Abstract
Objective:
Adolescent and young adults’ (AYAs) involvement in advance care planning and end-of-life discussions may enhance the decision-making process, reduce stress and improve the patient’s quality of life. Given the importance of establishing adequate communication and having culturally-appropriate tools to introduce advance care planning, our paper will describe the cross-cultural adaptation of the advance care planning guide, Voicing My CHOiCES™ in Australia and in Brazil.
Methods:
In Brazil, the process involved initially translating the document to Portuguese followed by evaluation by a group of providers and patients (aged 18–39) undergoing cancer treatment. The document was revised based on the feedback received, then back-translated to English and discussed with Voicing My CHOiCES™’ authors to refine the final version in Portuguese. In Australia, a multi-perspective interview-based study was undertaken with AYA cancer patients/survivors (aged 15–25), siblings, parents, and a range of healthcare providers from the oncology setting, to determine the perceived acceptability of the tool within the Australian clinical context.
Results:
These interviews pointed to a variety of recommended adaptations ranging from the aesthetic and linguistic, through to the re-structuring of content within the tool. Adaptations for the Australian setting were then revised in an iterative capacity within several focus groups of AYA participants and healthcare providers.
Conclusions:
The processes used in both countries highlight ways to engage youth living with a life-limiting illness in conversations about advance care planning and how to develop culturally-appropriate clinical tools.
Keywords: advance care planning, culturally competent care, decision-making, cancer, end-of-life
Introduction
Increasing data support the capability of adolescents to participate in healthcare decision-making, starting at diagnosis and extending through the illness trajectory, which for some includes end-of-life (EoL) care (Hinds et al., 2005). Adolescents’ active participation in EoL discussions and the respect for their preferences may help them enhance their decision-making process, manage uncertainty, reduce stress, develop realistic priorities, and improve their quality of life (Lyon, McCabe, Patel, & D’Angelo, 2004; Zadeh, Pao, & Wiener, 2014, Mack & Joffe, 2014). While there has been a growing emphasis for early integration of palliative concepts and advance care planning as part of pediatric oncology care (Institute of Medicine [IOM], 2013; IOM, 2015; Wiener, Zadeh, Wexler, & Pao, 2013; Weaver et al., 2015), the EoL needs of seriously ill adolescents and young adults (AYAs) and their families remain under-addressed in the existing literature.
Moreover, considerably less attention has been provided to the cultural aspects of EoL care in the AYA population including the need to better understand the meanings attributed to the disease and death in a specific culture, as well as the patient’ values and preferences of care (Wiener, McConnell, Latella, & Ludi, 2013). Relatedly, consideration for differences in how healthcare providers communicate to patients and families also need to be taken into account.
Different cultures differ in their expectations of the medical system, beliefs and attitudes about patient care and disease causation, and attitudes about death and rituals around death (Wiener, McConnell, Latella, Ludi, 2013; Wiener, Reader, & Kazak, 2015; Wiener, Alderfer, & Pao, 2015). Understanding, respecting and responding to these differences are vital during vulnerable periods, such as when a young person learns that his/her disease has progressed and at times when EoL care is being considered. Also critical is the need to explore and respond appropriately to how decisions are made within the family. For some cultures, information about important health care decisions are made by the elder in the family (Lipson et al., 1997; Mazanec & Tyler, 2003; Matthews et al., 2006) while for others, information is shared with community members who then assists with decisions pertaining to a child (Olsen et al., 2007). Familial and cultural differences often exist as to whether the young person should be present when difficult information is presented and whether the prognosis should be shared (Mazanec & Tyler, 2003; Brolley, Tu, & Wong, 2007; Cardenas, Garces, Johnson, Montes, & West, 2007). Without appreciating cultural norms and customs, conflict between the family and medical team can emerge and the young person’s care compromised.
Within the United States (US), shared decision-making is an increasingly used process for pediatric medical decision-making (Wyatt et al., 2015). This process is dependent on collaborative communication and the exchange of information between the medical team and the family. For shared decision-making to be effective, it is important for family members to share information regarding their goals and values so that care decisions can meet these needs and address each stakeholder’s perception of the disease process (Katz, Webb, Committee on Bioethics, 2016). Adolescents or older children living with a life-limiting illness often have the capacity to participate in decision-making when weighing the benefits and burdens of continued treatment, especially when the likelihood of a good prognosis is low (Pousset et al., 2009; Stegenga & Ward-Smith, 2008; Quinn et al., 2011; Miller et al., 2013; Hinds et al., 2005). In reality, however, how decisions are made is informed by the cultural, social, and religious diversity of physicians, patients, and families (Katz, Webb, Committee on Bioethics, 2016). Content and quality of conversations pertaining to prognosis, continued treatment, and preferences for EoL care can vary significantly between different providers and their adolescent patients.
Listening to the preferences of AYA who are living with a potentially life-limiting disease about how they want to be supported and cared for, where they wish to die, who they would like to have their belongings and how they would like to be remembered after their death should be given careful consideration by parents and the health care team. Understandably, discussing poor prognosis, progressive disease, and EoL care poses challenges for all involved. Nonetheless, engaging youth in cultural-appropriate conversations about advance care planning is critical for shared decision-making and open communication to occur.
Fortunately, there now exists a research-generated planning guide, Voicing My CHOiCES™, that allows AYAs the ability to document their preferences (Wiener et al, 2008; Wiener et al, 2012). This tool was initially developed in collaboration with youth living with cancer and HIV, as an adaptation of the adult advance care planning tool, Five Wishes™ (https://www.agingwithdignity.org/). Following focus groups and individual interviews with 90 AYAs (ages 16–28), the tool adapted sections addressing preferences for issues around medical decision-making and treatment choices, including life support (e.g., ‘Who I want to make my medical care decisions if I cannot make them on my own’), sections addressing preferences for comfort care and socio-emotional support when in pain, or upset (e.g., ‘How I want to be comforted’), expressing their wishes and preferences around their legacy and memory should they die from their disease (e.g., ‘How I wish to be remembered’), and sections addressing other values, wishes and preferences (e.g., ‘What I would like my family and friends to know about me’,) (Wiener et al., 2008; 2012; Zadeh et al., 2014). This tool has been translated into Spanish and Italian; however, until recently, it had not been evaluated in terms of its cultural appropriateness within other cultures and countries. Only by considering the cultural climate of the AYAs’ home, community and country, and the unique cultural needs of different clinical contexts, can such a document be successfully implemented.
Given the importance of having culturally-appropriate tools to introduce advance care planning, this paper describes the cross-cultural adaptation process for the planning guide, Voicing My CHOiCES™, within two different countries. The article presents key themes that emerged in each cultural context and identifies opportunities for other countries when considering the cross-cultural adaptation process of a clinical tool.
Methods
Having a thorough understanding of the cultural context of the country for which a tool will be created or adapted, is an important methodological first step. This phase preceded the process taken to adapt Voicing My CHOiCES™ in both Brazil and Australia. Part of this process involves careful consideration of whether there are important subgroups with different resources within each country and for these studies, how useful and acceptable an advance care planning tool would be in each setting. Table 1 highlights key socio-demographic information and cultural differences between Brazil and Australia that inform how EoL communication with young people takes place.
Table 1.
Cultural Context for Introducing Advance Care Planning for Adolescents and Young Adults
| Brazil | Australia | |
|---|---|---|
| Population | 190 million | 23. 4 million |
| Race/Ethnicity* | White (47.7%) Multiracial, (43.1%) Black (7.6%) Asian (1.1%) Indigenous (0.4%) |
English (25%) Australian (23.3%) Irish (7.6%) Scottish (6.4%) Chinese (3.9%) Aboriginal/Torres Strait Islander (2.8%) |
| Religion | Catholic (64.6%) Evangelical (22%) Other religions (5%) No religion (8%) |
No religion (30.1%) Catholic (22.6%) Anglican (13.3%) Uniting Church (3.7%) Islam (2.6%) Buddhism (2.4%) |
| Overall cancer diagnoses in AYA** | 236.16 cases per million (Brazil, 2016) | 419 cases per million (AIHW, 2011) |
| Cancer survival in AYA | 65%*** | 88%**** |
| Decision-making | Family-level discussions/consultations in both pediatric and adult treatment settings | Family-level discussions/ consultations in pediatric***** treatment settings, individual patient consultations (typically together with a partner/support person/caregiver) in adult treatment settings |
| Models of Care | Multidisciplinary approach; Transition from
paternalist to shared-decision making model |
Multidisciplinary approach; Shared-decision making model |
Notes. The statistic refers to the reported race/ethnicity, in Brazil (Brazil, 2012) and to the reported ancestry, in Australia (Australian Bureau of Statistics, 2017).
Age-standardized rate, for AYAs aged 15–29 years old.
Estimate survival for all cancers in AYAs aged 15–29 years old (Brazil, 2016).
5-year relative survival. This high survival rate is in part due to the prevalence of melanoma, which is the most prevalent cancer diagnosis among Australian AYAs, and has a 96% 5-year relative survival rate in Australia. A number of other cancers continue to experience poorer survival rates in Australia including central nervous system cancers (e.g., glioblastoma, anaplastic astrocytoma: 5-year relative survival rates of 41%) and rhabdomyosarcoma; 5-year relative survival of 49%).
For a newly diagnosed cancer patient, typically Australian pediatric hospitals cease admitting adolescents after the age of 17 years, though this may differ according to particular institutions’ policies, the type of cancer/presentation the adolescent presents with, and their access to different treatment options at a pediatric versus adult hospital site.
In approaching cross-cultural adaptations, we also needed to consider the different definitions of “AYAs” based on programs and country; for example, in the US, the National Cancer Institute (NCI) defines AYAs as young people aged 15–39 whereas this differs from a range of other westernized, developed nations (e.g., Australia: 15–25 years; UK: 13–24; US: 15–39; Canada: 15–29; Aubin et al., 2015). Given the variety of definitions around the age of an “AYA”, understanding how advance care planning may best occur across countries required investigations that attend to the cultural and social differences that exist for AYAs in those locations. While Australian AYA services/organizations support AYA cancer patients aged 15–25 years, in Brazil no formal definition was available when the study began. Consequently, the investigators chose to use the NCI definition. Considering that advance care planning is a new concept in Brazil, the NCI age range (15–39) allowed for a broader examination of the tool’s appropriateness.
Cultural Context
In Brazil, there are approximately 236.16 cases per million AYAs aged 15–25 years 1 diagnosed with cancer annually (Brazil, 2016). Diagnosis and treatment are provided in specialized cancer centers and, usually, patients under 18 years old are treated by pediatric oncology teams, whereas those over the age of 18 are followed by adult clinical oncology teams (Martins, Balmant, Silva, Santos, Reis, & Camargo, 2017). In 2014, a national recommendation established that a multidisciplinary approach is the gold standard for oncology care within the Brazilian Universal Health System (Brazil, 2014). Since this time, most oncology centers offer a multidisciplinary team approach for all patients with cancer and their families.
Family plays an important role in patients’ care and health-related decision-making, regardless of the patient’s age. Commonly, patients want to have their family informed about diagnosis and treatment options, which stresses the importance of having medical decisions discussed and made at the family-level, rather than at an individual patient-level (Gulinelli et at, 2004). Brazil is experiencing a shift paternalist model of care to an informed decision-making model, where the medical information is discussed, and patients’ autonomy and preferences are documented. The notion of shared decision-making is still new in Brazil, and initiatives have been established to enhance patient/population education and improve provider-patient-family relationship and communication quality (Abreu et al, 2011).
In Australia, approximately 1000 AYAs aged 15–25 years are diagnosed with cancer annually (Australian Institute of Health and Welfare [AIHW], 2018). Many AYAs within this age group (>18 years) will be treated in adult hospitals. The Australian Youth Cancer Services (YCS), established in 2008, provides multidisciplinary, age-appropriate clinical care in metropolitan centers across Australia for patients/survivors aged 15–25 years; this supplements the care provided by existing pediatric and adult cancer services (CanTeen Australia, 2017). Consequently, while the model of care (i.e., how family-focused/oriented it is) still depends largely on where the AYAs are treated (pediatric vs. adult sector), the Australian YCS model supports the age-appropriate autonomy of AYAs throughout psychosocial aspects of their care (e.g., through the use of AYA-focused psychosocial assessments and care plans).
As a westernized nation, Australia’s culture is more individualistic than collectivist in nature (Browne & Chan, 2012; Bornstein et al., 2007). However, models of care differ between pediatric and adult hospital centers: Australian pediatric hospitals, like those in the US, deliver a very family-focused model of care, with parents involved in all consultations and medical decision-making. As patients become older (i.e., into the adolescent years) they become increasingly included in these consultations, to the extent that they wish and in line with their maturity (Sanci et al., 2004; McCarthy et al., 2017). Adult medical care in Australia has been heavily influenced by the ‘shared decision-making’ movement that has been seen across many westernized, developed nations (Trevena et al, 2017; Hoffmann et al., 2014). However, it remains unclear how these models may be delivered differently with AYA patients (either in the pediatric or adult sectors), and particularly with regards to EoL conversations.
The Cross-Cultural Adaptation Process of Voicing My CHOiCES™
The cross-cultural adaptation of any measure, tool, or document for use in a new country, culture, and/or language requires being translated linguistically, but also being adapted to maintain the content validity of the instrument at a conceptual level across different cultures. Another essential step is to reach equivalence between the original and target versions of the document (Guillemin, Bombardier, & Beaton, 1993, Beaton, Bombardier, Guillermin, & Ferraz, 2000; International Test Commission [ITC], 2016). Beaton and colleagues (2000) recommend that different approaches are considered depending on the target scenario and how much it differs from the original source language and culture. For example, our studies required different procedures: in Brazil, the process included the translation to Portuguese and attention to cultural differences and adaptations needed, and in Australia, since English is the official language, it focused on investigating what cultural and language adjustments were needed (Figure 1). Each study focused on assessing the cultural appropriateness of the tool for the prevalent culture and official language in each country at the outset, to establish the initial utility of the tool for clinical use broadly prior to evaluating with other minority groups/cultures and secondary languages. We present here the most up-to-date multi-perspective data from across both Brazilian and Australian studies, for the purposes of illustrating how cross-cultural adaptation was undertaken in collaboration with different stakeholders/participant groups in each country.
Figure 1.
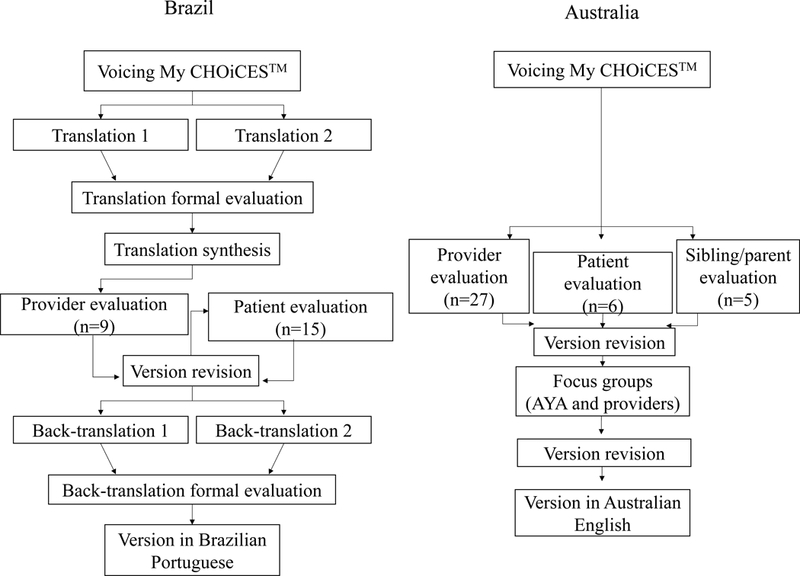
Flow chart of the steps followed for the cross-cultural adaptation process of Voicing My CHOiCES™ in Brazil and Australia.
Obtaining the target-population feedback during the cross-cultural adaptation process was critical to ensure appropriate linguistic and cultural adaptations in both countries (Borsa, Damasio, & Bandeira, 2012). IRB approval was obtained in both countries (Brazil: FFCLRP-USP process CAEE 54503216.8.0000.5407 and HC-FMRP-USP process CAEE 4503216.8.3001.5440; Australia: HREC ref no: 15/198).
Language Translation
In Brazil, the translation process involved two independent bilingual translators translating the document to Portuguese. Each translation version was submitted for a formal analysis. A 4-point scale was used ranging from “unaltered” to “very altered” to rate the similarity of the translated version with the original document in English, considering the global meaning of each item. The scientific committee created a synthesis document by prioritizing items with less modification compared with the English version and those that better expressed the original content (considering both technical terminology and language appropriateness for AYAs). In Australia, the original American English-language based tool was used as the basis for the multi-perspective evaluations undertaken.
Tool Evaluation
In Brazil, providers with experience with cross-cultural adaptation of tools and oncology care critically reviewed each page of the synthesized version of Voicing My CHOiCES™ in Portuguese and were invited to answer a questionnaire about the document’s structure, relevance, and appropriateness across oncology care settings. Once wording revisions were made, the document was introduced to AYAs aged 18–39 undergoing cancer treatment in face-to-face sessions. The AYAs read each page of the document and rated the perceived appropriateness, helpfulness, and stressfulness of the items, as well as if they would change, take out or add words and/or content, using the same questionnaire and Likert scale response format used in earlier phases of the development of the tool (Wiener et al, 2008, 2012). Additionally, participants were asked whether they found the content and wording to be age- and culturally-appropriate. Based on the feedback received, this version of Voicing My CHOiCES™ was revised and submitted to back-translation to English. The back-translations and all feedback received were then discussed with Voicing My CHOiCES™’ authors.
In Australia, a multi-perspective interview-based study was undertaken with AYA cancer patients/survivors (aged 15–25), siblings, parents, and a range of oncology healthcare providers to determine the perceived acceptability of the tool within the Australian clinical context. First, individuals from each of these groups were guided through a semi-structured interview process one-on-one, modeled on the questionnaire used during the tool’s development studies (Wiener et al, 2008, 2012), in which they provided feedback regarding the perceived appropriateness, helpfulness, and stressfulness of each section of Voicing My CHOiCES™. They were also invited to offer suggestions as to ways in which they might change each of these sections (by changing, adding, or removing content). Next, adaptations for the Australian setting were revised in an iterative capacity, within two separate focus groups, one with AYA participants and another with healthcare providers (further focus groups are underway).
Across both Brazilian and Australian studies, quantitative data was analyzed by descriptive statistics. Qualitative data was analyzed by content analysis. This strategy involved reading the full material to obtain a general idea of the content, the identification of emergent themes, followed by the development of a coding tree (Miles & Huberman, 1985; Elo & Kyngäs, 2008; Vaismoradi, Turunen & Bondas, 2013). Two independent coders each generated prominent themes relevant to EoL communication experiences, and the utility of the Voicing My CHOiCES tool. These were then discussed and agreed upon jointly to create a coding dictionary. From there, the responses were then independently coded and then checked for accuracy by the two investigators who met regularly to review the coding process. Discrepancies in coding were reviewed with an additional coder.
In both studies, the sample size was determined a priori, driven by a combination of pragmatic and local clinical-environmental factors. In Brazil, participants’ enrollment aimed to have a consistent representation of participants in terms of gender and different age groups, considering the wide age-range in this study. The Australian study used a purposive sample of different AYA healthcare providers, patients/survivors, and parents/siblings. We anticipate that continuing to recruit AYAs and parents/siblings (10–15 each) will yield thematic saturation. Given the relatively small numbers of AYAs with cancer in Australia, and the novelty of exploring best-practice EoL communication tools, these modest samples will still provide ample useful evidence to refine the Australian tool and allow us to demonstrate the process of adaptations in a variety of settings.
Results
Language translation
Both versions in Portuguese were considered similar to the original Voicing My CHOiCES™, with most items rated as “unaltered” and “a little altered”. The only item rated as “very altered” was for “My spiritual thoughts and wishes”, which used “spirituality” instead of “spiritual thoughts”. A synthesis version was created and used for the following tool evaluation.
Tool evaluation: Healthcare providers’ feedback
In Brazil, a group of nine providers composed of physicians, psychologists, a nurse and a lawyer, with mean professional experience of 23 years in oncology or in advance directives (range: 10–43 years), evaluated and revised the tool. Next, a social worker and a hospital clinical director were interviewed about specific aspects of the tool, such as the Brazilian Universal Health System and practical aspects of preferences of care documentation in Brazil, considering patients’ rights and medical profession regulation/law.
Using a 4-point scale ranging from “inadequate” to “totally adequate”, providers evaluated the document’s structure, relevance of topics covered and appropriateness of use across settings as “totally adequate” or “adequate”. Better wording choices for the translated version were suggested, based on language used in health care settings and by this age-group. Adaptations specific to the Brazilian Universal Health System and culture, and legal considerations were also suggested. Table 2 provides examples of suggested changes within each category.
Table 2.
Examples of Suggested Adaptations by Theme
| Brazil | Australia | |
|---|---|---|
| Linguistic | - suggestion to substitute ‘honor your wishes’ by ‘consider your wishes’ (more colloquial tone) | - differences in most commonly-used term e.g.,
tracheotomy vs. tracheostomy
(adjusted to the correct terminology in Australian English) - suggestion to substitute ‘what gives me joy’ by ‘what makes me happy’ (more colloquial tone) |
| Cultural | - rewording ‘When my
end-of-life is near” to “When the moment that the end
of my life is near arrives” (less direct approach to
end-of-life care) - remove references to ‘memorial services’ and ‘celebration of life’ (not relevant to Brazilian culture) |
- rewording elements of the section on
‘Religious/spiritual beliefs’ e.g.,
remove references to ‘asking/giving
forgiveness’ (due to considerations that this may either
be confronting, confusing or irrelevant for a more secular Australian
AYA population) - expand options for different religious figures in the section on the section on ‘Religious/spiritual beliefs’ (e.g., including ‘Imam’ for Muslim patients) (to account for a more diverse and different range of religious/cultural communities in Australia) |
| Health system | - remove references to
‘Medicaid’ (not relevant to Brazilian
health system) - differences in the definition of “benefits” (adjusted to the Brazilian health system context) |
- remove references to ‘Medicaid’, or ‘hiring or firing health care providers’ (not relevant to Australian public health system) |
| Legal | - keep information about emergency care, but remove direct reference to the ‘Do Not Resuscitate order’ (not relevant to Brazilian health system) | - include prompts to consider formalized/legal clinical processes and documentation in the Australian setting to ensure that the young person’s decision is legally-binding and actually acted upon (such as ‘not for resuscitation’ or ‘NFR’ forms, “No CPR” orders and ambulance plans, as well as a legal will) (to enhance utility within Australian healthcare system) |
In Australia, a group of 27 healthcare providers evaluated the tool. They were a diverse sample, representing medical, nursing, and allied health disciplines at all levels of seniority, from both pediatric and adult hospital sectors. In order to be eligible for the study, each professional had to have cared for at least one AYA who had died from cancer, although most had provided care for greater than 15 who had died. The sample had a mean number of 17 years’ working with AYAs with cancer (range: 5–30).
The Australian providers were generally very receptive to, and positive about, the potential for the tool’s use within AYAs clinical care in Australia. Healthcare providers rated each of the tool’s sections from “not at all helpful” to “very helpful”. Across all sections of the tool, over 85% of the health providers reported that all topics were at least “helpful” or “very helpful”. All sections were identified as being appropriate for AYAs with cancer, with the exception of the section on designating an agent for medical decision-making, which was not endorsed as appropriate by one medical professional. All sections were rated at least “a little stressful” by 88% of providers, with the section on wishes for types of life support being rated as “stressful” to “very stressful” by the majority. A variety of recommended adaptations were generated from these interviews; these ranged from the aesthetic and linguistic, through to the re-structuring of content within the tool (Table 2). Australian providers particularly raised the importance of the tool, more clearly prompting young people to discuss certain topics with their clinical care team (e.g., life support and other medical care options).
Tool evaluation: Adolescent and young adults’ feedback
In Brazil, 15 young adults between 18–39 years of age (mean age = 28.7) undergoing cancer treatment reviewed the revised document. The enrolled participants were balanced in terms of gender (53% male) and age groups (33.3% of 18–24 years old, 20% of 25–29 years old, 20% of 30–34 years old and 26.6% of 35–39 years old). Further information on patients’ characteristics is presented in Table 3. Over 80% considered all topics covered to be age and culturally-appropriate. Similarly, over 80% of the participants found all the topics to be “very helpful” or “helpful” except for the section that addresses funeral planning, which only 53% described as helpful and was also rated as being “very stressful” (33.3%). One participant highlighted how different funeral services are performed in Brazil, compared to the US. In Brazil, there are rarely speeches from family and friends. Funerals usually follow a pattern, which starts with a viewing of the body, followed by burial or cremation, and, sometimes, a religious eulogy. Also, there are no “memorial services” or a “celebration of life”, terms used in Voicing My CHOiCES™. Interestingly, participants’ feedback focused more on how to incorporate the tool into the treatment trajectory, than on language or legal considerations. They emphasized the importance of voicing their choices on care preferences, psychosocial support and family care throughout the cancer trajectory, not limited to EoL.
Table 3.
Patient Demographic and Clinical Characteristics
| Brazil (n=15) | Australia (n=6) | |
| Age (mean; range) | 28.67 years; 19–38 | 20.67 years; 16–24 |
| Sex | 46.6% female | 83.3% female |
| Religion | Catholic (n=5), Evangelical (n=4), Spiritism (n=1), Jehovah’s witness (n=1), Candomble (n=1) and no religion (n=3) | (Not collected) |
| Diagnosis | acute lymphoblastic leukemia (n=5), sarcoma of the bone (n=3), carcinoma (n=2), osteosarcoma (n=1), acute myeloid leukemia (n=1), Hodgkin’s lymphoma (n=1), adenocarcinoma (n=1), anaplastic ependymoma (n=1) | sarcoma of the bone (n=2), Hodgkin’s lymphoma (n=2), acute myeloid leukemia (n=1), brain cancer (n=1) |
| Time since diagnosis (mean; range) | 1.6 years; 0.2–10.1 | 4.5 years, 1–8 |
In Australia, a purposive sample of six AYAs aged 15–25 years old have also provided feedback on the American tool to date (data collection ongoing). They were all cancer survivors, treated for a range of cancer diagnoses between 15–19 years of age (Table 3). Similar to the Brazilian sample, Australian AYAs reviewed the document very positively in terms of its appropriateness, and also on average between ‘a little’ and ‘somewhat’ stressful to consider. They had fewer suggested revisions to the tool than did the healthcare providers, however a few suggested simplifying the medical terminology, and providing additional space and options for scenarios in several sections (e.g., adding options to specify who you want around you when you are in a particular mood, or how much information you want about medical procedures).
Discussion
Several important steps were taken to culturally adapt the advance care planning guide, Voicing My CHOiCES™ in Brazil and Australia. This included maintaining the content validity of the instrument at a conceptual level across the two different cultures and assuring equivalence between the original document and target versions of the document were reached. Having AYAs’ feedback during the cross-cultural adaptation process was critical to ensure appropriate linguistic and cultural adaptations in both countries.
Across our studies, the adapted versions of Voicing My CHOiCES™ were found to be a helpful tool to introduce EoL conversations for both the Brazilian and Australian populations, from health professionals and patients’ perspectives. Despite the many unique elements that emerged regarding EoL communication within each culture, such as the presentation of legal terms and how to word “When my end-of-life is near”, some common themes emerged. Health professionals and AYAs alike recognized that youth of this age face unique and complex psychosocial challenges that require tailored, age-appropriate methods of communication. Further, despite the distinct recommended adaptations within each culture, both Brazilian and Australian providers shared enthusiasm for the possibility of having an appropriate tool to guide difficult, but important conversations, in timely and sensitive ways.
Healthcare providers and AYAs alike found items within Voicing My CHOiCES™ stressful, particularly making medical care decisions and after death (e.g. funeral) planning. AYAs need assistance in making these types of decisions, and healthcare providers often report feeling unprepared to have those difficult conversations, in a timely, language appropriate and sensitive manner (Weaver et al., 2015; Wiener et al, 2013). Internationally, numerous opportunities remain to tailor or adapt tools such as Voicing My CHOiCES™ to better support AYAs living outside of countries such as the US, where such tools have often been developed. Our Australian study demonstrates that even other English-speaking, developed countries are likely to differ in subtle, but important cultural ways. Adapting culturally-appropriate advance care planning tools for AYAs with cancer and other potentially life-limiting conditions using the processes described here is just the first step to improving communication around these challenging topics. Future work is still needed to support these culturally-appropriate tools with additional training for healthcare providers, to better equip them with the skills, confidence, and language to navigate this terrain. Better understanding how shared decision-making with AYAs is occurring in each culture and the extent to which the patient is involved in decisions pertaining to EoL care, is also still needed. Additionally, studying the process of implementing advance care planning into routine clinical practice within different cultures is essential.
The processes described here are subject to a number of limitations. While these studies describe world-first efforts towards developing culturally- and age-appropriate advance care planning tools for youth with cancer in Australia and Brazil, we must acknowledge that both countries are diverse in terms of their cultural make-up and that the cultural adaptations at this point have catered primarily towards only the most prevalent culture in each country. For example, in Brazil, although Portuguese is the only official language, there are important variation of language use, cultural aspects, social-economics and health resource disparities within the country. In Australia, as noted, 21% of the population speak a language other than English at home, and 26% were born overseas (Australian Bureau of Statistics, 2017; de Witt et al, 2017). Existing research and clinical reports suggest that each of these cultures are likely to have unique and distinct perspectives on the content, nature, and timing of any EoL conversations that may occur with AYAs with cancer (Wiener et al, 2013; Rosenberg, Wolfe, Wiener, Lyon, & Feudtner, 2016). Additionally, 2.8% of Australians identify as Aboriginal or Torres Strait Islander, the first peoples of Australia, hereafter respectfully referred to as Indigenous Australians (Australian Bureau of Statistics, 2017; de Witt et al, 2017). Indigenous Australians report a range of unique beliefs around EoL, dying, funeral customs, and the afterlife (McGrath, Phillips, & Fox-Young, 2008; McGrath & Phillips, 2008a; McGrath & Phillips, 2008b; Shahid, Finn, Bessarab, & Thompson, 2009). This study took a pragmatic approach with a view to first establishing the general utility and appropriateness of Voicing My CHOiCES™ for the prevalent cultures/languages in both Australia and Brazil. Whether or not the new Australian and Brazilian adaptations of Voicing My CHOiCES™ appropriately meet the needs of these groups warrants further study. The unique needs of specific cultural groups is an important consideration for clinicians hoping to adapt tools such as Voicing My CHOiCES™ in other countries in the future. Another limitation to note was the different age range of AYAs between the two studies. Future studies should examine the role of developmental differences within such a wide AYA age span. Finally, we recognize that AYAs who have completed therapy might view the items within an advance care planning guide differently than those currently undergoing treatment. From a methodological stand-point, these patient-sample differences (i.e., age, treatment stage) may make direct comparisons between these cohorts more complex; however, it is also crucial that efforts to understand and better support gold-standard EoL communication are made across a range of clinical contexts. While one’s personal situation with regards to cancer (e.g., whether or not an AYA is currently undergoing active cancer treatment, or their prognosis) may impact the extent to which they view such EoL conversations as personally useful, AYAs who have completed cancer treatment may in fact be able to consider these questions in a different, and somewhat more abstract way (given that it is less immediately emotionally-confronting to their own situation), and this may also be useful in assessing the developmental appropriateness (nested within the cultural appropriateness) of advance care planning tools. There is ample data to support the fact that AYAs may not only consider EoL concepts much earlier than the ‘palliative’ phase, they also have valuable perspectives on how they feel these conversations should happen (Lyon, McCabe, Patel, & D’Angelo, 2004; Zadeh, Pao, & Wiener, 2014, Mack & Joffe, 2014). Therefore, seeking out and incorporating the voices of a diverse range of AYAs across the cancer trajectory is an important step.
Conclusions
The EoL needs of AYAs and their families remain under-addressed in the existing literature. Engaging youth in culturally-appropriate advance care planning conversations across life-limiting illnesses is critical to advance these clinical aspects of the field. Limited resources exist to assist with such conversations. This paper describes the careful steps taken to maintain the content validity of an US-developed advance care planning guide for AYAs with a life-limiting illness in Brazil and Australia. The adapted versions of Voicing My CHOiCES™ were found to be a helpful tool to introduce EoL conversations for both the Brazilian and Australian populations. Further study with the final versions will evaluate the tool’s feasibility and identify potential burdens and benefits of its use. Adapting gold-standard interventions to suit the unique cultural needs of different clinical contexts is crucial to enabling both patients and healthcare providers to take ‘ownership’ of how these sensitive interactions unfold.
Implications for Impact Statement: Engaging youth living with a life-limiting illness in conversations about advance care planning is critical to ensure that goals of care are understood and respected. Adapting gold-standard interventions to suit the unique cultural needs of different clinical contexts is essential in order to enable both patients and their healthcare providers to take ‘ownership’ on how these sensitive interactions unfold. Closely examining the process of how two different cultures went through the cross-cultural adaptation of the planning guide, Voicing My CHOiCES™, provides guidance for others who may wish to adapt communication tools in the future.
Acknowledgement
This work is supported, in part, by the Intramural Research Programs of the NIH, National Cancer Institute, Center for Cancer Research. Ms. Marina N. F. Arruda-Colli is supported by Sao Paulo Research Foundation (FAPESP – grant number 2016/15269–3). Dr. Ursula Sansom-Daly is supported by Early Career Fellowships from the CINSW (ID: 14/ECF/1–11) and the National Health and Medical Research Council (ID: APP1111800) and her work conducting the Australian study examining Voicing My CHOiCES™ is supported by the HCF Foundation. The Behavioural Sciences Unit is supported by the Kids with Cancer Foundation, the Kids Cancer Alliance, and a Cancer Council New South Wales Program Grant (PG16–02) with the support of the Estate of the Late Harry McPaul. Dr. Manoel A. dos Santos is supported by the National Council for Scientific and Technological Development (CNPq - Brazil).
Footnotes
The Brazilian study used the NCI definition of an AYAand included patients up to 39 years old. Recently, new data about cancer incidence, mortalityand hospital morbidity in Brazil, specific to AYAs between the ages 15-25 were published and the investigators considered the more recent data to be more reliable to report in this manuscript.
No conflicts of interest declared.
References
- Abreu MM, Battisti R, Martins RS, Baumgratz TD, & Cuziol M (2011). Shared decision making in Brazil: history and current discussion. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen, 105(4), 240–244. 10.1016/j.zefq.2011.04.009 [DOI] [PubMed] [Google Scholar]
- Aubin S, Barr R, Rogers P, Schacter B, Bielack SS, Ferrari A, Manchester RA, McMaster K, Morgan S, Patterson M, Petrilli AS, Ribera J-M, Shaw P, Thomas DM, Treadgold C (2011). What Should the Age Range Be for AYA Oncology? Journal of Adolescent and Young Adult Oncology, 1(1), 3–10. doi: 10.1089/jayao.2011.1505 [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics (2017). ‘Australia’ Census QuickStats’. Retrieved from: http://www.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/036?opendocument
- Australian Institute of Health and Welfare (2018). Cancer in adolescents and young adults in Australia Cat. no. CAN 110. Canberra: AIHW. [Google Scholar]
- Beaton DE, Bombardier C, Guillemin F, & Ferraz MB (2000). Guidelines for the process of cross-cultural adaptation of self-report measures. SPINE, 25(24), 3186–3191. [DOI] [PubMed] [Google Scholar]
- Bornstein MH, Hahn CS, Haynes OM, Belsky J, Azuma H, Kwak K, … Toda S (2007). Maternal personality and parenting cognitions in cross-cultural perspective. International Journal of Behavioral Development, 31(3), 193–209. 10.1177/0165025407074632 [DOI] [Google Scholar]
- Borsa JC, Damásio BF, & Bandeira DR (2012). Cross-cultural adaptation and validation of psychological instruments: some considerations. Paidéia (Ribeirão Preto), 22(53), 423–432. 10.1590/S0103-863X2012000300014 [DOI] [Google Scholar]
- Brazil (2012). Censo demográfico 2010: Características gerais da população, religião e pessoas com deficiência. Instituto Brasileiro de Geografia e Estatística: Rio de Janeiro, RJ, p.1–215. Retrieved from: https://biblioteca.ibge.gov.br/visualizacao/periodicos/94/cd_2010_religiao_deficiencia.pdf [Google Scholar]
- Brazil. Ministério da Saúde. Portaria nº 140, de 27 de Fevereiro de 2014. Retrieved from: http://www.sgas.saude.ms.gov.br/wp-content/uploads/sites/105/2016/08/Portaria-140-2014-UNACON.pdf
- Brazil. Ministério da Saúde (2016). Incidence, mortality and hospital morbidity for children, adolescents and young adults in Brazil: data from cancer registries and from the mortality system. Rio de Janeiro, RJ: Instituto Nacional do Câncer José Alencar Gomes da Silva. [Google Scholar]
- Brolley G, Tu A & Wong E (2007). Culture clues: Communicating with your Chinese patient: Patient and family education services at the University of Washington Medical Center. Retrieved from http://depts.washington.edu/pfes/CultureClues.htm.
- Browne JL, & Chan AY (2012). Mother-daughter communication about mammography in an Australian sample. Journal of family communication, 12(2), 129–150. 10.1080/15267431.2011.561144 [DOI] [Google Scholar]
- CanTeen Australia (2017). Australian youth cancer framework for adolescents and young adults with cancer. Retrieved from: https://www.canteen.org.au/wp-content/uploads/2017/09/Australian_Youth_Cancer_Framework_2017.pdf
- Cardenas D, Garces C, Johnson D, Montes K, & West L (2007). End of life care: The latino culture: Patient and family education services at the University of Washington Medical Center. Retrieved from http://depts.washington.edu/pfes/Culture-Clues.htm.
- de Witt A, Cunningham FC, Bailie R, Bernardes CM, Matthews V, Arley B, … & Walpole ET (2017). Identification of Australian Aboriginal and Torres Strait Islander cancer patients in the primary health care setting. Frontiers in Public Health, 5, 199 10.3389/fpubh.2017.00199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo S & Kyngäs H (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62, 107–115. [DOI] [PubMed] [Google Scholar]
- Guillemin F, Bombardier C; Beaton D (1993). Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. Journal of Clinical Epidemiology, 46(12),1417–1432. [DOI] [PubMed] [Google Scholar]
- Gulinelli A, Aisawa RK, Konno SN, Morinaga CV, Costardi WL … Martins MA (2004). Desire for information and participation in therapeutic decisions concerning severe diseases, in patients of a university hospital. Revista da Associação Médica Brasileira, 50(1), 41–47. [DOI] [PubMed] [Google Scholar]
- Hinds PS, Drew D, Oakes LL, Fouladi M, Spunt SL, Church C, & Furman WL (2005). End-of-life care preferences of pediatric patients with cancer. Journal of Clinical Oncology, 23(36), 9146–54. 10.1200/JCO.2005.10.538 [DOI] [PubMed] [Google Scholar]
- Hoffmann TC, Légaré F, Simmons MB, McNamara K, McCaffery K, Trevena LJ, …Del Mar CB (2014). Shared decision making: What do clinicians need to know and why should they bother?. The Medical Journal of Australia, 201(1), 35–39. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine [IOM] (2013). Identifying and addressing the needs of adolescents and young adults with cancer. Washington, DC: Institute of Medicine. [Google Scholar]
- Institute of Medicine [IOM] (2015). Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: Institute of Medicine. [DOI] [PubMed] [Google Scholar]
- International Test Commission [ITC] (2016). The ITC guidelines for translating and adapting tests (2nd edition). Retrieved from: www.InTestCom.org
- Katz AL, Webb SA, Committee on Bioethics (2016). Informed consent in decision-making in pediatric practice. Pediatrics, 138(2), e20161485. 10.1542/peds.2016-1485 [DOI] [PubMed] [Google Scholar]
- Lipson JG, Dibble SL, & Minarik PA (1997). Culture and nursing care: A pocket guide. San Francisco: UCSF Nursing Press. [Google Scholar]
- Lyon ME, McCabe MA, Patel KM, & D’Angelo LJ (2004). What do adolescents want? An exploratory study regarding end-of-life decision-making. Journal of Adolescent Health, 35(6), 529–e1–6.. 10.1016/j.jadohealth.2004.02.009 [DOI] [PubMed] [Google Scholar]
- Mack JW, & Joffe S (2014). Communicating about prognosis: Ethical responsibilities of pediatricians and parents. Pediatrics, 133(S1), S24–30. 10.1542/peds.2013-3608E [DOI] [PubMed] [Google Scholar]
- Martins HTG, Balmant NV, Silva NP, Santos MO, Reis RS, & Camargo B (2017). Who cares for adolescents and young adults with cancer in Brazil?. Jornal de Pediatria, in press. 10.1016/j.jped.2017.07.008 [DOI] [PubMed] [Google Scholar]
- Matthews RA, Del Priore RE, Acitelli LK, & Barnes-Farrell JL (2006). Work-to-relationship conflict: Crossover effects in dual-earner couples. Journal of Occupational Health Psychology, 11, 228–240. 10.1037/1076-8998.11.3.228 [DOI] [PubMed] [Google Scholar]
- Mazanec P, & Tyler MK (2003). Cultural considerations in end-of-life care—How ethnicity, age, and spirituality affect decisions when death is imminent. American Journal of Nursing, 103, 50–58. [DOI] [PubMed] [Google Scholar]
- McCarthy MC, McNeil R, Drew S, Orme L, & Sawyer SM (2017). Information needs of adolescent and young adult cancer patients and their parent-carers. Supportive Care in Cancer, 1–10. 10.1007/s00520-017-3984-1 [DOI] [PubMed] [Google Scholar]
- McGrath P, & Phillips E (2008a). Insights on end-of-life ceremonial practices of Australian Aboriginal peoples. Collegian, 15(4), 125–133. [DOI] [PubMed] [Google Scholar]
- McGrath P, & Phillips E (2008b). Aboriginal spiritual perspectives: research findings relevant to end-of-life care. Illness, Crisis & Loss, 16(2), 153–171. 10.2190/IL.16.2.e [DOI] [Google Scholar]
- McGrath P, Phillips E, & Fox-Young S (2008). Insights on Aboriginal grief practices from the Northern Territory, Australia. Australian Journal of Primary Health, 14(3), 48–57. [Google Scholar]
- Miles MB & Huberman AM (1985). Qualitative data analysis. Newbury Park, CA: Sage. [Google Scholar]
- Miller VA, Baker JN, Leek AC, Hizlan S, Rheingold SR, Yamokoski AD, … Kodish E (2013). Adolescent perspectives on phase I cancer research. Pediatric Blood & Cancer, 60(5), 873–8. 10.1002/pbc.24326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen P, Taualii M, Eteni L, et al. (2007). Culture clues: Communicating with your American Indian/Alaska Native patient: Patient and family education services at the University of Washington Medical Center. Retrieved from http://depts.washington.edu/pfes/CultureClues.htm
- Pousset G, Bilsen J, De Wilde J, Benoit Y, Verlooy J, Bomans A, … Mortier F (2009). Attitudes of adolescent cancer survivors toward end-of-life decisions for minors. Pediatrics, 124(6):e1142–e1148. 10.1542/peds.2009-0621 [DOI] [PubMed] [Google Scholar]
- Quinn GP, Murphy D, Knapp C, Stearsman DK, Bradley-Klug KL, Sawczyn K, & Clayman ML (2011). Who decides? Decision making and fertility preservation in teens with cancer: a review of the literature. The Journal of Adolescent Health, 49(4):e337–46. 10.1016/j.jadohealth.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg AR, Wolfe J, Wiener L, Lyon M, & Feudtner C (2016). Ethics, emotions, and the skills of talking about progressive disease with terminally ill adolescents: a narrative review. JAMA Pediatrics, 170(12), 1216–223. 10.1001/jamapediatrics.2016.2142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanci LA, Sawyer SM, Weller PJ, Bond LM, & Patton GC (2004). Youth health research ethics: time for a mature-minor clause?. Medical Journal of Australia, 180(7), 336–338. [DOI] [PubMed] [Google Scholar]
- Shahid S, Finn L, Bessarab D, & Thompson SC (2009). Understanding, beliefs and perspectives of Aboriginal people in Western Australia about cancer and its impact on access to cancer services. BMC Health Services Research, 9(1), 132 10.1186/1472-6963-9-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegenga K, & Ward-Smith P (2008). The adolescent perspective on participation in treatment decision making: a pilot study. Journal of Pediatric Oncology Nursing, 25(2), 112–117. 10.1177/1043454208314515 [DOI] [PubMed] [Google Scholar]
- Trevena L, Shepherd HL, Bonner C, Jansen J, Cust AE, Leask J, … Hoffmann T (2017). Shared decision making in Australia in 2017. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen, 123, 17–20. 10.1016/j.zefq.2017.05.011. [DOI] [PubMed] [Google Scholar]
- Vaismoradi M, Turunen H, & Bondas T (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing and Health Sciences, 15, 398–405. [DOI] [PubMed] [Google Scholar]
- Weaver MS, Heinze KE, Kelly KP, Wiener L, Casey RL, Bell CJ, … Hinds PS (2015). Palliative care as a standard of care in pediatric oncology. Pediatric Blood & Cancer, 62(S5), S829–S833. 10.1002/pbc.25695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener L, Alderfer M, & Pao M (2015). Psychiatric and Psychosocial Support for Child and Family In Pizzo PA & Poplack DG (Eds.) Principles and Practice of Pediatric Oncology (1124–1140). Philadelphia, PA: Lippincott. [Google Scholar]
- Wiener L, McConnell DG, Latella L, & Ludi E (2013). Cultural and religious considerations in pediatric palliative care. Palliative & Supportive Care, 11(1), 47–67. 10.1017/S1478951511001027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener L, Reader S, & Kazak AE (2015). Special considerations in working with families In: Wiener L, Pao M, Kazak AE, Kupst MJ & Patenaude AF, Arcici R (Eds.). Quick Reference for Pediatric Oncology Clinicians: The Psychiatric and Psychological Dimensions of Cancer Symptom Management (271–280). New York: Oxford University Press. [Google Scholar]
- Wiener L, Ballard E, Brennan T, Battles H, Martinez P, & Pao M (2008). How I wish to be remembered: the use of an advance care planning document in adolescent and young adult population. Journal of Palliative Medicine, 11(10), 1309–1313. 10.1089/jpm.2008.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener L, Zadeh S, Battles H, Baird K, Ballard E, Osherow J, & Pao M (2012). Allowing adolescents and young adults to plan their end-of-life care. Pediatrics, 130(5), 897–905. 10.1542/peds.2012-0663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener L, Zadeh S, Wexler LH, & Pao M (2013). When silence is not golden: Engaging adolescents and young adults in discussions around end-of-life care choices. Pediatric Blood & Cancer, 60(5), 715–718. 10.1002/pbc.24490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt KD, List B, Brinkman WB, Prutsky Lopez G, Asi N, … & LeBlanc A (2015). Shared decision making in pediatrics: A systematic review and meta-analysis. Academic Pediatrics, 15(6):573–83. 10.1016/j.acap.2015.03.011 [DOI] [PubMed] [Google Scholar]
- Zadeh S, Pao M, & Wiener L (2015). Opening end-of-life discussions: How to introduce Voicing My CHOiCES™, an advance care planning guide for adolescents and young adults. Palliative and Supportive Care, 13(3), 591–599. 10.1017/S1478951514000054 [DOI] [PMC free article] [PubMed] [Google Scholar]


