Abstract
Objective
To develop a multivariate tool that would predict recurrent instability after a first-time traumatic anterior shoulder dislocation.
Methods
Participants (aged 16–40 years) were recruited across New Zealand into a prospective cohort study. Baseline data were collected during a telephone interview and through examination of radiology records. Variables associated with recurrent instability were selected for the multivariate logistic regression model using backwards selection (p<0.10). Coefficients for those variables retained in the model were used to develop the predictive tool.
Results
Among the 128 participants, 36% had redislocated at least once in the first 12 months. Univariate analysis showed an increased likelihood of recurrent dislocation with bony Bankart lesions (OR=3.65, 95% CI 1.05 to 12.70, p=0.04) and participants who had: not been immobilised in a sling (OR = 0.38, 95% CI 0.15 to 0.98, p=0.05), higher levels of shoulder activity (OR=1.13, 95% CI 1.01 to 1.27, p=0.03), higher levels of pain and disability (OR=1.03, 95% CI 1.01 to 1.06, p=0.02), higher levels of fear of reinjury (OR=1.12, 95% CI 1.01 to 1.26, p=0.04) and decreased quality of life (OR=1.01, 95% CI 1.00 to 1.02, p=0.05). There was no significant difference in those with non-dominant compared with dominant shoulder dislocations (p=0.10) or in those aged 16–25 years compared with 26–40 years (p=0.07).
Conclusion
Six of seven physical and psychosocial factors can be used to predict recurrent shoulder instability following a first-time traumatic anterior shoulder dislocation.
Keywords: shoulder dislocation, prospective study, fear, recurrence, pain
Introduction
The incidence of first-time traumatic anterior shoulder dislocation (FTASD) is around 23 per 100 000 person-years1 with increased dislocation rate in contact athletes.2 Recurrent instability following such injuries ranges from 26%3 to 92%.4 This wide variation may be explained by the heterogeneous populations in these studies.5 Risk factors for recurrent instability following an FTASD have been described in recent systematic reviews and meta-analyses.6–8 These risk factors may be categorised as either modifiable or non-modifiable. Modifiable risk factors include manual occupations,9 occupations where the upper limb is used above shoulder height,10 immobilisation following the dislocation,11 involvement in collision sport12 and time to return to sport.12 Psychosocial factors such as higher levels of pain13 and fear of reinjury14 15 may also be modifiable risk factors. Non-modifiable risk factors include greater tuberosity fractures,3 9 11 12 16 Hill-Sachs lesions,11 16 17 bony Bankart lesions,9 11 17 18 axillary nerve palsy,12 18 age,3 9 11 16–18 gender3 9 11 12 and hypermobility.12 17
While knowledge of individual risk factors is important in clinical practice, prognostic models use multiple predictive factors to calculate risk of recurrent instability in individual patients.19 Personal, customised care is a goal of clinical practice.20 Customising healthcare carries the costs of additional communication, cognition, coordination and capability.20 21 However, these costs can be minimised through the use of decision-making aids which enable patients and clinicians to make informed treatment choices.
Decision-making tools and algorithms have been developed to assist clinicians and to enable patients with shoulder instability to make informed choices about their healthcare.22–30 Of these, only two5 27 tools have been developed to predict outcomes or management for people with an FTASD. These tools5 27 primarily use age and gender to predict recurrent instability. Incorporation of other known significant risk factors into a prognostic model would improve the accuracy of identifying those more likely to have recurrent instability and enhance clinical decision-making for people following an FTASD.
There are very few high-quality prospective studies examining risk factors for recurrent instability following an FTASD.6 7 We aimed to develop a multivariate prognostic tool which can be used to predict recurrent instability, based on known risk factors. We hypothesised that key variables, other than the established variables age and gender,12 would predict recurrent instability following an FTASD.
Methods
Design and setting
This prospective cohort study was approved by the university and Accident Compensation Corporation (ACC) ethics committees. Consultation with two orthopaedic surgeons, two sports physicians and two physiotherapists, who had a special interest in shoulder pathology, was undertaken to examine previously reported risk factors6 and determine whether additional variables of perceived clinical importance could be identified. Following this consultation, the variables identified from the meta-analysis6 and the clinical team were combined to form the beta version of the clinical prediction tool.
Participants
We completed this prospective study with people who had suffered an FTASD to examine the risk factors which predisposed them to recurrent shoulder instability or protected them from further instability. Participants were eligible for inclusion if they:
Were aged between 16 and 40 years.
Sustained an FTASD in New Zealand (NZ).
Had a shoulder radiograph.
Had an NZ contact address.
Had registered their shoulder dislocation with Accident Compensation Corporation (ACC) between the dates of May 2015 and April 2016.
Provided verbal informed consent to take part in the study.
Participants were excluded (n=81) if they had undergone surgical intervention for their current shoulder injury within 12 weeks of the injury as they were no longer able to demonstrate the natural history of an FTASD (n=3). Participants were also excluded if they reported a previous shoulder instability episode or other shoulder pathology such as impingement/acromioclavicular joint (ACJ) disruption at initial interview (n=43) or showed radiological evidence of a previous shoulder instability episode in subsequent radiological report (n=15). Radiological evidence excluded those who demonstrated pathology other than an anterior dislocation (n=18) and people who did not speak conversational English (n=2) were excluded (as they would be unable to participate in the telephone interview).
Recruitment procedure
New Zealanders who have a traumatic accident present to health professionals who record their injury details with ACC, a government-owned corporation responsible for administering the country’s universal no-fault injury scheme. People who had an FTASD were identified through the use of an injury coding system (READ codes) (see online supplementary file S1).
bmjsem-2018-000447supp001.docx (18.2KB, docx)
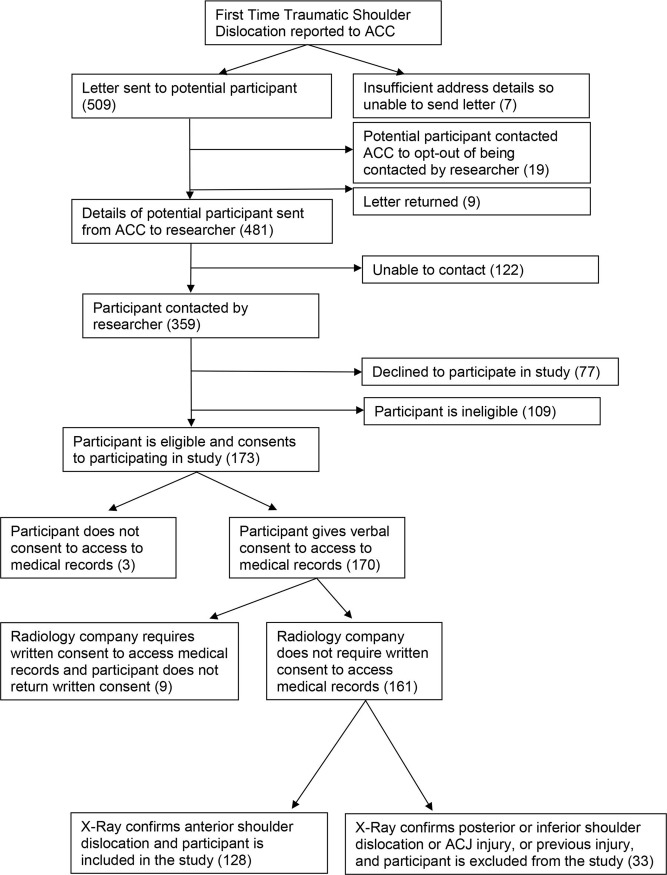
Eligible people with an FTASD were contacted by letter within 12 weeks of their dislocation by ACC with study information and a consent form (figure 1). They were given 2 weeks to opt out of the study. For those people who did not choose to opt out, contact details were forwarded to the primary researcher (MKO). Those people were then contacted by telephone. They were informed again about the study, had an opportunity to ask any questions and details of the shoulder injury were discussed to confirm a shoulder dislocation. Those who were eligible, who wished to take part in the study and permitted access to radiology records were consented into the study.
Figure 1.
Flow of participants. ACC, Accident Compensation Corporation; ACJ, acromioclavicular joint.
Participant involvement
People who have had a shoulder dislocation often ask health professionals for information regarding the likelihood of further instability events. People with FTASD were not involved in setting the research question or study design. They were included in the development of the tool to be tested. Dissemination to participants will take the form of an email summarising the main results.
Data collection
Baseline data
Following consent and inclusion in the study, participants could complete the beta version of the tool verbally over the phone, online via an internet hosted version (URL link provided by email) or a using a paper version that was posted. The beta version of the tool recorded participant’s primary predictive variables including age, gender, height, weight, ethnicity, hand dominance, side of dislocation, occupation, family history of instability, self-reported hypermobility, period of immobilisation and number of physiotherapy sessions attended after their injury (table 1). Operational definitions of these variables are provided in the online supplementary file. Ethnicity was categorised as per NZ Statistics31 with up to six ethnic categories recorded and the minority ethnicity coded if the alternate was NZ European. Mechanism of injury was categorised as sports injuries, motor vehicle accidents (MVA), assault, fall or other.12 Falls that occurred during sporting activities were classified as sports injuries.
Table 1.
Variables obtained from initial contact with participants
| Demographic | Clinical | Sport | Secondary variables |
| Age | Radiograph | Level of sport | Quality of life (WOSI) |
| Gender | Bony Bankart | Position played sport | Pain and function (SPADI) |
| Patient’s estimated height | Greater tuberosity fracture | Hours per week | Fear of reinjury (TSK-11) |
| Patient’s estimated weight | Hill-Sachs | Time to return to sport | Shoulder Activity Scale (SAS) |
| Hand dominance | US—rotator cuff tear | Type of sport (collision vs overhead) | |
| Side affected | US—bursitis | ||
| Occupation | US—haemarthrosis | ||
| Ethnicity | Apprehension | ||
| Family history | |||
| Hypermobility | |||
| Period of immobilisation | |||
| Physiotherapy sessions |
SPADI, Shoulder Pain and Disability Index; TSK-11, Tampa Scale of Kinesiophobia; US, ultrasonography; WOSI, Western Ontario Stability Index.
Secondary variables such as quality of life, level of shoulder activity, shoulder function and fear of reinjury were measured with the Western Ontario Stability Index (WOSI),32 Shoulder Activity Scale (SAS),33 Shoulder Pain and Disability Index (SPADI)34 and Tampa Scale of Kinesiophobia (TSK-11),35 respectively (table 1). Radiology records were reviewed to confirm an anteriorly directed shoulder dislocation and to confirm the presence of associated bony pathology. Radiology records that confirmed a dislocation in a direction that was not anterior or confirmed ACJ disruption or clavicle fracture resulted in participant exclusion. Those participants whose shoulder was reduced prior to radiograph and showed no evidence of another shoulder pathology or posterior/inferior dislocation were included in the study.
Follow-up data
Follow-up phone calls were made at 3, 6, 9 and 12 months following the date of injury, by research assistants blinded to baseline variables to limit recall and experimenter bias. When the participants preferred to be contacted by email, they were emailed with a link to the online version of the tool.
The primary outcome was recurrent instability of the previously dislocated shoulder. Recurrent instability was defined as a repeated event of instability of either a subluxation or dislocation.6 A dislocation was defined as complete separation of the humeral head from the articular surface of the glenoid and required external force to relocate the shoulder.36 37 A subluxation was defined as spontaneous reduction of the humeral head following complete separation of the humeral head from the glenoid without the requirement of external force.36 37 Research assistants with a health background were trained to identify recurrent instability events (see online supplementary file S2), and discussions of individual cases were undertaken at regular meetings to reach a consensus when there was uncertainty regarding the instability event.
Follow-up was limited to 1 year to examine the immediate impact of an FTASD. Some studies38 39 have advocated primary surgical intervention in this population of people following an FTASD, which would occur within the 12 months’ time frame. One-year follow-up was used to study the shorter term impact of an FTASD as approximately 70% of all dislocations that occur take place within 12 months.12 Additionally, this study was designed to elucidate variables which can be used to predict recurrent instability for the development of a multivariate prediction tool. It was not envisaged that these variables would alter beyond the first year of follow-up.
Sample size
The study was powered at 90% with a sample size of 84 participants and alpha at 0.05 to observe a recurrence rate as found by Robinson et al 12; 50% from ages 15 to 20, and 21–25, and a 25% recurrence rate for age groups 26–30, 31–35 and 36–40 years (online supplementary file S3). It was anticipated that 50% of patients would drop out of the study as the population is young and mobile. Therefore, a minimum of 127 participants were required for recruitment.
Data and statistical analysis
Data were analysed using Statistical Package for the Social Sciences software (SPSS V.24.0, IBM). Univariate logistic regression models were used to identify the risk factors predictive of recurrent shoulder instability (p<0.05). Multivariate logistic regression models used to identify the combined effect of variables for recurrent instability which were selected for using backwards selection (p<0.10). This lower cut-off is the statistical threshold used to identify when variables should be retained in a multivariate model (when other variables are being adjusted for).40 Coefficients for those variables retained in the multivariate model were used to develop the predictive tool.41 42
Results
Recruitment and participant demographics
One hundred and twenty-eight participants (110 males) were recruited from May 2015 to February 2016 (figure 1). Forty-nine (38.3%) participants were aged between 16 and 20 years, 30 (23.4%) between 21 and 25 years, 18 (14.1%) between 26 and 30 years, 17 (13.3%) between 31 and 35 years and 14 (10.9%) between 36 and 40 years. Baseline outcomes for demographic variables and secondary outcome measures are displayed in table 2. The rate of recurrent instability was 35.9% (46/128) at 1 year follow-up with the greatest recurrence in those aged 16–25 (figure 2). Fourteen per cent (18/128) of participants were lost to follow-up and 50% (64/128) of participants did not have recurrent instability.
Table 2.
Descriptive data of continuous variables
| n | Minimum | Maximum | Mean | SD | |
| Age (years) | 128 | 16 | 40 | 24.63 | 7.10 |
| Height (cm) | 127 | 154 | 198 | 179.00 | 8.71 |
| Weight (kg) | 128 | 50 | 128 | 82.95 | 16.31 |
| Body mass index | 127 | 18 | 41 | 25.72 | 4.41 |
| SPADI-Total | 128 | 0 | 89 | 18.41 | 17.30 |
| SPADI-Pain | 128 | 0 | 76 | 15.77 | 15.38 |
| SPADI-Function | 128 | 0 | 93 | 15.33 | 17.68 |
| TSK-11 | 128 | 16 | 37 | 26.74 | 3.88 |
| WOSI-Total | 128 | 0 | 166 | 78.16 | 46.31 |
| WOSI-Physical | 128 | 0 | 80 | 33.44 | 20.84 |
| WOSI-Life | 128 | 0 | 39 | 16.46 | 10.73 |
| WOSI-Recreation | 128 | 0 | 35 | 13.27 | 10.46 |
| WOSI-Emotion | 128 | 0 | 30 | 14.95 | 8.28 |
SPADI, Shoulder Pain and Disability Index; TSK-11, Tampa Scale of Kinesiophobia; WOSI, Western Ontario Stability Index.
Figure 2.
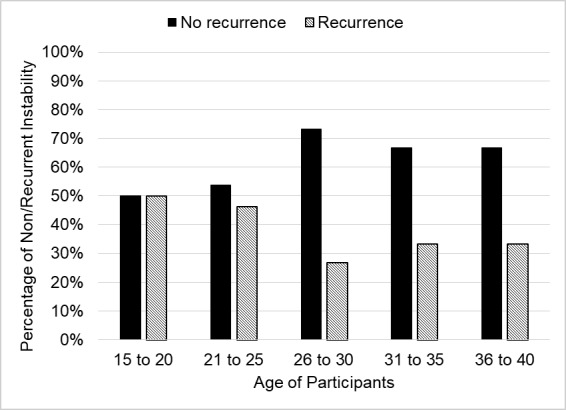
Rate of recurrent shoulder instability.
There were 110 (85.9%) right-hand dominant participants, and the right shoulder was affected in 72 (56.3%) participants. The dominant limb was affected in 63 (49.2%) participants. The predominant ethnicity of the participants was NZ European (70; 54.6%), followed by NZ Māori (19; 14.8%), Pasifika (15; 11.7%) and European Other (13; 10.2%) (online supplementary file S4). This is similar to the distribution of ethnicity in NZ.43
There were 51 (39.8%) manual workers and 77 (60.2%) sedentary workers. There were 35 (27.3%) participants who participated in occupations above shoulder height, while 93 (72.7%) participants were involved in occupations at shoulder height or below. There were 22 (17.2%) participants with a family history of shoulder dislocation and 105 (82.2%) participants who did not have a family history of shoulder dislocation (one data set missing). Thirty-one (24.2%) participants self-reported generalised hypermobility. The majority of participants (103; 80.5%) were immobilised following the dislocation, 24 (18.8%) were not immobilised and one participant did not recall their immobilisation status. Most participants (92; 71.9%) had received physiotherapy treatment while 35 (27.3%) had not, and one did not recall.
The most common mechanism of the first anterior shoulder dislocation was a sports injury (95; 74.2%), followed by a fall (13; 10.1%), other mechanism (12; 9.3%), MVA (4; 3.1%) and assault (4; 3.1%). Because of the small number of MVAs and large variance, they were grouped with ‘other’ for univariate analysis. There were 33 (25.8%) participants whose injury was not sport related. Of the 95 (74.2%) participants whose injury was sports related, 87 (91.6%) were recreational athletes and 8 (8.4%) were semiprofessional or professional. Of the 95 participants who identified a sports injury, 52 (54.7%) were involved in contact sport, 25 (26.3%) were involved in limited contact sports and 18 (18.9%) were involved in non-contact sports, as classified by Rice.44 At the time of injury, 38 of the 52 (73.1%) participants reporting contact injury were involved in collision sports. Rugby union, football, towed water sports and skateboarding all had a rate of recurrent instability of 50% or above. With regard to pathological injuries, there were 2 (1.6%) greater tuberosity fractures, 13 (10.2%) bony Bankart lesions and 36 (28.1%) Hill-Sachs lesions.
Recurrent instability
At 12 months following their injury, 46 (35.9%) participants had an episode of recurrent instability, 64 (50.0%) participants had no episode of instability and 18 (14.1%) participants were lost to follow-up.
Univariate analysis
The relationship between the variables and recurrent instability is displayed in table 3. Significant univariate baseline predictors (p≤0.05) of recurrence at 12 months were: bony Bankart lesion; not being immobilised; total scores for SPADI, SAS, TSK-11, and WOSI total score; ethnicity of not European Other, two subsections of the WOSI (Physical and Emotion) and the SPADI-Function score.
Table 3.
Univariate analysis of variables which predict recurrent instability
| Regression coefficient | SE | P value | OR | 95% CI | |
| Bony Bankart† | 1.29 | 0.64 | 0.04 | 3.65 | 1.05 to 12.70 |
| Hill-Sachs lesion | 0.37 | 0.43 | 0.38 | 1.45 | 0.63 to 3.35 |
| Age | −0.05 | 0.03 | 1.07 | 0.96 | 0.90 to 1.10 |
| 16–20 versus other | −0.54 | 0.40 | 0.17 | 0.58 | 0.27 to 1.27 |
| 21–26 versus other | −0.23 | 0.45 | 0.61 | 0.79 | 0.33 to 1.92 |
| 26–30 versus other | 0.78 | 0.62 | 0.21 | 2.18 | 0.65 to 7.34 |
| 31–35 versus other | 0.42 | 0.59 | 0.48 | 1.52 | 0.48 to 4.79 |
| 36–40 versus other | 0.41 | 0.65 | 0.53 | 1.50 | 0.42 to 5.32 |
| 16–25 versus other† | 0.74 | 0.41 | 0.07 | 2.10 | 0.94 to 4.72 |
| Gender | −0.16 | 0.61 | 0.79 | 0.85 | 0.36 to 3.84 |
| Height | −0.00 | 0.02 | 0.87 | 1.00 | 0.95 to 1.04 |
| Weight | 0.01 | 0.01 | 0.40 | 1.01 | 0.99 to 1.04 |
| BMI | 0.04 | 0.05 | 0.36 | 1.04 | 0.95 to 1.14 |
| Ethnicity | |||||
| Asian | −0.05 | 0.79 | 0.95 | 0.96 | 0.20 to 4.50 |
| European Other† | −1.63 | 0.79 | 0.04 | 5.08 | 1.08 to 23.92 |
| NZ European | −0.38 | 0.39 | 0.33 | 0.68 | 0.32 to 1.48 |
| NZ Māori | 0.71 | 0.58 | 0.22 | 2.04 | 0.65 to 6.33 |
| Other | 0.34 | 1.43 | 0.81 | 1.40 | 0.09 to 22.98 |
| Pasifika | 0.41 | 0.65 | 0.53 | 1.50 | 0.42 to 5.32 |
| Ethnic group: Other versus NZ Euro/NZ Māori/Pasifika* | −0.88 | 0.52 | 0.09 | 0.415 | 0.149 to 1.152 |
| Limb side | |||||
| Dominance | −0.98 | 0.69 | 0.16 | 0.38 | 0.10 to 1.46 |
| Side affected | −0.47 | 0.40 | 0.23 | 0.62 | 0.29 to 1.35 |
| Dominant affected* | 0.63 | 0.39 | 0.10 | 1.877 | 0.87 to 4.06 |
| Occupation | |||||
| Manual sedentary | 0.30 | 0.40 | 0.46 | 1.34 | 0.62 to 2.94 |
| Overhead below shoulder | 0.55 | 0.44 | 0.21 | 0.58 | 0.25 to 1.36 |
| Family history | 0.07 | 0.51 | 0.90 | 1.07 | 0.40 to 2.87 |
| Hypermobile | 0.49 | 0.45 | 0.27 | 0.61 | 0.25 to 1.47 |
| Mechanism | |||||
| Sports | 0.06 | 0.44 | 0.90 | 1.06 | 0.45 to 2.52 |
| Assault | −0.34 | 1.02 | 0.74 | 0.71 | 0.10 to 5.23 |
| Other/MVA | 0.67 | 0.63 | 0.29 | 0.54 | 0.15 to 1.76 |
| Falls | −0.81 | 0.68 | 0.23 | 0.44 | 0.12 to 1.68 |
| Immobilised† | −0.97 | 0.48 | 0.05 | 0.38 | 0.15 to 0.98 |
| Physiotherapy | 0.25 | 0.43 | 0.56 | 0.78 | 0.33 to 1.81 |
| Sport | |||||
| Contact versus other | −0.74 | 0.47 | 0.11 | 0.48 | 0.19 to 1.19 |
| Collision versus other | −0.69 | 0.46 | 0.13 | 0.50 | 0.20 to 1.23 |
| Limited contact versus other* | −0.97 | 0.58 | 0.09 | 0.38 | 0.12 to 1.17 |
| Non-contact versus other | 0.07 | 0.58 | 0.90 | 1.08 | 0.34 to 3.37 |
| Sports professional/recreation | −0.40 | 1.03 | 0.70 | 0.67 | 0.09 to 5.04 |
| SAS contact Y/N* | 0.72 | 0.40 | 0.07 | 2.05 | 0.94 to 4.46 |
| OH versus non-OH | −0.33 | 0.50 | 0.51 | 0.72 | 0.27 to 1.90 |
| Global rate of change | −0.02 | 0.01 | 0.18 | 0.98 | 0.96 to 1.01 |
| SAS† | 0.13 | 0.06 | 0.03 | 1.13 | 1.01 to 1.27 |
| Pain-Initial | 0.03 | 0.07 | 0.71 | 1.03 | 0.90 to 1.17 |
| Pain-Now | 0.15 | 0.11 | 0.15 | 1.16 | 0.95 to 1.43 |
| SPADI-Total† | 0.03 | 0.01 | 0.02 | 1.03 | 1.01 to 1.06 |
| SPADI-Pain* | 0.03 | 0.01 | 0.06 | 1.03 | 1.00 to 1.05 |
| SPADI-Function† | 0.04 | 0.02 | 0.01 | 1.04 | 1.01 to 1.07 |
| TSK-11† | 0.12 | 0.06 | 0.04 | 1.12 | 1.01 to 1.26 |
| WOSI-Total† | 0.01 | 0.01 | 0.05 | 1.01 | 1.00 to 1.02 |
| WOSI-Physical† | 0.02 | 0.01 | 0.03 | 1.02 | 1.00 to 1.04 |
| WOSI-Life* | 0.03 | 0.02 | 0.10 | 1.03 | 0.99 to 1.08 |
| WOSI-Recreation | 0.01 | 0.02 | 0.69 | 1.01 | 0.97 to 1.05 |
| WOSI-Emotion† | 0.07 | 0.03 | 0.01 | 1.07 | 1.02 to 1.13 |
*Significant at p≤0.10.
†Significant at p≤0.05.
BMI, body mass index; MVA, motor vehicle accident; NZ, New Zealand; non-OH, non-overhead sport; OH, overhead sport; SAS, Shoulder Activity Scale; SPADI, Shoulder Pain and Disability Index; TSK-11, Tampa Scale of Kinesiophobia; WOSI, Western Ontario Stability Index.
Multivariate analysis
Results of the multivariate analysis using backwards stepwise regression are tabled (table 4). Variables shown were retained in the model if p<0.10, even after adjusting for other significant risk factors of recurrent instability. Risk of recurrence at 12 months was predicted using both physical and psychosocial factors in the following equation:
Table 4.
Multivariate analysis of variables which predict recurrent instability
| Regression coefficient | SE | P value | OR | 95% CI | |
| Bony Bankart* | 1.798 | 0.746 | 0.016 | 6.040 | 1.40 to 26.062 |
| Ages16–25 versus other† | 1.062 | 0.482 | 0.028 | 2.892 | 1.124 to 7.439 |
| Dominant affected* | 0.801 | 0.454 | 0.077 | 2.227 | 0.916 to 5.418 |
| Immobilised† | −1.270 | 0.571 | 0.026 | 0.281 | 0.092 to 0.859 |
| SPADI-Total† | 0.033 | 0.015 | 0.031 | 1.034 | 1.003 to 1.066 |
| TSK-11† | 0.133 | 0.071 | 0.061 | 1.142 | 0.994 to 1.313 |
| Constant | 0.061 | 1.142 | 0.016 | 0.009 |
*Significance at p≥0.05.
†Significance at p≥0.10.
SPADI, Shoulder Pain and Disability Index;TSK-11, Tampa Scale of Kinesiophobia.
Risk of recurrence=−4.73 + 1.06 × (ages 16–25 years)+1.80 × (bony Bankart lesions)+0.80 × (dominant side affected) − 1.27 × (immobilised) +0.03 × (SPADI-Total)+0.13 × (TSK-11-Total).
Discussion
We present the first prospective cohort study to report an association between fear of injury and self-reported pain and function with recurrent shoulder instability. We report a positive relationship between psychosocial factors and self-reported pain and function near the time of injury, with recurrent shoulder instability following an FTASD. Psychosocial variables are common sequelae of an FTASD.45 However, in this population, fear of reinjury and self-reported pain and disability also identified those most at risk of further instability events at 12-month follow-up.
Variables associated with recurrent instability
We extend previous findings12 46 to highlight that being aged between 16 and 25 years was associated with increased rates of recurrent instability. While not statistically significant as a stand-alone variable in univariate analysis (p=0.07), age was a statistically significant risk factor (p=0.03) after adjusting for other variables.
Our study examined demographic risk factors of sex and limb dominance. While one author12 found male sex to be related to recurrent instability, our current study agreed with others,10 47 in that sex was not associated with recurrent instability following multivariate analysis. We believe that playing contact sport and the age of the participant may have confounded the influence of sex in that young males are more involved in contact sport in NZ than young females.48 Additionally, use of the dominant limb in both daily and high-risk activities may explain why participants who injured their non-dominant shoulder were less likely to have recurrent instability (p=0.10). In the presence of other variables, dislocation to the non-dominant limb trended towards significance (p=0.07). This may be related to the amount of use of the affected limb. However, this study was not sufficiently powered to examine the influence of shoulder activity on limb dominance on recurrent instability.
This study found that the presence of a bony Bankart lesion was associated with recurrent shoulder instability. In contrast, Salomonsson et al 17 found bony Bankart lesions to be a prognostic indicator for shoulder stability. Salomonsson et al 17 excluded participants with large bony Bankart lesions, thus biasing their sample. This study shows that patients with any sized bony Bankart lesion are more likely to have recurrent instability. The large variance in this study could result from dichotomising the size of bony Bankart lesions to present or absent.
The presence of a Hill-Sachs lesion was not significantly associated with recurrent instability, in line with other authors’ findings.11 17 This is in contrast to findings of a previous study16 and may be because of heterogeneity of pathological Hill-Sachs lesions. In our study, radiological examination was undertaken by a number of radiologists who were not consistent in the way they reported the size, shape, location or interaction of bony lesions. Further analysis of Hill-Sachs and bony Bankart lesions was not possible because of variations in the way this lesions were reported. While our study was not sufficiently powered to examine the relationship between greater tuberosity fractures and recurrent instability, others have reported that these decrease the risk.9 11 12 16 47
Immobilisation of the limb following a shoulder dislocation was found to decrease the risk of recurrent instability at 1 year follow-up. The number of days patients were immobilised ranged from 1 to 70 days and was not associated with recurrent shoulder instability. Itoi et al 49 reported decreased recurrence when the shoulder was immobilised in external rotation. However, more recent systematic reviews50 51 have failed to support the finding of Itoi and colleagues, and may be due to the effect of regional culture and healthcare systems. All participants in the current study who were immobilised were in a sling across the body and there was a significant association with decreased rates of recurrent instability.
This is one of the first studies to examine the ability of shoulder outcome measures to predict recurrent instability. All the questionnaires used (SAS, SPADI, TSK-11 and WOSI) were associated with recurrent instability. This finding illustrates the multifactorial nature of recurrent shoulder instability and the influence of patient beliefs, level of activity, fear of reinjury and self-reported pain and function as predictors of recurrent instability. Shoulder pain, function and quality of life are common sequelae of an FTASD. This study found that these variables are consequences of an FTASD, and predict future recurrent instability events.
Current non-surgical management appeared to be effective for over 60% of those who report with an FTASD at 12-month follow-up. Addressing factors such as patient education, psychosocial factors such as fear of injury and developing criteria for return to sport/work after a dislocation could further improve non-surgical management.
Limitations
We note several limitations. The outcome of recurrent instability was self-reported and was not validated with a follow-up radiograph. The requirement for radiograph to confirm a dislocation would have excluded subluxation events from the outcome of recurrent instability. However, categorising recurrent instability based on participants’ self-report may have influenced the results, particularly in the context of the ability of self-reported questionnaires to predict self-reported instability.
Conclusions
This prospective cohort study reports the rate of recurrent instability in NZ within 1 year of an FTASD. It is the first prospective cohort study to report an association between fear of injury and self-reported pain and function with recurrent shoulder instability. The findings that a bony Bankart lesion, ages between 16 and 25, dislocation of the dominant shoulder, not being immobilised and higher SPADI and TSK-11 scores can be used to predict recurrent instability will now be tested in a separate population to examine its predictive validity and reliability.
What are the findings?
A multivariate tool of age, bony Bankart lesion, immobilisation status, dominance of affected shoulder, fear of reinjury and pain and disability can be used to predict recurrent shoulder instability at 1 year.
How might it impact on clinical practice in the future?
Clinical tools can improve clinical decision-making.
Clinical tool such as this can be used for shared decision-making with patients regarding the likelihood of further episodes of recurrent instability given their patient-specific factors.
Acknowledgments
We acknowledge the work of Nitika Kumari, Alicia Beck, Tara George, Ema Tokolahi and Dave Beattie for their research assistance.
Footnotes
Contributors: MKO designed the study, collected the data, designed the statistical analysis, analysed the data and drafted and revised the paper. RE and PK monitored data collection, assisted with methods development, and helped draft and revise the manuscript. PP assisted with statistical design and data analysis.
Funding: We thank NZ Manipulative Physiotherapy Association, Shoulder Elbow Physiotherapy Australasia, Sports Medicine New Zealand, Physiotherapy New Zealand-Auckland Branch and Auckland University of Technology for their financial assistance.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Auckland University of Technology (14/256) and Accident Compensation Corporation (No 272) ethics committees.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data sharing statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1. Leroux T, Wasserstein D, Veillette C, et al. . Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med 2014;42:442–50. 10.1177/0363546513510391 [DOI] [PubMed] [Google Scholar]
- 2. Owens BD, Agel J, Mountcastle SB, et al. . Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med 2009;37:1750–4. 10.1177/0363546509334591 [DOI] [PubMed] [Google Scholar]
- 3. te Slaa RL, Wijffels MPJM, Brand R, et al. . The prognosis following acute primary glenohumeral dislocation. J Bone Joint Surg Br 2004;86:58–64. 10.1302/0301-620X.86B1.13695 [DOI] [PubMed] [Google Scholar]
- 4. Postacchini F, Gumina S, Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elbow Surg 2000;9:470–4. 10.1067/mse.2000.108385 [DOI] [PubMed] [Google Scholar]
- 5. Murray IR, Ahmed I, White NJ, et al. . Traumatic anterior shoulder instability in the athlete. Scand J Med Sci Sports 2013;23:387–405. 10.1111/j.1600-0838.2012.01494.x [DOI] [PubMed] [Google Scholar]
- 6. Olds M, Ellis R, Donaldson K, et al. . Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta-analysis. Br J Sports Med 2015;49:913–22. 10.1136/bjsports-2014-094342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Olds M, Donaldson K, Ellis R, et al. . In children 18 years and under, what promotes recurrent shoulder instability after traumatic anterior shoulder dislocation? A systematic review and meta-analysis of risk factors. Br J Sports Med 2016;50:1135–41. 10.1136/bjsports-2015-095149 [DOI] [PubMed] [Google Scholar]
- 8. Wasserstein DN, Sheth U, Colbenson K, et al. . The true recurrence rate and factors predicting recurrent instability after nonsurgical management of traumatic primary anterior shoulder dislocation: a systematic review. Arthroscopy 2016;32:2616–25. 10.1016/j.arthro.2016.05.039 [DOI] [PubMed] [Google Scholar]
- 9. Vermeiren J, Handelberg F, Casteleyn PP, et al. . The rate of recurrence of traumatic anterior dislocation of the shoulder. A study of 154 cases and a review of the literature. Int Orthop 1993;17:337–41. [DOI] [PubMed] [Google Scholar]
- 10. Sachs RA, Lou SM, Paxton E, et al. . Can the Need for Future Surgery for Acute Traumatic Anterior Shoulder Dislocation Be Predicted ? Can the Need for Future Surgery for Acute Traumatic Anterior Shoulder Dislocation Be Predicted? J Bone Jt Surg Am 2007;89:1665–74. [DOI] [PubMed] [Google Scholar]
- 11. Hoelen MA, Burgers AM, Rozing PM, et al. . Prognosis of primary anterior shoulder dislocation in young adults. Arch Orthop Trauma Surg 1990;110:51–4. 10.1007/BF00431367 [DOI] [PubMed] [Google Scholar]
- 12. Robinson CM, Howes J, Murdoch H, et al. . Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am 2006;88:2326–36. 10.2106/JBJS.E.01327 [DOI] [PubMed] [Google Scholar]
- 13. Parr J, Borsa P, Fillingim R, et al. . Psychological influences predict recovery following exercise induced shoulder pain. Int J Sports Med 2014;35:232–7. 10.1055/s-0033-1345179 [DOI] [PubMed] [Google Scholar]
- 14. Bot SDM, van der Waal JM, Terwee CB, et al. . Predictors of outcome in neck and shoulder symptoms: a cohort study in general practice. Spine 2005;30:E459–70. [DOI] [PubMed] [Google Scholar]
- 15. Lentz TA, Barabas JA, Day T, et al. . The relationship of pain intensity, physical impairment, and pain-related fear to function in patients with shoulder pathology. J Orthop Sports Phys Ther 2009;39:270–7. 10.2519/jospt.2009.2879 [DOI] [PubMed] [Google Scholar]
- 16. Kralinger FS, Golser K, Wischatta R, et al. . Predicting recurrence after primary anterior shoulder dislocation. Am J Sports Med 2002;30:116–20. 10.1177/03635465020300010501 [DOI] [PubMed] [Google Scholar]
- 17. Salomonsson B, von Heine A, Dahlborn M, et al. . Bony Bankart is a positive predictive factor after primary shoulder dislocation. Knee Surg Sports Traumatol Arthrosc 2010;18:1425–31. 10.1007/s00167-009-0998-3 [DOI] [PubMed] [Google Scholar]
- 18. Pevny T, Hunter RE, Freeman JR. Primary traumatic anterior shoulder dislocation in patients 40 years of age and older. Arthroscopy 1998;14:289–94. 10.1016/S0749-8063(98)70145-8 [DOI] [PubMed] [Google Scholar]
- 19. Steyerberg EW, Moons KGM, van der Windt DA, et al. . Prognosis research strategy (progress) 3: prognostic model research. PLoS Med 2013;10:e1001381 10.1371/journal.pmed.1001381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Federer AE, Taylor DC, Mather RC. Using evidence-based algorithms to improve clinical decision making: the case of a first-time anterior shoulder dislocation. Sports Med Arthrosc Rev 2013;21:155–65. 10.1097/JSA.0b013e31829f608c [DOI] [PubMed] [Google Scholar]
- 21. Benning TM, Kimman ML, Dirksen CD, et al. . Combining individual-level discrete choice experiment estimates and costs to inform health care management decisions about customized care: the case of follow-up strategies after breast cancer treatment. Value Health 2012;15:680–9. 10.1016/j.jval.2012.04.007 [DOI] [PubMed] [Google Scholar]
- 22. Balg F, Boileau P. The instability Severity Index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470–7. 10.1302/0301-620X.89B11.18962 [DOI] [PubMed] [Google Scholar]
- 23. Piasecki DP, Verma NN, Romeo AA, et al. . Glenoid bone deficiency in recurrent anterior shoulder instability: diagnosis and management. J Am Acad Orthop Surg 2009;17:482–93. 10.5435/00124635-200908000-00002 [DOI] [PubMed] [Google Scholar]
- 24. Emond M, Le Sage N, Lavoie A, et al. . Clinical factors predicting fractures associated with an anterior shoulder dislocation. Acad Emerg Med 2004;11:853–8. [DOI] [PubMed] [Google Scholar]
- 25. Bishop JA, Crall TS, Kocher MS. Operative versus nonoperative treatment after primary traumatic anterior glenohumeral dislocation: expected-value decision analysis. J Shoulder Elbow Surg 2011;20:1087–94. 10.1016/j.jse.2011.01.031 [DOI] [PubMed] [Google Scholar]
- 26. Crall TS, Bishop JA, Guttman D, et al. . Cost-effectiveness analysis of primary arthroscopic stabilization versus nonoperative treatment for first-time anterior glenohumeral dislocations. Arthroscopy 2012;28:1755–65. 10.1016/j.arthro.2012.05.885 [DOI] [PubMed] [Google Scholar]
- 27. Mather RC, Orlando LA, Henderson RA, et al. . A predictive model of shoulder instability after a first-time anterior shoulder dislocation. J Shoulder Elbow Surg 2011;20:259–66. 10.1016/j.jse.2010.10.037 [DOI] [PubMed] [Google Scholar]
- 28. Ahmed I, Ashton F, ChB M, et al. . Arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability functional outcomes and identification of risk factors for recurrence. [DOI] [PubMed]
- 29. Calvo E, Granizo JJ, Fernández-Yruegas D. Criteria for arthroscopic treatment of anterior instability of the shoulder: a prospective study. J Bone Joint Surg Br 2005;87:677–83. 10.1302/0301-620X.87B5.15794 [DOI] [PubMed] [Google Scholar]
- 30. van Kampen DA, van den Berg T, van der Woude HJ, et al. . Diagnostic value of patient characteristics, history, and six clinical tests for traumatic anterior shoulder instability. J Shoulder Elbow Surg 2013;22:1310–9. 10.1016/j.jse.2013.05.006 [DOI] [PubMed] [Google Scholar]
- 31. Ministry of Health Ethnicity data protocols for the health and disability sector, 2004. [Google Scholar]
- 32. Kirkley A, Griffin S, McLintock H, et al. . The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. Am J Sports Med 1998;26:764–72. 10.1177/03635465980260060501 [DOI] [PubMed] [Google Scholar]
- 33. Brophy RH, Beauvais RL, Jones EC, et al. . Measurement of shoulder activity level. Clin Orthop Relat Res 2005;439:101–8. 10.1097/01.blo.0000173255.85016.1f [DOI] [PubMed] [Google Scholar]
- 34. Roach KE, Budiman-Mak E, Songsiridej N, et al. . Development of a shoulder pain and disability Index. Arthritis Care Res 1991;4:143–9. 10.1002/art.1790040403 [DOI] [PubMed] [Google Scholar]
- 35. Woby SR, Roach NK, Urmston M, et al. . Psychometric properties of the TSK-11: a shortened version of the Tampa scale for Kinesiophobia. Pain 2005;117:137–44. 10.1016/j.pain.2005.05.029 [DOI] [PubMed] [Google Scholar]
- 36. Owens LCBD, Nelson BJ, Duffey ML, et al. . Pathoanatomy of first-time, traumatic, anterior glenohumeral subluxation events. J Bone Jt Surg Am Vol 2010;92:1605–11. 10.2106/JBJS.I.00851 [DOI] [PubMed] [Google Scholar]
- 37. Rockwood CA, Matsen FA, Wirth CJ. The Shoulder. 2nd ed Philadephia: Saunders, 1998. [Google Scholar]
- 38. Marshall T, Vega J, Siqueira M, et al. . Outcomes after arthroscopic bankart repair: patients with first-time versus recurrent dislocations. Am J Sports Med 2017;45:1776–82. 10.1177/0363546517698692 [DOI] [PubMed] [Google Scholar]
- 39. Polyzois I, Dattani R, Gupta R, et al. . Traumatic first time shoulder dislocation: surgery vs non-operative treatment. Arch Bone Jt Surg 2016;4:104–8. [PMC free article] [PubMed] [Google Scholar]
- 40. Bursac Z, Gauss CH, Williams DK, et al. . Purposeful selection of variables in logistic regression. Source Code Biol Med 2008;3 10.1186/1751-0473-3-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Courville T, Thompson B. Use of structure coefficients in published multiple regression articles: β is not enough. Educ Psychol Meas 2001;61:229–48. 10.1177/0013164401612006 [DOI] [Google Scholar]
- 42. Kraha A, Turner H, Nimon K, et al. . Tools to support interpreting multiple regression in the face of multicollinearity. Front Psychol 2012;3:1–16. 10.3389/fpsyg.2012.00044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Statistics New Zealand 2013 Census - Major ethnic groups in New Zealand. infographic, 2015. Available: http://www.stats.govt.nz/Census/2013-census/profile-and-summary-reports/infographic-culture-identity.aspx [Accessed 8 Nov 2017].
- 44. Rice SG. Medical conditions affecting sports participation and the Council on sports medicine and fitness. Paediatrics 2008;121:841–8. [DOI] [PubMed] [Google Scholar]
- 45. Dickens JF, Owens BD, Cameron KL, et al. . Return to play and recurrent instability after In-Season anterior shoulder instability. Am J Sports Med 2014;42:2842–50. 10.1177/0363546514553181 [DOI] [PubMed] [Google Scholar]
- 46. Hovelius L, Augustini BG, Fredin H, et al. . Primary anterior dislocation of the shoulder in young patients. a ten-year prospective study. J Bone Joint Surg Am 1996;78:1677–84. 10.2106/00004623-199611000-00006 [DOI] [PubMed] [Google Scholar]
- 47. te Slaa RL, Brand R, Marti RK, et al. . A prospective arthroscopic study of acute first-time anterior shoulder dislocation in the young: a five-year follow-up study. J Shoulder Elbow Surg 2003;12:529–34. 10.1016/S1058-2746(03)00218-0 [DOI] [PubMed] [Google Scholar]
- 48. Sport New Zealand Sport and active recreation in the lives of New Zealand adults. 2013/2014 active new Zealand survey results, 2015. [Google Scholar]
- 49. Itoi E, Hatakeyama Y, Sato T, et al. . Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence. A randomized controlled trial. J Bone Joint Surg Am 2007;89:2124–31. 10.2106/JBJS.F.00654 [DOI] [PubMed] [Google Scholar]
- 50. Paterson WH, Throckmorton TW, Koester M, et al. . Position and duration of immobilization after primary anterior shoulder dislocation: a systematic review and meta-analysis of the literature. J Bone Jt Surg - Am Vol 2010;92:2924–33. [DOI] [PubMed] [Google Scholar]
- 51. Liu A, Xue X, Chen Y, et al. . The external rotation immobilisation does not reduce recurrence rates or improve quality of life after primary anterior shoulder dislocation: a systematic review and meta-analysis. Injury 2014;45:1842–7. 10.1016/j.injury.2014.06.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2018-000447supp001.docx (18.2KB, docx)