Abstract
We are presenting a case of premature baby born at 32 weeks of gestation who was under regular follow-up with our retinopathy of prematurity (ROP) tele-screening team. During final follow-up at 41 weeks of postconceptional age, anterior segment image captured with RetCam showed a retrolental mass lesion in right eye resembling retinoblastoma or medulloepithelioma. The baby was referred to our base hospital for further evaluation, where a detailed examination showed no retrolental lesion or intraocular mass. This is the first case where imaging artifact, despite use of high-quality imaging system by well-trained staff, during ROP tele-screening appeared like a retrolental mass lesion and resulted in false-positive referral.
Keywords: Retrolental mass, teleophthalmology, tele-screening
Teleophthalmology is a progressively evolving branch in ophthalmology care which is meant to provide appropriate and timely distribution of ophthalmology assistance especially in underserved areas. It is being utilized for screening as well as diagnosis and to decide for urgency of referral for retinal pathologies, neuro-ophthalmology, glaucoma, uveitis, adnexal disease, and ocular emergency.[1] Teleophthalmology-based screening programs are well established for targeted conditions like diabetic retinopathy (DR) and retinopathy of prematurity (ROP). Diagnosis of nontargeted retinal disorders during tele-screening of targeted disorders is quite common.[2,3] Sometimes tele-screening might help in the diagnosis of acute ocular conditions such as retinal detachment and retinoblastoma, where immediate referral and early intervention prove to be highly valuable for final visual prognosis and morbidity.[3,4]
Tele-screening, however, may also result in unwarranted referral due to inherent limitations including poor imaging and inadequately trained staff causing avoidable psychological stress to the patients and their family.[1] We are presenting a case where imaging artifact, despite use of high-quality imaging system by well-trained staff, during ROP tele-screening appeared like a retrolental mass simulating as intraocular tumor and hence resulted in false-positive referral.
Case Report
A male baby born prematurely at 32 weeks of gestation with birth weight of 1,100 g with history of respiratory distress syndrome and consequently prolonged oxygen administration was examined at postnatal age of 3 weeks by our tele-screening team using RetCam shuttle pediatric retinal imaging system (Clarity Medical Systems, Inc, Pleasanton, CA). First examination showed immature vessels in both eyes. During further review, baby developed stage 2 ROP in zone 2 without plus disease in both the eyes, which gradually regressed spontaneously. During final tele-screening session at 41 weeks of post-conceptional age, though the fundus images showed mature vessels in both the eyes, anterior segment image of right eye showed a white mass with vascular component behind lens [Fig. 1]. The clarity of fundus images was good enough for ROP evaluation. The appearance of retrolental mass with resemblance to retinoblastoma or medulloepithelioma resulted in a referral of the baby to base hospital for further evaluation. The anterior segment as well as fundus examination at base hospital was found within normal limits. Ultrasound B scan and ultrasound biomicroscopic examination also showed no retrolental or posterior segment mass. On retrospective assessment of the image, we assumed that the retrolental whitish lesion could be an optic disc reflection resulting from imaging fallacies.
Figure 1.
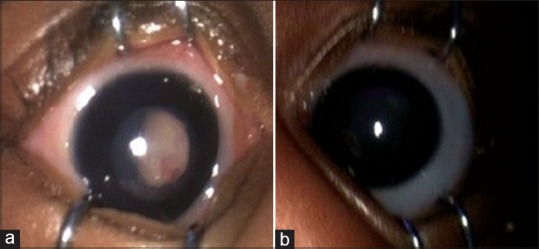
Anterior segment images taken with Retcam shuttle pediatric retinal imaging system (Clarity Medical Systems, Inc, Pleasanton, CA). (a) Right eye image showing pseudoretrolental whitish vascularized mass lesion with pharmacologically dilated pupil. (b) Left eye image showing normal appearing anterior segment with pharmacologically dilated pupil
Discussion
To our knowledge, this is the first case of false-positive referral during ROP tele-screening where imaging fallacy appeared as pseudoretrolental mass lesion. The anterior segment image taken during the final visit appeared very much like retinoblastoma or medulloepithelioma, and the baby was promptly referred for further evaluation. Detailed clinical examination ruled out the presence of any intraocular tumor or mass lesion.
Diagnosis of associated retinal and non-retinal pathologies in a tele-screening program is not uncommon. In a DR tele-screening study, nontargeted fundus findings were found in 67% eyes with hypertensive retinopathy (22%) and age-related macular degeneration (5.7%) being the most common.[2] Ocular conditions causing abnormalities of media transparency such as cataract and corneal opacity are also seen often.[2] In an ROP screening study by Vinekar et al., 7.66% infants had diagnosis other than ROP, which included cataract, lid abnormalities, corneal diseases, infective uveitis, and even retinoblastoma.[3] Capturing anterior segment images during tele-screening of retinal pathologies gives an added benefit of collateral diagnosis of various nonretinal ocular disease such as cataract, and corneal and adnexal pathologies. In our ROP tele-screening program, we capture anterior segment image as a routine procedure. This has helped us in timely referral of babies with congenital cataract and lacrimal swelling to tertiary center for further management (unpublished data).
Despite significant improvement in imaging technologies, poor-quality images are still mentioned as a critical cause for retina-specialist referral in tele-ophthalmology, with rates of approximately 3%–22%. Poor imaging itself is responsible for the large majority (86%) of referrals.[1] Usually, this issue may result from inadequate equipment and/or insufficient training. Therefore, adequately trained staffs are one of the pre-requisites to collect good quality images in tele-screening of ROP. However, image fallacy in our case was noted despite the use of excellent quality fundus imaging camera by experienced personnel.
In current era, there is increasing interest in the development of automated analysis software to replace human intelligence by artificial intelligence (AI). The main advantage of developing such AI-based screening system is to reduce the manpower, logistical, and cost-related burden involved in tele-medicine examination. In ophthalmology, AI-based screening system is being developed for detection and classification of DR and aggressive posterior ROP.[5,6] However, imaging artifact or poor-quality image as seen in our case can result in false or pseudodiagnosis leading to unwarranted referral. This case reminds us that teleophthalmology is not meant to substitute face-to-face eye examination.
Anterior segment imaging during tele-screening for retinal pathologies is a good practice, which could help in a collateral diagnosis of nontargeted anterior segment and adnexal pathologies. When Retcam is approached toward the eye while capturing anterior segment image, the optic disc might become visible from a distance resulting in artifact as seen in our case. The ophthalmic technicians must be aware of this finding, and a repeated imaging should be done to avoid the false-positive referral.
Conclusion
This case teaches us to keep in mind the possibility of pseudodiagnosis resulting from imaging fallacies despite the use of good-quality imaging techniques by well-trained staff. Nevertheless, in a screening program for diseases, such as ROP, a false-positive referral is better than a nonreferral due to false-negative reporting.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Grisolia ABD, Abalem FM, Lu Y, Aoki L, Matayoshi S. Teleophthalmology: Where are we now? Arq Bras Oftalmol. 2017;80:401–5. doi: 10.5935/0004-2749.20170099. [DOI] [PubMed] [Google Scholar]
- 2.Germain N, Galusca B, Deb-Joardar N, Millot L, Manoli P, Thuret G, et al. No loss of chance of diabetic retinopathy screening by endocrinologists with a digital fundus camera. Diabetes Care. 2011;34:580–5. doi: 10.2337/dc10-1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vinekar A, Bauer N, Mangalesh S, Mahendradas P, Kemmanu V, Mallipatna A, et al. Look what else we found – clinically significant abnormalities detected during routine ROP screening. Indian J Ophthalmol. 2015;63:373–7. doi: 10.4103/0301-4738.159859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCord SA, Lynch MG, Maa AY. Diagnosis of retinal detachments by a tele-ophthalmology screening program. J Telemed Telecare. 2018 doi: 10.1177/1357633X18760418. doi: 10.1177/1357633×18760418 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Pour EK, Pourreza H, Zamani KA, Mahmoudi A, Sadeghi AMM, Shadravan M, et al. Retinopathy of prematurity-assist: Novel software for detecting plus disease. Korean J Ophthalmol. 2017;31:524–32. doi: 10.3341/kjo.2015.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajalakshmi R, Subashini R, Anjana RM, Mohan V. Automated diabetic retinopathy detection in smartphone-based fundus photography using artificial intelligence. Eye. 2018;32:1138–44. doi: 10.1038/s41433-018-0064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


