Abstract
Thirty dentists with clinical practices outside of a university setting were trained and calibrated successfully in DMFS and ICDAS-scoring. This randomized, controlled, parallel-arm, double-blind 2-year clinical trial with individual-level caries risk assignment of 460 patients to standard of care as control versus active CAMBRA treatment as intervention demonstrated that caries risk level, as well as caries disease indicators, were significantly reduced in the CAMBRA intervention group compared to the controls at all recall time points.
Introduction
Dental caries is the most prevalent disease condition of humankind, imposing a significant burden at all life stages, from childhood to adult life.1 The disease is chronic, transmissible and infectious,2 and consequently, the disease develops under conditions which favor dysbiosis. In oral health a dynamic balance is reached between the host, the environment, and the microbiome (symbiosis). Frequent intake of sugar and/or reductions in saliva flow results in extended periods of low pH in the biofilm, which disrupts this symbiotic relationship. Such conditions inhibit the growth of beneficial species and drive the selection of bacteria with an acid-producing/acid-tolerating phenotype, thereby increasing the risk of caries (dysbiosis).3 Nevertheless, Dental practitioners and patients alike have often assumed that placing a restoration ‘‘fixes’’ dental caries, which is not true. Placing a filling or crown does not eliminate the load of cariogenic bacteria in the mouth or address other risk factors that cause the disease. Consequently, caries is not stopped by placing a restoration.4 The vicious cycle of caries, restoration, and secondary caries, followed by a new and larger restoration is not interrupted.5 Instead, the stability of the tooth declines over time through loss of structure at every successive treatment and retreatment.
When the principles of Caries Management By Risk Assessment (CAMBRA®) were introduced in 2003, a major transformation in how to conceptualize and treat the caries disease was underway.6–9 With CAMBRA, scientific, evidence-based solutions for prevention and treatment of caries as a manageable medical condition, not a mechanical problem, were translated into clinically relevant guidelines for dentists.10
The ideology of managing caries lesions very early, before they have reached the cavitated stage without drilling but by preventive measures has been embraced within many modern dental practices.11,12 Non-invasive and minimally invasive treatment concepts13–15 are now widely accepted by dental practitioners. Following these concepts, and taking into consideration each patient’s caries risk, invasive restorative treatments can be delayed and performed at more advanced caries lesion stages, if not avoided entirely.11,12,16
In many dental practices throughout the country and world the CAMBRA philosophy has been completely incorporated into the practice routine and embodied by the whole patient care team, including dental assistants and hygienists, front desk staff, and doctors.
In short, CAMBRA requires the dentist to identify the caries risk level of the individual patient by evaluating her/his disease indicators, risk factors and preventive factors using a caries risk assessment (CRA) form (see other papers in this issue). Taking those factors into account, a caries risk level of low, moderate, high or extreme is assigned. According to the assigned risk level, changes in the patient’s lifestyle are discussed, and if necessary, additional preventive chemical measures are recommended.10,17–22 CAMBRA also includes carrying out non-invasive therapies and minimally invasive restorative procedures for tooth structure conservation, and finally, recall and review.23
First CAMBRA clinical trial
The first CAMBRA study was performed at the University of California at San Francisco (UCSF) between 1999 and 2004.4 The study was a randomized, prospective, controlled clinical trial over two years. Impressively, the results indicated that an over-the-counter (OTC) fluoride toothpaste and/or rinse combined with an antibacterial agent (chlorhexidine) were able to significantly reduce the cariogenic bacterial load over the study period. Bacteria testing also strikingly revealed that, in the control group, placing restorations alone did not reduce the Mutans Streptococci (MS) bacterial challenge. Mutans Streptococci represent a group of major cariogenic bacteria. The MS bacterial challenge in the CAMBRA intervention group was significantly lower at each recall visit.
In addition, it was shown that with just placing restorations the caries risk level of individuals in the control group was not lowered either.4 In contrast, the intervention group receiving the antibacterial and preventive fluoride measures, showed a significantly decreased number of subjects at high caries risk. The antibacterial and fluoride therapy had altered successfully the balance between pathological and protective caries risk factors, lowering the caries risk level among intervention group patients.
One other major finding of the first CAMBRA clinical trial was a reduced number of new caries lesions over the two years for the high caries risk subjects in the intervention group. The participants in the intervention group developed fewer new cavities: a statistically significantly 24% lower increase in DMFS (decayed, missing, filled tooth surfaces) than the control subjects. In summary, the CAMBRA trial demonstrated that for high caries risk patients, employing fluoride and bactericidal agents lowers caries risk and fewer cavitated lesions will occur.4
Predictive validity of the CAMBRA risk assessment system
The CAMBRA caries risk assessment (CRA) system was evaluated in several outcomes studies.20,24 First at the UCSF School of Dentistry clinics, Doméjean and coworkers tracked charts of 2,571 patients who had been assessed for their caries risk. At baseline they were identified as having low, moderate, high or extreme caries risk.24 At a follow-up examination roughly 1.5 years later (16 ± 13 months), new cavitated lesions, radiographic lesion into dentin or approximal enamel lesions on X-rays were registered, and their occurrence was closely related to the earlier assigned risk level; among low risk patients, 24% developed those disease indicators, while disease occurrence was higher in each category of greater caries risk: moderate 39%, high 69%, and extreme 88% (Figure 1). These patients had not received the appropriate preventive measures,24 and they consequently developed new caries lesions.
Figure 1.
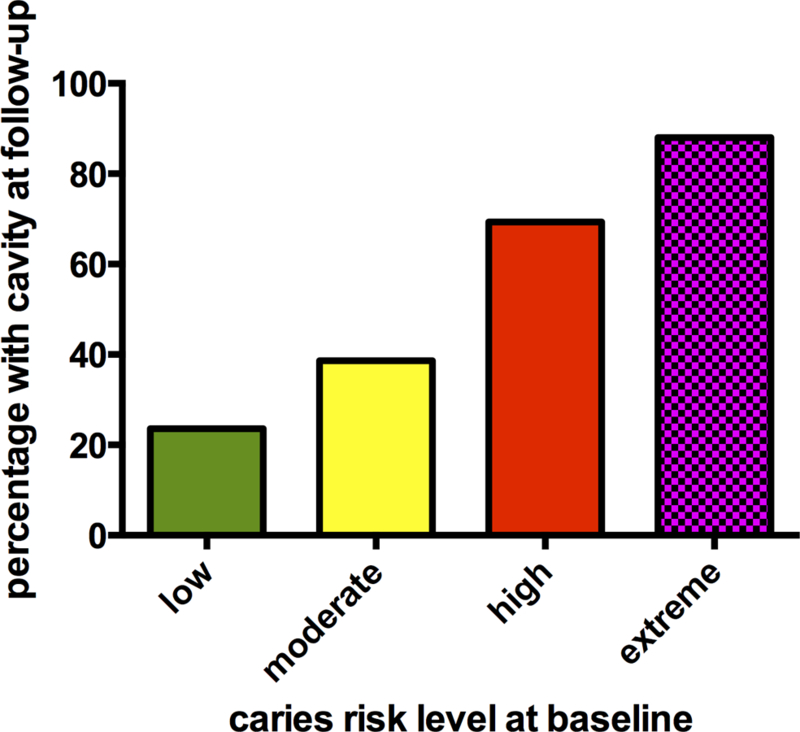
Percentage of patients with new cavities at follow up separated into low, moderate, high, and extreme high caries risk level at baseline (patients had not received the appropriate preventive measures); generated from Domejean S, White JM, Featherstone JD. Validation of the CDA CAMBRA caries risk assessment--a six-year retrospective study. J. Calif. Dent. Assoc. 2011;39(10):709–715.
In another outcomes study, Chaffee and coworkers reported and confirmed that baseline caries risk is strongly associated with future caries.25 From 18,004 patient charts with 4,468 recall visits at the UCSF student dental clinics, they found that the originally assigned risk level predicted the mean number of newly decayed or filled teeth (DFT) that patients developed: low risk patients showed a DFT increase of 0.94 at recall, and at each higher risk level, patients developed higher DFT values. Between each risk category changes in DFT increment were statistically significant, with extreme risk patients having an increment of 3.26 DFT between baseline and recall.25
In another electronic records study of 2,724 patients with follow-up at the UCSF School of Dentistry, Chaffee and coworkers reported the effectiveness of anti-caries agents, including 5,000 ppm fluoride toothpastes, chlorhexidine rinse, and xylitol. They showed that patients who had received any of these agents twice or more over 18 months had developed a 20% lower increase of decayed or filled teeth over those who never or only once had received those anti-caries products (Figure 2).26
Figure 2.
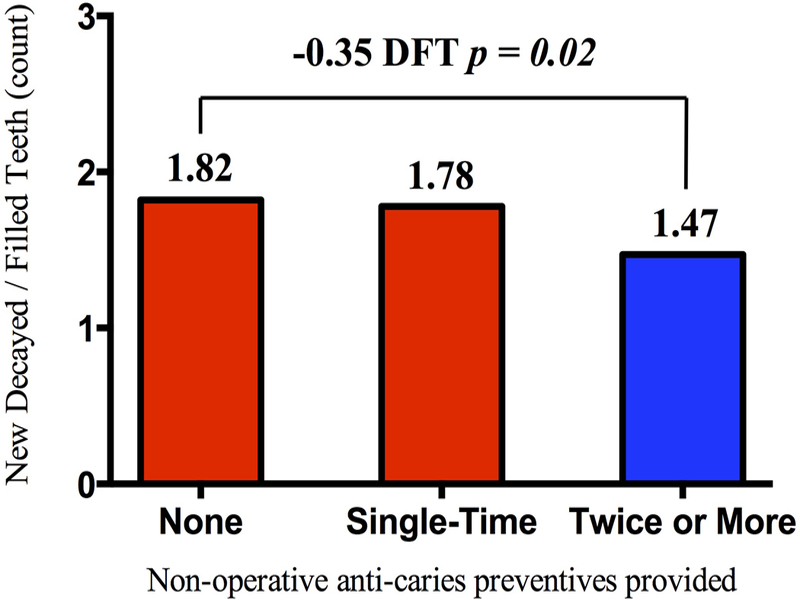
Number of new decayed/filled teeth of patients who received none, a single-time, and twice or more often anti-caries preventives; a 20% reduction in new decayed/filled teeth over 18 months in the group receiving twice of more anti-caries preventives was shown. (adapted from BMC Oral Health. 2015;15(1):111)
The Caries Management By Risk Assessment – Practice Based Research Network study – CAMBRA-PBRN
The original UCSF-CAMBRA trial took place in a university dental school setting.4 In order to demonstrate that CAMBRA not only works in a university “ivory tower” but can also successfully be implemented in the “real world,” a Practice Based Research Network (PBRN) was created in the California San Francisco Bay Area. The idea behind performing studies in practice-based research networks is to engage dentists in studies that are directly related to daily clinical practice.27 PBRNs should advance both research and dental practice, through quality improvement.27,28 PBRN studies are meant to move scientific advances rapidly into daily practice and simultaneously provide structure for sharing of information between practitioners.29
The California Dental Association (CDA) was instrumental in establishing the San Francisco Bay Area network. The network was created to conduct a CAMBRA study in dental offices and health care centers. The basic goal of the CAMBRA-PBRN trial was to recruit 30 dentists to perform a two-year randomized, controlled, double-blind study involving around 30 patients per dental practice. The hypothesis to be tested was that caries management based on caries risk level assignment significantly reduces patient caries risk level and reduces the need for caries restorative treatment over two years compared to generally accepted standard-of-care.
Materials & Methods
Dentist recruitment, training, and calibration
San Francisco Bay Area dentists were invited by CDA newsletter advertisements and phone calls to attend information meetings about the CAMBRA-PBRN study. The California Dental Association organized one-day information sessions. During these sessions, study design, expected involvement of the dentists in conducting the study, and requirements to join the PBRN were explained. Based on a priori power calculations, it was determined that a sample size of 30 dentists to be recruited into the study would be sufficient. Before the main CAMBRA-PBRN study started a total of 30 dentists (13 female, 17 male) had joined. Three dentists were employed at three different Federally Qualified Health Centers (FQHC), and 27 were dental office owners.
A calibration study was performed in order to assure that all participating dentists would record oral conditions in the same detailed way30 in the main CAMBRA study and to assure that results could be compared among participating practices. In order to minimize inter-examiner variability in data gathering, including the assessment of caries risk, carious lesion classification, and recording of existing restorations, the study dentists were required to attend one training meeting and one calibration workshop. Training meetings and calibration workshops were offered on multiple dates and attended by three to eight dentists per session. The study examiners participated in the training and calibration sessions with other staff members of their dental practices to enhance understanding and support of the study with the entire patient care team. The UCSF Institutional Review Board (IRB) had approved the pre-study dentist calibration (IRB #10–04804).
The attendees were trained and calibrated in two caries classification systems that were later used in the main CAMBRA-PBRN study. First, they were trained in examining and correctly charting decayed, missing, filled tooth surfaces - the DMFS Index,31,32 following strict scoring rules. Since non-cavitated caries lesions in enamel can be managed by remineralization without restorative intervention,33,34 the dentists were also calibrated in classifying caries lesions at a non-cavitated stage.35 The International Caries Detection and Assessment System (ICDAS)35,36 offers criteria for scoring of non-cavitated lesions.37 The dentists were specifically trained to differentiate between sound (ICDAS 0), non-cavitated caries lesions (ICDAS 1 or 2) (Figure 3), and cavitated caries lesions (ICDAS 3 and above). This allowed the participating dentists to record consistent and detailed clinical findings in the main study.
Figure 3.
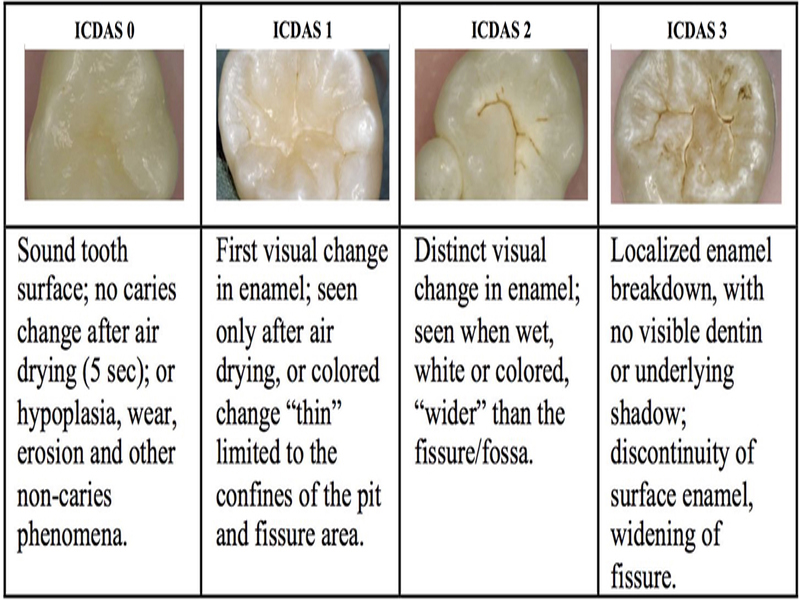
ICDAS scoring criteria for healthy (score 0), non-cavitated lesions (score 1 and 2) and first representation of a cavitated lesion (score 3) (adapted from BMC Oral Health. 2018;18(2))
Examinations occurred after the teeth were carefully cleaned (dental prophylaxis). Dentists performed a visual exam without tactile probing of enamel, using loupes with 2x magnification.
The 30 participating dentists were calibrated to a single gold standard examiner during the 6 calibration sessions.38 To determine the inter-examiner reliability with the gold standard an average of 13 or more patients per examiner were checked for DMFS and ICDAS. Each examiner scored between 1,036 and 2,220 tooth surfaces. To calculate the inter-examiner reliability, kappa statistics were used. All dentists achieved inter-examiner kappa values of >0.75 in comparison to the gold-standard examiner, with a mean inter-examiner kappa of 0.84 is considered as a ‘very good’ agreement with the gold standard. A ‘moderate’ kappa of 0.55 for agreement in non-cavitated lesions showed that this differentiation was more difficult and might require additional time and clinical education for future PBRN studies.39 For both indices, DMFS and ICDAS, inter-examiner reliability values achieved between the gold-standard examiner and future study examiners were at least as high as typically found in the literature and considered acceptable for high-quality dental assessments.40
Main study: eligibility criteria, enrollment, and treatment assignment
The UCSF Institutional Review Board (IRB) approved the main study (IRB #10–02153), and the study was registered on ClinicalTrials.gov (ID: NCT01176396). In the PBRN practices, potential patients were informed about the study goals, possible risks and participation requirements. UCSF’s Institutional Review Board had classified the study as minimal risk. When inclusion and exclusion requirements were fulfilled, the patients were finally consented (signing a written consent).
Of the 30 calibrated dentists who went through training and calibration, only 21 (11 female and 10 male) recruited patients for the study. Of those, three dentists were employees of a FQHC and 18 were practice owners.
After all existing restorative needs of a patient were met, the patient’s DMFS and ICDAS scores were recorded in Denticon, a web-based dental charting program (Planet DDS, Inc., Irvine, CA). Caries risk assessments with disease indicators, risk factors, protective factors, and patient’s caries risk level were also calculated with and recorded in Denticon, at baseline and at each recall visit, planned for 6, 12, 18, and 24 months after the initial risk assessment. In a 2014 study, dental university instructors had been asked to complete CRA forms for simulated patient cases and demonstrated only moderate reliability to assign caries risk levels in accordance with a gold-standard assessor.41 In that study, high caries risk cases were frequently categorized (erroneously) at low or moderate caries risk. Goolsby and Young confirmed similar findings.42,43 To reduce such risk level misclassification in the PBRN trial, a digital system was developed at UCSF41 that required information input about clinical findings and answers to questions found on CDA’s caries risk assessment form.44,45 The system automatically assigned risk level following an algorithm modeled after the way a gold-standard assessor and two experienced clinical instructors had assigned caries risk in the UCSF quality assurance study.41
For each caries risk level (i.e., low, moderate and high caries risk), randomization lists had been provided to help PBRN dentists to randomize their patient to the “active intervention” group or the “standard of care” control group. Providers were blinded to actual group assignment, which appeared on the randomization lists as two different colors: black or white. Extreme risk patients were excluded from the study due to ethical reasons (to avoid withholding anti-caries therapies). Intervention group products and recommendations were based on CAMBRA guidelines.19,45 Table 1 itemizes the provided products for each caries risk level, separated into “intervention” and “control” treatment. Patient participants, as well as all members of the dental practice, including the dentist, were blinded to actual group assignment. All products were covered with black or white wraps with printed user instructions on each product; thus, brand name and product content could not be identified. Products were given to the participant in black and white product bags, comprising all products suggested for the specific risk level. Patients received sufficient product supplies to last 6 months and were instructed to request more, if needed. Each product bag included laminated instruction sheets on how to use the products at home.
Table 1.
Dispensed treatment products based upon the assessed caries risk level for the intervention and the control group, respectively.
| Group assignment / products at risk level | Low Risk | Moderate Risk | High Risk | |||||
|---|---|---|---|---|---|---|---|---|
| Intervention group | Crest cavity protection (P&G) (1,100 ppm F) 2x daily | Crest cavity protection (P&G) (1,100 ppm F) 2x daily | Ortho wash rinse (3M ESPE) (0.05% F), daily | Xylitol candies (Epic) 4x/day (8 grams) | Clinpro 5000 (3M ESPE) (5,000 ppm F toothpaste) | Peridex (3M ESPE) Chlorhexidine gluconate (0.12%) rinse 1/day for 1 week, every month* | Xylitol candies (Epic) 4x/day (8 grams) | Vanish (3M ESPE) F-varnish |
| Control group | Crest cavity protection (P&G) (1,100 ppm F) 2x daily | Crest cavity protection (P&G) (1,100 ppm F) 2x daily | Crest Scope rinse (P&G) (mint taste), daily | Sorbitol candies (Epic) 4x/day (8 grams) | Crest cavity protection (P&G) (1,100 ppm F) 2x daily | Crest Scope rinse (P&G) (mint taste),
1/day for 1 week, every month* |
Sorbitol candies (Epic) (8 grams) 4x/day (8 grams) | Placebo varnish (3M ESPE) |
until the next periodic oral exam, then reassess
Finally, participants were schedule for a recall every 6 months for the 2-year study duration. The high caries risk patients received a phone call from the PBRN practice a week before a new calendar month started. During this phone call, patients were reminded to use their dispensed rinse for the first week of the month (1-minute rinse, 60 minutes after brushing teeth each evening). In addition, each PBRN practice was reminded by the UCSF study coordinator (BR) to place those reminder phone calls.
Of the 21 PBRN practices actively recruiting patients into the study, all data from one office were excluded from the final analysis (19 participants). The office did not follow recruitment, recall, and data collection instructions. The remaining 20 dentists enrolled 460 eligible patients. The eligibility criteria to be included in data analysis were: a baseline CRA was performed and assignment to the “black” or “white” group was recorded in the computer chart. Each practice enrolled a mean of 23.0±16.8 patients with a range from 2 to 55 patients.
CAMBRA-PBRN Study Results
At enrollment, of the 460 eligible patients, 192 patients were at low caries risk, 26 at moderate, and 242 were assessed as having high caries risk. Of the high-risk patients, 137 were randomly assigned to the intervention and 105 to the control group. For the low caries risk patients, 93 were assigned randomly to the intervention and 99 to the control (Figure 4). At baseline, the intervention and control group were not statistically significantly different in mean age (37 years intervention; 35 years control), and gender (69% female intervention; 68% female control). By chance, of the 242 baseline high caries risk patients, more (n=137) were assigned to the intervention group (57%) than to the control group (P=0.05).
Figure 4.
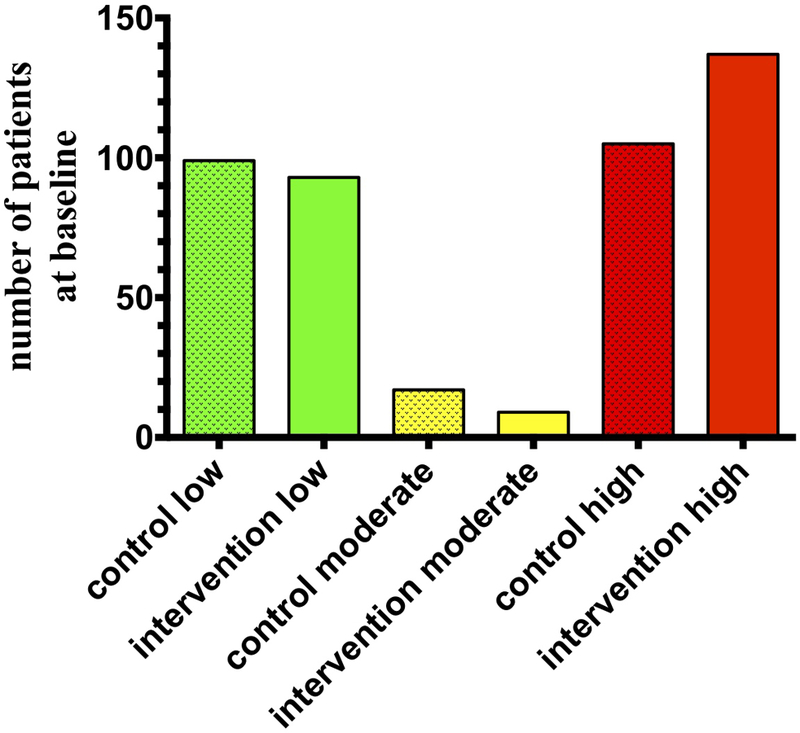
Number of eligible patients at baseline, separated into caries risk levels and assignment to control and intervention group treatment.
High caries risk
Table 2 illustrates the number and percentage of participants which at baseline were classified as having high caries risk. The table also shows for each follow-up visit, in total and by treatment group assignment, how many patients were still classified at high risk. The follow-up rate for the intervention group was 58.4% at 6-months, 50.4% at 12-months, 39.4% at 18-months and at 24-months 32.1%. For the control group the follow-up rates were similar (54.3%, 44.8%, 39.0%, and 37.1%, respectively). In total, 151 initially high-risk participants came to at least one follow-up visit with 85 (62.0% follow-up) in the intervention and 66 (62.9% follow-up) in the control group.
Table 2.
Caries risk category at baseline and follow-up visits, according to baseline caries risk and treatment group assignment.
| Total | Intervention Group | Control Group | |||||
|---|---|---|---|---|---|---|---|
| high caries risk at baseline | visit | n | Stay at high-risk: n | n | Stay at high-risk: n | n | Stay at high-risk: n |
| baseline | 242 | 137 | 105 | ||||
| 6-mo | 137 | 92 | 80 | 49 (61.3%) | 57 | 43 (75.4%) | |
| 12-mo | 116 | 60 | 69 | 30 (43.5%) | 47 | 30 (63.8%) | |
| 18-mo | 95 | 32 | 54 | 13 (24.1%) | 41 | 19 (46.3%) | |
| 24-mo | 83 | 32 | 44 | 11 (25.0%) | 39 | 21 (53.8%) | |
| low caries risk at baseline | visit | n | Change to moderate or high-risk: n | n | Change to moderate or high-risk: n | n | Change to moderate or high-risk: n |
| baseline | 192 | 93 | 99 | ||||
| 6-mo | 136 | 12 | 64 | 5 (7.8%) | 72 | 7 (9.7%) | |
| 12-mo | 126 | 14 | 56 | 3 (5.4%) | 70 | 11 (15.7%) | |
| 18-mo | 112 | 11 | 53 | 2 (3.8%) | 59 | 9 (15.3%) | |
| 24-mo | 85 | 15 | 36 | 4 (11.1%) | 49 | 11 (22.5%) | |
For patients classified at baseline as high caries risk (upper rows) or low caries risk (lower rows), the number of patients that remained high risk (upper rows) or changing to moderate or high risk (lower rows) are shown according to assigned treatment group.
Figure 5 shows for participants assessed as having high caries risk at baseline the percentage staying at high risk, separately at each recall. Over the two years the percentage of patients that stayed at high caries risk was lower in the intervention than the control group, with just 25% of participants staying at high caries risk in the intervention group at the 24-month recall. Interestingly, the percentage of high caries risk participants was also reduced over time for the control group down to 54% staying at high risk. Nevertheless, for all recall time points differences between the two groups were statistically significant (overall significance P<0.001).
Figure 5.
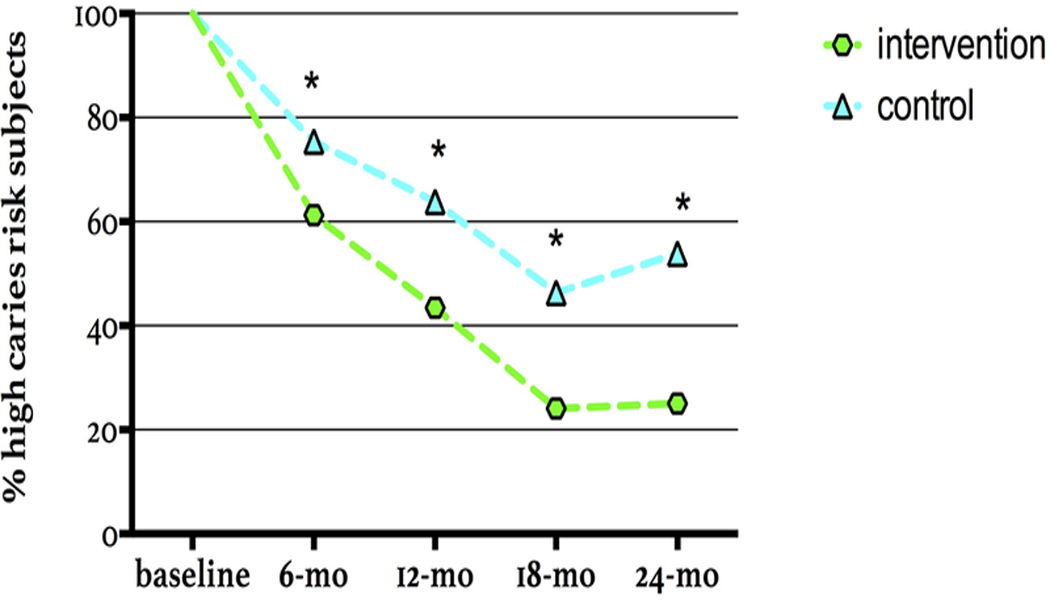
Change in caries risk levels for patients assessed as high caries risk at baseline; showing the percentage of patients staying at high risk over time for the intervention and the control group.
(* marks statistically significant difference at specific recall time point; overall significance P<0.001)
Low caries risk
Table 2 shows at each follow-up visit, in total and by treatment group, the number and percentage of patients, who at the beginning of the study were classified as having low caries risk and then later were assessed as increasing their risk level to moderate or high risk. For the intervention group the follow-up rate was 68.8% at 6-months, 60.2% at 12-months, 57.0% at 18-months, and finally at 24-months 38.7%. The follow-up rates for the controls were 72.7%, 70.7%, 59.6%, and 49.5%, respectively. In total, 154 initially low-risk participants provided data from at least one follow-up visit, with 73 (78.5% follow-up) patients in the intervention and 81 (81.8% follow-up) in the control group.
Figure 6 shows the percentage of patients who changed their caries risk level from low at baseline to a higher caries risk at recalls. Only a small percentage converted to high caries risk over time. At the 18-month recall, 3.9% of the intervention and 18.0% of the control group were assessed as having moderate or high caries risk, the difference being statistically significant (P=0.05) (Figure 6). The difference between intervention and control group was not significantly different at any other individual time point. Over the entire study period, the percentage of participants changing their caries risk from low to moderate or high was significantly lower in the intervention group (P=0.03).
Figure 6.
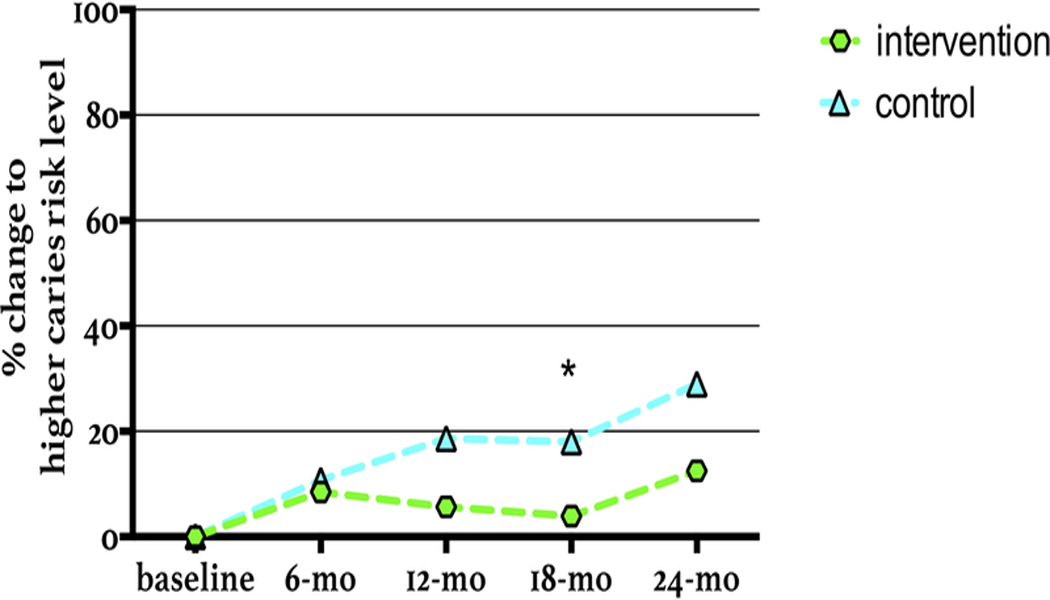
Percentage of participants classified as low caries risk at baseline, showing increased caries risk level to moderate or high caries risk, over time for intervention and control group (* marks statistically significant difference at specific recall time point).
Clinical outcomes - disease indicators
In this CAMBRA-PBRN trial the number of new fillings due to caries was very low in both groups. For this reason, we looked further into the registered disease indicators: namely, visually or radiographically observed cavities into dentin, proximal enamel lesions, restorations due to caries in the last year, and active white spot lesions at each recall time point with a white spot lesion defined as active, if the surface appeared chalky and considered as non-active, if the surface was shiny. These disease indicators include cavities and account for other signs of the existence of the caries disease. Consequently, they give a broader view of the caries situation of a patient. Figure 7 represents the percentage of initially high-risk patients demonstrating newly registered disease indicators. The percentage of newly developed disease indicators decreased over time in both study groups. At all recall time points the percentage of patients with newly registered disease indicators was lower for patients in the intervention than for those in the control group. These differences were statistically significant at the 12- and 18-month recall visits. The intervention group showed new disease indicators in only 46% and 31% at the 12- and at the 18-month recall, respectively, while in the control group 64% and 53%, respectively, had developed new disease indicators. The overall statistical significance for differences between intervention and control group was P=0.04 (Figure 7).
Figure 7.
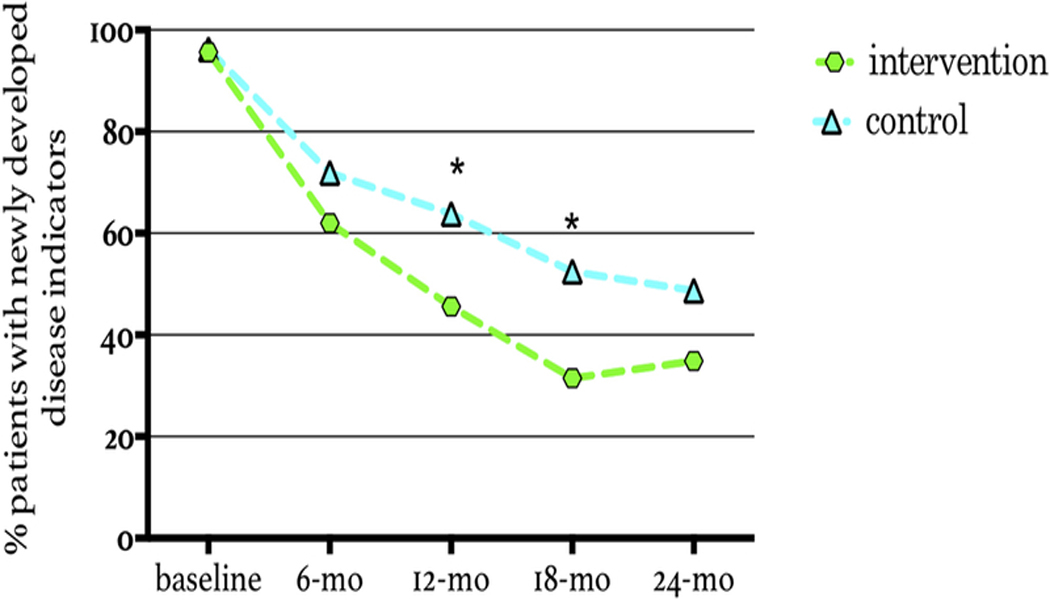
Percentage of patients with initial high risk at baseline developing any of the 4 clinical outcomes/disease indicators (cavities on radiographic into dentin, proximal enamel lesions on radiographs, active white spot lesions on smooth surfaces, restorations within prior year). *Percentages statistically significant different (cluster-adjusted P < 0.05) newly developed disease indicators (* marks statistically significant difference at specific recall time point).
Discussion
To study whether CAMBRA can be successfully implemented outside a structured university setting,4 a practice-based research network was created in the San Francisco Bay Area. Thirty dentists were enrolled to perform a two-year, randomized, controlled, double-blind clinical CAMBRA trial in their practices. The dentists were trained and calibrated to assess caries risk, score the conventional DMFS index, and use the ICDAS clinical scoring system.
The first UCSF-CAMBRA trial included only patients who were high caries risk at the study start.4 In that study, the chemical therapy (OTC fluoride toothpaste daily, OTC F mouth rinse daily, and 0.12% chlorhexidine gluconate mouth rinse once a day for one week every month) in the intervention group resulted in significantly lower numbers of patients at high caries risk over time. In the intervention group 50% to 70% of participants stayed at high caries risk, and in the control 70% to 90%. In contrast, in the present CAMBRA-PBRN study, only 25% of the participants in the intervention group and 54% of the control group remained at high caries risk after two years (Figure 5). Nevertheless, at all recall intervals, differences between control and intervention group in percentage of patients remaining at high risk were statistically significant.
Impressively, the percentage of high-risk participants remaining at this risk level during subsequent visits was much lower in the present CAMBRA-PBRN study than in the first UCSF-CAMBRA trial. There might be several reasons: for instance, in the UCSF-CAMBRA study 5000ppm prescription toothpaste was not available at that time, thus only 0.12% chlorhexidine plus OTC fluoride rinse (0.05% NaF) and OTC fluoride toothpaste (1,100ppm F-paste) were provided as intervention products. High caries risk participants assigned to the intervention in the CAMBRA-PBRN study received a combination of prescription 5000ppm F-paste, chlorhexidine rinse, xylitol mints, and fluoride varnish. In the UCSF-CAMBRA study, the control group “continued their usual products” – they did not receive any products. In the present PBRN study, the control group participants all received standard-of-care products. It is likely that these products contributed to the observed risk level reduction in this control group. The control products heightened saliva flow (sorbitol candies) and in addition might have had bactericidal effects (cetylpyridinium chloride rinse). Thus, the participants’ risk level in the control group was also dramatically reduced, unlike in the UCSF-CAMBRA study. Another important factor in the present study was that participants in both groups were called monthly to remind them to use their products. Most participants were also patients of record in private practices and, presumably, had ongoing personal relationships with the providers. Therefore, it is likely that compliance was much better in this study than in the university-based original UCSF-CAMBRA study, in which the primary providers were students in the predoctoral clinic, and the patients’ compliance may have been poor.
As a plausible consequence of using saliva-enhancing mints and other potentially beneficial products in the control group in the present study, newly developed diseases indicators (ongoing caries measures, as described above) decreased for both the intervention and control treatment groups. Nonetheless, the percentage of newly developed diseases indicators for participants in the intervention was lower than for those in the control group. Fewer newly developed disease indicators unmistakably establish a reduced manifestation of the caries disease, which is expressed by radiographically observed cavities into dentin, proximal enamel lesions, restorations due to caries in the last year, and active white spot lesions (Figure 7). Only 30–35% of intervention group patients and 50–55% in the control group, had new caries indicators at 18–24 months, whereas in the original CAMBRA study this number was about 55–60% in the intervention group and about 70–75% in the control group. Recorded disease indicators strongly determine the caries risk level of patient. Consequently, the monitored reduction in numbers of participants with high caries risk parallels the declined percentage of newly developed disease indicators.
In contrast to the original UCSF-CAMBRA study, the CAMBRA-PBRN not only enrolled high caries risk patients but also studied patients at moderate or low caries risk. The hypothesis was that provision of chemical therapy, including OTC fluoride rinse and xylitol products to moderate risk patients would prevent increases to high risk status over time. However, at baseline, few patients (5.7% of the total sample) were classified at moderate risk, and thus, there were insufficient numbers to allow assessment as a separate category. Among initially low-risk patients, as expected, only a small percentage showed an increased caries risk over time. This finding provides evidence that the initial low risk assignment was correct. The small number with increase in caries risk level at 24-months might have resulted from changes in participant behaviors or other risk or protective factors. At the 18-month visit a statistically significantly difference between groups was observed despite the fact that both intervention and control low-risk patients received the same prevention study products (1100 ppm F toothpaste).
All of the above discussion points are based upon the observed data for study participants who returned for further visits and examinations. As in all studies, as the study progresses, some participants do not return for further examination, or only return for some visits, not all. It is interesting to speculate that all of the no-show patients did not return because they were no longer at high risk and no longer felt they needed to seek dental care.
Conclusion
Thirty dentists as potential participants in a CAMBRA-PBRN trial were trained and calibrated successfully in DMFS and ICDAS-scoring. The inter-examiner reliability to a gold standard was high. The high inter-examiner reliability showed that dentists who work in their own primarily non-research practices can be successfully trained and calibrated in data collection, based on specific guidelines created to anticipate potential research study scenarios. However, separate reliability for assessment of non-cavitated lesions, as in other studies, was lower.
In this CAMBRA-PBRN study with clinical practices outside of a university setting it was demonstrated that the principles and philosophy of CAMBRA could be successfully implemented into dental practice, with dramatic reductions in caries risk and in the development of new caries clinical indicators. Twenty dentists of the network successfully completed the 2-year CAMBRA trial. The randomized, controlled, parallel-arm, double-blind clinical trial with individual-level caries risk assignment of 460 patients to standard of care as control versus active CAMBRA treatment as intervention demonstrated that caries risk level, as well as caries disease indicators, were significantly reduced in the CAMBRA intervention group compared to the controls at all recall time points.46
Acknowledgement
This study is a Principal Investigator Initiated Study and was funded in part by PacifiCare/UnitedHealthcare, DentaQuest, and the California Dental Association through the University of California, San Francisco’s Contracts & Grants Division. We acknowledge Proctor & Gamble, 3M Espe, and Epic for providing us at no cost or reduced cost with products for the participants. NIH-NCATS (grant KL2TR001870) supported B.W.C. We thank Planet DDS for adjusting the patient charting program to our needs. The authors are extremely thankful to the following dentist and their staff, who supported and performed the CAMBRA-PBRN trial in their practices: Drs. Pam Alston, Lawrence Bartlett, Susan Caliri, Marianela Carter, Tamara Clauson, Elizabeth Demichelis, Zarin Ferdowsi, Jan Gabus, Theresa Hall, Ted Hochstein, Nate Kaufman, Gordon Lai, Vince Lim, Ellen Pacleb, Curtis Raff, Andrew Rowe, Gayatri Sakhrani, Allen Sio, Norma Solarz, and Cathrine Steinborn.
Footnotes
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Disclosure:
There is no conflict of interest to report.
Contributor Information
Peter Rechmann, University of California, San Francisco, School of Dentistry, Department of Preventive and Restorative Dental Sciences, and Director of Clinical Sciences Research Group..
Benjamin W. Chaffee, University of California, San Francisco, School of Dentistry, Department of Preventive and Restorative Dental Sciences..
Beate M.T. Rechmann, University of California, San Francisco, School of Dentistry, Department of Preventive and Restorative Dental Sciences..
John D. B. Featherstone, University of California, San Francisco, School of Dentistry..
References
- 1.Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJL, Marcenes W. Global Burden of Untreated Caries:A Systematic Review and Metaregression. J Dent Res 2015;94(5):650–658. [DOI] [PubMed] [Google Scholar]
- 2.Berkowitz RJ. Mutans streptococci: acquisition and transmission. Pediatric Dentistry Mar-Apr 2006;28(2):106–109; discussion 192–108. [PubMed] [Google Scholar]
- 3.Marsh PD. In Sickness and in Health-What Does the Oral Microbiome Mean to Us? An Ecological Perspective. Adv Dent Res February 2018;29(1):60–65. [DOI] [PubMed] [Google Scholar]
- 4.Featherstone JD, White JM, Hoover CI, et al. A randomized clinical trial of anticaries therapies targeted according to risk assessment (caries management by risk assessment). Caries Res 2012;46(2):118–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brantley CF, Bader JD, Shugars DA, Nesbit SP. Does the cycle of rerestoration lead to larger restorations? J Am Dent Assoc October 1995;126(10):1407–1413. [DOI] [PubMed] [Google Scholar]
- 6.Featherstone JDB, Roth JR. Cariology in the new world order: Moving from restoration toward prevention. J Calif Dent Assoc 2003;31(2):123–124. [Google Scholar]
- 7.Featherstone JD. The caries balance: contributing factors and early detection. J Calif Dent Assoc February 2003;31(2):129–133. [PubMed] [Google Scholar]
- 8.Anderson MH, Bales DJ, Omnell KA. Modern management of dental caries: the cutting edge is not the dental bur. J Am Dent Assoc June 1993;124(6):36–44. [DOI] [PubMed] [Google Scholar]
- 9.Loe H Changing paradigms in restorative dentistry. J Am Coll Dent Fall 1995;62(3):31–36. [PubMed] [Google Scholar]
- 10.Featherstone JD. The caries balance: the basis for caries management by risk assessment. Oral Health Prev Dent 2004;2 Suppl 1:259–264. [PubMed] [Google Scholar]
- 11.Vidnes-Kopperud S, Tveit AB, Espelid I. Changes in the treatment concept for approximal caries from 1983 to 2009 in Norway. Caries Res 2011;45(2):113–120. [DOI] [PubMed] [Google Scholar]
- 12.Rechmann P, Domejean S, Rechmann BM, Kinsel R, Featherstone JD. Approximal and occlusal caries lesions: Restorative treatment decisions by California dentists. J Am Dent Assoc February 9 2016;147(5):328–338. [DOI] [PubMed] [Google Scholar]
- 13.Mertz-Fairhurst EJ, Curtis JW Jr., Ergle JW, Rueggeberg FA, Adair SM. Ultraconservative and cariostatic sealed restorations: results at year 10. J Am Dent Assoc January 1998;129(1):55–66. [DOI] [PubMed] [Google Scholar]
- 14.Walsh LJ, Brostek AM. Minimum intervention dentistry principles and objectives. Aust Dent J June 2013;58 Suppl 1:3–16. [DOI] [PubMed] [Google Scholar]
- 15.Tassery H, Levallois B, Terrer E, et al. Use of new minimum intervention dentistry technologies in caries management. Aust. Dent. J June 2013;58 Suppl 1:40–59. [DOI] [PubMed] [Google Scholar]
- 16.Domejean S, Leger S, Maltrait M, Espelid I, Tveit AB, Tubert-Jeannin S. Changes in Occlusal Caries Lesion Management in France from 2002 to 2012: A Persistent Gap between Evidence and Clinical Practice. Caries Res June 24 2015;49(4):408–416. [DOI] [PubMed] [Google Scholar]
- 17.Young DA, Featherstone JD, Roth JR. Curing the silent epidemic: caries management in the 21st century and beyond. J Calif Dent Assoc October 2007;35(10):681–685. [PubMed] [Google Scholar]
- 18.Young DA, Featherstone JD, Roth JR, et al. Caries management by risk assessment: implementation guidelines. J Calif Dent Assoc November 2007;35(11):799–805. [PubMed] [Google Scholar]
- 19.Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc October 2007;35(10):714–723. [PubMed] [Google Scholar]
- 20.Domejean-Orliaguet S, Gansky SA, Featherstone JD. Caries risk assessment in an educational environment. J Dent Educ December 2006;70(12):1346–1354. [PubMed] [Google Scholar]
- 21.Featherstone JDB, Gansky SA, Hoover CI, et al. Chlorehexidine and fluoride therapy reduces caries risk. J Dent Res 2005;84 (Spec Iss A, abstract 0023). [Google Scholar]
- 22.Hoover CI, Weintraub JA, Gansky SA, White JM, Wilson RS, Featherstone JDB. Effect of a caries management regimen on cariogenic bacterial population. J Dent Res 2004;83 (Spec Iss A, abstract 0779). [Google Scholar]
- 23.Ismail AI, Pitts NB, Tellez M, et al. The International Caries Classification and Management System (ICCMS) An Example of a Caries Management Pathway. BMC Oral Health 2015;15 Suppl 1:S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Domejean S, White JM, Featherstone JD. Validation of the CDA CAMBRA caries risk assessment--a six-year retrospective study. J. Calif. Dent. Assoc October 2011;39(10):709–715. [PubMed] [Google Scholar]
- 25.Chaffee BW, Cheng J, Featherstone JD. Baseline caries risk assessment as a predictor of caries incidence. J Dent May 2015;43(5):518–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaffee BW, Cheng J, Featherstone JD. Non-operative anti-caries agents and dental caries increment among adults at high caries risk: a retrospective cohort study. BMC Oral Health 2015;15(1):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Makhija SK, Gilbert GH, Rindal DB, et al. Dentists in practice-based research networks have much in common with dentists at large: evidence from the Dental Practice-Based Research Network. Gen Dent May-Jun 2009;57(3):270–275. [PMC free article] [PubMed] [Google Scholar]
- 28.Mold JW, Peterson KA. Primary care practice-based research networks: working at the interface between research and quality improvement. Ann Fam Med May-Jun 2005;3 Suppl 1:S12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lenfant C Shattuck lecture--clinical research to clinical practice--lost in translation? N Engl J Med August 28 2003;349(9):868–874. [DOI] [PubMed] [Google Scholar]
- 30.Nelson S, Eggertsson H, Powell B, et al. Dental examiners consistency in applying the ICDAS criteria for a caries prevention community trial. Community Dent Health September 2011;28(3):238–242. [PubMed] [Google Scholar]
- 31.Klein H, Palmer CE, Knutson JW. Studies on Dental Caries. I. Dental Status and Dental Needs of Elementary School Children. Pub Health Rep 1938;53(19):751–765. [Google Scholar]
- 32.World-Health-Organization. Oral Health Surveys: Basic Methods Vol 5th Edition: World Health Organization; 2013. [Google Scholar]
- 33.Baelum V, Machiulskiene V, Nyvad B, Richards A, Vaeth M. Application of survival analysis to carious lesion transitions in intervention trials. Community Dent Oral Epidemiol August 2003;31(4):252–260. [DOI] [PubMed] [Google Scholar]
- 34.Sbaraini A, Evans RW. Caries risk reduction in patients attending a caries management clinic. Aust Dent J December 2008;53(4):340–348. [DOI] [PubMed] [Google Scholar]
- 35.Ismail AI, Sohn W, Tellez M, et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol June 2007;35(3):170–178. [DOI] [PubMed] [Google Scholar]
- 36.ICDAS. Rationale and Evidence for the International Caries Detection and Assessment System (ICDAS II) International Caries Detection and Assessment System (ICDAS) Coordinating Committee 2005. 2005/2012.
- 37.Pitts N “ ICDAS”--an international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent Health 2004;21(3):193. [PubMed] [Google Scholar]
- 38.Rechmann P, Jue B, Santo W, Rechmann BMT, Featherstone JDB. Calibration of dentists for Caries Management by Risk Assessment Research in a Practice Based Research Network - CAMBRA PBRN. BMC Oral Health January 4 2018;18(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thompson VP, Schenkel AB, Penugonda B, et al. A pilot study of dentists’ assessment of caries detection and staging systems applied to early caries: PEARL Network findings. Gen Dent May-Jun 2016;64(3):20–27. [PubMed] [Google Scholar]
- 40.Braga MM, Oliveira LB, Bonini GA, Bonecker M, Mendes FM. Feasibility of the International Caries Detection and Assessment System (ICDAS-II) in epidemiological surveys and comparability with standard World Health Organization criteria. Caries Res 2009;43(4):245–249. [DOI] [PubMed] [Google Scholar]
- 41.Rechmann P, Featherstone JD. Quality assurance study of caries risk assessment performance by clinical faculty members in a school of dentistry. J Dent Educ September 2014;78(9):1331–1338. [PubMed] [Google Scholar]
- 42.Goolsby SP, Young DA, Chiang HK, Carrico CK, Jackson LV, Rechmann P. The Effects of Faculty Calibration on Caries Risk Assessment and Quality Assurance. J Dent Educ November 2016;80(11):1294–1300. [PubMed] [Google Scholar]
- 43.Young DA, Fa BA, Rogers N, Rechmann P. The Effect of Calibration on Caries Risk Assessment Performance by Students and Clinical Faculty. J Dent Educ 2017;in press. [DOI] [PubMed]
- 44.Featherstone JD, Adair SM, Anderson MH, et al. Caries management by risk assessment: consensus statement, April 2002. J Calif Dent Assoc March 2003;31(3):257–269. [PubMed] [Google Scholar]
- 45.Featherstone JD, Domejean-Orliaguet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc October 2007;35(10):703–707, 710–703. [PubMed] [Google Scholar]
- 46.Rechmann P, Chaffee BW, Rechmann BMT, Featherstone JDB. Changes in Caries Risk in a Practice-Based Randomized Controlled Trial. Adv Dent Res February 2018;29(1):15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]


