Abstract
Much research and attention has focused on addressing the extremes of the adolescent substance use spectrum: either the prevention of substance use prior to its onset or the treatment of those with a substance use disorder (SUD). Little research has looked at adolescents who fall mid-continuum. Adolescents who use substances in this mild-to-moderate range may be efficiently and cost-effectively treated using brief interventions based on cognitive-behavioral (CB) and motivational interviewing (MI) strategies. Accessibility and feasibility of providing interventions may also be enhanced by training parents in application of CB and MI principles. An innovative home-based brief intervention for parents whose children engaged in mild to moderate drug abuse was developed and evaluated using a quasi-experimental design. Participants were parents and their adolescent child from the 7-county metro area of Minneapolis-St. Paul, Minnesota. Decreased substance use and increased family cohesion were the predicted outcomes of the Home Base intervention. Results suggest decreased adolescent marijuana use frequency, decreased alcohol use disorder symptomology, and increased parental happiness with their adolescent child. Alcohol and tobacco use frequency were statistically unchanged. Baseline levels of drug use severity moderated the relation between intervention and outcomes. These findings support the potential utility of this approach and also indicate the need to further develop accessible and efficient interventions for mild to moderate SUD.
Keywords: Parents, Adolescent, Substance Use, Intervention, Family
1.0. Introduction
Despite a slight decline in overall adolescent substance use in the United States over the past two decades, drug and alcohol use is still common and has significant health consequences (Johnston, O’Malley, Bachman, & Schulenberg, 2008; Centers for Disease Control (CDC), 2015). The potential detrimental effects of alcohol and other drug use on adolescent behavior and brain development have been well documented (Casey, Jones, & Hare, 2008; Meier, et al., 2012; Squeglia, Jacobus, & Tapert, 2009). Use of alcohol and other drugs during adolescence is also a predictor of adult substance use disorder (SUD) (Hawkins et al., 1997).
There is an abundance of prevention programs and curricula aimed at deterring adolescents from initiating drinking or other drug use, including community and school based programs, e.g. Drug Abuse Resistance Education (Ringwalt et al., 1994), Life Skills Training (LST; Botvin, Griffin, Paul, & Macaulay, 2003), and Skills, Opportunities, And Recognition (SOAR; Hawkins, Catalano, Kosterman, Abbott & Hill, 1999). There are also numerous treatment options for SUD, varying widely in effectiveness, ranging from self-help groups to outpatient treatment to inpatient treatment, with most focusing on patients with higher severity of use. However, many adolescents experience problems associated with mild to moderate substance use (Levy & Williams, 2016), though caregivers may not yet be aware of the adolescent’s use or they may not know how to - or even if they should - address it.
Several obstacles deter families from seeking treatment options for mild to moderate substance use in adolescents, including the fact that mild to moderate use is typically less evident and parents may be unaware of use or the need for intervention (Williams, McDermitt, Bertrand, & Davis, 2003). Also, treatment programs for this level of severity are quite rare (Winters, Botzet, Dittel, Fahnhorst, & Nicolson, 2015) and health insurance policies might not provide adequate coverage or reimbursement to providers in the absence of a formal SUD diagnosis. The available options may be relatively inaccessible due to constraints of time, budget and travel. Further, the burden may be perceived as excessive when use patterns are not considered severe.
Brief interventions (BIs) have emerged as a reliable means for treating mild to moderate substance use (Carney & Myers, 2012; Tait & Hulse, 2003; Winters, Lee, Botzet, Fahnhorst, & Nicholson, 2014; Walton et al., 2010). Commonly, BIs incorporate cognitive-behavioral, psychoeducational, and motivational interviewing strategies. They often consist of one to four sessions, each lasting from 5 minutes to an hour, conducted by a trained counselor or provider in healthcare or clinical settings (Levy, Winters & Knight, 2011). The study presented here, however, took a less traditional approach in that it was adapted to be parent-led and implemented in the home. The aim was to test this primary research question: To what extent can a well-trained parent implement a BI to his or her teenager, who is in the early stages of drug use?
1.1. Premise for Current Study
The extant research literature supports the view that the great majority of parents overwhelmingly disapprove of drug use by their children (Allen et al., 2016; Fearnow, Chassin, Presson, & Sherman, 1998; Jackson, 2002; Kosterman et al., 2016; Steinberg, 2001). Parents also exert powerful positive influences (e.g., Nash, McQueen, & Bray, 2005; Barnes, Hoffman, Welte, Farrell, & Dintcheff, 2006). In particular, parents have a unique role in enforcing family norms with respect to adolescent drug use (Bronte-Tinkew, Moore & Carrano, 2006; Foley, Altman, Durant, & Wolfson, 2004; Van der Vorst, Engels, Meeus, & Dekovic, 2006). Studies have shown that strong parent-adolescent bonds reduce the likelihood of adolescent drug use (Burdzovic Andreas, Pape & Bretteville-Jensen, 2016; Van Ryzin, Fosco, & Dishion, 2012). Similarly, authoritative parenting styles (Calafat et al., 2014) and parenting topics such as communication, rule setting, monitoring, and guided experience (Clark Shamblen, Ringwalt & Hanley, 2012; Lamb & Crano, 2014; Siegel, Tan, Navarro, Alvaro & Crano, 2015; Stone, Becker, Huber & Catalano, 2012; Vermeulen-Smit, Verdurmen, Engels & Vollebergh, 2015) have been shown to influence children’s internalization of parents’ beliefs, values, attitudes, and health behaviors, including those concerning drug use. Moreover, family-based interventions have been reported to be effective for improving parenting self-efficacy (Hogue & Liddle, 2009). These programs offer parents a well-defined way to talk to their children about substance use as well as the skills to improve overall family communication and interaction (Bertrand et al, 2013; Booth & Kwiatkowski, 1999; Liddle, Rowe, Dakof, Ungaro, & Henderson, 2004; Plant & Panzarella, 2009; Yatchmenoff, 2005).
However, studies have shown that simply communicating with a teenager about the possible dangers of drug use is insufficient as a protective measure (e.g., Nonnemaker, Silber-Ashley, Farrelly & Dench, 2012) and that tepid or ambivalent communication can actually increase risk (Center for Behavioral Health Statistics and Quality, 2017). Also, parents are prone to complacency regarding drug-specific socialization during childhood or naively provide certain forms of pro-use socialization, such as expressing permissive attitudes or inadequate monitoring of substance use (e.g., Clark et al., 2012; Jackson, 2002), and it is unlikely that parents routinely engage in any formal type of home-based intervention when they learn that their adolescent has already begun to use drugs (Jackson, 2002).
Teaching parents to deliver an adolescent-friendly and effective BI has the potential to encourage and support their motivation to respond to teenage drug use and to affect change in their son or daughter. Parent-led Bis also address common service barriers including accessibility and financial burden. Preventive interventions to address early-stage adolescent drug involvement are not typically reimbursed by health insurance programs, and such programs are rare in most local community mental health service systems, where it is mostly the case that an adolescent meet criteria for a severe substance use disorder in order to be eligible for services.
Some research literature suggests that motivated parents can influence the health behaviors of their children. An ongoing longitudinal project showed that parents who held negative health beliefs about smoking revealed more “parental activism” (as measured by expressing more negatives toward smoking and greater monitoring of the child’s smoking behavior) which in turn was linked to reduced smoking by the child at home (Fearnow et al., 1998). Similarly, a research study testing a parent-led, home-based anti-smoking program was conducted by Jackson and Dickinson in 2003. That study examined tobacco-specific attitudes, behaviors, and prevention techniques within households in which at least one parent was a smoker. Three-month outcome data from the randomized controlled trial (RCT) showed that parents in the active condition (compared to parents in the control condition) reported significantly higher levels of self-efficacy to prevent smoking in the adolescent, greater engagement in tobacco-specific media literacy, more use of social contracts, and more instances of reinforcing their teenager to stay smoke-free. At the 3-year outcome point, adolescents in the treatment group reported significantly lower smoking initiation compared to the control adolescents (12% vs 19%, respectively; Jackson & Dickinson, 2006).
To summarize, the scientific premise for the Home Base program is supported by theory and empirical literature: 1) parents have an advantageous opportunity to edify vital behavioral skills and anti-drug attitudes in their adolescent and to provide continuous influences in terms of family norms and expectations during multiple teachable moments; 2) even in the face of strong developmental forces of individuation and separation during adolescence, parents maintain a key socializing influence on their adolescent’s attitudes and behaviors about drug use; and 3) a BI program can readily dovetail with parenting practices that the literature suggests can address adolescent health behaviors and attitudes (e.g., Hawkins et al., 1997; Jaccard et al. 2005). These considerations support the view that parents are important agents of change for their adolescent’s health when provided with suitable and usable information, tools, and resources.
Components of the Home Base program described here address the multiple obstacles to receiving treatment for mild to moderate substance use and capitalize on the influence and support of parents. Research goals were to: 1) teach parents the program curriculum and coach their delivery of the material to their adolescent child within the comforts of their own home; 2) decrease the frequency and severity of adolescent substance use; and 3) improve family cohesion.
2.0. Method
2.1. Home Base Program
2.1.1. Parent objectives.
The program was intended to empower parents to 1) increase knowledge of psychosocial factors that maintain and halt adolescent drug involvement; 2) strengthen parental communication skills; 3) improving parental monitoring of the adolescent’s adherence to and promoters of a drug-free lifestyle; 4) increase parental abilities in identifying adolescent’s drug use triggers and support their response in assisting the adolescent to cope with these triggers (e.g., drug use refusal skills during social situations), and; 5) strengthen parental self-competency by emphasizing that parents can influence change in their adolescent.
2.1.2. Adolescent objectives.
The adolescent objectives of the Home Base program were to 1) reduce drug use frequency and SUD symptomology; 2) improve communication and relationship with the parents; 3) encourage activities that build youth assets while minimizing situations and behaviors that are likely to trigger drug use; and 4) strengthen self-competency that positive behavioral and familial changes are possible and attainable.
2.1.3. Manual development and content.
The Home Base manual provided an overview of the objectives of the program and a detailed description of each of the BI, home-delivered sessions. Each session consisted of an introduction, core content, homework assignments, wrap-up summary, and reference material. The introduction described the goals of the intervention, the basic strategies and approaches to be learned, and how program implementation will contribute to positive behavior change. The core content included detailed, suggested script for each component of the session, side-bar statements of encouragement and tips for how to handle challenges (e.g., how to respond if the adolescent leaves the session), self-assessment questionnaires, activity guides, worksheets to supplement learning objectives, homework assignments, and several follow-up resources (e.g., guidelines, activities and self-evaluations).
Guided by the literature, several behavior-change strategies were integrated into the program: motivational interviewing, negotiating individualized and specific goals, role-modeling exercises, the use of behavioral rehearsal, cognitive reframing and restructuring, communication skills, and strategies for dealing with barriers and resistance. In addition, specific in-session tasks were described in the manual, which included: 1) communicating family expectations of a drug-free goal; 2) communicating the plan to monitor the adolescent’s access to peers and social situations that may be “trigger” situations; 3) teaching the adolescent problem solving skills to deal with triggers of drug involvement; 4) improving parent-adolescent communication, with a focus on how to “argue fairly”; and 5) clarifying the negative consequences if expectations are not met and the positive reinforcements when they are met.
The program’s length (3 sessions, with one session conducted per week) was guided by the intention to stay within the parameters of a typical brief intervention (see Tanner-Smith & Lipsey, 2014), and yet to be comprehensive enough to address a range of problems. As noted previously, Bis in the literature and in practice can be as brief as a single 5-minute conversation, whereas some consist of 4 to 5 hour-long sessions. This model represents a higher-frequency BI approach.
2.1.4. Parent training.
To address the goal of teaching parents the program curriculum, a single, 4-hour, training session was developed and delivered in an individual session to parent participants in both study conditions. Training materials were presented to the parent(s) by the Program Trainer and consisted of a detailed PowerPoint presentation, discussion sessions, and role-playing as part of the review sessions. The training presented relevant background information to parents, including adolescent brain development, developmental issues relevant to substance use, how early substance use increases the risk of future health problems, and the importance of parenting as an intervention agent. A detailed review of each intervention session was also provided to parents. For those in the intervention condition, additional information addressed the role of parental support by the coach during program implementation.
2.2. Participants
Participants were parents (or primary caregivers) and their adolescent, aged 12-17 years. Participation was limited to the parent who reported regular contact with the participating adolescent and who reported being the most responsible for the conduct and welfare of the adolescent. Biological parents, adoptive parents, step-parents, and legal guardians were included in this definition. Non-target parents/involved adults were also allowed to attend the parent training session, though they did not formally enroll in the program or complete assessments.
2.2.1. Recruitment.
Study participants were initially recruited from 12 different schools and educational settings within the Minneapolis/St. Paul metro area. School staff members helped to identify adolescents who were using substances at a mild-to-moderate level and provided those youth and families with study flyers. Identification of potential participants occurred per usual means by which school staff learns of student substance use (i.e. student suspected to be under the influence on school grounds, possession of paraphernalia, student conversations, etc.). School policies did not allow staff to directly recommend or mandate participation, so school staff presented the study flyer as an option for family involvement. Potential participants initiated contact with study staff. School staff did not consistently track the number of flyers handed out, making a reliable response rate unknown. Forty-two percent of the sample was recruited via schools.
Because the school recruitment method did not yield sufficient participation, it was subsequently necessary to expand recruitment to include radio and television advertising. Study recruitment ads, similar to the flyers used at the schools, were played on 4 different local radio stations and on 2 local television stations. Again, potential participants initiated contact with study staff. Fifty-eight percent of the sample was recruited via media advertising.
Adolescent participants had used alcohol or other drugs at a mild to moderate level, defined in this study by the endorsement of substance use at least once in the prior year and no engagement in formal SUD treatment in the same time frame. Though this mild-to-moderate use definition is admittedly broad, it was maintained that the wide variability is most representative of a community sample for this developmental stage; to measure a program’s effectiveness within a narrow group of adolescents who endorse a limited number of symptoms or frequency of use is counter-productive with the aims of this study. For this reason, adolescents who endorsed higher frequency of use and/or more problems associated with their substance were still included in the study, as long as they had not engaged in formal SUD treatment within the past year.
Diagnostic SUD criteria were not used as inclusionary or exclusionary criteria in this study; however, participants endorsed a mean of 1.4 symptoms for alcohol use disorder (sd=2.0), a mean of 2.8 symptoms for marijuana use disorder (sd = 3.3), and a mean of 0.3 symptoms for other drug use disorder (sd = 0.8), which falls under the DSM5 definition of mild to moderate use as 2-5 endorsed symptoms for a given substance. Other inclusion criteria for these adolescent-parent dyads were that both: 1) lived within the 7-county Minneapolis/St. Paul metro area, 2) could read and write fluent English, and 3) engaged in the informed consent/assent process and agreed to participate.
2.3. Measures
Self-report measures were obtained from the parent and the adolescent at baseline, 3-month, 6-month, and 12-month follow-up assessments.
2.3.1. Substance use data
were measured using the Adolescent Diagnostic Inventory (ADI; Winters & Henly, 1993) and the Timeline Follow Back (TLFB; Sobell & Sobell, 1992). The ADI (Winters & Henly, 1993) provided data on DSM-IV (American Psychiatric Association, 2000) SUD symptomology and diagnoses. TLFB was used to compute alcohol and drug use frequency. Both of these instruments have been widely used, and psychometric testing supports their validity and reliability (Winters, Stinchfield, Fulkerson, & Henly, 1993; Deas, Riggs, Langenbucher, Goldman, & Brown, 2000; Carey, 1997, Robinson, Sobell, Sobell, & Leo, 2014).
2.3.2. Family cohesion data
were measured using the Alabama Parenting Questionnaire (APQ; Frick, 1991), the Parent Happiness with Youth scale (PHYS; Donohue, DeCato, Azrin, & Teichner, 2001), and the Youth Happiness with Parent scale (YHPS; DeCato, Donohue, Azrin, & Teichner, 2001). The APQ (Frick, 1991) measures parenting practices, an important metric since maladaptive practices are associated with a number of adverse behavioral outcomes for adolescents (Gryczkowski, Jordan, & Mercer, 2010; Bahr & Hoffman, 2010). The APQ addresses 5 dimensions of parenting, including Positive Reinforcement, Parental Involvement, Inconsistent Discipline, Poor Monitoring and Supervision, and Harsh Discipline. In an effort to reduce the length of the interview and to focus on primary outcomes, only 3 of the 5 APQ scales were used in this study: Inconsistent Discipline, Positive Reinforcement, and Poor Monitoring and Supervision were combined to create a Total Score. The PHYS and YHPS were both developed to measure the familial satisfaction in common areas of conflict within a parent-adolescent relationship (e.g. chores, alcohol and drug use, illegal behavior, discipline, and communication). It is posited that familial satisfaction can actively guide interventions while being implemented to increase motivation to change in specific areas that are most dissatisfying. Familial satisfaction can also serve as a reminder of relationship strengths when parent-adolescent dyads reflect upon areas that are most satisfying (Donohue, et al., 2001).
2.3.3. Confounder and mediating variable data
were obtained from a variety of measures: Demographic information, adolescent life stressors, and family history data were reported on the ADI (Winters & Henly, 1993); the Peer Chemical Environment sub scale of the Personal Experience Inventory (Henly & Winters, 1989) measured the magnitude of alcohol and other drug use within the adolescent’s peer environment; adolescent problem-solving skills were measured using the Problem Solving Inventory (PSI; Heppner & Peterson, 1982); parenting practices were reported on the Alabama Parenting Questionnaire – short form (APQ; Frick, 1991); and parenting stressors were measured via the Stress Index for Parents of Adolescents (SIPA; Sheras, Abidin, & Konold, 1998).
2.4. Procedure
2.4.1. Assessment.
Following the informed consent process, adolescents and parents independently completed the intake battery. Parent assessments were completed by telephone or in person, according to the parent’s preference and availability. Adolescent assessments occurred in person, at a location she or he considered comfortable and convenient (e.g. school, local library, or local coffee shop). The goal of assessing both parent and adolescent within one week was typically achieved, though exceptions occurred (mean=5.2 days, range=0-42 days).
Follow-up assessments were completed at 3-, 6-, and 12-month post-intake intervals. Similar to the intake, parent assessments were completed by telephone or in person, according to the parent’s preference and availability, and adolescent assessments occurred in person. Follow-up assessments were sought from all participants, even if they did not complete the intervention components. All participants were compensated with a $40 gift card at the completion of each assessment. Additionally, a $50 bonus gift card was bestowed for completing all assessments in a timely manner.
2.4.2. Parent Training.
Within a month after intake data collection (mean=20.8 days, range=6-65), the parent (and other involved parent/caregivers, if desired) completed a 4-hour training program, in person, with a Program Trainer. Trainers were three project staff, each with an advanced degree in the behavioral sciences and highly experienced in delivering brief interventions to adolescents and parents. Program Trainers contributed substantially to intervention manual development and practiced curriculum administration extensively prior to initiating subject recruitment. Curriculum practice included role playing and demonstrations, as well as discussion of the curriculum and potential parent response. Program Trainers participated in bi-weekly staff meetings in which curriculum adherence, case consultation, and feedback were provided.
This 4-hour training session was offered to parents in both the intervention and comparison conditions. The training session consisted of an instructional meeting on the following topics: drug education; adolescent substance use; risk and protective factors for adolescent substance use; and parenting components (e.g., house rules, rewards, consequences). Training was conducted in an interactional manner; parents were encouraged to reflect upon real-life examples of behaviors or incidents observed with the adolescent or their own experiences. This interaction personalized the educational information with the expectation that the information would be better retained and utilized. The Trainers’ oral presentation was supported by a PowerPoint presentation. Parents in both conditions received a Parent Manual to take home as a resource that summarized the information provided in the oral training.
2.4.3. Intervention-Condition Participants.
Parents in the intervention condition were asked to facilitate three BI sessions with their adolescent, one-on-one, in a location that was comfortable and convenient for both of them. These sessions were conducted approximately 7-10 days apart, and supportive parents/other adults were not included in these BI meetings to preclude further confounds. The interactive sessions provided parents with an opportunity to promote important behavioral skills and attitude changes in the adolescent as well as facilitating family communication and interaction.
Intervention-condition parents were contacted by the Program Trainer via telephone prior to each of the three sessions to assist in planning the BI administration. These sessions were identified as “coaching calls” and consisted of a 15-20 minute conversation in which the parents described their knowledge and confidence in the curriculum material for the upcoming session. They also served to review the successes and perceived difficulties that occurred in the previous session. The Program Trainer provided support and guidance during these calls to enhance parental intervention skills.
2.4.4. Comparison Condition Participants.
Parents in this condition received the training session as an “education-only” experience, and were not encouraged or directed to discuss the curriculum content with the adolescent. These parents had no additional interaction with the Program Trainer following the 4-hour training session. They did receive the same curriculum content, though specific therapeutic strategies and on-going support were not provided.
2.5. Design and Analysis
The study utilized a quasi-experimental design. A standard, true randomization procedure was not conducive to the needs of school administrators, who mandated that the same opportunities be offered to all students. For this reason, study condition allocation was alternated over academic terms (e.g. semesters), thus assuring that all participants during that time period could receive the same intervention. As a result, a pure randomized design could not be obtained. A benefit of this recruitment method included minimization of possible cross contamination of conditions within schools.
2.5.1. Propensity Score Analysis
Propensity score analysis was conducted to statistically address the non-randomized comparison design. Propensity score is the probability of a particular individual receiving the treatment, conditional on the observed background covariates (Rosenbaum & Rubin, 1983; see Harder, Stuart, & Anthony, 2010; Tanner-Smith & Lipsey, 2014 for review). Effects of the Home Base intervention on drug use outcomes for adolescents (age 12-17) whose parent received the Home Base intervention (the average treatment effect [ATE]) were estimated using the inverse probability of treatment weights (IPTW; Hirano and Imbens 2001), a technique for propensity score analysis described below.
The analysis proceeded in four steps as described by Lanza, Tan & Bray (2013). First, propensity scores were estimated using a logistic regression model in which treatment status (i.e., receiving intervention) was regressed on the baseline demographic and drug use characteristics listed in Table 3. The two treatment condition groups were assessed to determine the degree of overlapping distributions of propensity scores using boxplots and histograms.
For the second step, the propensity score (pi) was applied to adjust for potential confounds. To estimate the ATE, each individual was weighted by the inverse probability of receiving the intervention that they received (for intervention IPTW= 1/ρi and for comparison IPTW= 1/(1 - ρi)).
Balance of the potential confounders across the two groups was assessed in the third step of the analysis. Standardized mean differences for the raw scores and the data that were adjusted using propensity scores were calculated to examine if balance was achieved. Treatment groups were considered to be balanced if the standardized mean differences are less than 0.20 for all covariates after adjustment (i.e., small effect size, Cohen, 1988).
Finally, to test the intervention effects on repeated measure count data (e.g., number of symptom count, drug used days), generalized estimating equations (GEEs; Liang & Zeger, 1986) were used in SAS 9.3. SAS PROC GENMOD was applied with Poisson distribution and autoregressive correlation structure. For repeated measure continuous outcomes, general linear mixed models were applied to the data using SAS PROC MIXED. Linear and quadratic time variables and linear time by condition and quadratic time by condition interactions were included in the analyses. All outcome analyses utilized the weighted sample (Marcus et al., 2008).
An exploration of the moderating effect of baseline adolescent drug use severity on the relationship between intervention condition and outcomes was conducted by recoding the baseline alcohol and marijuana symptom counts (alcohol range=0-9; marijuana range=0-10) based on DSM-IV symptom criteria number for individual participants (APA, 2000): 0=no disorder (0–1 symptoms), l=mild (2–3 symptoms), 2=moderate (4-5 symptoms), or 3=severe (6 or more symptoms). Then, a continuous drug use severity variable was created by calculating the sum of the recoded alcohol and marijuana symptom count variables (range=0-6).
2.5.2. Missing Data.
Of the 17 pre-intervention confounders that were included in the propensity score analysis, there was only one missing data point on peer substance use. Prior to running propensity score analysis, expectation maximization (EM) method was used to impute the missing value (Dempster, Laird, & Rubin, 1977). All 17 pre-intervention confounder variables and outcome follow-up data were included in the EM model to estimate the missing value. For outcome analyses, missing data in the repeatedly measured outcome variables were addressed using maximum likelihood estimation in SAS PROC MIXED. Little’s MCAR test indicated that absent data was random [χ2 (552) = 534.71, p = .69].
2.5.3. Attrition.
Three-hundred seventy-six potential participants initiated contact regarding participation in the Home Base study. Of those initial contacts, 57 (15%) did not qualify for participation, 27 (7%) directly refused participation, and 142 (38%) passively refused (i.e. did not return calls, stated interest but didn’t follow through). The remaining 150 potential participants began the consent process, though 8 were dropped from the final sample due to only one member of the dyad completing the consent process, resulting in a final sample of 142 parents/adolescent dyads.
Attrition for assessment completion was relatively low. Of the 142 enrolled participant dyads, 14 (9.9%; 3-month n=128) dropped out of the study at 3-month follow-up. Four more dropped out at the 6-month follow-up (12.7%; 6-month n=124), and an additional 5 at the 12-month follow-up (16.2%; 12-month n=l 19). Significantly more intervention participants dropped out, in relation to the comparison condition [22.9% intervention vs 6.8% comparison at the 12-month follow-up (χ2 = 6.595, p = .01)]. Attrition analysis showed that there were no significant differences between those who were retained and those who dropped out in any of the demographics or baseline measures of outcome variables, except in parent age (retained group M=46.81, SD=7.03; dropouts M=42.22, SD=6.17, p<01). One data point for a single participant was imputed for a missing value in the baseline confounder variable (peer substance use test), as noted above.
Note that participants were not excluded from follow-up assessments or data analyses if the parent did not complete the training session or Home Base sessions. In fact, training sessions were well-attended with 93% of parents in the intervention condition and 96% of parents in the comparison condition completing this training. The training completers versus non-completers did not differ significantly on baseline predictor variables, and the number of non-completers was so low that it did not significantly affect outcomes either.
Engagement in completing the three-session Home Base intervention was lower than anticipated. Forty-two percent of enrolled parents completed all 3 Home Base sessions, 19.3% completed 2 of the sessions. 15.7% completed 1 session, and 22.9% did not complete any of the curriculum sessions. On average, parents in the intervention condition completed 2.71 (sd 1.4) Home Base intervention sessions. Further, the number of completed sessions did not significantly vary by the three Program Trainers.
3.0. Results
The study sample was comprised of 142 parent/adolescent dyads (83 in the intervention condition and 59 in the comparison condition). The large majority of participating parents were Caucasian females who were in their mid-40s and had graduated from high school (Table 1). More “non-mother” caregivers were present in the intervention sample, reaching borderline significance (p=.052). In many of these cases, the primary caregiver tended to be a female relative caregiver, especially grandmothers. Parents in the comparison sample also reported having a history of substance use problems at a significantly higher rate than parents in the intervention sample.
Table 1.
Parent demographics at baseline
| Intervention sample (n=83) (mean or %) | Comparison sample (n=59) (mean or %) | |
|---|---|---|
| Age | 44.9 yrs | 47.7 yrs |
| Female * | 87.2% | 96.6% |
| Relationship to adol. = mom | 84.9% | 93.2% |
| Caucasian | 82.6% | 86.4% |
| Married | 53.5% | 42.4% |
| Education (yrs) | 14.9 yrs | 15.5 yrs |
| Employed | 80.2% | 86.4% |
| Annual income >$40K | 75.6% | 78.0% |
| Hx of substance use problem* | 14.0% | 27.1% |
| Hx of mental health problem | 66.3% | 67.8% |
p< .05
Adolescent participants in this study were most often 15-16 year old boys, with a higher frequency identifying as Caucasian in the comparison sample, though the difference between conditions was non-significant (Table 2). Baseline measurement of the adolescents’ substance use was obtained and found that the two groups did not significantly differ on their alcohol and marijuana DSM-IV (APA, 2000) symptomology. However, the comparison group used significantly more ‘other drugs’ than the intervention group and they used marijuana at a significantly higher frequency than the intervention group. In addition, more members of the comparison group used tobacco than the intervention group, though the difference was nonsignificant.
Table 2.
Adolescent demographics at baseline
| Intervention (n=83) (mean or %) | Comparison (n=59) (mean or %) | |
|---|---|---|
| Age | 15.6 yrs | 15.6 yrs |
| Female | 20.2 | 22.0 |
| Caucasian | 66.7 | 78.0 |
| Alc Use Disorder Symptom Count | 1.2 | 1.8 |
| Days alcohol use (past 90 days) | 4.0 days | 5.0 days |
| Mar Use Disorder Symptom Count | 2.5 | 3.3 |
| Days marijuana use (past 90 days) * | 31.1 | 42.1 |
| Count of other drugs ever used ** | .8 | 1.6 |
| Ever used tobacco | 66.7 | 79.7 |
p<.05
p<.01
Table 3 presents the unweighted and weighted standardized mean differences between the two intervention conditions for all confounder variables. The propensity score model included 17 pre-intervention confounder variables considered to be related to the parent’s enrollment and study outcomes including demographic variables, parenting style, parenting stress, family history of substance use, and peer substance use. Adolescent baseline drug use variables were included to account for the group differences at intake (Table 3). Among the 17 pre-intervention confounder variables, independent sample t tests showed that there were significant group differences at baseline for three variables: parent age, number of days marijuana was used by the adolescent, and count of other drugs used in the adolescent’s lifetime.
Table 3.
Balance table: raw means, standard deviations, and unweighted and weighted
| Confounder | HomeBase (n=83) M (SD) |
Control (n=59) M (SD) |
P | Unweighted Std Diff |
Weighted Std Diff |
|---|---|---|---|---|---|
| Parent age | 45.00 (7.01) | 47.56 (6.99) | .03 | 0.37 | 0.03 |
| Family annual income | 5.04 (1.31) | 5.07 (1.20) | .88 | 0.02 | 0.04 |
| Parent education (yrs) | 14.90 (2.71) | 15.49 (2.51) | .19 | 0.22 | 0.05 |
| Adolescents’ age | 15.59 (1.30) | 15.56 (1.28) | .89 | 0.02 | 0.05 |
| Adolescents’ gender | |||||
| (0=male, 1=female) | 0.20 (0.41) | 0.22 (0.42) | .83 | 0.04 | 0.08 |
| # of people in family | |||||
| with alcohol problem | 0.72 (0.74) | 0.86 (0.88) | .30 | 0.19 | 0.0005 |
| # of people in family | |||||
| with drug use problem | 0.63 (0.78) | 0.64 (0.87) | .90 | 0.02 | 0.02 |
| APQ total (parent) | 60.92 (7.36) | 60.99 (7.03) | .95 | 0.01 | 0.02 |
| Parenting Stress Index | 53.92 (9.65) | 53.78 (10.63) | .94 | 0.01 | 0.04 |
| Life stressors | 3.30 (1.89) | 3.46 (1.68) | .61 | 0.08 | 0.04 |
| Adolescent drug use | |||||
| AUD symp count | 1.19 (1.95) | 1.78 (2.09) | .09 | 0.30 | 0.05 |
| MUD symp count | 2.47 (3.26) | 3.29 (3.32) | .15 | 0.25 | 0.002 |
| Alcohol use days | 4.04 (6.10) | 5.00 (8.21) | .42 | 0.16 | 0.08 |
| Marijuana use days | 31.19 (27.54) | 42.05 (32.32) | .03 | 0.39 | 0.02 |
| Have used tobacco | 0.66 (0.48) | 0.80 (0.41) | .08 | 0.28 | 0.003 |
| # of other drugs used | |||||
| lifetime | 0.81 (1.57) | 1.59 (1.90) | .01 | 0.50 | 0.06 |
| Peer Substance Use | 16.64 (4.15) | 16.86 (3.90) | .73 | 0.05 | 0.04 |
Note. Standardized mean differences that are >=.20 are bolded.
There was substantial overlap of the propensity scores between the two groups that justified the application of the IPTW (Figure 1). Several confounder variables had standardized mean differences that were > 0.20, including parent age, parent education, and adolescent drug use variables. After adjusting for propensity score, all of the standardized mean differences in the weighted sample were less than 0.20, indicating that a desirable balance was achieved.
Figure 1.
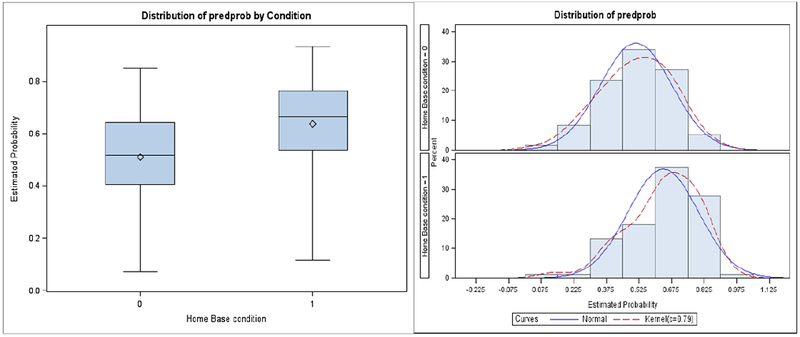
Boxplots and histograms of propensity score distributions for intervention (=1) vs. comparison (=0) groups.
Weighted means and standard deviations, and summary results from the longitudinal outcome analyses demonstrated there were significant quadratic time by intervention effects and a marginally significant linear time by intervention effect on marijuana used days (Table 4). Inspection of the means showed that participants in the intervention condition showed greater reduction in marijuana use days from baseline to 3-month follow-up compared to the comparison group. From the 3-month to 12-month follow-up, intervention participants showed gradual increase in days of marijuana use, while the comparison group maintained a relatively higher level over time.
Table 4.
Weighted means and standard deviations, and summary results of the longitudinal outcome analyses
| Home Base | Comparison | Condition | Linear | 1 × | Quadratic | q × | |||
|---|---|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | Time (1) | Condition | Time (q) | Condition | |
| AUD symptom count | 0.11 | −0.24** | 0.05 | 0.02** | −0.01 | ||||
| BL | 1.67 | 2.33 | 1.49 | 1.89 | |||||
| 3 mo FU | 0.72 | 1.59 | 0.59 | 1.48 | |||||
| 6 mo FU | 1.00 | 1.84 | 0.64 | 1.53 | |||||
| 12 mo FU | 1.26 | 2.46 | 1.27 | 2.02 | |||||
| MUD symptom count | 0.001 | −0.08 | 0.01 | 0.01 | −0.001 | ||||
| BL | 2.86 | 3.44 | 2.84 | 3.08 | |||||
| 3 mo FU | 1.91 | 2.34 | 2.06 | 2.37 | |||||
| 6 mo FU | 2.48 | 2.78 | 2.13 | 2.36 | |||||
| 12 mo FU | 2.80 | 2.80 | 2.60 | 3.03 | |||||
| Alcohol used days | 0.16 | 0.01 | −0.27 | 0.003 | 0.004 | ||||
| BL | 4.97 | 6.49 | 4.27 | 7.51 | |||||
| 3 mo FU | 7.63 | 13.98 | 5.34 | 10.63 | |||||
| 6 mo FU | 5.03 | 7.22 | 4.40 | 6.86 | |||||
| 12 mo FU | 8.86 | 13.78 | 5.92 | 9.93 | |||||
| Marijuana used days | −0.02 | −0.15*** | −0.12† | 0.01*** | 0.01* | ||||
| BL | 34.31 | 27.76 | 35.20 | 31.52 | |||||
| 3 mo FU | 19.96 | 26.43 | 27.69 | 33.38 | |||||
| 6 mo FU | 23.85 | 27.94 | 32.86 | 37.03 | |||||
| 12 mo FU | 28.90 | 27.46 | 30.36 | 33.81 | |||||
| APQ parenting (parent) | −0.23 | 0.80*** | 0.12 | −0.05*** | −0.01 | ||||
| BL | 61.52 | 7.57 | 61.31 | 6.73 | |||||
| 3 mo FU | 63.12 | 7.63 | 64.14 | 6.48 | |||||
| 6 mo FU | 63.62 | 7.37 | 63.26 | 7.52 | |||||
| 12 mo FU | 63.59 | 7.56 | 62.99 | 8.44 | |||||
| Parent Happiness with Youth | 1.00 | 3.32*** | 0.12 | −0.21*** | 0.02 | ||||
| BL | 45.10 | 15.02 | 45.99 | 14.75 | |||||
| 3 mo FU | 53.28 | 17.58 | 52.62 | 15.20 | |||||
| 6 mo FU | 56.51 | 15.49 | 57.08 | 14.86 | |||||
| 12 mo FU | 54.07 | 17.84 | 49.87 | 20.23 | |||||
| Youth Happiness with Parent | −0.57 | −0.75 | −0.61 | 0.11* | 0.05 | ||||
| BL | 52.31 | 17.60 | 53.26 | 17.63 | |||||
| 3 mo FU | 49.57 | 14.48 | 54.88 | 17.22 | |||||
| 6 mo FU | 52.12 | 15.48 | 54.15 | 17.06 | |||||
| 12 mo FU | 60.11 | 16.79 | 61.49 | 20.69 | |||||
| Peer Substance Use | −0.13 | 0.31 | 0.24 | −0.02 | −0.02 | ||||
| BL | 16.80 | 3.92 | 17.02 | 3.94 | |||||
| 3 mo FU | 17.39 | 3.76 | 17.29 | 3.65 | |||||
| 6 mo FU | 17.82 | 4.00 | 17.37 | 3.62 | |||||
| 12 mo FU | 17.49 | 3.97 | 17.24 | 3.65 | |||||
p < .05,
p < .01,
p < .001,
p = .06
Significant linear and quadratic time effects for the weighted sample were detected in AUD symptom count, days of marijuana use, APQ parenting, and parent happiness with adolescent (Table 4). The results indicated that both groups showed significant decreases in AUD symptom count and days of marijuana use from baseline to 3-month follow-up, as well as in the parenting and relationship happiness from baseline to 6-month follow-up. After the initial improvement, there were significant increases in drug use and reduction in parenting and relationship variables.
There were significant moderating effects on marijuana use frequency and Peer Substance Use (PSU) at the 3- and 6-month follow-ups (Figure 2). The data indicate that intervention adolescents with lower aggregate SUD symptom counts at baseline had fewer days of marijuana use at the 3- and 6-month follow-ups compared to those with higher baseline SUD count. Intervention adolescents with a lower initial SUD symptom count had fewer days of marijuana use at the 3- and 6-month follow-ups in relation to adolescents in the comparison condition. Initial SUD symptom count also was a significant moderator in consideration of their peer group. The moderating data indicate that adolescents in both conditions who had a higher aggregate count of SUD symptoms at baseline reported greater increase in associating with a non-drug using peer group over the course of the study.
Figure 2.
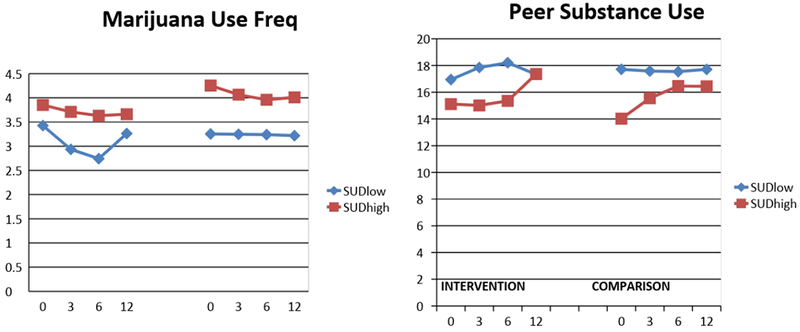
Interaction effects of time (linear and quadratic) x intervention x SUD severity (baseline) on marijuana use frequency and peer substance use outcomes.
Satisfaction ratings were provided by parents at the 3-month follow-up assessment regarding parent satisfaction on how the program changed their parenting behaviors, reduced their child’s substance use, improved their relationship with their child, and their overall satisfaction. Data from these items generally indicated nonsignificant differences between the conditions, but several items showed a trend suggesting that the intervention was beneficial to parents. These trends included: 1) intervention parents reported changing their parenting behaviors more as a result of the program (p=40.3% compared to 26.4%), 2) more intervention parents perceived a decrease in their child’s substance use (67.7% vs 54.7%), and 3) more intervention parents would highly recommend this program to others (85.1% vs 71.7%). One statistically significant result was found in the satisfaction items, which revealed that intervention parents were significantly more likely to report an improved relationship with their adolescent as a result of the Home Base program (χ2 = 7.5, p=.02).
4.0. Discussion
This Home Base study explored the impact of a home-based, parent-led, adolescent substance use early intervention. The intervention was created using Cognitive Behavioral and Motivational Interviewing methods and targeted families with adolescents using alcohol or other drugs at a subclinical level of severity, a population that generally has limited treatment or service options. The goals were to decrease adolescent substance use, increase family cohesion, and to effectively teach parents how to communicate with their teen on the topic of substance use.
We predicted the intervention condition would be more effective than the comparison condition, and the study results revealed this trend for some variables. In regard to substance use outcome variables, results showed a significantly greater decrease in days of marijuana use at the 3-month follow-up among adolescents in the intervention condition in relation to those in the comparison condition. Moderating data suggest that the Home Base intervention was most effective in reducing marijuana use when administered to adolescents with a mild initial SUD. Results also indicated a significant reduction in Alcohol Use Disorder symptom count for adolescents in the intervention condition versus the comparison condition at the 3-month followup. These substance use outcomes appeared to be greatest in the short-term, perhaps indicating that, as families became more temporally removed from the intervention, they returned to their old patterns of behavior, thus diminishing the initial impact of the intervention. Extended parental support, or “booster-sessions,” may be beneficial for longer-term benefits.
Family cohesion outcomes were somewhat more robust, revealing that intervention parents reported significantly greater happiness with their adolescent than the comparison parents. Intervention parents were also more likely to report an improvement in their relationship with their teen, as well as greater improvement in their parenting skills, as measured by the APQ (Frick, 1991). The adolescent participants revealed an increase in their happiness with their parent, but differences between the conditions were not significant.
Finally, variability in family dynamics, differences in adolescent response to altered parental approach and peer influences may substantially affect the impact of time-limited interventions, such as Home Base. These factors may have produced a biased perception that the parent was not able to influence change in their adolescent child. Because this intervention was intended to be a means for “planting seeds” in creating longer-term change within adolescent behaviors, it is important to recognize that change may not be fully established at a 12-month follow-up. Therefore the quantitative variables assessed during this timeframe may not necessarily reveal the small progression that may have occurred in the change process. Longer-term longitudinal follow up may permit differentiation of responder and non-responder dyads. Results could then be applied to directing supplementary intervention as needed.
There were several limitations. A quasi-experimental design was utilized in response to requests from school administrators. School policy did not allow, based on need for equivalence of service to all students, the random assignment necessary for a rigorous RCT. In addition, since school staff members were not blinded to study condition, a further confound may have emerged from “selection bias” in identifying students in need of intervention. Related, but based on need to enhance accrual, additional recruitment methods were required including advertisements. The comparison group was comprised of more participants recruited from radio and TV advertising, which eliminated the initial clinical judgement of the school staff member in the referral-recruitment process. Demographically, the majority of the parent sample was white, educated (at least some college), and middle class (annual income range $40,000-$75,000), which is fairly representative of the Minneapolis/St. Paul metro area (US Census Bureau, 2017). It is unclear if the findings will generalize to more diverse populations. Rigorous research that addresses these issues of bias is necessary.
Notably, only 42% of parents completed all three intervention sessions. On the other hand, assessment retention was quite good with 77% of the intervention dyads completing the full assessment battery, regardless of whether they completed all the intervention sessions. Moreover, 93% of the comparison dyads completed all the assessments. Undoubtedly, barriers to parental involvement exist. Time and energy constraints are abundant for parents and the intervention, though minimal, may have been burdensome for some parents. Differences between school referred participants and those responding to advertisements may have reflected greater investment in participation by the latter group.
Another limitation of this study may be within the definition of “mild-to-moderate” substance use and fluctuations in patterns (Tucker, Ellickson, Orlando, Martino, & Klein, 2005). Because inclusionary criteria were based upon adolescents’ self-report of substance use, it is possible that the recruited population did not adequately represent the population for whom the curriculum was intended. Though the mean number of self-reported Alcohol and Marijuana Use Disorder symptoms at intake indicated a mild-to-moderate population (Alcohol Use Disorder symptom count: x=1.4, sd = 2.0; Marijuana Use Disorder symptom count: x=2.8, sd=3.3), some participants reported higher frequencies and consequences of substance use. Ultimately, the intervention may be most effective for those with mild, rather than moderate, use patterns.
In summary, while not recommended to be used as a stand-alone intervention, the Home Base curriculum may serve as a worthwhile complementary component to other early-intervention services. Favorable parenting practices, such as monitoring and supervision, appropriate level of rewards and consequences, and clear communication are important components of effective prevention programs (Nation et al., 2003). These practices were clearly addressed in the Home Base curriculum and may serve families as a platform for long-term health.
Highlights:
This BI addresses a gap in service options for adolescent drug interventions.
Results indicate improvement in parental relationship with teen.
Data show a reduction in adolescent marijuana use frequency at 3-month follow-up.
Alcohol and tobacco use frequency were statistically unchanged.
Baseline drug use severity served as a moderator between intervention and outcome.
Acknowledgements:
We would like to express our sincere appreciation to Tamara Fahnhorst and other CASAR staff for their work and dedication to the program’s development and implementation, as well as to Kim Kirby and staff at Treatment Research Institute for their unwavering support.
Author Acknowledgement: This study was supported by Award Number P50DA027841 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This clinical trial is registered under NCT01591239 on clinicaltrials.gov. Some of the data presented in this manuscript were presented at the Hennepin County Spring Conference on 5/3/18.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None
Contributor Information
Andria M. Botzet, University of Minnesota, Minneapolis, Minnesota
Christine Dittel, University of Minnesota, Minneapolis, Minnesota.
Robyn Birkeland, University of Minnesota, Minneapolis, Minnesota.
Susanne Lee, University of Minnesota, Minneapolis, Minnesota.
John Grabowski, University of Minnesota, Minneapolis, Minnesota.
Ken C. Winters, Oregon Research Institute
5.0 References
- Allen ML, Garcia-Huidobro D, Porta C, Curran D, Patel R, Miller J, & Borowsky I (2016). Effective parenting interventions to reduce youth substance use: a systematic review. Pediatrics, e20154425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (APA; 2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association. [Google Scholar]
- Bahr SJ, & Hoffmann JP (2010). Parenting style, religiosity, peers, and adolescent heavy drinking. Journal of Studies on Alcohol and Drugs, 71(4), 539–543. [DOI] [PubMed] [Google Scholar]
- Barnes GM, Hoffman JH, Welte JW, Farrell MP, & Dintcheff BA (2006). Effects of parental monitoring and peer deviance on substance use and delinquency. Journal of Marriage and Family, 68(4), 1084–1104. [Google Scholar]
- Bertrand K, Richer I, Brunelle N, Beaudoin I, Lemieux A, & Menard JM (2013). Substance abuse treatment for adolescents: How are family factors related to substance use change? Journal of Psychoactive Drugs, 45, 28–38. [DOI] [PubMed] [Google Scholar]
- Booth RE & Kwiatkowski CF (1999). Substance abuse treatment for high-risk adolescents. Current Psychiatry Report, 1, 185–190. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Griffin KW, Paul E, & Macaulay AP (2003). Preventing tobacco and alcohol use among elementary school students through life skills training. Journal of Child & Adolescent Substance Abuse, 12(4), 1–17. [Google Scholar]
- Bronte-Tinkew J, Moore K, & Carrano J (2006). The father-child relationship, parenting styles, and adolescent risk behaviors in intact families. Journal of Family Issues, 27, 850–881. [Google Scholar]
- Burdzovic Andreas J, Pape H, & Bretteville-Jensen AL(2016). Who are the adolescents saying “No” to cannabis offers? Drug and Alcohol Dependence, 163 (1), 64–70. 10.1016/i.druqalcdep.2016.03.025 [DOI] [PubMed] [Google Scholar]
- Calafat A, García F, Juan M, Becoña E, & Fernández-Hermida JR (2014). Which parenting style is more protective against adolescent substance use? Evidence within the European context. Drug and alcohol dependence, 138, 185–192. [DOI] [PubMed] [Google Scholar]
- Carey KB (1997). Reliability and validity of the time-line follow-back interview among psychiatric outpatients: A preliminary report. Psychology of Addictive Behaviors, 77(1), 26. [Google Scholar]
- Carney T, & Myers B (2012). Effectiveness of early interventions for substance-using adolescents: findings from a systematic review and meta-analysis. Substance Abuse Treatment, Prevention, and Policy, 7(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, & Hare TA (2008). The adolescent brain. Annals of the New York Academy of Sciences, 1124, 111–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2017). 2016 National Survey on Drug Use and Health: Detailed Tables Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2015). MMWR. Morbidity and Mortality Weekly Reports. Youth Risk Behavior Surveillance. Retrieved from: www.cdc.gov/yrbss
- Clark HK, Shamblen SR, Ringwalt CL, & Hanley S (2012). Predicting high risk adolescents’ substance use over time: The role of parent monitoring. Journal of Primary Prevention, 33, 67–77. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. (2nd edition). Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Deas D, Riggs P, Langenbucher J, Goldman M, & Brown S (2000). Adolescents are not adults: Developmental considerations in alcohol users. Alcoholism: Clinical and Experimental Research, 24(2), 232–237. [PubMed] [Google Scholar]
- DeCato L, Donohue B, Azrin NH, & Teichner GA (2001). Satisfaction of conduct-disordered and substance-abusing youth with their parents. Behavior Modification, 25, 44–61. [DOI] [PubMed] [Google Scholar]
- Dempster AP, Laird NH, Rubin DB (1977). Maximum likelihood from incomplete data via the EM algorithm. Journal of the Royal Statistical Society, B39, 1–38. [Google Scholar]
- Donohue B, DeCato L, Azrin NH, & Teichner GA (2001). Satisfaction of parents with their conduct-disordered and substance-abusing youth. Behavior Modification, 25, 21–43 [DOI] [PubMed] [Google Scholar]
- Fearnow M, Chassin L, Presson CC, & Sherman SJ (1998). Determinants of parental attempts to deter their children’s cigarette smoking. Journal of Applied Developmental Psychology, 19, 453–468. [Google Scholar]
- Foley KL, Altman D, Durant RH, & Wolfson M (2004). Adults’ approval and adolescents’ alcohol use. Journal of Adolescent Health, 35, 345, e17–26. [PubMed] [Google Scholar]
- Frick PJ (1991) The Alabama Parenting Questionnaire. Retrieved from: http://fs.uno.edu/pfrick/APQ.html
- Gryczkowski MR, Jordan SS, & Mercer SH (2010). Differential relations between mothers’ and fathers’ parenting practices and child externalizing behavior. Journal of Child and Family Studies, 79(5), 539–546. [Google Scholar]
- Harder VS, Stuart EA, & Anthony JC (2010). Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychological Methods, 15 (3), 234–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Kosterman R, Abbott R, & Hill KG (1999). Preventing adolescent health-risk behaviors by strengthening protection during childhood. Archives of Pediatrics & Adolescent Medicine, 755(3), 226–234. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Graham J, Maguin, Abbott R, Hill K, & Catalano R (1997). Exploring the effects of age of alcohol use initiation and psychosocial risk factors on subsequent alcohol misuse. Journal of Studies on Alcohol, 58, 280–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henly GA & Winters KC (1989). Development of psychosocial scales for the assessment of adolescent alcohol and drug involvement. The International Journal of the Addictions, 24, 973–1001. [DOI] [PubMed] [Google Scholar]
- Heppner PP & Petersen CH (1982). The development and implications of a personal problem-solving inventory. Journal of Counseling Psychology, 29, 1, 66–75. [Google Scholar]
- Hirano K, & Imbens GW (2001). Estimation of causal effects using propensity score weighting: An application to data on right heart catheterization. Health Services and Outcomes Research Methodology, 2(3-4), 259–278. DOI: 10.1023/A:1020371312283 [DOI] [Google Scholar]
- Hogue A & Liddle HA (2009). Family-based treatment for adolescent substance abuse: controlled trials and new horizons in services research. Journal of Family Therapy, 31, 126–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaccard J, Blanton H, & Dodge T (2005). Peer influences on risk behavior: an analysis of the effects of a close friend. Developmental psychology, 47(1), 135. [DOI] [PubMed] [Google Scholar]
- Jackson C (2002). Perceived legitimacy of parental authority and tobacco and alcohol use during early adolescence. Journal of Adolescent Health, 31, 425–432. [DOI] [PubMed] [Google Scholar]
- Jackson C, & Dickinson D (2003). Can parents who smoke socialise their children against smoking? Results from the Smoke-free Kids intervention trial. Tobacco control, 72(1), 52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson C, & Dickinson D (2006). Enabling parents who smoke to prevent their children from initiating smoking: results from a 3-year intervention evaluation. Archives of pediatrics & adolescent medicine, 760(1), 56–62. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2008). Monitoring the future national survey results on drug use, 1975– 2007: Volume I. Secondary school students (NIH Publication No. 08-6418A) Bethesda, MD: National Institute on Drug Abuse. [Google Scholar]
- Kosterman R, Bailey JA, Guttmannova K, Jones TM, Eisenberg N, Hill KG, & Hawkins JD (2016). Marijuana legalization and parents’ attitudes, use, and parenting in Washington State. Journal of Adolescent Health, 59(4), 450–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb CS, & Crano WD (2014). Parents’ beliefs and children’s marijuana use: Evidence for a self-fulfilling prophecy effect. Addictive behaviors, 39(1), 127–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Tan X, & Bray BC (2013). Latent class analysis with distal outcomes: A flexible model-based approach. Structural Equation Modeling, 20, 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy SJ, & Williams JF (2016). Substance use screening, brief intervention, and referral to treatment. Pediatrics, 138(1), e1–e15. [DOI] [PubMed] [Google Scholar]
- Levy S, Winters KC, & Knight JR (2011). Screening and brief interventions for adolescent substance use in the general office setting In Clinical manual of adolescent substance abuse treatment (pp. 65–81). American Psychiatric Publishing, Arlington (VA). [Google Scholar]
- Liang KY, & Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73, 13–22. [Google Scholar]
- Liddle HA, Rowe CL, Dakof GA, Ungaro RA, & Henderson CE (2004). Early intervention for adolescent substance abuse: Pretreatment to posttreatment outcomes of a randomized clinical trial comparing multidimensional family therapy and peer group treatment. Journal of Psychoactive Drugs, 36, 49–63. [DOI] [PubMed] [Google Scholar]
- Marcus SM, Siddique J, Have TRT, Gibbons RD, Stuart E, & Normand ST (2008). Balancing treatment comparisons in longitudinal studies. Psychiatric Annals, 38(12) 805–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Ambler A, Harrington HL, Houts R, Keefe RSE, McDonald K, Ward A, Poulton R, & Moffitt TE (2012). Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academy of Sciences Plus, 109, 2657–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash SG, McQueen A, & Bray JH (2005). Pathways to adolescent alcohol use: Family environment, peer influence, and parental expectations. Journal of Adolescent Health, 57(1), 19–28. [DOI] [PubMed] [Google Scholar]
- Nation M, Crusto C, Wandersman A, Kumpfer KL, Seybolt D, Morrissey-Kane E, & Davino K (2003). What works in prevention: Principles of effective prevention programs. American Psychologist, 58, 449–456. [DOI] [PubMed] [Google Scholar]
- Nonnemaker JM, Silber-Ashley O, Farrelly MC, & Dench D (2012). Parent-child communication and marijuana initiation: Evidence using discrete-time survival analysis. Addictive behaviors, 57(12), 1342–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant RW & Panzarella P (2009). Residential treatment of adolescents with substance use disorders: Evidence-based approaches and best practice recommendations In Leukefeld C, Gullotta TP, & Staton-Tindall M, (eds.), Adolescent substance abuse: evidence-based approaches to prevention and treatment (pp.135–154). New York: Springer. [Google Scholar]
- Ringwalt CL, Greene JM, Ennett ST, Iachan R, Clayton RR, & Leukefeld CG (1994). Past and future directions of the DARE program: An evaluation review. Retrieved August 1, 2017 from https://www.ncjrs.gov/pdffilesl/Digitization/152055NCJRS.pdf
- Robinson SM, Sobell LC, Sobell ΜB, & Leo GI (2014). Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use. Psychology of addictive behaviors, 25(1), 154. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR & Rubin DB (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70, 41–55. [Google Scholar]
- Sheras PL, Abidin RR, & Konold TR (1998). Stress index for parents of adolescents: Professional manual. Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Siegel JT, Tan CN, Navarro MA, Alvaro EM, & Crano WD (2015). The power of the proposition: Frequency of marijuana offers, parental knowledge, and adolescent marijuana use. Drug and alcohol dependence, 148, 34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, & Sobell ΜB (1992). Timeline follow-back: A technique for assessing self-reported alcohol consumption In Litten RZ & Allen JP (Eds.), Measuring alcohol consumption: Psychosocial and biochemical methods (pp. 41–72), Humana Press. [Google Scholar]
- Squeglia LM, Jacobus BA, & Tapert SF (2009). The Influence of Substance Use on Adolescent Brain Development. Clinical EEG and Neuroscience, 40, 31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L (2001). We know some things: Parent-adolescent relationships in retrospect and prospect. Journal’ofResearch on Adolescence, 11, 1–19. [Google Scholar]
- Stone AL, Becker LG, Huber AM, & Catalano RF (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive behaviors, 37(1), 747–775. [DOI] [PubMed] [Google Scholar]
- Tait RJ & Hulse GK (2003). A systematic review of brief interventions with substance using adolescents by type of drug. Drug and Alcohol Review, 22, 337–346. [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2014). Identifying Baseline Covariates for Use in Propensity Scores: A Novel Approach Illustrated for a Non-randomized Study of Recovery High Schools. PJE. Peabody Journal of Education, 59(2), 183–196. 10.1080/0161956X.2014.895647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, Orlando M, Martino SC, & Klein DJ (2005). Substance use trajectories from early adolescence to emerging adulthood: A comparison of smoking, binge drinking, and marijuana use. Journal of Drug Issues, 55(2), 307–332. [Google Scholar]
- U.S. Census Bureau (2017). American Community Survey 1-year estimates. Retrieved from Census Reporter Profde page for Minneapolis-St. Paul-Bloomington, MN-WI Metro Area https://censusreporter.org/profiles/31000US33460-minneapolis-st-paul-bloomington-mn-wi-metro-area/
- Van der Vorst H Engels RC, Meeus WH & Dekovic M (2006). The impact of alcohol-specific rules, parental norms about early drinking and parental alcohol use on adolescents’ drinking behavior. Journal of Child Psychology and Psychiatry, 47, 1299–1306. [DOI] [PubMed] [Google Scholar]
- Van Ryzin MJ, Fosco GM, & Dishion TJ (2012). Family and peer predictors of substance use from early adolescence to early adulthood: An 11-year prospective analysis. Addictive behaviors, 37(12), 1314–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeulen-Smit E, Verdurmen JEE, Engels RCΜE, & Vollebergh WAM (2015). The role of general parenting and cannabis-specific parenting practices in adolescent cannabis and other illicit drug use. Drag and alcohol dependence, 147, 222–228. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, & Cunningham RM (2010). Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. Jama, 304(5), 527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams RJ, McDermitt DR, Bertrand LD, & Davis RM (2003). Parental awareness of adolescent substance use. Addictive behaviors, 25(4), 803–809. [DOI] [PubMed] [Google Scholar]
- Winters KC, Botzet A, Dittel C, Fahnhorst T, & Nicolson A (2015). Can parents provide brief intervention services to their drug-abusing teenager? Journal of Child and Adolescent Substance, 24, 134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Lee S, Botzet A, Fahnhorst T, & Nicholson A (2014). One-year outcomes of a brief intervention for drug abusing adolescents. Psychology of Addictive Behaviors, 28, 464–474. NMMSID #600646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, & Henly GA (1993). Adolescent Diagnostic Interview (ADI): Manual. Western Psychological Services. [Google Scholar]
- Winters KC, Stinchfield RD, Fulkerson J, & Henly GA (1993). Measuring alcohol and cannabis use disorders in an adolescent clinical sample. Psychology of Addictive Behaviors, 7(3), 185. [Google Scholar]
- Yatchmenoff DK (2005). Measuring client engagement from the client’s perspective in nonvoluntary child protective services. Research on Social Work Practice, 15, 84–96. [Google Scholar]


