Abstract
The major papilla of Vater can be ectopically present in the stomach, pyloric canal, duodenal bulb, and third or fourth portion of the duodenum. In this study, we determined the clinical significance of ectopic papilla of Vater by endoscopic retrograde cholangiopancreatogram (ERCP).
A retrospective study was conducted by reviewing the medical records of 6133 patients receiving ERCP from 1988 to 2011. The diagnosis was confirmed if both the common bile duct (CBD) and the main pancreatic duct (PD) drained into the same opening, either by ERCP or magnetic resonance cholangiopancreatography.
Eight patients with major papilla of Vater in the duodenal bulb were identified among 6133 patients receiving ERCP from 1988 to 2011, with an incidence rate of 0.13%. The mean age was 67 years and patients were predominantly male. Duodenal bulb deformity was noted in all patients and three of them had shallow gastric and/or duodenal ulcers. Hook-shaped CBD configuration was seen only in half of our cases. Three patients with CBD stones were treated successfully after endoscopic sphincterotomy or papillary balloon dilation.
Ectopic orifice of papilla is a rare finding of ERCP. Opacification of both the CBD and main PD from the same opening is an essential criterion for diagnosing an ectopic papilla of Vater in the duodenal bulb.
Keywords: duodenal bulb, ectopic papilla of Vater, endoscopic retrograde cholangiopancreatography, magnetic resonance cholangiopancreatography, pancreatic opacification
1. Introduction
Pathology of biliary tract anatomy is commonly encountered and it can also present a considerable diagnostic and therapeutic challenge via endoscopic retrograde cholangiopancreatography (ERCP). One of the main challenges is the variability in the anatomy of the biliary system. The common bile duct (CBD) and the main pancreatic duct (PD) unite to form a short papilla of Vater, which typically enters into the posteromedial aspect of the second portion of duodenum at the summit of the major duodenal papilla.[1] However, atypical termination may also arise, with the CBD and PD draining into stomach, pyloric canal, duodenal bulb, or third or fourth portion of the duodenum.[2–13]
During ERCP, the endoscopist may be confused as to the location of the orifice of the papilla in patients with ectopic orifice of papilla. The usual location of the papilla is the second portion of the duodenum. Anatomic variance can lead to clinical pathology, and thus if a papilla is detected at an atypical site, this is a potential cause for concern, and in most cases of ectopic orifice of papilla, treatment is recommended.[10,14]
Most studies on ectopic orifice of papilla are case reports. One series reported a frequency of about 2% in Turkey.[10] The study observed that ectopic biliary drainage was combined with gastric outlet obstruction, which was thought to be due to peptic ulcer formation accompanied by cholangitis/cholestasis. More surveys on this condition need to be conducted worldwide, particularly in Asia. Thus, we conducted a retrospective case review and determined the clinical significance of ectopic orifice of papilla in our ERCP series.
2. Patients and methods
From 1988 to 2010, a total 6133 subjects received ERCP. The patients’ X-ray films and records of ERCP were retrospectively reviewed by the 2 authors at a gastrointestinal endoscopic unit in a single hospital. The medical records included 6133 patients, who received about 15,000 ERCP events performed by a single experienced endoscopist (WK Chow). This study was approved by the Institutional Review Board of our institution (CE-17014A).
Patients were included in the study if they met any of the following criteria. The inclusion criteria were as below:
-
a)
major papilla of Vater could not be located within the second portion of the duodenum;
-
b)
major papilla of Vater could be located over the duodenal bulb;
-
c)
opacification of CBD after contrast injection into the major papilla;
-
d)
main PD opacification from the same opening in the duodenal bulb, either by ERCP or magnetic resonance cholangiopancreatography (MRCP).
Medical and surgical history, as well as endoscopic, ERCP, and MRCP findings of patients with ectopic orifice of papilla were reviewed. The characteristics of the opening, CBD configuration, presence of biliary stones, and stone retrieval after sphincterotomy were also analyzed.
3. Results
3.1. Epidemiology and demographics
During 1988 to 2010, a total 8 of 6133 patients (i.e., incidence rate of 0.13%) receiving ERCP were diagnosed as having ectopic papilla of Vater in the duodenal bulb in this hospital-based study. The patients’ mean age was 67 years old, ranging from 45 to 77 years old, and males predominated (7 males vs 1 female). Three of them had a history of cholecystectomy before the procedure, but none of them had ever received choledochoduodenostomy. (Table 1)
Table 1.
The clinical characteristics of the patients with ectopic opening of papilla of Vater into the duodenal bulb (n = 8).
3.2. Endoscopic findings
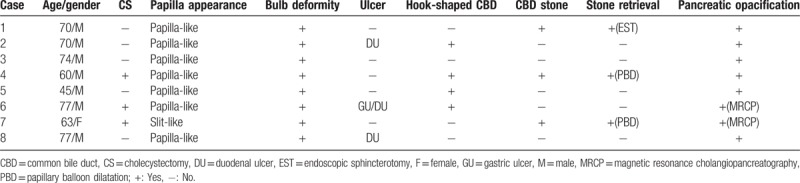
All 8 patients had a deformed duodenal bulb. The ectopic opening in the duodenal bulb of the eight patients was papilla-like (Fig. 1A), except for one which had a slit-like appearance (Fig. 1B). Separate orifice of CBD and main PD was seen in four patients. The separate orifice was indeterminate in case 6 because the diagnosis was made by MRCP. While all of the patients had a deformed duodenal bulb, shallow gastric and/or duodenal ulcers were only seen in 3 patients.
Figure 1.
Papilla-like (A) and slit-like (B) opening ectopically located in the duodenal bulb.
3.3. ERCP and MRCP findings and procedures
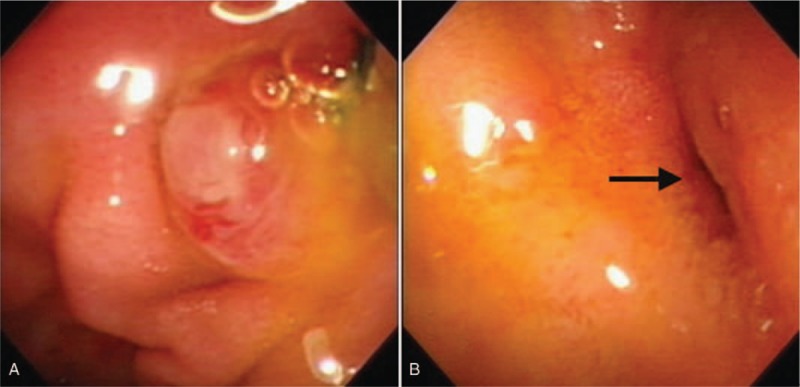
There were 4 patients (50%) with hook-shaped CBD in our study (Fig. 2). Three of 8 patients with ectopic orifice of the duodenal bulb had CBD stones, and all of them underwent stone retrieval successfully after endoscopic sphincterotomy (EST) by traction sphincterotome in one patient and papillary balloon dilation (PBD) in 2 patients. One of them had recurrent CBD stones, and the other 2 patients remained asymptomatic. The main PD of all of the patients was opacified via the same opening of CBD ectopically in the duodenal bulb, either by ERCP (6 cases) or MRCP (2 cases) with special designation.
Figure 2.

X-ray configuration of distal common bile duct without hook shape.
4. Discussion
Eight of 6133 patients (0.13%) receiving ERCP were diagnosed with ectopic orifice of the duodenal bulb in this hospital-based study. The patients with ectopic orifice of papilla of the duodenal bulb were older and predominantly male. Endoscopic findings revealed that most patients had a duodenal bulb deformity and duodenal ulcer. ERCP disclosed deformed CBD, and CBD stone was present in less than half of such cases.
Most studies on patients with ectopic orifice of papilla have been case reports.[3–9,11–13,15] The prevalence of anomalous opening of the CBD distal to the second portion of the duodenum has been reported widely, ranging from 5.6% to 23%. However, proximal opening, such as into the stomach, pylorus or duodenal bulb, is much less frequently found, with prevalence rates of 0.1% to 2.5%.[2,6,10] In this study, we included patient numbers, instead of the numbers of ERCP procedures. The rate of ectopic papilla of Vater in our ERCP study population was 0.13%. We believe that this figure closely corresponds to the prevalence rate of the general population. This is currently the only available figure in Taiwan. Male predominance was noted in this study, which is consistent with the findings of previous reports.[2,6] A study from Turkey reported an incidence of around 2%, which was higher than that found in our patients. Although it is difficult to accurately determine the incidence of on ectopic orifice of papilla owing to the limited number of studies on this condition and the fact that most such studies are case reports, we estimate the incidence to be between 0.13% and a little more.
This rare condition has been reported to be associated with biliary stone. It has also been linked with anomalous PD anatomy.[16] However, we did not found PD abnormality in our patients.
Deformed CBD, such as hook-shaped CBD, has been described as a predominant feature of ectopic orifice of papilla in the literature[2,8] In our series, half of the patients were found to have ectopic orifice of papilla. According to our results, one of the four patients with deformed CBD, that is, hook-shaped CBD had CBD stones.
There may be pitfalls in the diagnosis of ectopic orifice of papilla. Fistula formation between the CBD and the GI tract usually occurs as a result of prolonged and repeated attacks of cholangitis. Clinically, it is important to differentiate the “real” ectopic papilla of Vater from the “acquired” choledochoduodenal fistula.
The opening of a normal biliopancreatic duct has a papilla-like appearance, whereas, a slit-like opening is often found in cases of choledochoenteral fistula. With one exception, all of our patients with ectopic papilla of Vater had a papilla-like opening (Fig. 1A), a finding that differs from previously reported results.[2,6,8,10] In the literature, ectopic slit-like opening without opacification of the PD from the same opening should not necessarily be regarded as ectopic papilla of Vater. Indeed, choledochoenteral fistula should be considered in these cases.
Based on the ERCP findings, only 4 patients (50%) had distal hook-shaped CBD in our study. This result was quite different from results in previous studies,[6,17,18] which reported hook-shaped configuration rates of 100%. It is important to keep in mind that the configuration of CBD recorded on fluoroscopic film may alter dynamically according to the patient's position. Therefore, we believe that hook-shaped CBD does not serve as a reliable criterion for ectopic papilla of Vater.
Choledocholithiasis accounted for the majority of patients with this anomaly in a number of studies, with prevalence rates ranging from 51% to 61%.[2,6,10] Our data showed that 3 out of eight patients (37%) had CBD stones. With respect to the prevalence reported in the general population, at least 10% had gallstones, of which 15% had CBD stones. Moreover, prevalence of gallstones in women was twice the rate found in men.[19] Our data demonstrate that the association of choledocholithiasis with ectopic papilla of Vater was high, especially in men.
EST was successful in one of the patients with papilla-like opening by traction sphincterotome without obvious complications. Some endoscopists have suggested endoscopic balloon dilatation for papilla, but not EST, due to the higher risk of perforation.[10,20] In our view, EST may not be as risky as previous authors have contended. Nevertheless, EST must be performed with great care by an experienced ERCP endoscopist. All of the patients with choledocholithiasis in our study underwent stone retrieval successfully without evidence of recurrence at the time of writing.
Deformity of the duodenal bulb was seen in all of the patients, though only 3 patients had shallow gastric and/or duodenal ulcers during ERCP procedure in our study. The etiology of bulb deformity has been postulated to involve chronic mucosal damage and gastric metaplasia, which may occur as a result of alkaline bile acids and pancreatic juice draining into the duodenal bulb from the ectopic opening.[6,17,18] However, gastric and/or duodenal ulcers were only discovered in three out of 8 patients during ERCP examination in our study, and no history of intractable or recurrent peptic ulcer could be traced. From our clinical experience, deformity of the duodenal bulb resulting from chronic duodenal ulcers has become a relatively rare owing to the widespread use of proton pump inhibitor. Therefore, further investigation is needed to establish whether bulb deformity is secondary to recurrent chemical irritation or due to evolving embryology.
We included patients more strict criteria with “real” ectopic papilla of Vater, which was confirmed by opacification of the CBD and the main PD simultaneously from the same opening. Six of them were confirmed by ERCP, and 2 were confirmed by MRCP. In case number 6, a papilla-like structure was noted in the deformed duodenal bulb during esophagogastroduodenography in a community hospital, but no papilla-like structure was identified in the second portion of the duodenum. Because ERCP was not available in that community hospital, MRCP was arranged. Saline injection (30cc in total) was injected into the submucosa of the pylorus and second portion of the duodenum right before MRCP. This enabled the endoscopist to locate the distal opening of the hook-shaped CBD and the main PD between the two injections (Fig. 3). The procedure proved that the ectopic papilla of Vater was in the duodenal bulb. In case number 7, despite several attempts, opacification of the main PD via the ectopic papilla of Vater failed during ERCP. MRCP was then arranged and the diagnosis was confirmed (Fig. 4). The diagnosis of ectopic papilla of Vater can sometimes be accomplished by MRCP in special circumstances.
Figure 3.
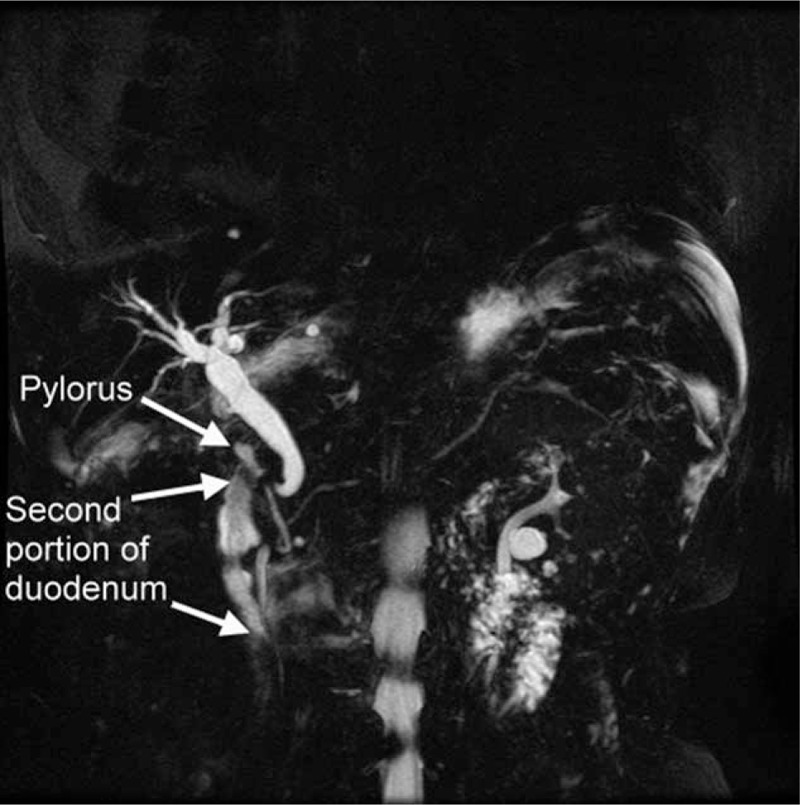
Submucosal saline injection over pylorus and second portion of the duodenum before MRCP confirmed that the drainage of CBD and PD went into the same opening in the duodenal bulb. The configuration of the main PD showed an unusual fusion of ventral and dorsal pancreatic buds during embryologic development. CBD = common bile duct, MRCP = magnetic resonance cholangiopancreatography, PD = pancreatic duct.
Figure 4.
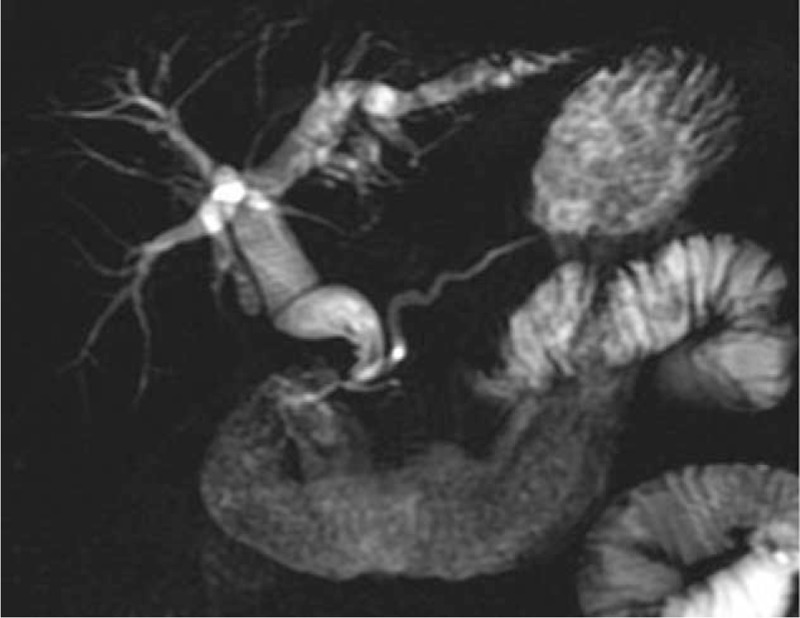
MRCP showed the PD and CBD drained into the same opening. CBD = common bile duct, MRCP = magnetic resonance cholangiopancreatography, PD = pancreatic duct.
We demonstrated ectopic papilla of Vater in a strict follow-up data. However, our studies were restrospective, thus there would be situations as incomplete studies, which may be ectopic papilla. Besides, our survey was based on a data of population of ERCP. The incidence of ectopic papilla of Vater in general population is still needed to be investigated.
5. Conclusion
Ectopic orifice of papilla in the duodenal bulb is rare. In order to establish a definitive diagnosis, opacification of both CBD and main PD from the same opening is essential, and choledochoduodenal fistula must be excluded before reaching a diagnosis of ectopic papilla of Vater.
Author contributions
Conceptualization: Wai-Keung Chow.
Data curation: Yen-Chun Peng, Wai-Keung Chow.
Formal analysis: Yen-Chun Peng, Wai-Keung Chow.
Funding acquisition: Yen-Chun Peng, Wai-Keung Chow.
Investigation: Yen-Chun Peng, Wai-Keung Chow.
Methodology: Yen-Chun Peng, Wai-Keung Chow.
Project administration: Wai-Keung Chow.
Resources: Wai-Keung Chow.
Software: Wai-Keung Chow.
Supervision: Wai-Keung Chow.
Validation: Wai-Keung Chow.
Visualization: Wai-Keung Chow.
Writing – original draft: Yen-Chun Peng, Wai-Keung Chow.
Writing – review & editing: Yen-Chun Peng, Wai-Keung Chow.
Footnotes
Abbreviations: CBD = common bile duct, ERCP = endoscopic retrograde cholangiopancreatography, EST = endoscopic sphincterotomy, MRCP = magnetic resonance cholangiopancreatography, PD = pancreatic duct.
The authors have no conflicts of interest to disclose.
References
- [1].Vakili K, Pomfret EA. Biliary anatomy and embryology. Surg Clin North Am 2008;88:1159–74. [DOI] [PubMed] [Google Scholar]
- [2].Disibeyaz S, Parlak E, Cicek B, et al. Anomalous opening of the common bile duct into the duodenal bulb: endoscopic treatment. BMC Gastroenterol 2007;7:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Doty J, Hassall E, Fonkalsrud EW. Anomalous drainage of the common bile duct into the fourth portion of the duodenum. Clin Sequelae Arch Surg (Chicago, Ill: 1960) 1985;120:1077–9. [DOI] [PubMed] [Google Scholar]
- [4].Kanematsu M, Imaeda T, Seki M, et al. Accessory bile duct draining into the stomach: case report and review. Gastrointest Radiol 1992;17:27–30. [DOI] [PubMed] [Google Scholar]
- [5].Krstic M, Stimec B, Krstic R, et al. EUS diagnosis of ectopic opening of the common bile duct in the duodenal bulb: a case report. World J Gastroenterol 2005;11:5068–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lee SS, Kim MH, Lee SK, et al. Ectopic opening of the common bile duct in the duodenal bulb: clinical implications. Gastrointest Endosc 2003;57:679–82. [DOI] [PubMed] [Google Scholar]
- [7].Lindner HH, Peña VA, Ruggeri RA. A clinical and anatomical study of anomalous terminations of the common bile duct into the duodenum. Ann Surg 1976;184:626–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ozaslan E, Saritas U, Tatar G, et al. Ectopic drainage of the common bile duct into the duodenal bulb: report of two cases. Endoscopy 2003;35:545. [DOI] [PubMed] [Google Scholar]
- [9].Quintana EV, Labat R. Ectopic drainage of the common bile duct. Ann Surg 1974;180:119–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Saritas U, Senol A, Ustundag Y. The clinical presentations of ectopic biliary drainage into duodenal bulbus and stomach with a thorough review of the current literature. BMC Gastroenterol 2010;10:2–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Turner MA, Cho SR, Messmer JM. Pitfalls in cholangiographic interpretation. Radiographics Rev Publ Radiol Soc North Am Inc 1987;7:1067–105. [DOI] [PubMed] [Google Scholar]
- [12].Lee HJ, Ha HK, Kim MH, et al. ERCP and CT findings of ectopic drainage of the common bile duct into the duodenal bulb. AJR Am J Roentgenol 1997;169:517–20. [DOI] [PubMed] [Google Scholar]
- [13].Guerra I, Rabago LR, Bermejo F, et al. Ectopic papilla of Vater in the pylorus. World J Gastroenterol 2009;15:5221–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Vijungco JD, Prinz RA. Management of biliary and duodenal complications of chronic pancreatitis. World J Surg 2003;27:1258–70. [DOI] [PubMed] [Google Scholar]
- [15].Nasseri-Moghaddam S, Nokhbeh-Zaeem H, Soroush Z, et al. Ectopic location of the ampulla of vater within the pyloric channel. Middle East J Dig Dis 2011;3:56–8. [PMC free article] [PubMed] [Google Scholar]
- [16].Li L, Yamataka A, Wang YX, et al. Anomalous pancreatic duct anatomy, ectopic distal location of the papilla of Vater and congenital biliary dilatation: a new developmental triad. Pediatr Surg Int 2003;19:180–5. [DOI] [PubMed] [Google Scholar]
- [17].Walker MM, Dixon MF. Gastric metaplasia: its role in duodenal ulceration. Aliment Pharmacol Ther 1996;10suppl 1:119–28. [DOI] [PubMed] [Google Scholar]
- [18].Savarino V, Mela GS, Zentilin P, et al. Effect of Helicobacter pylori eradication on 24-hour gastric pH and duodenal gastric metaplasia. Dig Dis Sci 2000;45:1315–21. [DOI] [PubMed] [Google Scholar]
- [19].Lambou-Gianoukos S, Heller SJ. Lithogenesis and bile metabolism. Surg Clin North Am 2008;88:1175–94. [DOI] [PubMed] [Google Scholar]
- [20].Ersoz G, Akay S, Ozutemiz O, et al. Patients with bulbar papilla and choledocholithiasis and their endoscopic management. Hepatogastroenterology 2009;56:29–33. [PubMed] [Google Scholar]


