Abstract
A 62-year-old man presented with a 1-month history of right eye pain unresponsive to artificial tears and topical steroids. At presentation, bullous yellowish fluid collection was noted in the nasal conjunctiva. Corneal thinning and opacity were observed at the 3 o’clock position of the cornea. High-frequency radiowave ablation and biopsy were performed at the affected area. Conjunctival lymphangiectasia was confirmed by excisional biopsy. An improvement in the degree of corneal dellen and chemosis was evident 1 week after ablation. Use of a high-frequency radiowave electrosurgical device may be a simple and effective treatment option for symptomatic conjunctival lymphangiectasia.
Keywords: Anterior segment optical coherence tomography, chemosis, electrosurgery, lymphangiectasis
Conjunctival lymphangiectasis is characterized by dilated lymphatic vessels of the bulbar conjunctiva and it occurs mainly in the interpalpebral area.[1] Although it usually resolves spontaneously without causing ocular symptoms, it can be associated with ocular symptoms such as irritation, dryness, epiphora, and pain.[2,3] In such situations, more active treatment is necessary. Several therapeutic options, including topical steroid administration, surgical excision, and liquid nitrogen and subconjunctival bevacizumab injection, have been reported.[4,5,6] Han et al.[3] reported that high-frequency radiowave electrosurgery is a safe and effective modality for the treatment of symptomatic lymphangiectasis. However, in previous studies, lymphangiectasis was confirmed only by clinical diagnosis without histological confirmation by biopsy. To our knowledge, however, corneal dellen in symptomatic lymphangiectasis has not been reported. Herein, we report a case of biopsy-proven conjunctival lymphangiectasia accompanied by corneal dellen, which was successfully treated using a high-frequency radiowave electrosurgical device.
Case Report
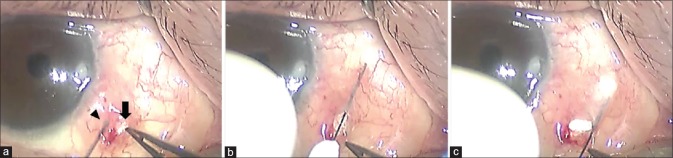
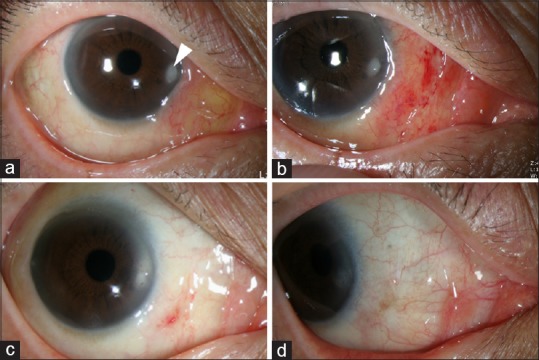
A 62-year-old man presented with a 1-month history of redness and ocular pain in the right eye. He was diagnosed with allergic conjunctivitis at a local clinic and was prescribed olopatadine twice per day and 0.5% loteprednol etabonate 4 times per day. Examination of the right eye revealed dilated lymphatic vessels and bullous conjunctival swelling, with a yellowish subconjunctival fluid in the nasal bulbar conjunctiva [Fig. 1a]. Focal corneal thinning and opacity were observed at the 3 o’clock position of the cornea. Anterior segment optical coherence tomography imaging revealed numerous dilated lymphatic vessels in the subconjunctival tissue [Fig. 2]. A clinical diagnosis of corneal dellen secondary to conjunctival lymphangiectasia was suspected. Because the patient did not respond to conventional therapy, complained of severe pain due to dellen, we decided to undergo immediate treatment involving radiowave electro-ablation in the right eye. Before the ablation, a small piece of subconjunctival tissue was excised for confirmation of conjunctival lymphangiectasia. Conjunctival ablation was performed with reference to a protocol previously described by Han et al.[3] After instillation of 0.5% proparacaine (Alcaine, Alcon Laboratories, Fort Worth, TX), dilated lymphatic vessels and surrounding swollen conjunctiva were determined as target lesions. A fine-needle electrode from the 4.0-MHz radiowave system (Ellman Surgitron Dual Frequency RF; Ellman International, Inc., Hewlett, NY, USA) was inserted into the target area [Fig. 3a and b]. One to 2 s of ablation caused a gradual change in the conjunctiva to a dusky white color (blanching) [Fig. 3c]. All ablations were performed at the lowest power setting of 1 (of 100) in the cutting mode. Histopathological examination revealed dilated lymphatic vessels and fluid collection, which is consistent with conjunctival lymphangiectasia [Fig. 4].
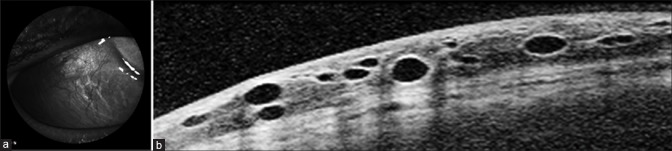
Figure 1.
Slit-lamp photographs of the patient. (a) Chemosis and dilated lymphatics of the right inferonasal and inferotemporal conjunctiva and corneal dellen (arrow head) were observed preoperatively. (b) One-week postoperatively, photograph revealing marked improvement in conjunctival lymphangiectasia and chemosis. (c) Photograph 1 month after treatment reveals complete resolution of yellowish subconjunctival fluid accumulation and corneal dellen. (d) Four weeks postoperatively, there is little conjunctival scarring and no lymphatic dilatation
Figure 2.
Optical coherence tomography (OCT) imaging of conjunctival lymphangiectasia. (a) Infrared image revealing vessel-like configurations. (b) Anterior segment OCT image revealing numerous dilated lymphatic vessels
Figure 3.
Surgical procedure for electrosurgical ablation of lymphangiectasia. (a) The tip of the electrode was inserted into the target area (arrow head). To avoid bleeding, electrode was inserted away from the blood vessels. Excisional biopsy site was observed (arrow). (b) After passing through the conjunctiva, the electrode advanced further through the subconjunctival space. (c) To avoid scleral injury, the conjunctiva was lifted and ablated for 1–2 s until the conjunctiva turned white. Ablation was repeated until the dilated lymphatic vessels and surrounding area turned white
Figure 4.
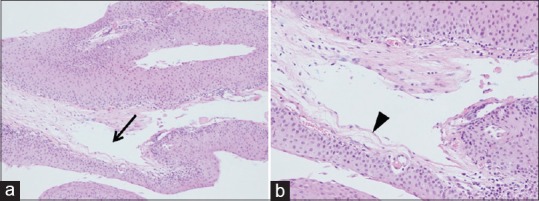
Hematoxylin–eosin staining of conjunctival lymphangiectasia. (a) Pathological examination after conjunctival excisional biopsy reveals localized dilatation of lymphatic vessels (arrow) (magnification ×100). (b) The dilated lymphatics have thin vessel walls (arrow head) and contain clear fluid in the lumen (magnification ×200)
One-week postoperatively, subconjunctival fluid accumulation was markedly decreased and corneal dellen was improved [Fig. 1b]. One-month postoperatively, the conjunctival injection had improved, with complete resolution of subconjunctival fluid accumulation and conjunctival lymphatic vessels [Fig. 1c]. The patient remained asymptomatic, with no signs of recurrence of lymphatic vessels at 4 months postoperatively, and no adverse effects were observed [Fig. 1d].
Discussion
Conjunctival lymphangiectasis may occur in association with previous ophthalmic surgery, radiotherapy, or other ocular diseases.[2,7] It may disappear naturally without symptoms, however, when conjunctival edema is merged or enlarged, and symptoms such as irritation, dryness, and epiphora may occur. Surgical treatment is considered if there is no response to conservative treatment.[2] Dellen is the result of topical stromal dehydration caused by a reduced tear film spread over a focal corneal area.[8,9,10] Corneal dellen is characterized by corneal thinning and accompanied by an adjacent focal conjunctival or corneal elevation. Therefore, lymphaniectasia may cause corneal dellen. In general, lubrication and preservative-free artificial tear drops can be tried when corneal dellen is encountered. However, in this case, we decided to attempt surgical treatment because the patient showed no improvement on using topical therapy, and conjunctival chemosis due to lymphangiectasia persisted.
High-frequency radiowave electrodevices use high-frequency (4 MHz) waves and have been applied to tissue for incision, dissection, hemostasis, and dehydration. These devices have been widely used in dermatology, general surgery, and plastic surgery. In ophthalmology, they are used for incision of the eyelid, treatment of distichiasis, conjunctivochalasis, superior limbic keratoconjunctivitis, and conjunctival cyst ablation.[11,12,13,14,15] The use of high-frequency radiowave electrodevices has been reported to be less time-consuming, cause less bleeding, and be less likely to cause complications because of less thermal injury to the surrounding tissues.[12,15] When a high-frequency radiowave is applied to the subconjunctival tissue, it causes coagulation by local burns to tissues because of the friction of water molecules by the conversion of radiowaves into heat.[16] It is believed that lymphangiectasis is improved by inhibiting lymphatic fluid from entering the subconjunctival space as the dilated lymphatic wall and surrounding tissues collapse.[3] In this case, subconjunctival fluid decreased significantly at 7 days postoperatively, and at 1-month postoperatively, complete recovery was achieved. However, unlike previous studies, our case is more meaningful because conjunctival lymphangiectasia was confirmed on biopsy. In addition, in our case, corneal dellen accompanied lymphangiectasis. When a small piece of subconjunctival tissue is removed for biopsy, some subconjunctival fluid may leak, and the target area may consequently become ambiguous. However, as shown in Fig. 3, in our case, the subconjunctival fluid did not leak through the simple drainage passage and the use of the preoperation anterior photograph allowed for ablation to be performed on the target area. We postulated that high-frequency electrosurgery is considered safer and more effective than surgical procedure because it has less effect on ocular surface irregularity and it can preserve more conjunctival tissues compared with surgical resection, which may contribute to delayed recovery of corneal dellen.
Conclusion
We confirmed conjunctival lymphangiectasis through biopsy and could effectively treat conjunctival lymphangiectasis and secondary corneal dellen in a short time period using a high-frequency radiowave electrosurgery device. Because high-frequency radiowave electrosurgery can preserve conjunctival tissue compared with surgical removal and has little effect on ocular surface irregularity, it appears to be a satisfactory treatment option that can be considered a preferential treatment before attempting an operative procedure in patients with conjunctival lymphangiectasis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Stewart DE. 1st ed. Vol. 8. St Louis: Mosby; 1965. System of Ophthalmology; p. 40. [Google Scholar]
- 2.Welch J, Srinivasan S, Lyall D, Roberts F. Conjunctival lymphangiectasia: A report of 11 cases and review of literature. Surv Ophthalmol. 2012;57:136–48. doi: 10.1016/j.survophthal.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Han KE, Choi CY, Seo KY. Removal of lymphangiectasis using highfrequency radio wave electrosurgery. Cornea. 2013;32:547–9. doi: 10.1097/ICO.0b013e31825d569f. [DOI] [PubMed] [Google Scholar]
- 4.Meisler DM, Eiferman RA, Ratliff NB, Burns CD. Surgical management of conjunctival lymphangiectasis by conjunctival resection. Am J Ophthalmol. 2003;136:735–6. doi: 10.1016/s0002-9394(03)00398-2. [DOI] [PubMed] [Google Scholar]
- 5.Fraunfelder FW. Liquid nitrogen cryotherapy of lymphangiectasia. Cornea. 2009;28:594–6. doi: 10.1097/ICO.0b013e318191432d. [DOI] [PubMed] [Google Scholar]
- 6.Fraunfelder FW. Liquid nitrogen cryotherapy of conjunctival lymphangiectasia: A case series. Arch Ophthalmol. 2009;127:1686–7. doi: 10.1001/archophthalmol.2009.306. [DOI] [PubMed] [Google Scholar]
- 7.Tan JC, Mann S, Coroneo MT. Successful treatment of conjunctival lymphangiectasia with subconjunctival injection of bevacizumab. Cornea. 2016;35:1375–7. doi: 10.1097/ICO.0000000000000899. [DOI] [PubMed] [Google Scholar]
- 8.Mai G, Yang S. Relationship between corneal dellen and tear film breakup time. Yan Ke Xue Bao. 1991;7:43–6. [PubMed] [Google Scholar]
- 9.Moesen I, Hafezi F, Paridaens D. Corneal dellen secondary to conjunctival chemosis following transconjunctival orbital decompression. Klin Monbl Augenheilkd. 2007;224:856–7. doi: 10.1055/s-2007-963618. [DOI] [PubMed] [Google Scholar]
- 10.Fresina M, Campos EC. Corneal dellen as a complication of strabismus surgery. Eye (Lond) 2009;23:161–3. doi: 10.1038/sj.eye.6702944. [DOI] [PubMed] [Google Scholar]
- 11.Hurwitz JJ, Johnson D, Howarth D, Molgat YM. Experimental treatment of eyelashes with high-frequency radio wave electrosurgery. Can J Ophthalmol. 1993;28:62–4. [PubMed] [Google Scholar]
- 12.Youm DJ, Kim JM, Choi CY. Simple surgical approach with high-frequency radio-wave electrosurgery for conjunctivochalasis. Ophthalmology. 2010;117:2129–33. doi: 10.1016/j.ophtha.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 13.Woo KI, Choi CY. High-frequency radiowave electrosurgery for persistent conjunctival chemosis following cosmetic blepharoplasty. Plast Reconstr Surg. 2014;133:1336–42. doi: 10.1097/PRS.0000000000000175. [DOI] [PubMed] [Google Scholar]
- 14.Ahn JM, Choi CY, Seo KY. Surgical approach with high-frequency radiowave electrosurgery for superior limbic keratoconjunctivitis. Cornea. 2014;33:210–4. doi: 10.1097/ICO.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 15.Park J, Lee S, Suh E. Removal of conjunctival cyst with high-frequency radio-wave electrosurgery. Can J Ophthalmol. 2015;50:378–3. doi: 10.1016/j.jcjo.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Huang SK. Advances in applications of radiofrequency current to catheter ablation therapy. Pacing Clin Electrophysiol. 1991;14:28–42. doi: 10.1111/j.1540-8159.1991.tb04044.x. [DOI] [PubMed] [Google Scholar]