Abstract
Lumbar disc hernia is common disease, affecting about 5% of the population. Many studies to date reported regression of disc herniation without surgical intervention.
Medical records of the patients who applied to the spine clinic in an outpatient setting were retrospectively reviewed. Age, sex, radiological findings, neurological examinations, and medical treatments of the patients were evaluated.
Male patients constituted 52.6% of the cases (n = 40) and 47.4% (n = 36) were female. The ages of the patients ranged from 25 to 82 years, with a mean of 48.5 ± 12.1 years. Visual analog scale (VAS) measurements ranged from 0 to 8 and the mean was determined as 2.65 ± 1.98. The VAS score of pain severity of 12 (15.78%) cases was 0, VAS score of 39 (51.31%) cases was 1 to 3, VAS score of 20 (26.31%) cases was 4 to 6, VAS score of 5 (6.57%) cases was 7 to 10. Eighteen (23.68%) of the cases underwent neuropathic pain treatment for more than 6 months. Fifteen (19.7%) patients also developed permanent motor deficits.
Findings of our study show that there was no direct association between radiological improvement and clinical improvement. Indication for surgery still existed in a high number of patients, substantial of which developed permanent motor deficits. Current results suggest that we need to advise our patients in favor of early surgery as soon as indication for surgery is established upon neurological and radiological examination.
Keywords: lumbar disc herniation, magnetic resonance imaging, spontaneous regression
1. Introduction
Low-back pain is an important medical condition that is reported to affect 80% of the individuals at least once in their life span. While being not a life-threatening condition, it is listed among leading reasons for loss of social activity and workload. Lumbar disc herniation (LDH) is the displacement of lumbar intervertebral disc tissues, nucleus pulposus, and annulus fibrosus, within the vertebral column. The LDH is common disease, affecting about 5% of the population. While LDH-induced pain accounts for 5% of all low-back pain cases, only 15% all LDH cases are managed with surgical intervention.[1]
Therapeutic options for LDH include conservative and surgical treatment. Many patients benefit from conservative treatment, yet surgical treatment may also be advised if cauda equine syndrome or symptoms such as motor weakness or pain refractory to conservative treatment exist. Numerous studies have shown regression of disc herniation without surgical intervention.[2–4] It was 1st reported by Guinto in 1984.[5] Many of such studies reported good response to conservative treatment and improvement of patients without surgical treatment.
This study aimed to identify patients who had spontaneous resorption of herniation in lumbar spinal magnetic resonance imaging (MRI) during follow-up visits after voluntarily declining surgical intervention despite indicated for extruded or sequestered LDH and to determine their responses to the conservative treatment.
2. Materials and method
In this study, medical records of the patients who were diagnosed with LDH upon applying to the outpatient spine clinic were retrospectively reviewed. Assessed parameters included age, sex, radiological examinations, neurological examinations, medical treatments, comorbidities, smoking, exercise, and trauma (Table 1).
Table 1.
Distribution of variables.

Severity of pain was assessed by visual analog scale (VAS) and presence/absence of neuropathy was assessed by electromyography (EMG).
The study included cases who had evidence of regression in LDH on follow-up lumbar spinal MRI that was performed upon persistence of symptoms after declining indicated surgical treatment for extruded or sequestered LDH on lumbar spinal MRI with clinical presentation of low-back and radicular pain. The records in the automation system were examined. As a result of neurological examination and radiological evaluation, all patients, surgical treatment was recommended for all patients at the time of admission and emergency surgical treatment was recommended for patients with neurological deficit. However, patients who were recommended to undergo surgical treatment did not accept surgical treatment on their own initiative. These patients were included in the study and other patients were excluded from the study. The patients included in the study were admitted to our clinic again at different times at their own request out of the control of the clinic upon the continuation of their complaints. The lumbar spinal MRIs of the patients done at their own request at the time of admission were evaluated and the elapsed time with the 1st MRI determined the time between 2 MRIs. Disc resorption was calculated in the MRIs of these patients. Since the groups, non-surgical patients, were evaluated at their own requests, we did not have any patient groups who had early surgery and they were not compared with the results of the study.
The cases were divided into 2 groups by their time of application with complaints. Group I consisted of cases who applied with low-back and radicular pain within 6 months, and Group II consisted of cases who were presented after 6 months. The study algorithm was summarized in Figures 1 and 2.
Figure 1.
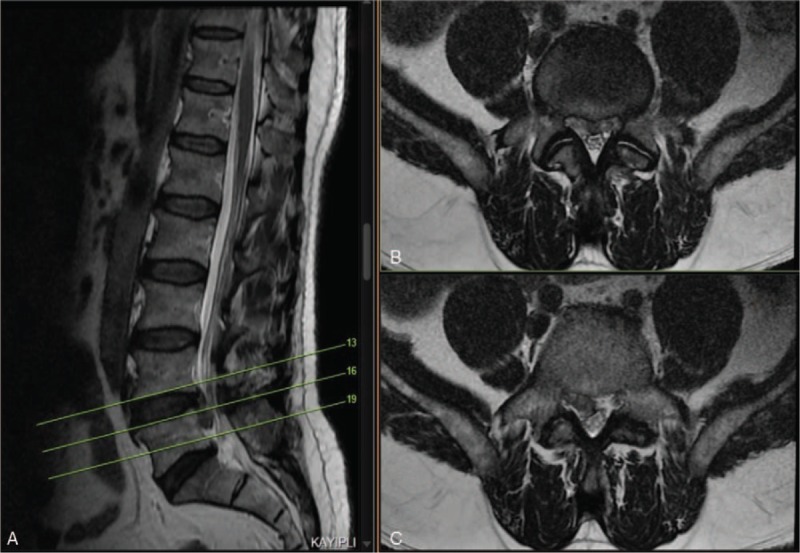
(A, B, C) Demonstrative case (L4–5 extruded disc herniation).
Figure 2.
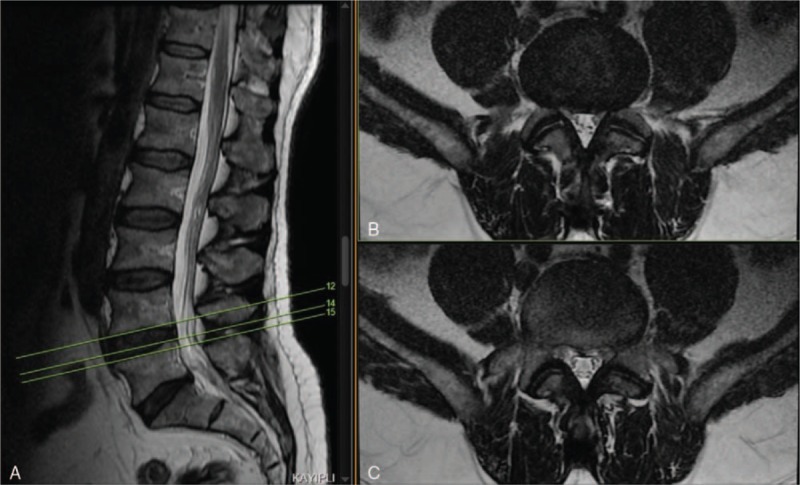
(A, B, C) Demonstrative case (4 months later).
The study included 76 cases after applying exclusion criteria. Forty cases (52.6%) were male and 36 (47.4%) of them were female (Figs. 3–5).
Figure 3.
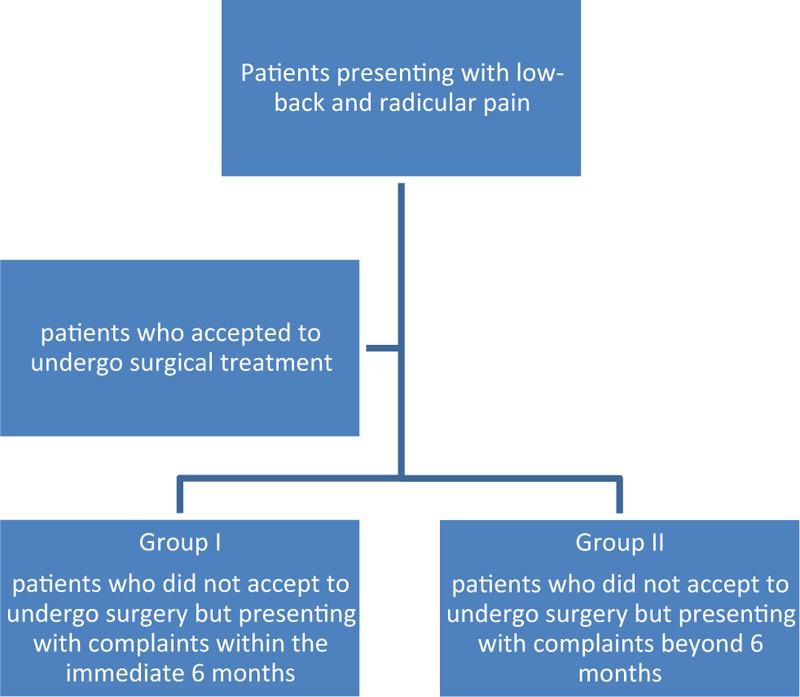
Algorithm for assigning study groups.
Figure 5.
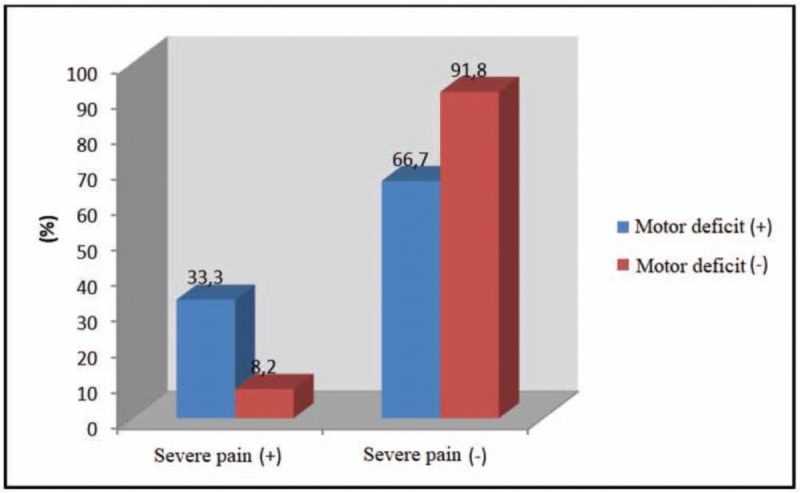
The distribution of severe pain according to motor deficit.
Figure 4.
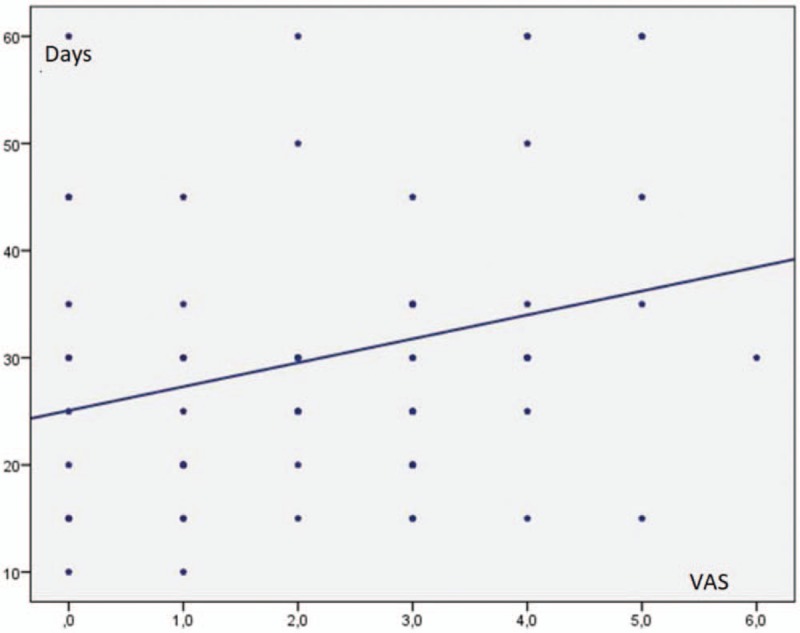
The relationship between VAS scores and relief of severe pain. VAS = visual analog scale.
2.1. Statistical analysis
For statistical analyzes, Number Cruncher Statistical System (NCSS) 2007 and Power Analysis and Sample Size (PASS) 2008 Statistical Software (UT) programs were used. While descriptive study data were presented as mean, standard deviation, median, frequency, percentage, minimum and maximum values, Mann–Whitney U test was used to compare 2 groups and Kruskal–Wallis test to compare more than 2 groups for non-normally distributed quantitative data. The relation between parametric values was assessed with Spearman's correlation analysis. Logistic regression was used to group multivariable data. While a P value between .01 and .05 was accepted as statistically significant difference; a P < .001 indicated highly statistically significant difference in our study.
3. Results
Male patients constituted 52.6% of the cases (n = 40) and 47.4% (n = 36) were female. The ages of the patients ranged from 25 to 82 years, with a mean of 48.5 ± 12.1 years. There were 46 patients (60.5%) in Group I and 30 patients (39.5%) in Group 2. The mean time interval between initial MRI at presentation and follow-up MRI was 11 weeks. The shortest time between these 2 MRI was 4 weeks. Forty-nine patients (64.5%) had sequestered disc herniation (Tables 2 and 3).
Table 2.
Evaluation of patients in Group I.
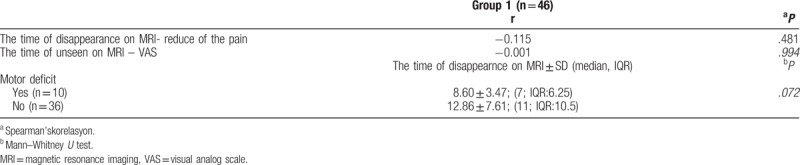
Table 3.
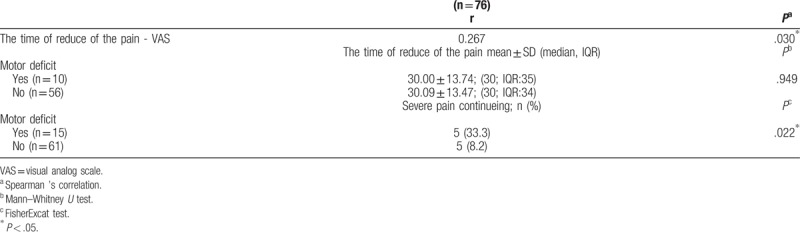
Evaluation of all patients.
The distribution of the study groups by their disc herniation on axial lumbar MRI showed 34 patients (73.9%) with paracentral, 4 patients (8.7%) with central, 1 patient (2.2%) with foraminal, and 7 patients (15.2%) with both central and paracentral disc hernia in Group I. On the other hand, 21 patients (70%) had paracentral, 3 patients (10%) had central, and 6 patients (20%) had both central and paracentral disc herniation in Group 2. Comorbidities (diabetes mellitus, hypertension, prior ischemic vascular disease, chronic obstructive pulmonary disease, etc.) were present in 13 patients (28.3%) in Group 1 and 10 patients (33.3%) in Group 2. The evaluation of the causes for seeking medical help showed that 13 patients (28.3%) applied after mild exercise, 7 patients (15.2%) after heavy exercise, 3 patients (6.5%) after trauma, and 23 patients (50%) without any exercise or trauma in Group I. In Group II, 4 patients (13.3%) were presented after mild exercise, 5 patients (16.7%) after heavy exercise, 5 patients (16.7%) after trauma, and remaining 16 patients (53.3%) with no exercise or trauma.
The mean VAS score was found to be 2.65 ± 1.98 (range: 0–8). The VAS stratification showed 12 patients (15.8%) with VAS score of 0, 39 patients (51.3%) with VAS scores of 1–3, 20 patients (26.3%) with VAS scores of 4–6, and 5 patients (6.6%) with VAS score of 7–10. The duration when severe pain reduced lasted from 10 to 60 days, with a mean of 30.1 ± 13.4 days. There were 10 cases with severe pain.
Treatment for neuropathic pain was started in a number of cases with varying degrees of pain; 41 cases received such treatment for their complaints at any time. The treatment has been still continued (at least for 6 months) in 18 patients (23.7%). When all possible reasons that might affect formation of neuropathic pain were excluded, no significantly difference was found between Group I and II in terms of neuropathic pain (P > .05), (Table 4).
Table 4.
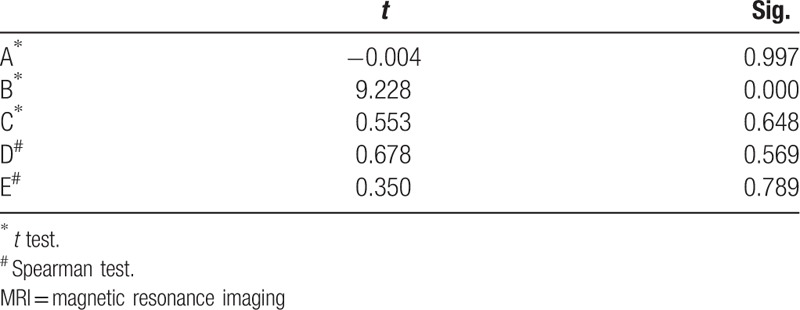
When effects of smoking, comorbidity, localization of disc herniation, absence/presence of physical activity were excluded; (A) Formation of neuropathic pain when groups 1 and 2 were compared, (B) Removal time of the sequestered disc in magnetic resonance imaging (MRI) examination when groups 1 and 2 were compared, (C) Localization of the sequestered disc when groups 1 and 2 were compared, (D) Correlation of the localization of the disk with the presence of neuropathic pain, (E) Correlation between the location of the disc and the removal time of the disc in MRI.
The mean duration for reduction of complaints in patients who had severe and disturbing complaints at presentation was found as 30 days. Fifteen cases (19.7%) developed permanent motor deficit and 11 cases (14.5%) underwent surgery upon persistence of clinical manifestations despite resorbed disc herniation. Hypoesthesia was detected in 14 patients (18.4%) in dermatomes consistent with the radiological findings.
The EMG was performed in 53 subjects, of which 14 (26.4%) had abnormal nerve conduction findings consistent with the radiological data.
The mean time for disappearance of extruded or sequestered discs on lumbar spinal MRI was 25.93 ± 21.28 weeks (range: 4–90 weeks).
The weak negative association found between the time for disappearance of disc herniation on MRI and the time for reduction of pain (the time for relieving of pain shortened as the time for disappearance prolonged) was not statistically significant (P > .05). There was no statistically significant association between the time for disappearance of MRI findings and VAS pain (P > .05). When all possible reasons that might affect formation of neuropathic pain were excluded, a significant relation was found between Group I and Group II in terms of the time from disappearance of lumbar disc herniation on MRI to the formation of neuropathic pain (P < .005), (Table 4). Resorption of LDH occurred earlier in patients of Group I.
In cases with motor deficits, the time for disappearance of MRI findings was detected to be shorter where the difference was slightly above the significance limit; it did not reach statistical significance probably due to the small number of cases in the groups (P > .05). When the pain severity was evaluated by presence of motor deficit, 33.3% of patients with motor deficits had ongoing severity compared to that in 8.2% of cases without motor deficits. A significant difference was found between motor deficit and severity (P < .05). The rate of persistence of pain was found to be high in patients with motor deficits. No significant difference was detected between those with and without motor deficits in terms of the time for persistence of pain among those whose pain severity was declined (P > .05).
There was a significantly positive correlation of 26.7% between the time required for the pain to reduce and VAS score (r = 0.267; P < .05).
Smoking, comorbidity, localization of disc herniation, and presence of physical activity did not statistically differ between study groups (P > .05).
4. Discussion
The LDH is one of the most common reasons for low-back pain and extremity radicular syndrome. The management approaches include conservative therapies such as bed rest, oral anti-inflammatory and analgesic medication, spinal anesthetic blocks and/or physical therapy.[1–5] Surgery is indicated in cauda equine syndrome or in the presence of symptoms such as motor weakness or pain refractory to conservative treatment. No definitive conclusion on the necessity of early surgery was reached in the literature. However, the benefits of early surgery were mentioned in most studies.[6–8] Although the radiological improvement was achieved in the light of the results of our study, patients continued to complain. Although early surgical treatment has been performed, permanent neurological symptoms may not improve. We have the same opinion. Nevertheless, we believe that the possibility of improvement can be increased with early surgical treatment.
Spontaneous resorption of intervertebral disc herniation on computed tomography and MRI have been reported in the literature.[1–5,9] Though several mechanisms were described for spontaneous regression, the exact mechanism has not been elucidated. Three hypotheses have been described in the literature. The 1st hypothesis is the retraction of the protruded disc. The 2nd hypothesis states that disc regression is due to gradual dehydration and contraction. Bozzao et al proposed the hypothesis that dehydration within the nucleus pulposus caused extruded material to retract back into the annulus fibrosus.[10] Third hypothesis states enzymatic degradation and phagocytosis of disc tissue due to inflammatory reaction and neovascularization.[1,5,9,11] This is the most noticeable mechanism. It describes an inflammatory reaction where the autoimmune system recognizes extruded disc material as a “foreign body” in the epidural vascular space of the vertebra. This causes neovascularization of the disc tissue and infiltration by inflammatory cells such as macrophages, granulocytes, and lymphocytes.[1,10,12–19] This has been supported by several histopathological studies of the surgery, tissue specimens, and experimental animal research.[13,15,18,20–23] However, it is possible for the 3 mechanisms together to be involved in the regression and disappearance of herniated disc tissue.
Many studies have been reported regarding spontaneous regression of LDH in the literature. In majority of these studies, patients had spontaneous regression while follow-up without surgery, and the condition completely resolved with conservative approach. These were small series of 1 or several cases.[2–5,24] Patients with complete regression and remission were presented as case reports. In our study, cases with and without decreased complaints and spontaneous disc regression were included. Our findings showed that satisfactory clinical improvement was not seen in the majority of patients with spontaneous regression. The number of patients (n = 33) who underwent surgical intervention, or had motor deficits, EMG findings, or high VAS scores despite spontaneous regression suggests no complete remission among our patients. Approximately 1/5th of all subjects developed permanent motor deficits. In contrast to the literature, conservative treatment did not yield satisfactory benefits in all patients in our study.
In our study, only 15.8% of the patients had complete recovery. This supports the findings reported in the literature. In the remaining patients, various degrees of complaints persisted and no response to conservative treatment was obtained. Among these patients, 14.5% of cases (n = 11) underwent surgery. Complete recovery was observed in these patients after the procedure. This suggests that recovery is achieved by resolution of adhesions secondary to inflammatory changes around the root during disc resorption. It further explains the reason for insufficient clinical improvement despite resorption of the disc.
The mean time between MRIs between regression and disappearance in our study was 11 weeks, while the shortest time was determined as 4 weeks. Serdal et al reported spontaneously disappeared disc herniation on MRI after 14 days.[23] This shows that though varied among patients at individual level, the disc tissue could be resorbed as early as 2 weeks.
Spontaneous disappearance of sequestered and free disc fragments are more common than that seen in subligament disc herniations.[22] This is supported by the large proportion of sequestered disc herniations in our series. In another study, Buttermann reported that larger disc herniations (especially extruded and sequestered) exhibited comparably more resorption.[25] This contributes to the idea that there may be a relationship between the size of the disc and resorption.
Clinical improvement is often associated with radiological disc regression. Nevertheless, no direct relationship between clinical and radiological improvement has been reported.[1] In our study, the complaints of the patients decreased within an average of 30 days. However, no corresponding radiological improvement was seen in early MRIs.
5. Conclusion
Findings of our study show that there was no direct association between radiological improvement and clinical improvement. Indication for surgery still existed in a high number of patients, substantial of which developed permanent motor deficits. In the light of these results, we believe that early surgical treatment will provide more benefit to the patients when neurological examination and surgical indication have been performed radiologically.
Author contributions
Conceptualization: Okan Türk, Can Yaldiz.
Data curation: Okan Türk, Can Yaldiz.
Investigation: Veysel Antar, Can Yaldiz.
Resources: Veysel Antar, Can Yaldiz.
Supervision: Can Yaldiz.
Footnotes
Abbreviations: EMG = electromyography, LDH = lumbar disc herniation, MRI = magnetic resonance imaging, VAS = visual analog scale.
Ethics: The work described in this article has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans; Uniform Requirements for manuscripts submitted to Biomedical journals.
The authors have no conflicts of interest to disclose.
References
- [1].Komori H, Shinomiya K, Nakai O, et al. The natural history of herniated nucleus pulposus with radiculopathy. Spine 1996;21:225–9. [DOI] [PubMed] [Google Scholar]
- [2].Kim SG, Yang JC, Kim TW. Spontaneous regression of extruded lumbar disc herniation: three cases report. Korean J Spine 2013;10:78–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Yang X, Zhang Q, Hao X, et al. Spontaneous regression of herniated lumbar discs: report of one illustrative case and review of the literature. Clin Neurol Neurosurg 2016;143:86–9. [DOI] [PubMed] [Google Scholar]
- [4].Ryu SJ, Kim IS. Spontaneous regression of a large lumbar disc extrusion. J Korean Neurosurg Soc 2010;48:285–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Guinto FC, Jr, Hashim H, Stumer M. CT demonstration of disk regression after conservative theraphy. AJNR Am J Neuroradiol 1984;5:632–3. [PMC free article] [PubMed] [Google Scholar]
- [6].Hardy RW, Jr, Ball PA. Winn HR, Dacey RG. Treatment of disk disease of the lumbar spine. Youmans neurological surgery vol. IV 5th ed.New York: Saunders; 2004. 4507–20. [Google Scholar]
- [7].Oktenoglu T, Ozer AF, Sasani M, et al. Posterior dynamic stabilization in the treatment of lumbar degenerative disc disease: 2-year follow-up. Minim Invasive Neurosurg 2010;53:112–6. [DOI] [PubMed] [Google Scholar]
- [8].Hu Y, Gu YJ, Xu RM, et al. Short-term clinical observation of the Dynesys neutralization system for the treatment of degenerative disease of the lumbar vertebrae. Orthop Surg 2011;3:167–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Teplick JG, Haskin ME. Spontaneous regression of herniated nucleous pulposus. AJR Am J Roentgenol 1985;145:371–5. [DOI] [PubMed] [Google Scholar]
- [10].Bozzao A, Gallucci M, Masciocchi C, et al. Lumbar disk herniation: MR imagingassessment of natural history in patients treated without surgery. Radiology 1992;185:135–41. [DOI] [PubMed] [Google Scholar]
- [11].Slavin KV, Raja A, Thornton J, et al. Spontaneous regression of a large lumbar disc herniation: Report of an illustrative case. Surg Neurol 2001;56:333–6. [DOI] [PubMed] [Google Scholar]
- [12].Borota L, Jonasson P, Agolli A. Spontaneous resorption of intradural lumbar disc fragments. Spine J 2008;2:397–403. [DOI] [PubMed] [Google Scholar]
- [13].Haro H, Shinomiya K, Komori H, et al. Furuya K:Up regulated expression of chemokines in herniated nucleus pulposus resorption. Spine 1996;14:1647–52. [DOI] [PubMed] [Google Scholar]
- [14].Doita M, Kanatani T, Harada T, et al. Immunohistologic study of the ruptured intervertebral disc of the lumbar spine. Spine 1996;21:235–41. [DOI] [PubMed] [Google Scholar]
- [15].Hirabayashi S, Kumano K, Tsuiki T, et al. A dorsally displaced free fragment of lumbar disc herniation and its interesting histologic findings. A case report. Spine 1990;15:1231–3. [DOI] [PubMed] [Google Scholar]
- [16].Reyentovich A, Abdu WA. Multiple independent, sequential, and spontaneously resolving lumbar intervertebral disc herniations: a case report. Spine 2002;27:549–53. [DOI] [PubMed] [Google Scholar]
- [17].Henmi T, Sairyo K, Nakano S, et al. Natural history of extruded lumbar intervertebral disc herniation. J Med Invest 2002;49:40–3. [PubMed] [Google Scholar]
- [18].Ito T, Yamada M, Ikuta F, et al. Histologic evidence of absorption of sequestration-type herniated disc. Spine (PhilaPa 1976) 1996;21:230–4. [DOI] [PubMed] [Google Scholar]
- [19].Sei A, Nakamura T, Fukuyama S, et al. Spontaneous regression of lumbar hernia of the nucleus pulposus. Follow-upstudy of 4 cases by repeated magnetic resonance imaging. Rev Chir Orthop Reparatrice Appar Mot 1994;80:144–9. [PubMed] [Google Scholar]
- [20].Minamide A, Hashizume H, Yoshida M, et al. Tamaki T: effects of basic fibroblast growth factor on spontaneous resorption of herniated intervertebral discs. An experimental study in the rabbit. Spine (PhilaPa 1976) 1999;24:940–5. [DOI] [PubMed] [Google Scholar]
- [21].Rätsep T, Minajeva A, Asser T. Relationship between neovascularization and degenerative changes in herniated lumbar intervertebral discs. Eur Spine J 2013;22:2474–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Sang HA, Myun WA, Woo MB. Effect of the transligamentous extension of lumbar disc herniations on the irregression and the clinical outcome of sciatica. Spine 2000;25:475–80. [DOI] [PubMed] [Google Scholar]
- [23].Albayrak S, Durdag E, Atci BA, et al. Rapid spontaneous regression of lumbar disc herniation accompanying neurological recovery: case report. J PMR Sci 2012;15:89–91. [Google Scholar]
- [24].Sabuncuoglu H, Ozdogan S, Timurkaynak E. Spontaneous regression of extruded lumbar disc herniation: report of two illustrative case and review of the literature Turkish. Neurosurgery 2008;18:392–6. [PubMed] [Google Scholar]
- [25].Buttermann GR. Lumbar disc herniation regression after successful epidural steroid injection. J Spinal Disord Tech 2002;15:469–76. [DOI] [PubMed] [Google Scholar]


