Case Report
A 14-year-old boy, known patient of juvenile idiopathic arthritis (JIA) since 2008, was under follow-up with us since the past 2.5 years for the management of uveitis. He was investigated for other possible causes of uveitis elsewhere initially which included a negative Mantoux test and normal chest X-ray. He was initially started on oral methotrexate 25 mg/week and subsequently switched over to subcutaneous injection of adalimumab biosimilar (Exemptia). He received 40 mg subcutaneous injection of adalimumab every 2 weeks for 6 months, and then every 3 weeks for 6 months while on low-dose oral methotrexate (10 mg/week). He responded well to the systemic treatment and was maintaining quiet eyes for the past 1 year. Recently, he was diagnosed to have pulmonary tuberculosis and started on antitubercular treatment by the chest physician. His Mantoux test was positive (25 mm), and high-resolution computed tomography of the chest was suggestive of pulmonary tuberculosis. His best-corrected visual acuity in the right eye was 6/5 and left eye was 6/9. Slit-lamp examination revealed occasional cells in the anterior chamber of the right eye, posterior synechiae with minimal posterior subcapsular cataract in the left eye, and cells in anterior vitreous of the right eye. Fundus examination of the right eye revealed a solitary, choroidal nodule less than 1-disc diameter in size slightly temporal to the fovea [Fig. 1a]. Fundus examination of the left eye was normal. Swept-source optical coherence tomography of the right eye revealed a large homogeneous, hyporeflective area in the choroid, and fundus fluorescein angiogram of the right eye revealed early hypofluorescence in early phase of the angiogram followed by hyperfluorescence [Fig. 2a and b]. Indocyanine green angiography detected multiple small hypocyanescent spots in addition to the clinically evident choroidal nodule [Fig. 2c and d]. The patient was advised oral corticosteroid (40 mg/day) on a tapering schedule and to continue ATT. He was reexamined after a month. Fundus examination of the right eye revealed resolution of choroidal nodule. He was advised to continue the same treatment [Fig. 1b]. Fundus examination after 3 months of follow-up revealed healed choroidal nodule [Fig. 1c] and he was advised to stop oral steroid and continue ATT as per the advice of the chest physician.
Figure 1.

(a) Fundus examination of the right eye revealed a solitary, choroidal nodule less than 1-disc diameter in size slightly temporal to the fovea. (b) Fundus examination of the right eye revealed gradual resolution of choroidal nodule. (c) Fundus examination of the right eye showing healed choroiditis at 3-month follow-up
Figure 2.
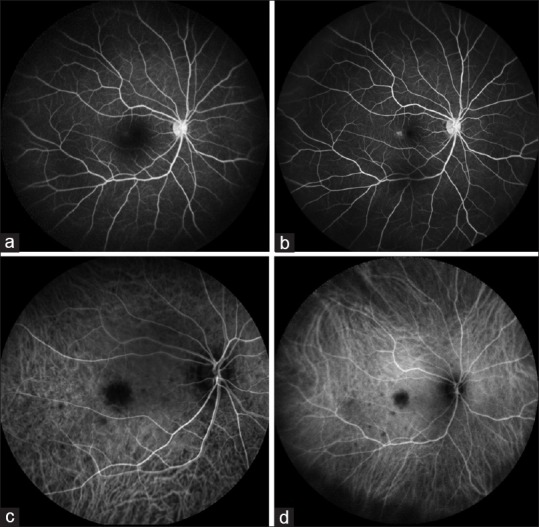
(a and b) Fundus fluorescein angiography of the right eye showing area of hypofluorescence corresponding to the choroidal tubercle and subsequent hyperfluorescence in late frames of the angiogram. (c and d) Indocyanine green angiography photographs of the right eye showing choroidal nodule as hypocyanescent spot throughout angiogram. Kindly also note the multiple small hypocyanescent lesions seen on indocyanine green angiography
Discussion
Adalimumab is considered the biological with the strongest level of evidence of efficacy for treatment of JIA when added to methotrexate.[1,2] However, use of the drug has been reported to be associated with increased risk of tuberculosis and there are many reports of the disseminated tuberculosis following adalimumab therapy despite negative screening for tuberculosis prior to the initiation of the drug.[3] Choroidal tubercle is the most characteristic clinical manifestation of ocular tuberculosis and represents the hematogenous dissemination of tubercular bacilli from pulmonary or extrapulmonary sites. In an endemic country like India, our case report exerts caution and importance of close vigilance following the use of biological agents. It also highlights the importance of routine ophthalmological examination even in visually asymptomatic patients developing tuberculosis following biological therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ramanan AV, Dick AD, Jones AP, McKay A, Williamson PR, Compeyrot-Lacassagne S, et al. Adalimumab plus methotrexate for uveitis in juvenile idiopathic arthritis. N Engl J Med. 2017;376:1637–46. doi: 10.1056/NEJMoa1614160. [DOI] [PubMed] [Google Scholar]
- 2.Sen ES, Ramanan AV. Juvenile idiopathic arthritis-associated uveitis. Best Pract Res Clin Rheumatol. 2017;31:517–34. doi: 10.1016/j.berh.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Cantini F, Niccoli L, Goletti D. Adalimumab, etanercept, infliximab, and the risk of tuberculosis: Data from clinical trials, national registries, and postmarketing surveillance. J Rheumatol Suppl. 2014;91:47–55. doi: 10.3899/jrheum.140102. [DOI] [PubMed] [Google Scholar]


