Abstract
Background:
Removing an indwelling urinary catheter as soon as possible is the cornerstone of catheter-associated urinary tract infections (CAUTI) prevention. However, implementing this measure may be challenging in clinical settings. To evaluate the impact of implementing a healthcare workers (HCWs) educational program and a daily checklist for indwelling urinary catheter indications among critical patients on the incidence of CAUTI.
Methods:
This was a quasi-experimental study performed in a general intensive care unit of a tertiary-care hospital over a 12 years period, from January 1, 2005 to December 31, 2016. Rates of urinary catheter use and incidence density of CAUTI were monthly evaluated following the Centers for Disease Control and Prevention (CDC) criteria throughout the study period. Phase I (2005–2006) was the pre-intervention period. In phase II (2007–2010), HCWs routine training on CAUTI prevention was performed twice-a-year. In phase III (2011–2014), we implemented a daily checklist for indwelling urinary catheter indications, in addition to the biannual training. In phase IV, (2015–2016) the biannual training was replaced by training only newly hired HCWs and the daily checklist was maintained.
Results:
The mean rate of urinary catheter utilization decreased from phase I to phase IV (73.1%, 74.1%, 54.9%, and 45.6%, respectively). Similarly, the incidence density of CAUTI decreased from phase I to phase IV (14.9, 7.3, 3.8, and 1.1 per 1000 catheter-days, respectively).
Conclusions:
HCWs education and daily evaluation of indwelling urinary catheter indications were highly effective in reducing the rates of catheter utilization as well as the incidence density of CAUTI.
Keywords: catheter-associated urinary tract infections, healthcare workers education, implementation research, intensive care unit, prevention
1. Introduction
Today, healthcare-associated infections are considered a major public health problem by the World Health Organization (WHO) as they increase morbidity and mortality, length of stay in hospital, and healthcare-associated costs, causing additional suffering for affected patients and their families.[1]
Urinary tract infections are among the most common healthcare-associated infections, accounting for up to 40% of all hospital infections in the United States of America (USA).[2] The most important risk factor for urinary tract infections in a hospital is the temporary use of a indwelling urinary catheter.[3] Catheter-associated urinary tract infections (CAUTI) are the most common urinary tract infections in the United States, causing approximately 13,000 death per year in that country.[4,5] Since patients admitted to intensive care units tend to have a higher use of indwelling urinary catheters than patients admitted to general wards (83% vs 21%, in one study), they are at higher risk for developing CAUTI.[6]
A large survey performed in 703 intensive care units among 50 countries from 2010 to 2015 documented a mean incidence density of 5.07 episodes of CAUTI per 1000 catheter-days.[7] In Brazil, a study performed in 2 intensive care units estimated the rate of CAUTI by 7 episodes per 1000 catheter-days.[8]
However, the true impact of health-care associated infections and CAUTI remains unknown in a large part of the low-income countries in the world,[9] due to the absence or weakness of their surveillance systems, which is essential to determine the magnitude of the problem and to lead the implementation of prevention strategies.[10]
Proven effective strategies include healthcare workers (HCWs) training, active surveillance of CAUTI incidence, use of appropriate technique for the insertion and the maintenance of the catheter, and especially catheter removal as soon as it is not clinically necessary.[11]
One of the main obstacles in the decision regarding removal of the indwelling urinary catheter is the perception of HCWs that patients with severe conditions need to use the device.[10,12] One way to change from perception-based to evidence-based decisions is to promote the implementation of protocols in the clinical setting, with well-defined criteria for the indications of using indwelling urinary catheters.
In the present study, we aimed to evaluate the impact of implementing a HCWs educational program and a daily checklist for indwelling urinary catheter indications among critical patients on the incidence of CAUTI.[13]
2. Methods
This was a quasi-experimental study performed in a 9-beds general intensive care unit of a tertiary-care public-affiliated hospital in Southeast Brazil. The study was carried out over a 12 years period, from January 1st, 2005 to December 31, 2016. The study protocol was approved by the Ethics Committee of the institution.
2.1. Protocol description
The protocol for insertion and maintenance of indwelling urinary catheters was developed and implemented by 2 of the authors, who also worked as an infectious diseases specialist and a registered nurse of the hospital Infection Control Service. This article reports on the protocol implementation during which we collected data on the utilization of indwelling urinary catheters and rates of CAUTI in the intensive care unit.
The protocol implementation had 4 distinct phases. In the first phase, which we call baseline (2005–2006), when an outbreak of CAUTI happened, the clinical team was reminded of prevention measures. This phase corresponds to the status quo prior to the protocol implementation.
A second phase, denominated biannual training (2007–2010), consisted of training of the entire clinical team every 6 months. The training was based on the guide for prevention of CAUTI from the CDC.[11,14] The topics included: criteria for indication of use of indwelling urinary catheter which consisted of patients who: have urinary retention, bladder obstruction or coagulation problems that prevent them from having an intermittent catheter, undergone an urologic procedure or had urethra trauma. The training also included aseptic techniques for catheter insertion and measures for preventing CAUTI.[11,14] Also, during training, the clinical team was presented with the rates of utilization of indwelling urinary catheter and the number and rate of CAUTI occurring in the past 6 months.
In the third phase, denominated checklist plus biannual training (2011–2014), the biannual training sessions continued and a daily checklist to evaluate the indication and/or maintenance of any indwelling urinary catheter was added. During daily rounds, the clinical staff reviewed the criteria for necessity of use of indwelling urinary catheter for each patient in the unit. Three days per week, the physician and nurse of the Infection Control Service reviewed the decisions with the clinical staff, and discussed any cases that did not conform to the indication criteria until and agreement on removing or keeping the indwelling urinary catheter was reached. In this phase, the addition of the checklist intended to facilitate the decision-making by the clinical team.
In the last phase, called checklist and initial training (2015–2016), the biannual training of the entire staff was substituted by a mandatory training to newly-hired personnel, while the daily checklist was maintained. This phase allowed us to evaluate if removal of biannual training would be detrimental to the rates of utilization of indwelling urinary catheter and CAUTI.
2.2. Outcomes and data analysis
The primary study outcome was the rate of indwelling urinary catheters utilization. The secondary study outcome was the incidence density of CAUTI over the 4 phases of the protocol implementation. The number of patient-days was calculated by the sum of all patients per day in the intensive care unit for each month. Similarly, the number of catheter-days was the sum of all patients with an indwelling urinary catheter per day during each month. The percent of catheter utilization was calculated by dividing catheter-days by patient-days and multiplied by 100. The incidence rate of CAUTI per 1000 catheter-days in a month was calculated by the number of new episodes by number of catheter-days and multiplied by 1000.
A new episode of CAUTI was defined as a urinary tract infection that occurred while the patient had an indwelling urinary catheter or within 48 hours from the catheter's removal. We used the CDC criteria for CAUTI, defined as at least 1 of the following signs or symptoms: fever (>38 °C); suprapubic tenderness; costovertebral angle pain or tenderness, and a positive urine culture of ≥105 colony-forming units (CFU)/mL and with no >2 species of microorganisms.[14]
For a comparison of the patients’ severity over the different phases, we evaluated the mean score of the Acute Physiology and Chronic Health Evaluation II (APACHE II)[15] for all the patients admitted in the unit during each phase. For the time-series data, smoothing curves were calculated using lowess procedure to show the tendency of the data over time.
3. Results
Table 1 shows the descriptive analysis of data on indwelling urinary catheter utilization and occurrence of CAUTI. Mean scores for APACHE II were between 23 and 24 and did not vary between different study phases.
Table 1.
Collected data, including utilization of indwelling urinary catheter and catheter-associated urinary tract infections, during each phase of the study.
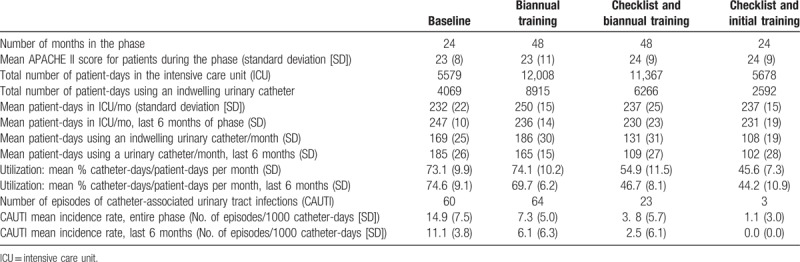
We expected a period of adaptation to each of the protocol implementations, followed by the stabilization of the effect of the protocol. Therefore, for each outcome measure, we present the values calculated for the entire period and for the last 6 months of each phase, when it would be expected that the full effect of the protocol in that phase had been achieved.
The average number of patient-days per month was comparable among the 4 phases, both for the entire periods (means varying from 232 to 250 patient-days per month) and for the last 6 months of each phase (means of 230–247 patient-days per month). The number of catheter-days per month decreased along the phases, from a mean of 169 catheter-days in the baseline to 102 in the last phase. For the last 6 months of each phase, there was a decrease in mean number of catheter-days per month from 185 in the baseline to 102 in the last phase.
The percent of catheter utilization decreased from a mean of 74.6% in the baseline to 44.2% in the last phase. Figure 1 shows the percent of catheter utilization per month for all phases of the study. The percent of catheter utilization decreased consistently in both, the entire period and within each period (specially the second and third phases).
Figure 1.
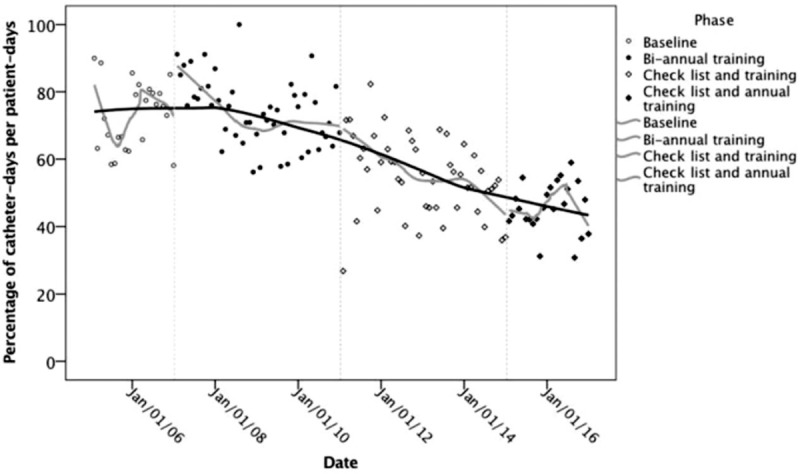
Percent of catheter utilization per month for all phases of the study.
The number of CAUTI decreased substantially over the 4 phases (60 in 24 months during baseline, 64 in 48 months in the biannual training phase, 23 in 48 months in the checklist and biannual training phase, and 3 in 24 months in the checklist and initial training phase). Consequently, the incidence rates decrease during the 4 phases of the study (14.92, 7.34, 3.78, and 1.10 per 1000 catheter-days, respectively), representing a relative decrease of 50% or more from one phase to the next one. Figure 2 shows CAUTI incidence monthly rates for the entire study. The large rate variation from 1 month to another in the baseline decreased as each new infection control measure was implemented. After each new measure was implemented, there was a rapid decrease in the rate, with a subsequent leveling of the rate until the implementation of the next measure. In the last phase, a floor was reached, with most of the months presenting with no case of CAUTI, and with only 1 case per month identified in 3 months.
Figure 2.
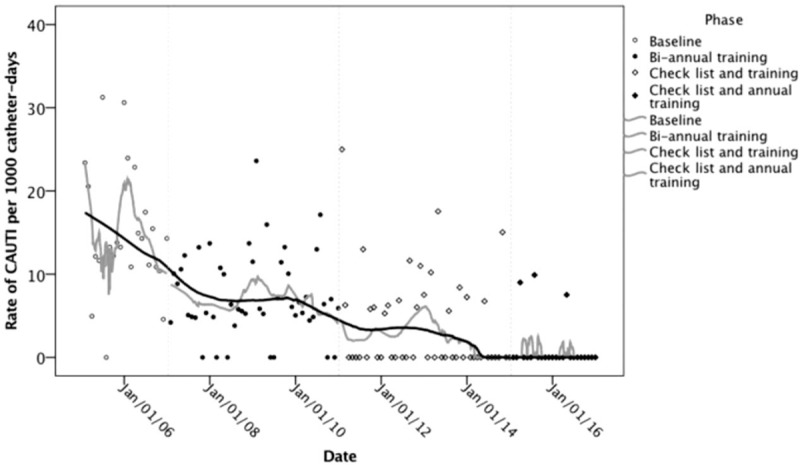
Catheter-associated urinary tract infections incidence monthly rates for all phases of the study.
4. Discussion
HCWs training and implementation of a daily checklist for reviewing the indication of indwelling urinary catheters had a long-term positive impact on the reduction of CAUTI rates in a general intensive care unit in Southeastern Brazil. The rate decreased from 14.9 to 1.1 episodes per 1000 catheter-days from the beginning to the end of the study period. The mean APACHE II was similar in the 4 phases of the study and the type of patients and characteristics of the unit did not significantly change over the study period. Therefore, it is unlikely that those factors might have caused the observed changes and we can attribute the reduction in CAUTI to the implementation of the protocol.
Our results confirm the findings of other studies. Rosenthal et al[16] conducted the implementation of a protocol to reduce the incidence of CAUTI in 57 intensive care units in 15 countries. The protocol implemented in a single phase included education of clinical staff, active surveillance of CAUTI, and feedback on the rates of CAUTI. Before, the protocol implementation, the incidence rate was 7.86 CAUTI per 1000 catheter-days, which was reduced to 4.95 per 1000 catheter-days at the end of the implementation period.
In a study in the Netherlands, physicians participated in educational sessions that emphasized daily re-evaluation of the need of an urinary catheter.[17] Data on catheter use and CAUTI were collected for 2 months before and 2 months after the educational intervention. There was a reduction of days using a catheter (from a median of 7 to 5 days), length of stay in the hospital (from a median of 13 to 9 days), and number of CAUTI (from 4 to 0).
A study conducted in Minneapolis, USA, focused on reducing the unnecessary use of indwelling urinary catheter.[18] In the first phase of the study, the clinical teams received educational material, documented the necessity of the use of the catheter, and received feedback, leading to a reduction of percent of time with catheter from 15.2% to 9.3% during the intervention (5.5 months). However, in the period immediately after (1.2 months), without an intervention, the percentage increased again. In a second phase (27 months), with the same intervention as the first phase, the percentage reduced to 13.6%. A third phase (22.8 months) where a nurse was dedicated to evaluate the indication and need for a catheter, the percent of time with catheter reduced to 12%. During the third phase the percent of use of a catheter in a non-indicated situation reduced from 15% to 1.2%. Apparently, according to the literature, 2 characteristics may be fundamental to the success of the CAUTI prevention: the training or re-training of the clinical staff and the daily evaluation of the need for or continuation of use the urinary catheter in patients in the intensive care.
Our study was performed in a single intensive care unit in Brazil. It would be important to study the implementation of the same protocol in other hospitals or regions to assess if this protocol could be implemented in the entire country. It would be possible that the results we observed were caused by factors other than the implementation of the protocol, such as the introduction of a new type of catheter, for example. However, there were no changes in type of patients and the only changes in procedures that occurred within the intensive care unit were the ones related to the protocol implementation. In addition, reductions in indwelling catheter use and in incidence rate of CAUTI occurred immediately after each new measure implementation and did not increase over the time of the study.
One possible limitation of our study is that we only had aggregated data for patient-days and catheter-days by month, as it is the current practice of hospital surveillance methods. In a future study, one could collect data at the individual level for the patients in intensive care units. For example, one could study the probability that a person develops CAUTI according to the individual's time using an indwelling urinary catheter, while adjusting for other factors such as age, patient severity, and presence of comorbidities, for example.
5. Conclusion
HCWs education and daily evaluation of indwelling urinary catheter indications were highly effective in the long-term reduction of catheter utilization rates as well as the incidence density of CAUTI among critical patients admitted to a general intensive care unit.
Acknowledgments
The authors would like to thank to Ribeirão Preto College of Nursing, University of São Paulo (EERP/USP), and the University Hospital of the Ribeirão Preto Medical School for their support to the study implementation.
Author contributions
Study concept and design: Mayra Gonçalves Menegueti, Fernando Bellissimo-Rodrigues, Ana Maria Laus, Maria Auxiliadora-Martins. Acquisition of data: Mayra Gonçalves Menegueti, Gilberto Gambero Gaspar, and Maria Auxiliadora-Martins. Drafting of the manuscript: Mayra Gonçalves Menegueti, Silvia Rita Marin da Silva Canini, Maria Auxiliadora-Martins, and Marcia A. Ciol. Statistical analysis: Marcia A. Ciol, Mayra Gonçalves Menegueti. Critical revision of the manuscript for important intellectual content: Mayra Gonçalves Menegueti, Fernando Bellissimo-Rodrigues, Maria Auxiliadora-Martins, Ana Maria Laus, Silvia Rita Marin da Silva Canini, Anibal Basile-Filho, Gilberto Gambero Gaspar, Marcia A. Ciol. All authors read and approved the final manuscript.
Conceptualization: Mayra Gonçalves Menegueti.
Formal analysis: Mayra Gonçalves Menegueti, Marcia A. Ciol, Fernando Bellissimo-Rodrigues, Silvia Rita Marin da Silva Canini, Ana Maria Laus.
Investigation: Mayra Gonçalves Menegueti, Fernando Bellissimo-Rodrigues, Maria Auxiliadora-Martins, Gilberto Gambero Gaspar.
Methodology: Mayra Gonçalves Menegueti, Marcia A. Ciol, Fernando Bellissimo-Rodrigues, Anibal Basile-Filho, Ana Maria Laus.
Supervision: Ana Maria Laus.
Writing – original draft: Mayra Gonçalves Menegueti, Marcia A. Ciol.
Writing – review & editing: Marcia A. Ciol, Fernando Bellissimo-Rodrigues, Maria Auxiliadora-Martins, Gilberto Gambero Gaspar, Silvia Rita Marin da Silva Canini, Anibal Basile-Filho, Ana Maria Laus.
Footnotes
Abbreviations: APACHE II = Acute Physiology and Chronic Health Evaluation II, CAUTI = catheter-associated urinary tract infections, CDC = Centers for Disease Control and Prevention, HCWs = healthcare workers, WHO = World Health Organization.
A scholarship to conduct part of doctoral research that provided the accomplishment of this study by the Brazilian Federal Agency for Support and Evaluation of Graduate Education – CAPES.
Publication fee was paid by the Fundação de Apoio ao Ensino, Pesquisa e Assistência do Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FAEPA), a non-profit for organization.
The anonymised datasets analyzed during the current study are available from the corresponding author (MGM; mayramenegueti@usp.br) on reasonable request, as long as this meets local ethics and research governance criteria.
The study protocol was reviewed by the Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto Ethics Committee and approved in its current format (process number 7076). All data were anonymized.
Consent to participate: not applicable.
Consent for publication: not applicable.
The authors declare that they have no competing interest.
None of the authors have any conflict of interest to disclose.
References
- [1].Pittet D. Infection control and quality health care in the new millennium. Am J Infect Control 2005;33:258–67. [DOI] [PubMed] [Google Scholar]
- [2].Saint S, Chenowith CE. Biofilms and catheter-associated urinary tract infections. Infect Dis Clin North Am 2003;17:411–32. [DOI] [PubMed] [Google Scholar]
- [3].Ha US, Cho YH. Catheter-associated urinary tract infections: new aspects of novel urinary catheters. Int J Antimicrob Agents 2006;28:485–90. [DOI] [PubMed] [Google Scholar]
- [4].Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Healthcare Infection Control Practices Advisory Committee. Guideline for Prevention of Catheter-Associated Urinary Tract Infections; 2009. Available at: http://www.cdc.gov/hicpac/cauti/001_cauti.html Accessed July 16, 2015. [DOI] [PubMed] [Google Scholar]
- [5].Klevens RM, Edwards JR, Richards CL, Jr, et al. Estimating health care-associated infections and deaths in U.S. hospitals, 2001. Public Health Rep 2007;122:160–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lewis SS, Knelson LP, Moehring RW, et al. Comparison of non-intensive care unit (ICU) versus ICU rates of catheter-associated urinary tract infection in community hospitals. Infect Control Hosp Epidemiol 2013;34:744–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Rosenthal VD, Al-Abdely HM, El-Kholy AA, et al. International nosocomial infection control consortium report, data summary of 50 countries for 2010-2015: device-associated module. Am J Infect Control 2016;44:1495–504. [DOI] [PubMed] [Google Scholar]
- [8].Regagnin DA, da Silva Alves DS, Maria Cavalheiro A, et al. Sustainability of a program for continuous reduction of catheter-associated urinary tract infection. Am J Infect Control 2016;44:642–6. [DOI] [PubMed] [Google Scholar]
- [9].Allegranzi B, Pittet D. Preventing infections acquired during health-care delivery. Lancet 2008;372:1719–20. [DOI] [PubMed] [Google Scholar]
- [10].Al Nasser W, El-Saed A, Al-Jardani A, et al. Rates of catheter-associated urinary tract infection in tertiary care hospitals in 3 Arabian Gulf countries: a 6-year surveillance study. Am J Infect Control 2016;44:1589–94. [DOI] [PubMed] [Google Scholar]
- [11].Gould CV, Umscheid CA, Agarwal RK, et al. Healthcare Infection Control Practices Advisory Committee. Guideline for Prevention of Catheter-Associated Urinary Tract Infections; 2009. Available at: http://www.cdc.gov/hicpac/cauti/001_cauti. html Accessed July 16, 2017. [DOI] [PubMed] [Google Scholar]
- [12].Saint S, Greene MT, Krein SL, et al. A program to prevent catheter-associated urinary tract infection in acute care. N Engl J Med 2016;374:2111–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].World Health Organization, Peters DH, Tran NT, Adam T. Implementation research in health: a practical guide. Alliance for Health Policy and Systems Research 2013. [Google Scholar]
- [14].Centers for Disease Control and Prevention (CDC), Division of Healthcare Quality Promotion, Brooks J. Using the National Healthcare Safety Network for CAUTI Surveillance. 2012. [Google Scholar]
- [15].Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818–29. [PubMed] [Google Scholar]
- [16].Rosenthal VD, Todi SK, lvarez-Moreno CA, et al. Impact of a multidimensional infection control strategy on catheter-associated urinary tract infection rates in the adult intensive care units of 15 developing countries: findings of the International Nosocomial Infection Control Consortium (INICC). Infection 2012;40:517–26. [DOI] [PubMed] [Google Scholar]
- [17].Janzen J, Buurman BM, Spanjaard L, et al. Reduction of unnecessary use of indwelling urinary catheters. BMJ Qual Saf 2015;22:984–8. [DOI] [PubMed] [Google Scholar]
- [18].Knoll BM, Wright D, Ellingson L, et al. Reduction of inappropriate urinary catheter use at a Veterans Affairs hospital through a multifaceted quality improvement project. Clin Infect Dis 2011;52:1283–90. [DOI] [PubMed] [Google Scholar]


