Abstract
Objective
To examine the effects of a harm reduction policy, specifically Good Samaritan (GS) policy, on overdose deaths.
Data Sources/Study Setting
Secondary data from multiple cause of death, mortality records paired with state harm reduction and substance use prevention policy.
Study Design
We estimate fixed effects Poisson count models to model the effect of GS policy on overdose deaths for all, prescription, and illicit drugs, controlled substances, and opioids, while controlling for other harm reduction and substance use prevention policies.
Data Collection/Extraction Methods
We merge secondary data sources by state and year between 1999 and 2016.
Principal findings
We fail to identify a statistically significant effect of GS policy in reducing overdose deaths broadly.
Conclusions
While we are unable to identify an effect of GS policy on overdose deaths, GS policy may have important effects on first‐stage outcomes not investigated in this paper. Given recent state policy changes and rapid increase in many categories of overdose deaths, additional research should continue to examine the implementation and effects of harm reduction policy specifically and substance use prevention policy broadly.
Keywords: controlled substance, Good Samaritan, harm reduction, mortality, opioid, overdose, poisoning, policy, substance use
1. INTRODUCTION
Substance use and misuse can result in negative short‐ and long‐run health effects as well as overdose.1 Timely emergency medical response can play a critical role in preventing overdose from ending in death. Those involved in illegal activities, however, may be reluctant to call for emergency response for fear of legal consequences. As the opioid overdose epidemic, underage binge drinking, and other types of prescription and illicit drug use escalate, encouraging contact with law enforcement and emergency medical services (EMS) is an important piece of combatting the consequences of substance misuse. Between 1999 and 2016, the drug overdose death rate (per 100, 000) increased over 200 percent from 5.93 in 1999 to 20.78 in 2016. Drug overdose death rates in 2015 were higher for men than women (20.8 vs 11.8, respectively) and were highest for adults between the ages of 45 and 54 (30.0) and non‐Hispanic whites (21.1).2
In particular, the United States is facing an opioid epidemic, which President Trump called a national public health emergency in October 2017. In 2017, opioids were responsible for almost 70 percent of all drug overdose deaths.3 The opioid overdose death rate per 100,000 was 2.21 in 1999 and rose to 13.78 in 2016, an increase of 500 percent (authors' calculations). Similar to overall overdose deaths, opioid‐related overdose deaths are concentrated among non‐Hispanic whites, individuals aged 25‐54, and men,2, 4, 5 although female opioid overdose death rates are also increasing.6 Other prescription drugs (eg, benzodiazepines) and illicit drugs (eg, cocaine) have also seen large increases in overdose deaths.
Many states have adopted policies aimed at combatting the overdose epidemic. Some regulate access to prescription drugs, such as prescription drug monitoring programs (PDMPs) and pain management clinic policies (PMCs). Additionally, some states have adopted medical marijuana laws (MMLs), which some research has identified to be associated with reduced reliance on prescription painkillers. This set of policies is aimed (directly or indirectly) at preventing substance misuse broadly and prescription drug addiction particularly. Along with these primary and secondary prevention strategies, some states have adopted harm reduction approaches with respect to substance misuse more broadly. Harm reduction strategies acknowledge that alcohol and substance misuse occur but put policies in place that attempt to mitigate the negative consequences associated with such misuse. One example of a harm reduction policy adopted by many states is the Good Samaritan (GS) policy that encourages calls for emergency response in the event of an overdose. Forty (40) states and D.C. have enacted GS policies since 2007. Most of these laws protect the individual reporting the overdose from the consequences of controlled substance possession, while some laws (also) protect the individual from drug paraphernalia charges. All GS laws are designed to increase emergency calls for overdose by providing immunity to those involved. In North Carolina (NC Statute §90‐96.2), for example, the statute provides limited immunity for the person seeking medical assistance on behalf of an individual experiencing a drug overdose when contacting 911, law enforcement, or EMS as well as the overdose victim. Other harm reduction approaches undertaken at the state‐level address opioid overdose specifically through access to naloxone (a medication which can reverse an opioid overdose). Naloxone policies (NA) are aimed at increasing access to this antidote through immunity provisions (layperson and/or prescriber) and/or layperson access (standing orders or third‐party prescribing provisions).
Surprisingly, few studies have investigated the effects of GS policies despite the policy first originating with New Mexico in 2007 and diffusing across the country.7, 8 Our study investigates the effect of GS policy, while accounting for other changes in harm reduction and substance use policies, on overdose deaths for several categories of drugs including all, prescription, and illicit drug poisonings. We then consider more refined measures including controlled substances and opioids specifically. In what follows, we use a difference‐in‐difference approach and a Poisson count model to investigate the effects of GS policies on drug overdose mortality for all, prescription, and illicit drugs as well as controlled substance and opioids specifically. We also conduct several specification and robustness tests to support our identification strategy and results.
2. REVIEW OF EXISTING LITERATURE
There is a large and growing literature on the effects of policies and programs designed to address substance misuse, dependence, and overdose. There is a much smaller population‐based literature evaluating harm reduction policies and Good Samaritan policies in particular. Importantly, there are other bodies of literature evaluating program‐level effects of other harm reduction efforts including naloxone distribution, syringe exchange programs, and safe injection sites. For brevity and most direct relevance, we focus mainly on papers evaluating state‐level policy change that utilize population‐level data.
The recent published and working paper literature has identified different effects of harm reduction policies using a variety of different assumptions and empirical methods and has focused exclusively on opioid overdose mortality. McClellan et al,8 using data from 2002‐2014, find negative effects of both GS and NA policies on opioid overdose mortality, with no effect on non‐medical opioid use. The GS policy effects appear to be driven by effects for blacks, Hispanics, 35‐ to 44‐year‐olds, and 55‐ to 64‐year‐olds. In a recent working paper, Rees et al7 studied the effects of NA and GS policy on opioid overdose deaths between 1999 and 2014 finding a negative effect of NA and no effect of GS on opioid overdose. With respect to population‐level NA‐specific studies, Gertner and Domino9 find NA policies to be associated with increases in naloxone dispensing in Medicaid, mainly driven by state standing order provisions. In a recent working paper, Doleac and Mukherjee10 find that NA policies increase opioid‐related crime and opioid‐related emergency department visits. They also find no overall effect of NA policy on opioid overdose mortality but positive effects in some areas of the United States, which the authors suggest is a possible moral hazard effect of naloxone access. Much of the additional existing literature on naloxone has focused on interventions such as naloxone distribution programs in a single state or local area,11, 12, 13 distribution programs through pharmacies,14 take‐home naloxone programs,15 and naloxone‐on‐release for prisoners.16
Other population‐based evaluations have investigated the effects of primary and secondary prevention efforts on overdose outcomes, such as PDMPs, PMCs, and MMLs. Mixed evidence exists on the effect of PDMPs on opioid overdose deaths.17, 18, 19, 20, 21, 22 PDMPs have been found to reduce opioid prescribing following the online access of PDMPs23, 24 and reduce opioid prescriptions for Medicaid enrollees.25 If the use of medical marijuana is an alternative to prescription medications,26, 27 then such policies could affect opioid use and misuse for pain management. MMLs have been associated with lower opioid overdose mortality, either from MML policies broadly28 or from MML dispensaries specifically.29 MML dispensaries are also associated with a reduction in substance use treatment admissions for pain relievers29 and with reductions in opioid positivity for drivers in fatal crashes.30 Additionally, PMC laws were associated with a reduction in opioid overdose deaths.18
Our study investigates the effects of GS policies on drug overdose deaths using population mortality data between 1999 and 2016, while controlling for other harm reduction and substance use policies. Our approach differs from the existing literature by exploring important categories of misused substances beyond opioids including all, prescription, and illicit drugs as well as controlled substances and opioids specifically. Additionally, we follow CDC guidelines for identifying poisoning deaths and use all available overdose data from mortality records over a longer and more recent time period. We model overdose deaths using a Poisson count model due to the skewness and relatively low incidence of occurrences. In what follows, we find no identifiable effect of GS policy on overdose deaths. GS policy, however, may have important first‐stage effects such as higher volume of emergency response calls or emergency department visits not explored in this paper. We do, however, find evidence that accessible PDMPs reduce the incidence of overdose deaths for some pharmaceutical substances, suggesting the importance of a multifaceted approach in preventing overdose death.
3. DATA
3.1. Policy data
State‐level data on GS policy are drawn from LawAtlas.org31 and supplemented with information from the Network for Public Health Law32 and additional state‐specific statutes. According to these reports, 40 states plus DC have implemented GS overdose prevention policies (35 relevant policies during our data period through 2016). GS laws encourage the contact of emergency personnel for medical assistance by ensuring that those involved will face limited legal consequences. Most GS policies provide immunity for the possession of controlled substances, while other states have added provisions that provide protection for paraphernalia. Figure S1 displays two maps of the United States, in 2010 and in 2016, respectively. In 2010, very few states had GS policies, but by 2016, a majority of the country had passed a GS policy. Details of this policy variation are contained in Table S1.
Additional substance use prevention policies are also included in our empirical specification. First, we control for the presence of a PDMP, defined as when the PDMP was accessible to medical professionals. A PDMP is a database of certain prescribed and dispensed prescriptions by providers and pharmacies with the goals of monitoring prescribing patterns and doctor shopping behaviors to limit prescription drug misuse and diversion. These data were gathered from Yarbrough,33 which were originally gathered from the National Alliance for Model State Drug Laws (NAMSDL) and supplemented with additional state‐specific information. While some states have adopted subsequent regulations to their PDMPs such as mandatory use provisions, these policies are rather recent in our data period and vary with respect to which prescription substances trigger a mandated query of the PDMP and at what time intervals the PDMP must queried. Thus, we capture the initial adoption of an accessible PDMP in the state. Second, we control for PMC regulations or restrictions on pain management or “pill mill” clinics, which are clinics that may be prescribing controlled substances inappropriately or for non‐medical reasons. Regulations of such clinics may involve state oversight and/or rules about ownership and operation. These data were drawn from CDC (2015), Dowell et al (2016), and supplemented with additional state‐specific information.18, 34 Finally, there is recent evidence that MMLs affect the use and misuse of prescription drugs (and opioids in particular).26, 27, 28 We control for MMLs, specifically the presence of a medical marijuana dispensary, which indicates a greater level of access than medical marijuana legalization alone, home cultivation, or patient registries. These data were provided to us by Bradford and Bradford (2016).26, 27
With respect to the opioid epidemic specifically, some states have also adopted harm reduction strategies through policies promoting naloxone access. Use of naloxone can only reverse the effects of an opioid overdose. Forty‐seven (47) states and DC have adopted naloxone (NA) policies aimed at increasing access to the overdose antidote between 2001 and 2016. State‐level policy data on NA are drawn from the same sources as GS policy. NA policies either provide immunity (civil and/or criminal) for prescribers and/or laypersons, increase access to the drug through third‐party prescribing provisions or standing orders, or a combination. Third‐party prescribing allows a prescription to be written and dispensed to one person with the purpose of administering it to another person. Under a standing order, physicians can designate others to distribute naloxone, for example, employees of a harm reduction program, to individuals who would be in a position to administer naloxone in an emergency situation (eg, friends and family), or permit pharmacists to dispense naloxone under the law (eg, similar to other efforts to increase use of emergency contraception or influenza vaccinations). While there are multiple components of NA policy, the majority of these policies were passed simultaneously and many quite recently. As such, in what follows, we model the NA policy variable as any naloxone policy in a subset of models focused on opioid overdose.
3.2. Outcomes data
The outcome variable of interest is the state by year count of overdose deaths from the National Vital Statistics System (NVSS) multiple cause of death files from 1999 to 2016 obtained through CDC WONDER. Per CDC guidance,35 we defined drug overdose deaths as those with an underlying cause of death from drug poisoning that were of any intent (unintentional, intentional, or undetermined) using the International Classification of Disease, 10th revision [ICD‐10] codes X40‐X44 (accidental poisoning), X60‐64 (intentional self‐poisoning), X85 (assault), and Y10‐Y14 (undetermined intent). For these poisoning deaths, we identified deaths using multiple cause of death ICD‐10 codes (which are not mutually exclusive, since polysubstance use is common and deaths can be caused by more than one substance). We first identify deaths for all, pharmaceutical, and illicit drugs (see notes, Table 2). Since GS policies target controlled substance possession, we specifically investigate controlled substances (all and prescription, as illicit and controlled illicit substances are identical; see notes, Table 3).36 Given the current opioid epidemic and contribution of opioids to aggregate rates of drug overdose, we also explored the potential effect of GS policy on opioid overdose specifically. We analyze all opioids (exclusive and inclusive of the category “other and unspecified narcotics,” which includes opioids but also other substances), prescription opioids, and illicit opioids (see notes, Table 4). It is important to note the changing landscape of opioid deaths over this period, and in particular, the rise of fentanyl‐related deaths, a highly potent synthetic prescription opioid used to treat cancer pain which is more recently illegally produced and laced with heroin and other substances. Fentanyl deaths have spiked (increasing more than 80 percent between 2015 and 2016) and are captured in the measures of the any, prescription, and illicit opioid categories.
Table 2.
Poisson regression results: all, illicit, and pharmaceutical drugs, 1999‐2016
| All drugs | Illicit | Pharmaceuticals | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GS | −0.0566 [0.0893] | −0.0578 [0.0913] | −0.0582 [0.0842] | −0.0650 [0.0824] | −0.1238 [0.1398] | −0.1153 [0.1464] | −0.0833 [0.1248] | −0.0901 [0.1160] | −0.0690 [0.1352] | −0.0616 [0.1343] | −0.0613 [0.1243] | −0.0714 [0.1243] |
| PDMP | 0.0059 [0.0404] | 0.0024 [0.0386] | −0.0004 [0.0384] | −0.0471 [0.0736] | −0.0528 [0.0699] | −0.0484 [0.0677] | −0.0359 [0.0402] | −0.0445 [0.0381] | −0.0427 [0.0389] | |||
| PMC | 0.0004 [0.0994] | −0.0154 [0.0910] | 0.1438 [0.1865] | 0.0996 [0.1681] | 0.0170 [0.1365] | −0.0208 [0.1257] | ||||||
| MML | 0.0635 [0.0736] | 0.0533 [0.0686] | 0.0467 [0.0876] | 0.0294 [0.0807] | 0.1481 [0.1401] | 0.1305 [0.1297] | ||||||
| N | 917 | 917 | 917 | 917 | 840 | 840 | 840 | 840 | 912 | 912 | 912 | 912 |
| Covariates | No | No | No | Yes | No | No | No | Yes | No | No | No | Yes |
| State/Year Fixed Effects | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Tables contain Poisson regression coefficients and clustered standard errors in brackets. Deaths derived from CDC WONDER, 1999‐2016, with underlying causes of death (X40‐44; Y10‐14; X85; X60‐64) and multiple cause of death by category of drug. All drugs (T36‐T50); all illicit drugs (T40.1, T40.5, T40.7, T40.8, T40.9, T43.6); all pharmaceutical drugs (T36‐39, T40.2, T40.3, T40.4, T41‐42, T43.1‐43.5, T43.8‐43.9, T44‐49, T50.0‐50.8). Per CDC (2013) guidance, the term “pharmaceutical” is used as opposed to “prescription” because a small number of codes include both prescription and over‐the‐counter drugs. Counts of deaths have a minimum of 10 per CDC WONDER; counts of less than 10 are suppressed and recorded as missing in the data.
GS, Good Samaritan policy; MML, presence of medical marijuana dispensary; PDMP, prescription drug monitoring program; PMC, pain management clinic policy.
*P < 0.10, **P < 0.05, ***P < 0.01.
Table 3.
Poisson regression results: controlled substances, 1999‐2016
| Controlled substances | Controlled prescription substances | |||||||
|---|---|---|---|---|---|---|---|---|
| GS | −0.1196 [0.1165] | −0.1202 [0.1184] | −0.1097 [0.1077] | −0.1181 [0.1040] | −0.0849 [0.1128] | −0.0715 [0.1094] | −0.0740 [0.1056] | −0.0815 [0.1077] |
| PDMP | 0.0031 [0.0487] | 0.0004 [0.0471] | 0.0022 [0.0475] | −0.0652* [0.0381] | −0.0681* [0.0377] | −0.0666* [0.0382] | ||
| PMC | 0.0673 [0.1423] | 0.0420 [0.1285] | −0.0211 [0.1329] | −0.0538 [0.1251] | ||||
| MML | 0.0425 [0.0940] | 0.0318 [0.0873] | 0.0523 [0.1192] | 0.0361 [0.1085] | ||||
| N | 907 | 907 | 907 | 907 | 886 | 886 | 886 | 886 |
| Covariates | No | No | No | Yes | No | No | No | Yes |
| State/Year Fixed Effects | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Tables contain Poisson regression coefficients and clustered standard errors in brackets. Deaths derived from CDC WONDER, 1999‐2016, with underlying causes of death (X40‐44; Y10‐14; X85; X60‐64) and multiple cause of death by category of drug. Controlled substances (T40.0‐T40.9, T42.3‐42.4, T43.6, T41.2; excluded 52.8 as this category is not in Table 2 definitions per CDC guidelines) and controlled prescription substances (T40.2‐40.3, T41.2, T42.3‐42.4; excluded 40.4 and 40.6 as these are not categories which are exclusively prescription). Counts of deaths have a minimum of 10 per CDC WONDER; counts of less than 10 are suppressed and recorded as missing in the data.
GS, Good Samaritan policy; MML, presence of medical marijuana dispensary; PDMP, prescription drug monitoring program; PMC, pain management clinic policy.
*P < 0.10, **P < 0.05, ***P < 0.01.
Table 4.
Poisson regression results: opioids, 1999‐2016
| All opioids—Panel A (prescription and illicit opioids) | All opioids—Panel B (prescription and illicit opioids and other/unspecified narcotics) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| GS | −0.0413 [0.1552] | −0.0335 [0.1554] | −0.0307 [0.1427] | −0.0413 [0.1425] | −0.0689 [0.1485] | −0.1273 [0.1373] | −0.1289 [0.1393] | −0.1102 [0.1268] | −0.1196 [0.1235] | −0.1407 [0.1300] |
| PDMP | −0.0367 [0.0533] | −0.0476 [0.0502] | −0.0453 [0.0512] | −0.0525 [0.0518] | 0.0075 [0.0604] | 0.0024 [0.0589] | 0.0039 [0.0589] | −0.0022 [0.0594] | ||
| PMC | 0.0346 [0.1808] | −0.0030 [0.1651] | 0.0003 [0.1560] | 0.1242 [0.1656] | 0.0965 [0.1503] | 0.1000 [0.1438] | ||||
| MML | 0.1628 [0.1354] | 0.1469 [0.1255] | 0.1598 [0.1246] | 0.0745 [0.1171] | 0.0628 [0.1091] | 0.0730 [0.1071] | ||||
| NA | 0.1295 [0.0935] | 0.0943 [0.0805] | ||||||||
| N | 892 | 892 | 892 | 892 | 892 | 901 | 901 | 901 | 901 | 901 |
| Prescription Opioids—Panel C | Illicit Opioids—Panel D | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| GS | −0.0824 [0.1573] | −0.0753 [0.1563] | −0.0734 [0.1457] | −0.0879 [0.1461] | −0.1201 [0.1529] | 0.0805 [0.1980] | 0.0956 [0.2153] | 0.1537 [0.1712] | 0.1385 [0.1661] | 0.1152 [0.1619] |
| PDMP | −0.0337 [0.0496] | −0.0463 [0.0470] | −0.0413 [0.0475] | −0.0474 [0.0473] | −0.0644 [0.1376] | −0.0860 [0.1323] | −0.0695 [0.1349] | −0.0888 [0.1358] | ||
| PMC | 0.0373 [0.1516] | −0.0185 [0.1397] | −0.0154 [0.1314] | 0.2417 [0.3065] | 0.1616 [0.2702] | 0.1616 [0.2588] | ||||
| MML | 0.2111 [0.1711] | 0.1835 [0.1560] | 0.1964 [0.1534] | 0.1290 [0.1665] | 0.0948 [0.1575] | 0.1144 [0.1643] | ||||
| NA | 0.1475 [0.0980] | 0.1315 [0.0904] | ||||||||
| N | 884 | 884 | 884 | 884 | 884 | 577 | 577 | 577 | 577 | 577 |
| Covariates | No | No | No | Yes | Yes | No | No | No | Yes | Yes |
| State/Year Fixed Effects | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Tables contain Poisson regression coefficients and clustered standard errors in brackets. Deaths derived from CDC WONDER, 1999‐2016, with underlying causes of death (X40‐44; Y10‐14; X85; X60‐64) and multiple cause of death by category of drug. All opioids—Panel A (T40.0‐T40.4); all opioids—Panel B (T40.1‐T40.4, T40.6); prescription opioids—Panel C (T40.2‐T40.4); illicit opioids—Panel D (T40.0‐T40.1). Counts of deaths have a minimum of 10 per CDC WONDER; counts of less than 10 are suppressed and recorded as missing in the data.
GS, Good Samaritan policy; PDMP, prescription drug monitoring program; PMC, pain management clinic policy; MML, presence of a medical marijuana dispensary.
*P < 0.10, **P < 0.05, ***P < 0.01.
In the analysis that follows, we add a set of additional state‐level control variables including the percent of the state population that is African American (US Census), median household income (in thousands of $2016, US Census), and state unemployment rate (Bureau of Labor Statistics). The mortality data are available from 1999 to 2016. Summary statistics are provided in Table 1. Our dataset consists of 917 possible state‐year observations (we exclude New Jersey in 2009 per CDC guidance due to measurement issues during our data period). Over our sample period, the average drug overdose rate per 100 000 for all drugs poisonings was 12.10. Figure 1A,B show the trends in overdose death rates for our main outcome measures and for opioid measures specifically between 1999 and 2016. Figure 1A shows the rate of all drug overdose deaths rising, with large observed increases for opioids. Figure 1B shows a similar pattern, with large observed increases for controlled substance and opioid subcategories.
Table 1.
Descriptive Statistics, 1999‐2016
| Mean | Std. deviation | Min | Max | |
|---|---|---|---|---|
| All overdose deaths—count | 688.6 | 777.1 | 12 | 4728 |
| All overdose deaths—rate | 12.11 | 5.91 | 1.8 | 48.30 |
| Illicit overdose deaths—count | 234.1 | 304.1 | 10 | 2351 |
| Illicit overdose deaths—rate | 4.01 | 2.92 | 0.4 | 26 |
| Pharmaceutical overdose deaths—count | 366.6 | 421.3 | 10 | 3238 |
| Pharmaceutical overdose deaths—rate | 7.08 | 4.93 | 0.8 | 40.50 |
| Controlled substances overdose deaths—count | 480.2 | 552.5 | 10 | 3965 |
| Controlled substances deaths—rate | 8.76 | 5.55 | 0.8 | 45.20 |
| Prescription controlled substances overdose deaths—count | 349.0 | 391.0 | 10 | 3160 |
| Prescription controlled substances deaths— rate | 6.7 | 4.68 | 0.7 | 39 |
| All opioid deaths—count | 350 | 419.1 | 10 | 3493 |
| All opioid deaths—rate | 6.59 | 5.02 | 0.4 | 39.80 |
| All opioid deaths and other/unspecified narcotics—count | 390.1 | 443.8 | 10 | 3613 |
| All opioid deaths and other/unspecified narcotics—rate | 7.29 | 25.4 | 0.6 | 40 |
| Prescription opioid overdose deaths—count | 281.4 | 333.2 | 10 | 2875 |
| Prescription opioid deaths—rate | 5.49 | 4.33 | 0.4 | 35 |
| Illicit opioid overdose deaths—count | 144.9 | 193.0 | 10 | 1478 |
| Illicit opioid deaths—rate | 2.37 | 2.31 | 0.1 | 17.90 |
| Good Samaritan policy | 0.12 | 0.31 | 0 | 1 |
| Accessible PDMP | 0.39 | 0.48 | 0 | 1 |
| Pain management clinic policy | 0.065 | 0.24 | 0 | 1 |
| Medical marijuana dispensary | 0.10 | 0.29 | 0 | 1 |
| Naloxone policy | 0.16 | 0.35 | 0 | 1 |
| Median household income ($1,000s) | 56.61 | 8.71 | 36.0 | 81.02 |
| Percent black | 11.90 | 11.34 | 0.35 | 62.09 |
| Unemployment rate | 5.71 | 1.98 | 2.30 | 13.70 |
| Observations | 917 |
Deaths derived from CDC WONDER, 1999‐2016, with underlying causes of death (X40‐44; Y10‐14; X85, X60‐64). N = 917 is the max number of observations, but in some cases, data are missing on some outcomes (we exclude New Jersey in 2009 per CDC guidance). Rates represent number of deaths per 100 000. Median household income in $2016 (thousands).
PDMP, prescription drug monitoring program.
Figure 1.
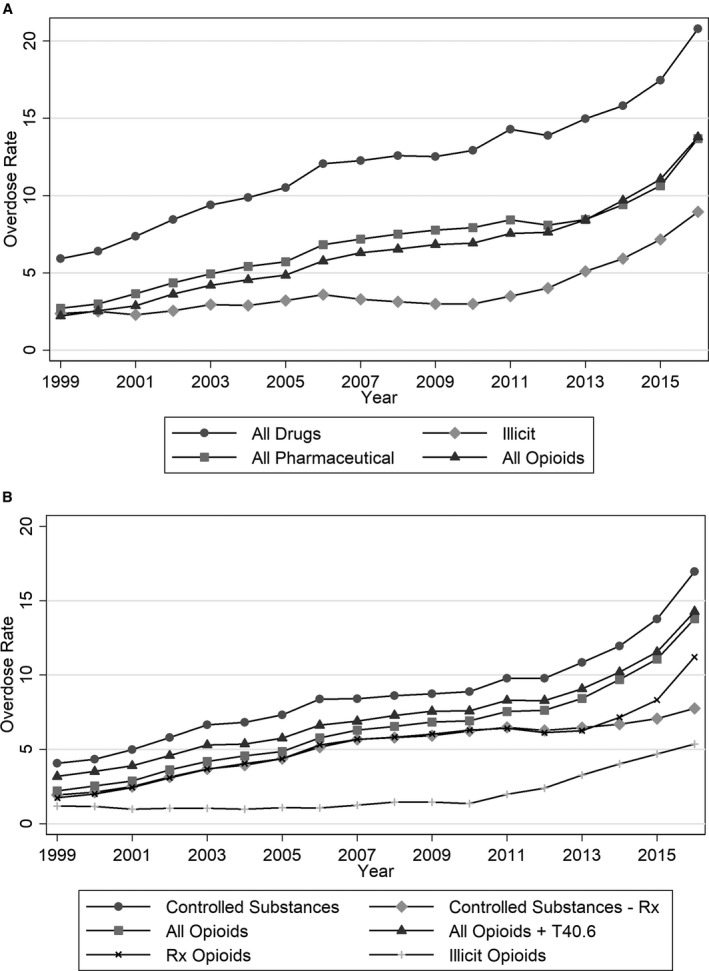
- Notes: Overdose death rates calculated per 100 000 population and derived from CDC WONDER, 1999‐2016, with underlying causes of death (X40‐44; Y10‐14; X85, X60‐64) and multiple cause of death ICD‐10 codes (all drugs (T36‐T50); all illicit drugs (T40.1, T40.5, T40.7, T40.8, T40.9, T43.6); all pharmaceutical drugs (T36‐39, T40.2, T40.3, T40.4, T41‐42, T43.1‐43.5, T43.8‐43.9, T44‐49, T50.0‐50.8); controlled substances (T40.0‐T40.9, T42.3‐42.4, T43.6, T41.2; excluded 52.8 as this category is not in Table 2 definitions per CDC guidelines) and controlled prescription (Rx) substances (T40.2‐40.3, T41.2, T42.3‐42.4; excluded 40.4 and 40.6 as these are not categories which are exclusively prescription); all opioids (T40.0, T40.1, T40.2, T40.3, T40.4); all opioids + other/unspecified narcotics (T40.0, T40.1, T40.2, T40.3, T40.4, T40.6); prescription (Rx) opioids (T40.2‐40.4); illicit opioids (T40.0‐40.1).
4. EMPIRICAL STRATEGY
In this study, we employ a difference‐in‐difference (DD) approach to estimate the effect of state‐level GS laws on drug overdose mortality, while controlling for other potentially important harm reduction and substance use prevention policies. DD estimation involves identifying sets of states with and without GS policy changes and the timing of those changes. We then compare the difference in overdose deaths before and after the policy change in states with the policy change to states without the policy change. Because of the relatively low incidence of overdose deaths and skewness of overdose death counts, our model specification is characterized by using a Poisson count data model:
| (1) |
where Y st is the state (s) overdose death count in year t and the state/year population is the exposure variable (which allows the incidence of overdose to be relative to the state/year population). GS is an indicator (full or partial year) for the presence of any GS policy, and OtherPolicy is a vector with indicators for the presence of PDMP, PMC laws, and the presence of a MML dispensary. For opioid outcomes, we also include any naloxone (NA) policy. X st represents state‐level control variables previously described. The model also includes state fixed effects (Өs), year fixed effects (π t), and standard errors clustered at the state level. Table S2 contains results from event studies that support our identification strategy and pretreatment trend assumption.
5. EMPIRICAL FINDINGS
Our empirical results are presented in Tables 2, 3, 4. Table 2 displays the fixed effects Poisson coefficients for poisoning deaths of all intent involving all, pharmaceutical, and illicit drugs. We fail to identify a statistically significant effect of GS on deaths for each outcome. The categories of all drugs and all pharmaceutical drugs are broad, and some of these may not be drugs that are commonly misused or overdosed. Additionally, most GS policies are aimed at encouraging calls for emergency response by mitigating the legal consequences from controlled substance possession specifically. As such, we consider controlled substances in Table 3.36 If GS policy has an identifiable effect on overdose mortality, it would likely be on substances that are being used in violation of the law. GS policy remains statistically insignificant. We find some support for accessible PDMPs in reducing overdose for prescription controlled substances by approximately 6 percent. Importantly, this suggests that the effect of PDMPs in reducing pharmaceutical overdose deaths may not be solely due to restrictions in opioid access.
Given the importance of the opioid epidemic in the rise of drug overdose rates, we further consider the effects of GS policy by analyzing opioids specifically in Table 4. Here, we examine all opioids (inclusive and exclusive of other and unspecified narcotics, T40.6), prescription opioids, and illicit opioids. We acknowledge that these measures are not mutually exclusive and moreover that there are concerns about reporting differences across states and over time regarding the specificity of the substances involved in a death.18, 37, 38 As such, we prefer the results for all opioids, as this measure is less affected by differences in reporting or changes in reporting over time. We also tested the results to the inclusion of the category of “unspecified drugs” (T50.9)38 and found similar results. In Table 4, GS policy is not statistically significantly associated with any opioid overdose measure.
We test these findings in several different ways and compare to our fully adjusted models above. First, GS policy may have a greater effect on unintentional drug overdose. There are some concerns, however, about the coding of intent in the mortality data over time and across states.39 Regardless, as a test, we consider Equation (1) for unintentional drug overdose deaths as our outcome measures. The results of this exercise are comparable to the results shown in Tables 2, 3, 4. Second, we also lagged GS policy to allow for the possibility of a delayed effect, given knowledge by either citizens or law enforcement, and we continue to find a statistically insignificant relationship between GS policy and overdose mortality. We also explored replacing the missing overdose counts with different values in the Poisson regressions. We continue to find a statistically insignificant relationship between GS and overdose, and the coefficients are of similar magnitudes as the results presented in Tables 2, 3, 4. We also estimated OLS regressions on the natural logarithm of overdose rates (which are suppressed below death counts of 20) and continued to find no effect of GS laws on overdose deaths. Finally, we explored the interaction between GS and NA policy and found that the interaction was not statistically significant in the opioid models.
6. DISCUSSION AND LIMITATIONS
Our study has several limitations, some of which could be the subject of future research. First, using data at the state level necessarily masks any local level differences (county; urban/rural) which could be important. Second, substance‐specific overdose deaths may be underreported as a result of coding differences across and within states as well as over time, making policy evaluation more difficult. Ruhm38 highlights the undercounting of opioid overdose deaths due to inconsistencies and changes in coding practices over time. Third, many state‐level harm reduction policies were enacted at the same time and very recently, making respective policy effects difficult to estimate.
The prior literature has found mixed effects of harm reduction policy on opioid overdose mortality. In our analysis, we consider overdose deaths broadly and are unable to identify a statistically significant effect of GS policy. Overdose death is one substance misuse outcome; there are many others. Even though we do not identify a statistically significant effect of GS on overdose deaths, GS policies play an important harm reduction role and may have an identifiable effect on first‐stage outcomes (eg, 911 calls) or other less severe, policy‐relevant outcomes (eg, emergency department visits) which are not examined in this study. Analysis of overdose deaths by substance and intent is, of course, limited by the coding of such information on death certificates. The lack of finding could be a result of several factors related to policy implementation and does not imply that GS policies are not important or potentially effective policies. First, the effectiveness of GS on overdose death is a function of a number of factors such as how quickly emergency response is called, the response time of emergency medical services, and the life‐saving medications that emergency responders carry. For example, not all law enforcement departments have been trained to administer or carry naloxone. Second, awareness of GS policy could be incomplete. Third and related, the success of GS policy is related to trust in police and the law.
In the opioid outcome models, we also controlled for another harm reduction policy, naloxone access laws. Naloxone is an opioid overdose antidote. Unlike some of the existing literature, we did not find an identifiable effect of policies increasing access to naloxone on opioid overdose mortality. Like GS policy, there may be several reasons for this lack of finding. Most naloxone policies are very recent, and it may take more time for naloxone policy to have a strong impact and be evident in population‐level mortality data. Naloxone access laws aim to increase access to naloxone but do not ensure naloxone is available, affordable, purchased, on‐hand, or effectively used. Additionally, these policies do not capture increased EMS or law enforcement access and/or administration.
Finally, our results show a negative effect of PDMP access on prescription controlled substances. These results suggest that PDMPs may protect against overdose for prescription drugs generally monitored by a PDMP (eg, opioids, benzodiazepines, and sedatives) and emphasize the role that primary and secondary prevention policies can play in reducing fatal drug overdose. Policies affecting access to prescription controlled substances, such as PDMPs (when used appropriately by physicians), may limit diversion or reduce substance use initially and result in fewer individuals who ever misuse such drugs and later suffer a fatal overdose. Although, these same policies have the potential to restrict access to medication for those with chronic pain and/or lead to substitution with illicit substances. We note that more recent PDMP efforts include mandatory provider registration and mandatory provider review, which can be further explored by future research.
Much of the existing state‐level policy is aimed at primary or secondary prevention of prescription drug misuse. This study examines the effect of the GS harm reduction policy on drug overdose mortality. Considering that the success of GS policy is dependent on a number of other coinciding factors, a complete evaluation of this policy will need to consider many of the first‐stage effects outlined above. Ultimately, combatting the overdose crisis will require policy action on multiple fronts.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: We received no additional financial support for this project other than the financial support from our respective institutions (Atkins and Durrance). We have no conflicts of interest to report. Key personnel include Danielle N. Atkins, Christine Piette Durrance, and Yuna Kim. The project was designed by Atkins, Durrance, and Kim. Most of the data collection and analysis was conducted by Atkins and Durrance. Drafting and revisions of the paper were done by Atkins, Durrance, and Kim.
Disclosures: None.
Atkins DN, Durrance CP, Kim Y. Good Samaritan harm reduction policy and drug overdose deaths. Health Serv Res. 2019;54:407–416. 10.1111/1475-6773.13119
The views reflected in this paper do not reflect the views or opinions of Toronto Employment and Social Services or of the City of Toronto.
REFERENCES
- 1. National Institute on Drug Abuse . Health consequences of drug misuse. 2017. https://www.drugabuse.gov/related-topics/health-consequences-drug-misuse. Accessed February 1, 2017.
- 2. Hedegaard H, Warner M, Miniño AM. Drug overdose deaths in the United States, 1999–2015. NCHS data brief, no 273. Hyattsville, MD: National Center for Health Statistics; 2017. [Google Scholar]
- 3. Centers for Disease Control and Prevention . Drug overdose deaths. https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed January 28, 2019.
- 4. Kolata G. Death rates rising for middle‐aged White Americans, Study Finds. New York Times. 2015.
- 5. Case A, Deaton A. Rising morbidity and mortality in midlife among white non‐Hispanic Americans in the 21st century. Proc Natl Acad Sci USA. 2015;112(49):15078‐15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Astone NM, Martin S, Aron L. Death rates for US Women Ages 15‐54, some unexpected trends, social determinants of health. 2015:1‐12.
- 7. Rees DI, Sabia JJ, Argys LM, Latshaw J, Dave D. With a little help from my friends: the effects of naloxone access and Good Samaritan policies on opioid‐related deaths. NBER Working Paper #23171. 2017;1‐41.
- 8. McClellan C, Lambdin BH, Ali MM, et al. Opioid‐overdose laws association with opioid use and overdose mortality. Addict Behav. 2018;86:90‐95. [DOI] [PubMed] [Google Scholar]
- 9. Gertner AK, Domino ME. Do naloxone access laws increase outpatient naloxone prescriptions? Evidence from Medicaid. Drug Alcohol Depend. 2018;190:37‐41. [DOI] [PubMed] [Google Scholar]
- 10. Doleac JL, Mukherjee A. The moral hazard of lifesaving innovations: naloxone access, opioid abuse, and crime. SSRN Working Paper. 2018. https://ssrn.com/abstract=3135264 or 10.2139/ssrn.3135264. [DOI] [Google Scholar]
- 11. Doe‐Simkins M, Quinn E, Xuan Z, et al. Overdose rescues by trained and untrained participants and change in opioid use among substance‐using participants in overdose education and naloxone distribution programs: a retrospective cohort study. BMC Public Health. 2014;14(297):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Piper TM, Stancliff S, Rudenstine S, et al. Evaluation of a naloxone distribution and administration program in New York State. Subst Use Misuse. 2008;43(7):858‐870. [DOI] [PubMed] [Google Scholar]
- 13. Walley AY, Xuan Z, Quinn E, Sorenson‐Alawad A, Ozonoff A. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bachyrycz A, Shrestha S, Bleske BE, Tinker D, Bakhireva LN. Opioid overdose prevention through pharmacy‐based naloxone prescription program: innovations in health care delivery. Subst Abus. 2017;38(1):55‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dettmer K, Saunders B, Strang J. Take home naloxone and the prevention of deaths from opiate overdose: two pilot schemes. BMJ. 2001;322(7291):895‐896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Parmar MKB, Strang J, Choo L, Meade AM, Bird SM. Randomized controlled pilot trial of naloxone‐on‐release to prevent post‐prison opioid overdose deaths. Addiction. 2017;112(3):502‐515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paulozzi LJ, Kilbourne EM, Deasi HA. prescription drug monitoring programs and death rates from drug overdose. Pain Med. 2011;2011(12):747‐754. [DOI] [PubMed] [Google Scholar]
- 18. Dowell D, Zhang K, Noonan R, Hockenberry J. Mandatory provider review and pain management clinics reduce the amounts of opioids prescribed and overdose death rates. Health Aff. 2016;35(1):1876‐1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pardo B. Do more robust prescription drug monitoring programs reduce prescription drug opioid overdose? Addiction. 2016;112(10):1773‐1783. [DOI] [PubMed] [Google Scholar]
- 20. Patrick SW, Fry CE, Jones TF, Buntin MB. Implementation of prescription drug monitoring programs associated with reductions in opioid‐related death rates. Health Aff. 2016;35(7):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mallat J. The effect of prescription drug monitoring programs on opioid prescriptions and heroin crime rates. 2017. Working paper. https://www.krannert.purdue.edu/programs/phd/working-papers-series/2017/1292-Justine-Mallatt-Prescription-Drug-Monitoring.pdf.
- 22. Grecu AM, Dave DM, Saffer H. Mandatory access prescription drug monitoring programs and prescription drug abuse. Journal of Policy Analysis and Management. 2019;38(1):181‐209. [PubMed] [Google Scholar]
- 23. Bao Y, Pan Y, Taylor A, et al. Prescription drug monitoring programs are associated with sustained reductions in opioid prescribing by physicians. Health Aff. 2016;35(6):1045‐1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pauly NJ, Slavova S, Delcher C, Freeman PR, Talbert J. Features of prescription drug monitoring programs associated with reduced rates of prescription opioid‐related poisonings. Drug Alcohol Depend. 2018;2018(184):26‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wen H, Schackman BR, Aden B, Bao Y. States with prescription drug monitoring mandates saw a reduction in opioids prescribed to Medicaid enrollees. Health Aff. 2017;36(4):733‐741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bradford WD, Bradford AC. Medical marijuana laws reduce prescription medication use in Medicare Part D. Health Aff. 2016;35(7):1230‐1236. [DOI] [PubMed] [Google Scholar]
- 27. Bradford WD, Bradford AC. Medical Marijuana laws may be associated with a decline in the number of prescriptions for Medicaid enrollees. Health Aff. 2017;36(5):945‐951. [DOI] [PubMed] [Google Scholar]
- 28. Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical Cannabis laws and opioid analgesic overdose mortality in the United States, 1990‐2010. JAMA Intern Med. 2014;174(10):1668‐1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Powell D, Pacula RL, Jacobson M. Do medical marijuana laws reduce addictions and deaths related to pain killers? RAND BING Center for Health Economics Working Paper 1130. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kim JH, Santaella‐Tenorio J, Mauro C, et al. State Medical Marijuana laws and the prevalence of opioids detected among fatally injured drivers. Am J Public Health. 2016;106(11):2032‐2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. LawAtlas.org . Naloxone Overdose Prevention Laws Map. http://lawatlas.org/query?dataset=laws-regulating-administration-of-naloxone. Accessed June 1, 2016.
- 32. Network for Public Health Law . Legal interventions to reduce overdose mortality: naloxone access and overdose Good Samaritan Laws. https://www.networkforphl.org/_asset/qz5pvn/network-naloxone-10-4.pdf. Accessed April 3, 2017.
- 33. Yarbrough CR. Prescription drug monitoring programs produce a limited impact on painkiller prescribing in Medicare Part D. Health Serv Res. 2018;53(2):671‐689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Centers for Disease Control and Prevention . Menu of Pain Management Clinic Regulation. 2012. https://www.cdc.gov/phlp/docs/menu-pmcr.pdf. Accessed March 30, 2017.
- 35. Centers for Disease Control and Prevention . Prescription Drug Overdose Data & Statistics, Guide to ICD‐9‐CM and ICD‐10 Codes Related to Poisoning and Pain. 2013. https://www.cdc.gov/drugoverdose/pdf/pdo_guide_to_icd-9-cm_and_icd-10_codes-a.pdf. Accessed March 12, 2016.
- 36. Dasgupta N, Proescholdbell S, Sanford C, et al. Defining controlled substances overdose: should deaths from substance use disorders and pharmaceutical adverse events by included? J Clin Toxicol. 2013;3(3):1‐8. [Google Scholar]
- 37. Slavova S, O'Brien DB, Creppage K, et al. Drug overdose deaths: let's get specific. Public Health Rep. 2015;130:339‐342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ruhm C. Geographic variation in opioid and heroin involved drug poisoning mortality rates. Am J Prevent Med. 2017;53(6):745‐753. [DOI] [PubMed] [Google Scholar]
- 39. Warner M, Trinidad JP, Bastian BA, Miniño AM, Hedegaard H. Drugs most frequently involved in drug overdose deaths: United States, 2010‐2014. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2016;65(10):1‐15. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


