Supplemental Digital Content is available in the text
Keywords: coma, plasma exchange, Prussian blue, thallium poisoning
Abstract
Rationale:
This is the first reported severe thallium poisoning patient successfully treated with Prussian blue (PB) and plasma exchange (PE).
Patient concerns:
A 42-year-old woman in a coma owing to severe thallium poisoning was admitted to our department after day 44 of poisoning. At admission, blood and urine thallium concentrations were 380.0 and 2580.0 ng/mL, respectively.
Diagnosis:
The patient was diagnosed with toxic encephalopathy induced by thallium poisoning; in addition, she was also diagnosed with bilateral pneumonia, respiratory failure, moderate anemia, hypoproteinemia, and electrolyte imbalance based on her chest X-ray, blood gas analysis, Hb level, albumin levels, and serum electrolyte results.
Interventions:
The patient was intubated and treated with PB (6600 mg/d, 15 days in total) combined with PE (once daily, 5 days in total) as well as other symptomatic supportive care measures.
Outcomes:
After treatments, her blood and urinary thallium concentrations gradually decreased and on the 13th day after admission, the blood thallium concentration decreased to 0 ng/mL. The oxygenation index gradually improved, meantime, the patient gradually regained consciousness, and on the 50th day of admission, the patient's consciousness reverted to a clear-headed state. The patient recovered mostly after 37 months of follow-up.
Lessons:
Through this case, we learned that the gradual reduction in blood and urine thallium concentration and the patient's improved condition is correlated with PB and PE treatment. For patients with severe thallium poisoning, this treatment method might be effective; but the exact curative effect is unconfirmed, requiring further research to verify.
1. Introduction
Thallium is an extremely toxic metal, it has been used as a medicinal agent and in many manufacturing processes but also as a rodenticide.[1,2] Because of its frequent use in suicide and criminal poisonings, it has been banned in many countries, but many developing countries including China still have cases of thallium poisoning.[2–8] Because of the small number of cases, the study of thallium poisoning is not comprehensive and most notably, data on patients with severe poisoning is lacking; hence, treatment of thallium poisoning remains a difficult clinical problem. Prussian blue (PB) has been the most commonly prescribed antidote to treat thallium poisoning; however, its availability is limited in many locations.[3,9] Besides PB, blood purification treatments are also a beneficial treatment option, especially for patients with severe thallium poisoning.[3] However, the efficacy of blood purification treatments still needs more research to verify[3] and there is no study reporting on the efficacy of plasma exchange (PE). Here, we report a case of severe thallium poisoning in a patient who experienced a coma and was successfully treated with PB and PE to provide an account of this treatment experience for other clinicians.
2. Case report
A 42-year-old woman with a history of viral hepatitis and a 3-year history of anemia developed abdominal pain, abdominal distension, and limb pain without any reason. After several referrals and treatments, the condition was not alleviated. The cause of the disease was not determined, until poison test results on the 35th day after symptom onset revealed that blood and urine thallium concentrations were 950 and 7600 ng/mL, respectively. On the 44th day from onset, the patient presented to the poisoning intensive care unit (ICU) of our department. On admission, the patient was in a deep coma state and thus was administered endotracheal intubation for airway protection and assisted breathing through a ventilator. Arterial blood gas analysis (FiO2, 60.0%; body temperature, 38.5°C) results were as follows: pH, 7.5; PCO2, 37.6 mm Hg; PO2, 54.0 mm Hg; BE, 6.1 mmol/L; lactate, 0.8 mmol/L; and HCO3-, 29.3 mmol/L. Routine blood test results at admission showed white blood cell (WBC) count of 10.27 × 109/L, neutrophil count of 0.896, red blood cell count of 2.87 × 1012/L, and Hb level of 78 g/L. Blood biochemical test results at admission showed Na+ levels of 155 mmol/L, K+ levels of 2.84 mmol/L, Cl- levels of 124 mmol/L, ALT levels of 51 U/L, and albumin levels of 30 g/L. Chest radiograph shows bilateral lung exudative changes. The patient's diagnosis was: toxic encephalopathy induced by thallium poisoning, bilateral pneumonia, respiratory failure, moderate anemia, hypoproteinemia with electrolyte imbalance (low K+, high Na+, high Cl-).The poison test (on the 45th day from onset) showed that the blood and urine thallium concentrations were 380.0 and 2580.0 ng/mL, respectively, whereas the thallium concentration in the cerebrospinal fluid was 80.0 ng/mL. Electroencephalography (EEG) results showed moderate abnormality. The patient was treated with Prussian blue (PB; 6600 mg/d), PE (once/day), and other symptomatic support (liver protection, stomach protection, anti-infection, improvement of circulation, nutritional nerves, and other symptomatic supportive treatments). Detailed volume and substitution fluid of PE are presented in Supplemental File 1. After the fifth PE, the patient's blood thallium concentration was 120.0 ng/mL; doctors decided to stop the PE treatment. Changes in blood thallium concentrations in the patient during PE treatment are shown in Fig. 1. On the 57th day from onset (the 14th day from admission), no thallium ions were detected in the blood or cerebrospinal fluid, whereas the urine thallium concentration was only 80 ng/mL. PB treatment was stopped after 15 days of treatment. On the 83rd day from onset (the 39th day from admission), skull computed tomography (CT) scan showed suspicious low-density lesions. During the treatment, the thallium concentration decreased, oxygenation index increased, and the patient gradually recovered consciousness. The partial clinical course (from deep coma to consciousness) is shown in Fig. 2. EEG still showed moderate abnormality 119 days after admission. After 137 days of hospitalization, the patient was discharged to a local hospital for further treatment. On discharge, the patient was conscious. Her muscle strength was partially restored, and there was no further need for ventilator-assisted breathing, but she still had hypoxemia; thus, low-level oxygen supplementation (2 L/min) was administered. After 37 months of follow-up, the symptoms gradually improved according to a report by the family. Currently, the patient experiences foot pain, an inability to walk independently, and memory loss after discharge, but she is able to speak freely, and her memory is gradually recovering. Informed written consent was obtained from the patient for publication of this case report and accompanying images, and this study design was approved by the appropriate ethics review board of our hospital.
Figure 1.
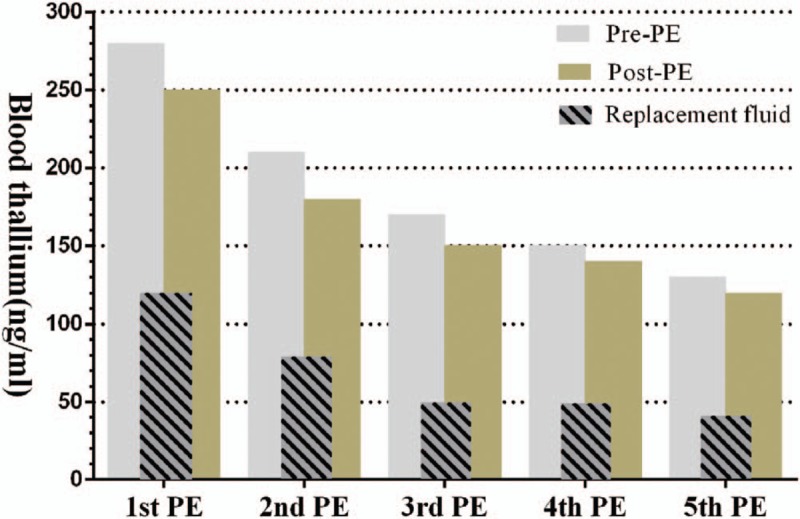
Changes of blood thallium concentration in patients during PE treatment. PE = plasma exchange.
Figure 2.
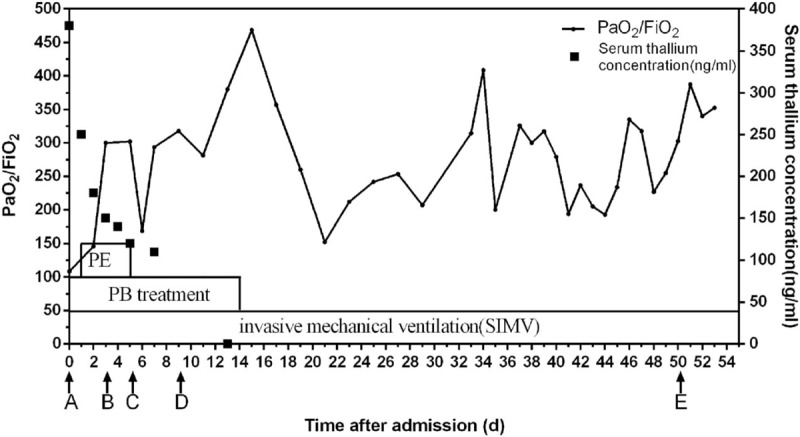
Partial clinical course (from deep coma to consciousness). PE = plasma exchange (1/d, 5 times in total). PB = Prussian blue (6600 mg/d, 15 days in total). A, The patient was in a deep coma when admission. B, The patient turn moderate coma on the 4th day. C, The patient turned into a light coma on the 6th day. D, The patient turned into confusion on the 10th day. E, The patient's consciousness is restored to clear-headed state on the 51st day.
3. Discussion
Acute thallium poisoning can cause severe central nervous system damage. In severe cases, paralysis of the respiratory muscles may occur, even leading to coma.[2,10] Here, we report on a patient in a coma caused by severe thallium poisoning and untimely diagnosis and treatment. After PB and PE treatment, as well as other symptomatic supportive treatments, the patient's condition gradually recovered. Furthermore, this is the first reported severe thallium poisoning patient successfully treated with PB and PE. Therefore, we concluded that PB combined with PE may play a therapeutic role in treating thallium poisoning in patients with associated toxic encephalopathy.
There are no clear guidelines for thallium poisoning treatment. The treatment should aim to remove the poison as soon as possible. The efficacy of PB has been widely recognized; however, there are still many uncertainties regarding treatments that involve blood purification. Considering the patient's severe toxic encephalopathy (in a deep coma) and high blood thallium, we provided treatment with PB combined with PE. A previous study[11] had reported that double-filtration plasmapheresis (DFPP) might have a therapeutic effect on thallium poisoning. The efficacy of plasma exchange has not been reported. The possible PE treatment mechanisms include removal of toxins and inflammatory mediums from the circulation. Furthermore, despite the theoretical advantage of PE to efficiently remove highly protein-bound toxins with a small volume of distribution (plasma protein-binding rate of thallium ions is 0, and distribution volume is 3–10 L/kg), studies show that PE may have wider utility such as for those with deterioration despite intensive care and those having toxicities or worsening of the central nervous system function.[12] The efficiency of PE in this patient can be summarized into 2 aspects; on the one hand, substitution fluid containing thallium ions clarifies that PE can help accelerate the elimination of thallium; on the other hand, the recovery of the patients’ condition may be related to the ability of PE to remove inflammatory mediators and other pathogenic factors induced by thallium ions in the body. PE can remove thallium ions, but its removal efficiency still needs further research to verify this. Furthermore, because the patient's recovery is accompanied by PB and PE intervention, it is impossible to judge the efficacy of each treatment alone. Further research is needed to explore the clear efficacy of PB and PE respectively. Regrettably, owing to the serious condition of the patient, CT or MRI examination could not be performed in the early stage of the coma, which can’t aid in more clearly understanding the early central damage of this condition. In reporting this treatment experience, we hope that clinicians will benefit when treating patients with severe thallium poisoning and that the information reported here will lay foundation for further research in thallium treatment.
4. Conclusion
PB combined with PE may play a therapeutic role in treating severe thallium poisoning in patients with associated toxic encephalopathy. However, because the 2 interventions are carried out at the same time, it is impossible to understand the efficacy of each treatment alone. PE did have the ability to clear thallium during this study, but its removal efficiency still requires further research to verify.
Author contributions
Data curation: Guodong Lin, Luo Yuan, Lili Bai, Yanqing Liu.
Investigation: Lili Bai, Yanqing Liu.
Writing – original draft: Guodong Lin, Luo Yuan, Yongan Wang.
Writing – review & editing: Yongan Wang, Qiu Zewu.
Supplementary Material
Footnotes
Abbreviations: DFPP = double-filtration plasmapheresis, EEG = electroencephalography, ICU = intensive care unit, PB = Prussian blue, PE = plasma exchange, WBC = white blood cell.
The authors have no conflicts of interest to disclose.
References
- [1].Sun TW, Xu QY, Zhang XJ, et al. Management of thallium poisoning in patients with delayed hospital admission. Clin Toxicol (Phila) 2012;50:65–9. [DOI] [PubMed] [Google Scholar]
- [2].Cvjetko P, Cvjetko I, Pavlica M. Thallium toxicity in humans. Arhiv Hig Rada Toksikol 2010;61:111–9. [DOI] [PubMed] [Google Scholar]
- [3].Ghannoum M, Nolin TD, Goldfarb DS, et al. Extracorporeal treatment for thallium poisoning: recommendations from the EXTRIP Workgroup. Clin J Am Society Nephrol 2012;7:1682–90. [DOI] [PubMed] [Google Scholar]
- [4].Yumoto T, Tsukahara K, Naito H, et al. A successfully treated case of criminal thallium poisoning. J Clin Diagn Res 2017;11:OD01–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Li JM, Wang W, Lei S, et al. Misdiagnosis and long-term outcome of 13 patients with acute thallium poisoning in China. Clin Toxicol (Phila) 2014;52:181–6. [DOI] [PubMed] [Google Scholar]
- [6].Huang C, Zhang X, Li G, et al. A case of severe thallium poisoning successfully treated with hemoperfusion and continuous veno-venous hemofiltration. Hum Exp Toxicol 2014;33:554–8. [DOI] [PubMed] [Google Scholar]
- [7].Yang G, Li C, Long Y, et al. Hair loss: evidence to thallium poisoning. Case Rep Emerg Med 2018;2018:1313096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Almassri I, Sekkarie M. Cases of thallium intoxication in Syria: a diagnostic and a therapeutic challenge. Avicenna J Med 2018;8:78–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hoffman RS. Thallium toxicity and the role of Prussian blue in therapy. Toxicol Rev 2003;22:29–40. [DOI] [PubMed] [Google Scholar]
- [10].Osorio-Rico L, Santamaria A, Galvan-Arzate S. Thallium toxicity: general issues, neurological symptoms, and neurotoxic mechanisms. Adv Neurobiol 2017;18:345–53. [DOI] [PubMed] [Google Scholar]
- [11].Tian YR, Sun LL, Wang W, et al. A case of acute thallotoxicosis successfully treated with double-filtration plasmapheresis. Clin Neuropharmacol 2005;28:292–4. [DOI] [PubMed] [Google Scholar]
- [12].Schutt RC, Ronco C, Rosner MH. The role of therapeutic plasma exchange in poisonings and intoxications. Semin Dial 2012;25:201–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


