear osmolarity and ocular changes in pterygium. Cornea. 2012;31(12):1417–1421. doi: 10.1097/ICO.0b013e318259c934. [DOI] [PubMed] [Google Scholar]
- 13.Tomlinson A., Madden L.C., Simmons P.A. Effectiveness of dry eye therapy under conditions of environmental stress. Curr Eye Res. 2013;38(2):229–236. doi: 10.3109/02713683.2012.757323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee S.Y., Wong T.T., Chua J., Boo C., Soh Y.F., Tong L. Effect of chronic anti-glaucoma medications and trabeculectomy on tear osmolarity. Eye (Lond) 2013;27(10):1142–1150. doi: 10.1038/eye.2013.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee J.E., Kim N.M., Yang J.W., Kim S.J., Lee J.S., Lee J.E. A randomised controlled trial comparing a thermal massager with artificial teardrops for the treatment of dry eye. Br J Ophthalmol. 2014;98(1):46–51. doi: 10.1136/bjophthalmol-2013-303742. [DOI] [PubMed] [Google Scholar]
- 16.Iester M., Orsoni G.J., Gamba G. Improvement of the ocular surface using hypotonic 0.4% hyaluronic acid drops in keratoconjunctivitis sicca. Eye (Lond) 2000;14(Pt 6):892–898. doi: 10.1038/eye.2000.244. [DOI] [PubMed] [Google Scholar]
- 17.Messmer E.M., Bulgen M., Kampik A. Hyperosmolarity of the tear film in dry eye syndrome. Dev Ophthalmol. 2010;45:129–138. doi: 10.1159/000315026. [DOI] [PubMed] [Google Scholar]
- 18.Cömez A.T., Tufan H.A., Kocabıyık O., Gencer B. Effects of lubricating agents with different osmolalities on tear osmolarity and other tear function tests in patients with dry eye. Curr Eye Res. 2013;38(11):1095–1103. doi: 10.3109/02713683.2013.806670. [DOI] [PubMed] [Google Scholar]
- 19.Montani G. Intrasubject tear osmolarity changes with two different types of eyedrops. Optom Vis Sci. 2013;90(4):372–377. doi: 10.1097/OPX.0b013e318288bdbe. [DOI] [PubMed] [Google Scholar]
- 20.Bunya V.Y., Langelier N., Chen S., Pistilli M., Vivino F.B., Massaro-Giordano G. Tear osmolarity in Sjögren syndrome. Cornea. 2013;32(7):922–927. doi: 10.1097/ICO.0b013e31827e2a5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sullivan B.D., Crews L.A., Sönmez B. Clinical utility of objective tests for dry eye disease: variability over time and implications for clinical trials and disease management. Cornea. 2012;31(9):1000–1008. doi: 10.1097/ICO.0b013e318242fd60. [DOI] [PubMed] [Google Scholar]
- 22.Di Tommaso C., Valamanesh F., Miller F. A novel cyclosporin a aqueous formulation for dry eye treatment: in vitro and in vivo evaluation. Invest Ophthalmol Vis Sci. 2012;53(4):2292–2299. doi: 10.1167/iovs.11-8829. [DOI] [PubMed] [Google Scholar]
- 23.Larmo P.S., Järvinen R.L., Setälä N.L. Oral sea buckthorn oil attenuates tear film osmolarity and symptoms in individuals with dry eye. J Nutr. 2010;140(8):1462–1468. doi: 10.3945/jn.109.118901. [DOI] [PubMed] [Google Scholar]
- 24.Khanal S., Tomlinson A., Esakowitz L. Changes in corneal sensitivity and tear physiology after phacoemulsification. Ophthalmic Physiol Opt. 2008;28(2):127–134. doi: 10.1111/j.1475-1313.2008.00539.x. [DOI] [PubMed] [Google Scholar]
- 25.Wei Y., Asbell P.A. The core mechanism of dry eye disease is inflammation. Eye Contact Lens. 2014;40:248–256. doi: 10.1097/ICL.0000000000000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacobi C., Jacobi A., Kruse F.E., Cursiefen C. Tear fil osmolarity measurements in dry eye disease using electrical impedance technology. Cornea. 2011;30(12):1289–1292. doi: 10.1097/ICO.0b013e31821de383. 11. [DOI] [PubMed] [Google Scholar]