Abstract
Objective
To determine the impact of the inclusion of pediatric dental care in the Affordable Care Act's (ACA) core package of essential health benefits on dental coverage and utilization.
Data Sources
Children aged 1‐18 years included in the nationally representative 2010‐2015 National Health Interview Survey (NHIS).
Study Design
We used regression‐adjusted difference‐in‐differences to examine changes in rates of dental coverage and visits pre‐ and post‐ACA for children likely to be affected by the ACA (have a parent working for a small employer) to a comparison group of children who were unlikely to be affected (have a parent in a firm with ≥50 employees). Models adjusted for relevant health and sociodemographic measures.
Data Collection
NHIS is an annual household survey conducted by the National Center for Health Statistics.
Principal Findings
Comparing pre‐ and post‐ACA periods, private dental insurance increased by 4.6 percentage points more (P = 0.013) and annual dental visits were unchanged (2.7 percentage points, P = 0.071) among children likely to be affected by the ACA compared to children unlikely to be affected by the ACA.
Conclusion
Inclusion of pediatric dental care as an ACA essential health benefit increased dental insurance coverage, but not dental visits among children likely to be affected by this policy.
Keywords: affordable care act, dental care, dental insurance
1. INTRODUCTION
Beginning in 2014, the Affordable Care Act (ACA) required most insurers to cover a package of health care services, known as essential health benefits (EHB). The ten categories of health care services listed in the EHB package include pediatric services, with pediatric dental care explicitly identified as a covered service. Thus, pediatric dental insurance coverage is available for purchase on all state‐based insurance marketplaces and the federally facilitated marketplace. Moreover, the dental coverage offered in all states covered a minimum set of benefits to ensure children have coverage for essential dental services. Dental benefit packages offered in states were comparable to the Federal Employee Dental and Vision Insurance Program in 25 states and the State Children's Health Insurance Program (CHIP) in 24 states.1 Thus, the inclusion of pediatric dental care as one component of the EHB package may make dental coverage easier for families to purchase for their children and, because studies have suggested associations between private dental insurance and dental visits for children,2, 3 has the potential to increase dental visits and potentially improve children's oral health.
The ACA allows insurance marketplaces flexibility in how benefits for pediatric dental care are offered. Marketplaces offer pediatric dental coverage through stand‐alone dental plans and through health plans with an embedded pediatric dental care benefit. This means that most families using the marketplaces have the option to purchase pediatric dental coverage. During the 2016 plan year, stand‐alone dental plans were selected for more than 100 000 children through the federally facilitated marketplace.4 When examining children in both the federally facilitated marketplace and the state‐based marketplaces during the 2017 plan year, stand‐alone dental plans were selected for more than 172 000 children, representing 16.7 percent of children obtaining coverage on these insurance marketplaces.5 The U.S. Department of Health and Human Services does not track the number of children obtaining coverage on the federally facilitated marketplace with embedded dental benefits.
For families obtaining health insurance outside of the marketplaces, health insurance plans must cover the EHB package, including pediatric dental care, unless the carrier can be “reasonably assured” that coverage for pediatric dental care was obtained elsewhere. States vary in how they define “reasonably assured,” with most states simply requiring health insurance plans to disclose if the plan covers or does not cover pediatric dental care.1
Because most families obtaining health insurance on and off the marketplaces have the option of whether to purchase pediatric dental coverage, is uncertain how the inclusion of pediatric dental care in the ACA's EHB package will affect rates of dental coverage and dental visits for children. While there is evidence that the ACA's policy extending parents’ health insurance to young adults increased dental coverage for young adults,6, 7 to our knowledge, ours is the first study to examine whether the ACA's EHB package increased dental insurance coverage and dental visits for children, a population with high unmet dental needs.8 In this study, we used national survey data to first examine children's rates of private dental insurance and dental visits, both before and after the ACA, in a group likely to be affected by the ACA's EHB package compared to a group of privately insured children unlikely to be affected by the ACA's EHB package. Second, using a regression‐adjusted difference‐in‐differences model, we tested the hypothesis that the ACA increased children's dental insurance coverage and dental visits.
2. METHODS
We used final data files for the 2010‐2015 NHIS, an annual household survey conducted by the Centers for Disease Control and Prevention's National Center for Health Statistics, which provides quarterly estimates of insurance status and utilization of dental care among other relevant measures of socioeconomic status, health, and utilization. Our treatment and comparison groups were constructed using a combination of the NHIS sample child file and sample adult file.
We estimated difference‐in‐differences multivariable linear probability regression models to compare outcomes before (2011‐2013) and after (2014‐2015) the implementation of the ACA's EHB package on January 1, 2014, for a group of children likely to be affected by this ACA policy (EHB group, hereafter referred to as treatment group) and a group of children unlikely to be affected by this policy (no EHB group, hereafter referred to as comparison group). For this analysis of six years of cross‐sectional data, each observation represented a unique child, i, in a given year, t, thus the unit of analysis was the child‐year. In the regression framework, let
where Y it represents an indicator of private dental coverage in the first model and receipt of a dental visit in the past 12 months in the second model for child i at time t; and EHBi is an indicator that identifies the “treatment” group (EHB = 1, 0 otherwise). Since 2014, all nongrandfathered plans in the nongroup (ie, individual) and small‐group markets, whether offered inside or outside of the marketplaces, were required to offer the EHB package, including pediatric dental care.9 Therefore, the EHB group included children with direct purchase individual insurance plans or a parent working in a firm with fewer than 50 employees, the firm size eligible to purchase coverage for their employees through the Small Business Health Options Program (SHOP) insurance marketplaces. These children were likely to be affected by the EHB regardless of whether they actually enrolled in plans required to offer the EHB because, to our knowledge, no data source provides detailed individual information about type of health plan, dental insurance, and dental visits.
The comparison group (no EHB) included children with a parent working in a firm with 50 or more employees because large employers offering health insurance were not required to cover the EHB package. Employment information for parents, including firm size, was collected in the NHIS sample adult file for a sample adult in each household. We linked children to parents using the parent linkage identifier and only included dyads where (a) a parent was the sample adult and (b) insurance status, source of insurance, and details about the parent's employment status and employer size were available.
Postt is equal to one if the ACA policy was in effect at time t, and zero, otherwise. We define t t as a vector of year‐quarter dummy variables, X is a vector of explanatory variables described below and εit represents the error term.
We used the person file to determine whether children had private dental benefits coverage at the time of the survey. The NHIS asks all respondents if they have a private insurance plan that pays “for any of the costs for dental care.” We constructed a dichotomous variable at the child‐level identifying children with responses of “yes” a plan pays for any of the costs for dental care (reference group = no plan that covers the costs for dental care). This variable is used to monitor the Healthy People 2020 objective of increasing the percent of persons with dental insurance.10 We used the sample child file to determine when children last visited a dentist. We combined two response categories regarding timing of the last dental visits (fewer than 6 months and between 6 and 12 months) to construct a dichotomous variable at the child‐level identifying children having had at least one dental visit that occurred in the last 12 months (reference group=never or more than 1 year). Additional variables from the person file included a measure of age in years, gender, race (white, black, and other), indicator of Hispanic ethnicity, a continuous measure of family size, and dichotomous indicators of rural location and family income less than 300 percent of the Federal Poverty Level (FPL). We used a three‐level variable for physical health (excellent, very good, and good or worse health), and two dichotomous variables to indicate having a well visit in the last year and to indicate a limitation of activity.
Table 1 describes the selection criteria for the analytic sample. The NHIS sample child questionnaire included 44 801 respondents aged 1‐18 years without public insurance coverage. We excluded children with public insurance because Medicaid and CHIP provide pediatric dental benefits. Because the sample adult questionnaire provided important information about parental employment, we dropped 13 532 children in households that did not have a parent complete the sample adult questionnaire. We dropped children that did not meet criteria for inclusion in our EHB or no EHB groups (N = 11 725) and children with missing information on family income (N = 1491). We dropped 1649 observations in the first two quarters of 2014 because open enrollment on the marketplaces ran from October 1, 2013 to March 31, 2014 and because there is likely to be a lagged effect on dental visits due to the biannual dental visit periodicity schedule.
Table 1.
Identification of analytic sample
|
EHB, essential health benefits.
We obtained additional data from the Area Health Resources File (AHRF) and the Kaiser Family Foundation to adjust for relevant state and county‐level characteristics. State and county are restricted variables that were accessed through the Research Data Center. From the AHRF, we obtained the annual county‐level number of dentists per 10 000 child population. From Kaiser Family Foundation, for each state, we obtained a quarterly indicator of state Medicaid expansion and the annual CHIP eligibility upper‐income limit.
Sampling weights were used to generate means accounting for the fact that each observation in the NHIS represents a number of subjects in the population. Sampling weights were constructed by summing individual person‐level weights within each year across all years and dividing by the number of years of data, the approach recommended by the National Center for Health Statistics.11 We reported weighted, unadjusted annual percentages of children with dental coverage and dental visits. To compare differences in annual rates of the dependent variables by year within the pre‐ACA period, we estimated weighted linear probability regression models separately for the EHB and no EHB groups, including only dummy variables for survey year, and examined differences using Wald tests. To compare differences in rates of the dependent variables pre‐ and post‐ACA, we estimated similar models adjusting only for an indicator of pre/post‐ACA and examined differences in rates of the dependent variables using t tests.
We estimated weighted linear probability regression models to obtain direct estimates of absolute changes in the probability of having dental coverage or having a dental visit in the last year for a child.12 To ensure our results were not sensitive to our choice of a linear model, we also estimated logistic regression models using the same unit of analysis and our results did not change in substantive or statistical significance (results available upon request). These models included state fixed effects, adjusted for relevant health and sociodemographic measures, were estimated with sampling weights, and included cluster‐robust standard errors at the state level to correct for potentially problematic serial correlation within states.13 We conducted all analyses using the statistical software Stata, version 13 (College Station, TX, USA: StataCorp LP).
3. RESULTS
Table 2 presents unadjusted characteristics of the 16 404 children in our sample for the pre‐ACA and post‐ACA periods and the EHB (treatment) and no EHB (comparison) groups. In both the pre‐ and postperiods, children likely to be impacted by the ACA's EHB package were more likely to be Hispanic and live in families with incomes below 300 percent FPL compared to children in the no EHB group.
Table 2.
Characteristics of children in sample, NHIS 2010‐2015
| Pre‐ACA period (2010‐2013) | Post‐ACA period (2014‐2015) | |||||
|---|---|---|---|---|---|---|
| No EHB Group (N = 6661) | EHB Group (N = 5372) | P‐value comparing groups in preperiod | No EHB Group (N = 2445) | EHB Group (N = 1926) | P‐value comparing groups in post period | |
| % or Mean | % or Mean | % or Mean | % or Mean | |||
| Had dental coverage | 40.71% | 27.64% | 0.000 | 41.28% | 32.13% | 0.000 |
| Dental visit in last 12 months | 79.13% | 73.60% | 0.000 | 80.48% | 80.02% | 0.767 |
| Age in years | 9.22772 | 9.22159 | 0.953 | 8.95148 | 9.6549 | 0.000 |
| Male | 52.14% | 50.98% | 0.316 | 50.31% | 47.98% | 0.244 |
| Family size | 4.12 | 4.13 | 0.60 | 4.03 | 4.20 | 0.002 |
| Race | ||||||
| Black | 11.42% | 7.53% | 0.000 | 10.98% | 7.08% | 0.000 |
| White | 77.01% | 82.89% | 0.000 | 78.70% | 82.51% | 0.012 |
| Other | 11.56% | 9.58% | 0.002 | 10.31% | 10.40% | 0.937 |
| Hispanic | 14.81% | 19.32% | 0.000 | 14.79% | 17.64% | 0.025 |
| Health status | ||||||
| Excellent health | 62.13% | 61.08% | 0.340 | 66.43% | 67.42% | 0.599 |
| Very good health | 26.77% | 26.00% | 0.451 | 25.14% | 22.54% | 0.121 |
| Good health or worse | 11.09% | 12.92% | 0.013 | 8.44% | 10.04% | 0.125 |
| Well medical visit in past 12 months | 80.18% | 75.33% | 0.000 | 85.57% | 80.16% | 0.000 |
| Limitation of activity | 7.32% | 6.84% | 0.430 | 7.77% | 7.46% | 0.798 |
| Family income <300% FPL | 38.30% | 50.48% | 0.000 | 34.82% | 44.01% | 0.000 |
| Urban | 81.71% | 76.48% | 0.000 | 81.25% | 78.15% | 0.097 |
| CHIP eligibility upper‐income limit | 249 | 242 | 0.000 | 265 | 257 | 0.001 |
| Dentists per 10 000 child population | 23.59 | 22.85 | 0.005 | 25.37 | 25.14 | 0.642 |
| State expanded Medicaid | 37.53% | 41.46% | 0.001 | 97.21% | 97.32% | 0.900 |
ACA, Affordable Care Act; CHIP, Children's Health Insurance Program; EHB, essential health benefits; FPL, federal poverty level; NHIS, National Health Interview Survey.
Figure 1 presents the weighted, unadjusted annual percentages of children with any private dental insurance coverage for the EHB and no EHB groups. Annual mean rates of dental coverage were not significantly different for the EHB group in the pre‐ACA period (P = 0.945), ranging from 27.0 percent (95 percent confidence interval [CI] = 23.9 percent, 30.0 percent) in 2010 to 28.4 percent in 2013 (95 percent CI = 24.9 percent, 31.5 percent). Rates were significantly higher in the post‐ACA period (30.6 percent, 95 percent CI = 28.3 percent, 32.9 percent) than the pre‐ACA period (27.7 percent, 95 percent CI = 26.1 percent, 29.3 percent) for the EHB group (P = 0.035), with the highest rate of 32.7 percent observed in 2015 (95 percent CI = 29.2 percent, 36.2 percent). In the no EHB group, annual mean rates of dental coverage were not significantly different in the pre‐ACA period (P = 0.266), ranging from 38.8 percent (95 percent CI = 35.6 percent, 41.7 percent) in 2010 to 43.1 percent (95 percent CI = 39.8 percent, 46.2 percent) in 2013. Rates in the pre‐ACA period (41.0 percent, 95 percent CI = 39.5 percent, 42.6 percent) were not significantly different from rates in the post‐ACA period (41.8 percent, 95 percent CI = 39.6 percent, 44.1 percent) for the no EHB group (P = 0.506).
Figure 1.
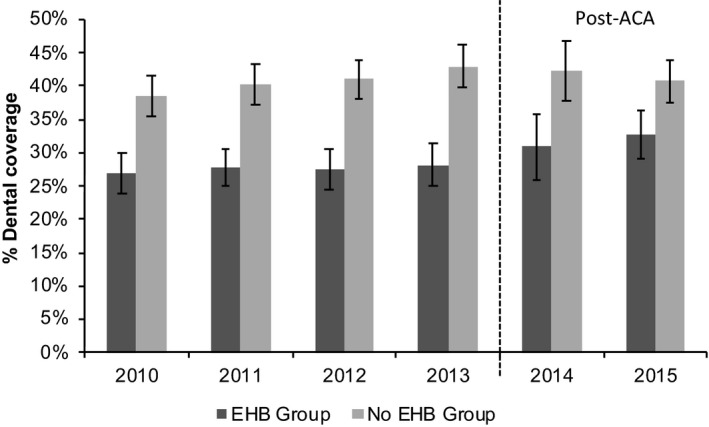
Percentage of children with private dental coverage, NHIS 2010‐2015. EHB, essential health benefits; NHIS, National Health Interview Survey
Figure 2 presents the weighted, unadjusted annual percentages of children with private dental insurance coverage and any dental visits in the last 12 months for the EHB and no EHB groups. During the pre‐ACA period, annual rates of dental visits were not significantly different for the EHB group (P = 0.100). Rates were significantly higher in the post‐ACA period (79.4 percent, 95 percent CI = 77.5 percent, 81.3 percent) than the pre‐ACA period (73.8 percent, 95 percent CI = 72.3 percent, 75.2 percent) for the EHB group (P < 0.001), with the highest rate of 82.1 percent observed in 2014 (95 percent CI = 78.5 percent, 85.7 percent). For the no EHB group, annual rates of dental visits were significantly different during the pre‐ACA period (P = 0.266), ranging from 75.8 percent (95 percent = 73.4 percent, 78.2 percent) in 2010 to 81.4 percent in 2013 (95 percent = 79.0 percent, 83.8 percent). Rates in the pre‐ACA period (79.2 percent, 95 percent CI = 78.0 percent, 80.4 percent) were not significantly different from rates in the post‐ACA period (80.8 percent, 95 percent CI = 79.1 percent, 82.5 percent) for the no EHB group (P = 0.122).
Figure 2.
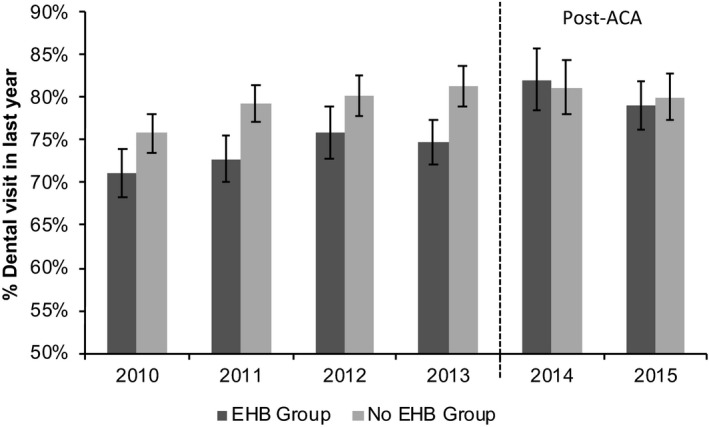
Percentage of children with a dental visit in the last year, NHIS 2010‐2015. NHIS, National Health Interview Survey; EHB, essential health benefits
Rates of dental coverage and dental visits for the EHB and no EHB groups had similar quarter‐to‐quarter changes. We tested prepolicy trends using observations from 2010 to 2013 and found no significant differences in trends between the treatment and comparison groups during any of the preperiod years for both dental coverage and dental visits (P < 0.15 from joint test of significance), which supports our choice of comparison group. These results are available in Appendix S1.
3.1. Effect on dental coverage
Table 3 presents the results of the regression models examining the effect of the ACA's EHB package. The regression results including the year‐quarter fixed effects are provided in Appendix S2. Our difference‐in‐differences results indicate that private dental benefits coverage increased by 4.6 percentage points (P = 0.013) more for children likely to be affected by the EHB compared to a comparison group of children unlikely to be affected by the ACA's EHB package in 2014 and 2015, relative to the prepolicy period of 2010‐2013. Other factors significantly associated with dental coverage included having a well medical visit in the past 12 months and family income greater than 300 percent FPL.
Table 3.
Results from linear regression models examining impact of ACA on dental coverage and dental visits, NHIS 2010‐2015
| Dental coverage in last year | Dental visit in last year | |||||
|---|---|---|---|---|---|---|
| Coefficient | Cluster standard error | P‐value | Coefficient | Cluster Standard Error | P‐value | |
| Post‐ACA * EHB Group | 0.046* | 0.018 | 0.013 | 0.027 | 0.015 | 0.071 |
| EHB Group | −0.122*** | 0.012 | 0.000 | −0.034** | 0.009 | 0.001 |
| Male | 0.013 | 0.010 | 0.194 | −0.007 | 0.009 | 0.438 |
| Race (reference: white) | ||||||
| Black | 0.05** | 0.018 | 0.008 | −0.002 | 0.010 | 0.891 |
| Other | 0.002 | 0.015 | 0.900 | −0.018 | 0.015 | 0.228 |
| Hispanic | −0.023 | 0.017 | 0.189 | −0.048** | 0.013 | 0.001 |
| Health status (reference: Excellent health) | ||||||
| Very good health | 0.003 | 0.010 | 0.758 | −0.008 | 0.008 | 0.332 |
| Good health or worse | 0.002 | 0.016 | 0.924 | −0.042* | 0.016 | 0.012 |
| Well medical visit in past 12 months | 0.038** | 0.014 | 0.010 | 0.114*** | 0.016 | 0.000 |
| Limitation of activity | 0.011 | 0.019 | 0.580 | 0.0203 | 0.016 | 0.216 |
| Family income <300% FPL | −0.068*** | 0.012 | 0.000 | −0.093*** | 0.008 | 0.000 |
| State expanded Medicaid | −0.008 | 0.018 | 0.660 | −0.011 | 0.016 | 0.494 |
| Urban | 0.006 | 0.020 | 0.775 | 0.011 | 0.011 | 0.320 |
| Age in years | 0.001 | 0.001 | 0.627 | 0.030*** | 0.001 | 0.000 |
| Family size | −0.004 | 0.004 | 0.298 | 0.0123** | 0.004 | 0.002 |
| CHIP eligibility upper‐income limit | −0.00004 | 0.000 | 0.935 | −0.00004 | 0.000 | 0.833 |
| Dentists per 10 000 child population | −0.002*** | 0.001 | 0.000 | 0.0005 | 0.001 | 0.350 |
| Intercept | 0.331** | 0.123 | 0.010 | 0.423*** | 0.069 | 0.000 |
| Total observations | 16 404 | 16 404 | ||||
| Adjusted R‐squared | 0.0519 | 0.1565 | ||||
Notes: Models included standard errors clustered at the state‐level, state fixed effects, year‐quarter dummy variables, and probability weights. The full regression results are available in the Supporting Information, exhibit 1. The first two quarters of 2014 are dropped. *P < 0.05, **P < 0.01, ***P < 0.001.
ACA, Affordable Care Act; CHIP, Children's Health Insurance Program; EHB, essential health benefits; FPL, federal poverty level; NHIS, National Health Interview Survey.
3.2. Effect on dental visits
Table 3 also presents estimates of the effect of the ACA's EHB package on utilization, as measured by whether a child had a dental visit in the last year. The percentage of children having a dental visit in the past year increased by a nonsignificant 2.7 percentage points (P = 0.071) in the EHB group compared to the no EHB group after this ACA policy took effect, thus there was no significant difference in visit rates in the EHB vs no EHB groups. Other factors significantly associated with having a dental visit included having a well medical visit in the past 12 months, family income greater than 300 percent FPL, older age, and larger family size. Additionally, children in worse physical health were less likely to have a dental visit than children with excellent physical health.
3.3. Robustness checks
To test the assumption that no other trends are differentially impacting the EHB group of children as compared to the no EHB group, we estimated a difference‐in‐differences specification with interaction terms for each treated group‐quarter combination. If dental insurance rates were diverging between the EHB and no EHB groups prior to 2014, we could not attribute our regression estimates to the ACA. In Appendix S3, the results illustrate that the coefficients from the dental coverage model for the EHB group‐quarter interactions in the preperiod quarters are insignificant and there was a slight negative trend for the EHB group. Starting in 2014 quarter 4, the coefficients are positive, although not significant. Together, this is further evidence that the increase in private dental insurance for children only began after the implementation of the ACA policy. The results from the dental visits model are less conclusive. Of the 15 EHB group‐quarter interactions coefficients in the pre‐ACA period, four are significant at the P < 0.05 level. Starting in 2014, quarter 3, the coefficients are positive and the coefficient for 2015 quarter 4 is significant (P = 0.02).
4. DISCUSSION
While the ACA remains law, support for the EHB package in its current form by Congress, the White House, and individual states remains uncertain, especially since CMS issued a final rule in April 2018 giving states flexibility in defining services included in the EHB package beginning in 2020.14 In this study, we found that the inclusion of pediatric dental care as an ACA essential health benefit led to a significant increase in private dental insurance, but no significant improvement in rates of dental visits for children likely to be affected by this policy. Dental coverage is provided to all publicly insured children and the inclusion of pediatric dental care through the ACA as an essential health benefit is an important step toward making dental coverage available to all children.
Increasing rates of dental coverage are important because many children remain without dental insurance coverage. Estimates of children without dental insurance exhibit great variability depending on the data source, ranging from 11.0 percent (from the 2014 MEPS for children aged 2‐18) to 52.3 percent (reported by the 2016 NHIS for children younger than 18, the source used to monitor Healthy People 2020 objectives).15, 16 The insurance marketplaces are convenient venues to reach a large population in need of coverage. During the 2014 open enrollment period, parents of nearly half a million children selected a marketplace insurance plan17 increasing to over one million children for the 2018 plan year.18 As states reevaluate how they offer dental coverage and the EHB package overall,14 steps can potentially be taken to further increase the number of children with dental coverage. States vary in how pediatric dental coverage is offered on marketplaces, and this may affect access to coverage and affordability of coverage. During 2015, four states required families to purchase pediatric dental coverage and five states offered only dental plans embedded into health plans, de facto requiring purchase of pediatric dental coverage.1, 19 One potential strategy would be for CMS or the remaining individual states to require families to purchase pediatric dental coverage or offer only health plans with embedded dental benefits on marketplaces. An American Dental Association analysis of 40 states found that on average, 36 percent of medical plans embedded pediatric or family dental benefits during the 2015 plan year.20 Of note, there is not yet evidence to support the claim that embedded dental benefits promote dental visits more so than requiring purchase of dental benefits or another strategy. However, health plans with an embedded pediatric dental benefit typically share a single deductible and out of pocket maximum payment for both medical and dental care, helping families to meet their deductible sooner.1 In addition to potentially increasing dental coverage, embedded plans provide an opportunity for greater coordination between medical and dental providers, something that is likely to increase in importance as more children receive preventive dental services from pediatricians.
While other studies have reported an association between private dental coverage and children's dental visits,2, 3 we did not find a significant association between the ACA and dental visits. Although the ACA aims to make pediatric dental coverage more available, it does little to address other barriers to dental care. Many factors affect children's receipt of dental care beyond dental coverage, including cost,21 distance to care,22 and parents’ prioritization of oral health.23 For example, in 2014, the maximum out of pocket cost on stand‐alone pediatric dental plans was $700 for a single child, which decreased to $350 in 2015.21 It is possible that there may be a delayed effect and that it may take more time to see a relationship between the ACA and dental visits. For example, studies of states expanding adult Medicaid dental benefits via the ACA reported no change in dental visits after one year,24 and significant increases in dental visits after three years.25 However, given the variety of obstacles that children encounter, dental coverage may not be sufficient to increase access to dental care in this population.
CMS has already taken steps to make dental coverage more affordable. During our study period, stand‐alone dental plans were not included in the calculation of these cost‐sharing subsidies. The Internal Revenue Service, however, issued a final rule in December 2016 that will require cost‐sharing subsidies to be based on the premiums of both a benchmark health plan and dental plan for the 2019 plan year.26 Requiring all health plans to embed pediatric dental coverage could also help to reduce patient costs. A study of expected out of pocket costs for pediatric dental care reported that costs were lower when dental coverage was embedded within a medical plan compared to stand‐alone dental plans.21
Finally, eleven Senators wrote to HHS Secretary Burwell in 2016 requesting a standardized definition of the pediatric benefits included in the EHB package.27 Because each state has its own benchmark health plan outlining the minimum scope of services to be covered, there is much variation in the pediatric services covered by states, including the types of dental services covered. For example, Utah requires that only preventive services be offered and not restorative treatments.1 The Senators suggested a standardized definition could be based on the Medicaid Early and Periodic Screening, Diagnostic and Treatment benefit, a state's CHIP plan, or recommendations from the American Academy of Pediatrics. Having standardized pediatric EHB benefits at the federal level would mean that all children, regardless of where they live, have coverage for similar, affordable care.
Despite the high individual, familial, and societal costs of poor oral health, few components of the ACA were designed to improve access to dental care and oral health. The ACA allows young adults to remain on their parents’ private insurance policies until age twenty‐six, which has helped to increase this population's dental coverage and access to dental care.6, 7 Although more adults gained Medicaid coverage in states that expanded eligibility,28 16 state Medicaid programs do not provide any adult dental benefits or benefits beyond emergency care.29 Our findings of the success of the EHB policy at increasing rates of dental coverage for children suggests that additional policies that ease access to dental insurance coverage for adults should be considered. For example, expanding the essential health benefit to require dental coverage for all ages could help to reduce the 33 percent adults without dental coverage.30
This study has important limitations, including the use of self‐reported NHIS data. Our treatment and comparison groups were defined according to a parent's reported employer size and the accuracy of self‐reported of firm size is unknown. Additionally, our measure of pediatric dental coverage may be understated if a parent is unaware they purchased a health plan with embedded pediatric dental benefits, which is particularly problematic in states that offered only embedded plans. While we are not aware of any research focused on this, prior research on caregivers of Medicaid enrolled children, all of whom have dental benefits, suggests lack of knowledge of dental benefits may be a barrier to care.31, 32 Relatedly, if a parent is not aware they purchased pediatric dental coverage, they may be less likely to take their child to the dentist. Thus, we may underestimate the effect of the EHB policy on coverage and visits.
Importantly, our measure of “treatment,” in this case whether the child is likely to be affected by the EHB, may suffer from measurement error. First, the treatment group includes children in families who directly purchased health insurance prior to the implementation of the ACA and these children may have grandfathered plans that were not required to cover the EHB. These children make up only 7 percent of our analytic sample. According to the Kaiser Family Foundation, 25 percent of covered workers in 2015 were enrolled in a grandfathered health plan.33 Additionally, although children in the treatment group are eligible to receive coverage via the small‐group insurance markets, they may have received coverage through self‐insured small‐group market health plans, which were not required to cover the EHB. However, only about 8 percent to 16 percent of firms with fewer than 100 full‐time employees’ self‐insure.34 Taken together, these limitations imply that our “treatment” group may actually contain some “comparison” individuals, which would attenuate our estimated treatment effect. Thus, we view our results as a conservative or lower bound of the true treatment effect.
Our findings may have limited generalizability because we restricted our sample to parent/child dyads in the NHIS, which represents a subset of children who may be eligible for plans with the EHB package. We may underestimate the effect of the EHB package on dental coverage and visits if children most likely to obtain these plans are less likely to live in households where the sample adult is the child's parent, as was required for our data linkage and analysis. Conversely, we may overestimate the effect of the EHB package on dental coverage and visits if children most likely to obtain these plans are most likely to live in households where the sample adult is the child's parent. While the NHIS's selection of the sample adult is random, the sample adult may not be the child's parent in multigenerational families. Finally, our key interest was the difference in outcomes for the treatment and control groups pre and post‐ACA implementation, however, as reported by prior studies we note that our NHIS estimates of dental visits are likely overstated.35, 36
5. CONCLUSION
To our knowledge, our study is the first to demonstrate that the inclusion of pediatric dental care in the ACA's EHB package was associated with a significant increase in rates of dental insurance coverage. Our findings of the positive impact of the EHB of pediatric dental coverage should be kept in mind as Congress, CMS, and individual states consider changing the EHB. Legislation or regulations that eliminate the pediatric dental benefit in the EHB are likely to have a negative impact on children's access to private dental coverage.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: This project was funded by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number R40MC29442. The information, content and/or conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
This study used data from the Research Data Center. The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the Research Data Center, the National Center for Health Statistics, or the Centers for Disease Control and Prevention.
Kranz AM, Dick AW. Changes in pediatric dental coverage and visits following the implementation of the affordable care act. Health Serv Res. 2019;54:437‐445. 10.1111/1475-6773.13093
REFERENCES
- 1. Snyder A, Kanchinadam K, Hess C, Dolan R. Improving integration of dental health benefits in health insurance marketplaces. https://nashp.org/improving-integration-dental-health-benefits-health-insurance-marketplaces/. Updated April 2014. Accessed Mar 23, 2017.
- 2. Lewis C, Mouradian W, Slayton R, Williams A. Dental insurance and its impact on preventive dental care visits for U.S. children. J Am Dent Assoc. 2007;138(3):369‐380. [DOI] [PubMed] [Google Scholar]
- 3. Zhou JY, Elyasi M, Amin M. Associations among dental insurance, dental visits, and unmet needs of US children. J Am Dent Assoc. 2017;148(2):92‐99. [DOI] [PubMed] [Google Scholar]
- 4. ADA Health Policy Institute . 2016 Take‐up rate of stand‐alone dental plans in HealthCare.gov. https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIgraphic_0416_3.pdf?la=en. Updated April 2016. Accessed February 22, 2018.
- 5. ADA Health Policy Institute . 2017 Take‐up rate of stand‐alone dental plans. https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIGraphic_0517_1.pdf?la=en. Updated May 2017. Accessed February 22, 2018.
- 6. Vujicic M, Yarbrough C, Nasseh K. The effect of the Affordable Care Act's expanded coverage policy on access to dental care. Med Care. 2014;52(8):715‐719. [DOI] [PubMed] [Google Scholar]
- 7. Sommers BD, Buchmueller T, Decker SL, Carey C, Kronick R. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Aff. 2013;32(1):165‐174. [DOI] [PubMed] [Google Scholar]
- 8. Dye BA, Thornton‐Evans G, Li X, Iafolla TJ. Dental caries and sealant prevalence in children and adolescents in the United States, 2011–2012. https://www.cdc.gov/nchs/data/databriefs/db191.pdf. Updated March 2015. Accessed January 25, 2017. [PubMed]
- 9. Uberoi N. The patient protection and affordable care act's essential health benefits (CRS Report R44163). https://fas.org/sgp/crs/misc/R44163.pdf. Updated August 27, 2015. Accessed January 24, 2017.
- 10. HHS Office of Disease Prevention and Health Promotion . Healthy People 2020: Access to health services. https://www.healthypeople.gov/2020/topics-objectives/topic/Access-to-Health-Services/objectives. Updated 2017. Accessed December 3, 2017.
- 11. National Center for Health Statistics . Variance estimation guidance, NHIS 2006‐2015 https://www.cdc.gov/nchs/data/nhis/2006var.pdf. Updated June 13, 2016. Accessed October 3, 2018.
- 12. Karaca‐Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health Services Res 2012;47(1pt1):255‐274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bertrand M, Duflo E, Mullainathan S. How much should we trust differences‐in‐differences estimates? Q J Econ. 2004;119(1):249‐275. [Google Scholar]
- 14. Centers for Medicare and Medicaid Services . Patient protection and affordable care act; HHS notice of benefit and payment parameters for 2019. Final rule. Federal Reg. 2018;83(74):16930. [PubMed] [Google Scholar]
- 15. Nasseh K, Vujicic M. Dental benefits coverage increased for working‐age adults in 2014. https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_1016_2.pdf?la=en. Updated October 2016. Accessed Feb 12, 2018.
- 16. HHS Office of Disease Prevention and Health Promotion . AHS‐1.2 Increase the proportion of persons with dental insurance. https://www.healthypeople.gov/2020/data/disparities/detail/Chart/3967/4/2016. Updated 2018. Accessed July 2, 2018.
- 17. Office of the Assistant Secretary for Planning and Evaluation . Health insurance marketplace: Summary enrollment report for the initial annual open enrollment period. http://aspe.hhs.gov/sites/default/files/pdf/83656/ib_2015mar_enrollment.pdf. Updated March 10, 2015. Accessed August 12, 2018.
- 18. Centers for Medicare & Medicaid Services . 2018 Marketplace open enrollment period public use files: Table 6. Consumers by age, gender, race/ethnicity, rural/non‐rural. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Marketplace-Products/2018_Open_Enrollment.html. Updated April 4, 2018. Accessed August 12, 2018.
- 19. Cousart C, Snyder A, Mention N. Dental benefits in health insurance marketplaces: An update on policy considerations. http://www.nashp.org/wp-content/uploads/2015/11/Dental-Benefits-11.151.pdf. Updated November 2015. Accessed August 12, 2018.
- 20. Yarbrough R, Vujicic M, Nasseh K. More dental benefits options in 2015 health insurance marketplaces. https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0215_1.ashx. Updated February 2015. Accessed March 26, 2017.
- 21. Vujicic M, Yarbrough C. Estimating premium and out‐of‐pocket outlays under all child dental coverage options in the federally facilitated marketplace. J Pediat. 2017;182:349‐355. [DOI] [PubMed] [Google Scholar]
- 22. Kranz AM, Lee J, Divaris K, Baker AD, Vann W. North Carolina physician‐based preventive oral health services improve access and use among young medicaid enrollees. Health Aff. 2014;33(12):2144‐2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Isong IA, Zuckerman KE, Rao SR, Kuhlthau KA, Winickoff JP, Perrin JM. Association between parents’ and children's use of oral health services. Pediatrics. 2010;125(3):502‐508. [DOI] [PubMed] [Google Scholar]
- 24. Nasseh K, Vujicic M. Early impact of the affordable care act's Medicaid expansion on dental care use. Health Serv Res. 2017;52(6):2256‐2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nasseh K, Vujicic M. The impact of the affordable care act's Medicaid expansion on dental care use through 2016. J Public Health Dent. 2017;77(4):290‐294. [DOI] [PubMed] [Google Scholar]
- 26. Internal Revenue Service . Premium Tax Credit Regulation VI. In. 81 FR 91755 Vol 2016‐300372016 Dec 19:91755‐91768.
- 27. US Senate . Letter from Senate Democrats to Secretary Sylvia Burwell of the Department of Health and Human Services. https://www.childrenshospitals.org/-/media/Files/CHA/Main/Issues_and_Advocacy/Key_Issues/Exchanges_and_Private_Coverage/Letters_and_Testimony/2016/Senate_Democrat_Dear_Colleague_Letter_on_Pediatric_EHBs.pdf. Updated May 5, 2016. Accessed March 23, 2017.
- 28. Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low‐income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501‐1509. [DOI] [PubMed] [Google Scholar]
- 29. Center for Health Care Strategies . Medicaid adult dental benefits: An overview. https://www.chcs.org/media/Adult-Oral-Health-Fact-Sheet_072718.pdf. Updated July 2018. Accessed October 10, 2018.
- 30. Nasseh K, Vujicic M. Dental benefits coverage rates increased for children and young adults in 2013. http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_1015_3.pdf?la=en. Updated October 2015. Accessed March 23, 2017.
- 31. Kelly SE, Binkley CJ, Neace WP, Gale BS. Barriers to care‐seeking for children's oral health among low‐income caregivers. Am J Public Health. 2005;95(8):1345‐1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nagahama SI, McNabb K, Vanderlinde M, et al. Improving utilization of preventive dental services by medicaid–enrolled children: focus on the parents. J Dent Child. 2002;69(3):325‐331. [PubMed] [Google Scholar]
- 33. Kaiser Family Foundation and the Health Research & Educational Trust . Employer health benefits 2015 annual survey. https://www.kff.org/health-costs/report/2015-employer-health-benefits-survey/. Updated September 22, 2015. Accessed June 24, 2017.
- 34. Pozen R, Vinjamoori A. Incentives for small firms to self fund their healthcare plans. https://www.brookings.edu/research/incentives-for-small-firms-to-self-fund-their-healthcare-plans/. Updated November 19, 2014. Accessed March 26, 2017.
- 35. Macek MD, Manski RJ, Vargas CM, Moeller J. Comparing oral health care utilization estimates in the United States across three nationally representative surveys. Health Serv Res. 2002;37(2):499‐521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Romaire MA, Bell JF, Huebner CE. Variations in children's dental service use based on four national health surveys. Pediatrics 2012;130(5):e1182‐9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


