Abstract
Falling in the elderly is an important social issue, especially for those who are in long-term care (LTC) facilities, in addition to being a significant economic burden. This study aims to investigate the epidemiological characteristics and identify the factors influencing falls in LTC residents.
We enrolled 260 participants aged 60+ years by multistage sampling across 13 LTC facilities in Xiamen, China, in 2016. Epidemiological characteristics and falls were observed and recorded during a 12-month period using a revised FROP-Com Scale. Multiple logistic regression modeling was performed to determine the factors influencing falls.
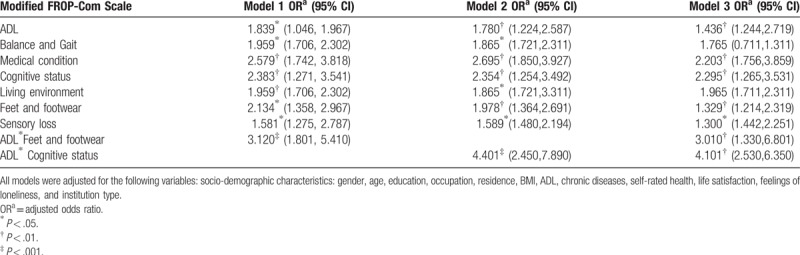
A total of 218 (83.8%) valid questionnaires were returned. 152 falls (range 1–7, mean 0.7 ± 1.3 falls/person/y) occurred in the previous year, with 69 residents (31.7%) experiencing 1 or more falls. Most participants who fell were female (71%), living in cities (85.5%), had a higher BMI (22.1 ± 4.2), and had a chronic disease (99.9%). Of all falls, 39.1% occurred in the bedroom and 26.1% in the bathroom, 58% during daytime hours between 6:00 am and noon. Thirty-six percent of falls resulted in an injury (e.g., bruises and fractures). The principal reason for falling was due to slipping (23.2%). There were 2 interactions on fall rate between ADL and feet and footwear (OR = 3.120, P<.001; OR = 3.010, P = .007 in Models 1 and 3), and between ADL and cognitive status (OR = 4.401, P<.001; OR = 4.101, P = .005 in Models 2 and 3). Multiple regression analysis indicated that ADL, balance and gait, medical conditions, cognitive status, living environment, feet and footwear and sensory loss were factors influencing falls among elderly adults in LTC facilities.
Falls occur frequently and mostly unwitnessed among elderly adults in LTC facilities, highlighting the need for more effective and individualized fall prevention. Fall efficacy enhancing programs for nursing home residents should take degree of self-care, chronic diseases, sensory loss, foot injuries, cognitive impairment, living environment, and gender into account.
Keywords: epidemiological characteristics, fall, influencing factors, long-term care facilities
1. Introduction
With the rapid growth of the world's elderly population, their health causes unprecedented concern. Falls and fall-related injuries are an important aspect of the health problems of elderly people, accounting for 40% of all deaths due to injury. The World Health Organization (WHO) definition of a fall in a 2007 report was “inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest in furniture, wall, or other objects.” Fall-related injuries are common,[1–3] resulting in considerable burden on healthcare institutions and are a major cause of long-term pain and functional impairment among older adults.[4] They also substantially increase the risk of discharge to a nursing home[5] and result in high economic cost.[6]
Approximately 28% to 35% of people aged 65 and over fall each year, increasing to 32% to 42% for those over 70 years of age (WHO 2007). The frequency of falls increases with age and level of frailty.[7] Older people living in nursing homes fall more often than those living in the community. WHO stated in the “World Report on Ageing and Health” in 2015 that approximately 30% to 50% of people living in long-term care (LTC) institutions fall each year, and 40% of those experienced recurrent falls. Falls can cause moderate to severe injuries, such as hip fractures and head trauma, increasing the risk of early death.[8] Among older adults, falls are the leading cause of death due to injury. They are also the most common cause of nonfatal injury and hospital admissions due to trauma. Many who fall, even those who are not injured, develop a fear of falling. This fear may cause them to limit activity—leading to reduced mobility and loss of physical fitness, which in turn increases the risk of falling.[9]
LTC facilities, also known as residential care or nursing homes, include institutional facilities for residents that require on-site staff for routine care, owing to chronic illnesses, disabilities, or cognitive impairment.[10] Design of LTC facilities for older people has become increasingly crucial policy concerns in developing countries and the rapidly aging Asia, especially China. Falls are more common in older people who are in nursing and residential care facilities than in those who live in the community, and it has been argued that screening is not needed in this population because all residents are at increased risk.[11] The circumstances associated with falls leading to fractures have been well documented in some developed countries, but little is known about such accidents in developing countries, where the elderly population is increasing rapidly.[12] In addition, the current epidemiological studies on falls in institutions of different types and regions are not sufficiently comprehensive.[13] Although there have been many studies of falls in the elderly and the factors that influence them, there remains a lack of research on their epidemiological status and the factors influencing falls among the elderly in LTC institutions.[14–16] In particular, little existing research involves institutional-level considerations of falls such as gender differences in different residential settings or the attributes of institutions.[17] Therefore, this study aims to investigate the epidemiological characteristics and identify the factors influencing falls in LTC residents.
2. Methods
2.1. Participants
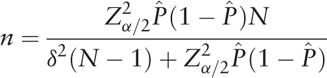
A cross-sectional study was performed on individuals aged ≥60 years living in LTC institutions for at least 1 year. The initial sample size was calculated by the following formula. A total of 32 LTC facilities (3250 elderly people) are located in Xiamen, China in 2016.  was set at 12% to 19%, according to the previous survey in China.[18,19] Hence, the calculated sample size was 154 to 220 individuals. However, in order to ensure the quantity and quality of the questionnaire, we intended to recruit 260 participants. In the first stage, there were 32 LTC institutions in Xiamen, including 22 in urban areas and 10 in townships by the end of 2015. Based on the urban-rural differences and the ratio of about 2:1, LTC institutions of 9 cities and 4 towns were selected according to the random number table method. The second stage, based on the nature of the LTC institutions and the ratio of about 1:1, this study randomly selected 4 public and 5 private LTC institutions in the city, as well as 2 public and 2 private LTC institutions in the township area. Finally, we selected participants from 13 LTC institutions, including 8 private agencies and 5 public nursing facilities across urban and rural areas. Two hundred sixty elderly residents were selected (20 seniors per facility; 8% of the overall elderly population in those LTC facilities) for on-site investigation, according to the urban or rural areas and institutional attributes in 2016 (June 1 to September 30).
was set at 12% to 19%, according to the previous survey in China.[18,19] Hence, the calculated sample size was 154 to 220 individuals. However, in order to ensure the quantity and quality of the questionnaire, we intended to recruit 260 participants. In the first stage, there were 32 LTC institutions in Xiamen, including 22 in urban areas and 10 in townships by the end of 2015. Based on the urban-rural differences and the ratio of about 2:1, LTC institutions of 9 cities and 4 towns were selected according to the random number table method. The second stage, based on the nature of the LTC institutions and the ratio of about 1:1, this study randomly selected 4 public and 5 private LTC institutions in the city, as well as 2 public and 2 private LTC institutions in the township area. Finally, we selected participants from 13 LTC institutions, including 8 private agencies and 5 public nursing facilities across urban and rural areas. Two hundred sixty elderly residents were selected (20 seniors per facility; 8% of the overall elderly population in those LTC facilities) for on-site investigation, according to the urban or rural areas and institutional attributes in 2016 (June 1 to September 30).
 |
The study protocol was approved by the ethical review committee of the School of Public Health, Xiamen University. All participants read a statement that explained the purpose of the survey and provided signed informed consent prior to participation in the study.
2.2. Data collection
Respondents of the questionnaire were elderly residents, or their family members or caregivers if the participants were unable to answer. The content of the survey mainly comprised questions describing the residents, epidemiological characteristics of the falls, and the revised Falls Risk for Older People-Community setting (FROP-Com) Scale. This FROP-Com scale was from The National Ageing Research Institute (NARI) in Australia.[20] The survey was conducted from June 1, 2016 to July 5, 2016. No gifts or rewards were given to any participant. Each interview required between 30 and 40 minutes to complete. In order to ensure the orderly conduct of the investigation, a standard operating procedure (SOP) was created to provide uniform training to the investigators. A return survey was conducted in order to check missing data if questionnaires were incomplete.
2.3. Characteristics of the participants
Social demographic and socioeconomic data, including gender, age, marital status, occupation, residence, economic status, and relevant health indicators, were collected. Health data mainly included degree of self-care, the presence of any chronic disease and mental health status.
2.4. Fall characteristics
An event was considered a fall when the staff saw an elderly person landing on the floor or they were found lying on the floor as a result of a fall. Staff recorded all witnessed and unwitnessed falls on a structured table in LTC facilities. This structured table only recorded simple information such as the number of falls and whether the fall was witnessed. The total number of falls suffered over a 12-month period (May 31, 2015 to May 31, 2016) was entered onto the structured table by institutional managers. Fall rate was expressed as the mean number of falls per year per resident. In addition, details of the most recent fall, including the precise time, location, direction, reason and consequences of the fall for the elderly were collected through the questionnaire.[21]
2.5. Revised FROP-Com scale
Due to the FROP-com scale was designed for the elderly in the community, the elderly in the LTC institutions may be different from the elderly in the community in terms of their physical condition and fall rate. Previous literatures have shown that the FROP-com scale should be modified properly to study the falls of the elderly in LTC institutions.[22] Therefore, based on the risk factors of falling in elderly people retrieved from the existing research literature, the FROP-Com scale was revised by combining the actual description of each resident in the LTC institutions, comprising principally the following information: Activity of Daily Living (ADL), balance and gait, medical conditions, cognitive status, living environment, foot injuries and footwear and sensory loss. The score range for each parameter was 0 to 4. The higher the score, the worse the physical condition or living environment of the resident.
ADL was measured using a modified Katz Activities of Daily Living Scale, which included 6 basic activities: eating, toileting, bathing, dressing, getting in and out of bed and mobility. The degree of self-care of each resident was collated and classified into 4 categories: completely independent, relatively independent, moderately disabled, or totally disabled.[23] Balance and gait were measured using the Dynamic Gait Index (DGI), and included eight items: walking, turning, crossing, bypassing, stepping up and down, etc.[24] Residents’ medical conditions, including diseases and medications, were extracted from the electronic medical records in the LTC facilities. The survey mainly asked about their medical history, quantity of prescription drugs, whether they suffered a chronic medical condition(s) affecting their balance or mobility, etc. Since the measurement of cognitive function in the original FROP-com scale is relatively simple, cognitive status was measured using a Mini-Mental State Examination (MMSE) and graded residents into complete cognitive function, mild cognitive impairment, moderate cognitive impairment, or severe cognitive dysfunction.[25] The safety of the living environment was determined principally by the number of risk factors, including antiskid devices, lighting conditions, and unreasonable placement of furniture, etc. We trained investigators to investigate the indoor (living room, bathroom, aisle, etc.) and outdoor (corridor, staircase, armrest, etc.) living environment of the elderly in LTC institutions. Foot injuries and footwear were evaluated by enumerating the number of foot problems, including corns, bunions, swellings, etc. and whether inappropriate, poorly fitting, or worn footwear were used. Sensory loss was evaluated using a comprehensive assessment of the auditory, visual, tactile, and positional perception capabilities of each resident.[26]
2.6. Statistical analysis
We reported the mean, standard deviation, percentage, range and frequency with respect to fall rate, circumstances of falls, and characteristics of the elderly residents. Differences between the group of residents who suffered falls and those who did not were tested for statistical significance using a χ2 or t test. Multiple logistic regression was performed to determine the factors that influenced falls. Mutually adjusted odds ratios (OR) with 95% confidence intervals were calculated. All statistical calculations were carried out using SAS version 9.3 software (SAS Institute Inc, Cary, NC).
3. Results
3.1. Characteristics of the residents and falls
During the study period, a total of 260 participants who resided in LTC facilities were selected for the study. Forty-two residents were excluded due to incomplete data, thus 218 patients were analyzed (mean age 80.1 ± 8.3 years; range 63–97). Sixty-nine residents (31.7%) experienced 1 or more falls, the majority of whom were female (71%), lived in cities (85.5%), had a high BMI (22.1 ± 4.2), and had chronic diseases (99.9%) (Table 1).
Table 1.
Prevalence of the elderly characteristics in the research population.
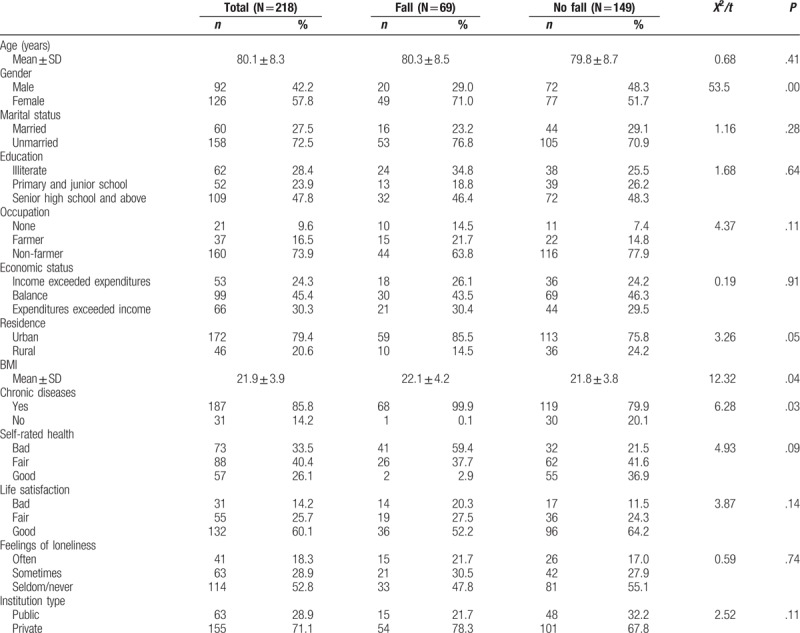
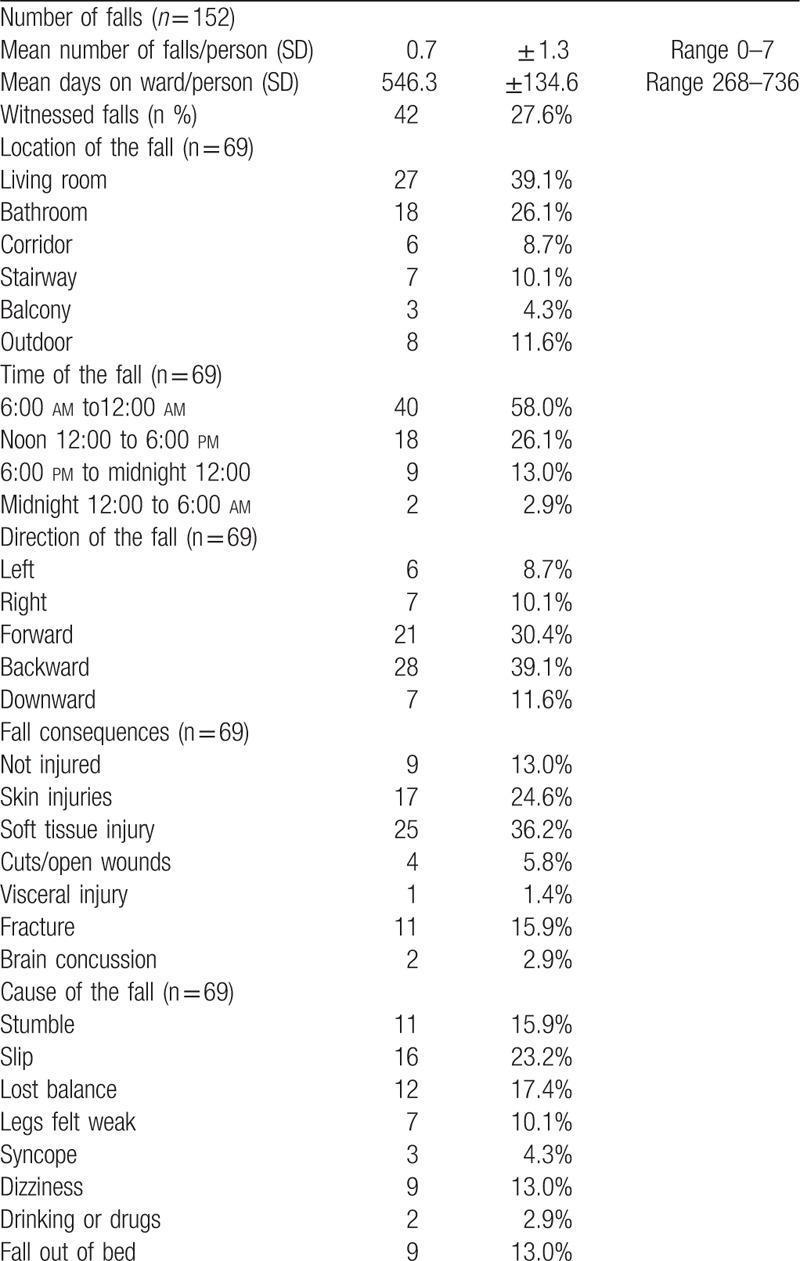
A total of 152 falls (female 92; range 1–7; mean 0.7 ± 1.3 falls/person/y) occurred in 12 months, 39.1% of which occurred in the bedroom and 26.1% in the bathroom. Staff witnessed 27.6% of falls. Most occurred during daytime hours, 58% between 6:00 am and noon. Almost a quarter of falls (23.2%) were due to slipping and 36% resulted in an injury (e.g., bruises, fractures), but 15.9% suffered a hip fracture and died within a month from complications (Table 2).
Table 2.
Characteristics of falls.
3.2. Fall-related factors
As the number of criteria for each of the 7 core parts of the revised FROP-Com scale differed, the mean score of each concept was used in the analysis. The results in Table 3 show that the elderly who had fallen had significantly higher scores for ADL, balance and gait, medical conditions, cognitive status, living environment, feet and footwear and sensory loss, compared with elderly residents who had not fallen (P < .01).
Table 3.
Mean and standard deviation scores for the Modified FROP-Com Scale in the study population.
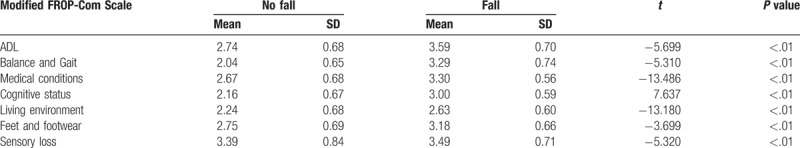
The main effects and the significant interaction effects of the fall rate in the 7 core parts of the modified FROP-Com Scale among the elderly by multiple logistic regression analysis are shown in Table 4. All 3 models are adjusted for all socio-demographic characteristics. As model 3 shows, the elderly who had higher ADL, balance and gait, medical conditions, cognitive status, living environment, feet and footwear, and sensory loss scores were more likely to fall. Importantly, there were 2 interactions on fall rate between ADL and feet and footwear (OR = 3.120, P<.001; OR = 3.010, P = .007 in Models 1 and 3), and between ADL and cognitive status (OR = 4.401, P<.001; OR = 4.101, P = .005 in Models 2 and 3). The above 2 interactions were examined by likelihood ratio tests P = .032, .013, respectively.
Table 4.
Main effects and interaction effects of the fall rate among the elderly characteristics in the research population.
4. Discussion
In this study, the main findings were that 31.7% of residents experienced 1 or more falls during the study period. Falls had serious consequences, were most often unwitnessed, and occurred within the bedroom or bathroom. As many as 15.9% of residents suffered a hip fracture and died within a month from complications. Falls occurred most frequently during the daytime. Furthermore, there were 2 interactions on fall rate between ADL and feet and footwear, and ADL and cognitive status. The elderly who had higher ADL, balance and gait, medical conditions, cognitive status, living environment, feet and footwear or sensory loss scores were more likely to fall.
In our study, 31.7% of residents experienced 1 or more falls during the 12-month long study period. In previous studies, the median incidence of falls was 18%, although 24.6% had a recurrent fall over a 1-year period in elderly Chinese people in Mainland China, Hong Kong, Macau, Singapore, and Taiwan.[27,28] Older people living in LTC facilities fell more often than those living in the community, mainly because older people living in LTC institutions are generally in worse physical condition than those in the community.
In addition, we found a large number of falls occurred without staff being present. For 72.4% of the falls the precise cause is unknown. To prevent a fall, it is important to know what happened before and during a fall. Similar findings have been reported in previous studies, with most falls occurring in the bedroom or common areas.[29] Recent studies have shown that falls in common areas in a nursing home occur due to incorrect weight shifting during walking, sitting down and when changing position while standing.[30] This study further confirms that the location of falls is most frequently within the bedroom or bathroom, generally in the morning and most often due to slipping. Therefore, to get more insight into the exact circumstances, it may be necessary to monitor bathroom and bedrooms all day long. Monitoring could prevent falls by providing feedback to the patient before making a high-risk movement, or the monitoring system could signal nursing staff for help.
Another finding in our study was that falls mainly affected women, the poor self-care ability and those with poor cognitive functioning, consistent with the previous findings.[31–33] Previous reports confirm that women's activity and participation in LTC institutions is significantly higher than that of men, which increases the risk of falls.[34] In addition, with declining ability to perform self-care and cognitive function, this study found that the number of female falls was significantly higher than that of men. On one hand, the reason may be that women are more likely than men to sustain fractures when they fall.[12] On the other hand, relevant research reports that women's fear of falling may hinder their participation in physical exercise or social activities[35] and suggests that women are 2 to 3 times more likely to report symptoms of depression,[36,37] which may result in women being more prone to falls as they become more debilitated.
An important finding in our study was that the main causes of falls include both internal and external causes. External causes are mainly related to the living environment and shoes. According to the survey, 39% of falls in LTC institutions are closely related to the surrounding living environment. Moreover, inappropriate footwear has been described as a risk factor for injurious falls of residents in nursing homes.[14,38] Our study suggests that 23.2% the elderly fell due to slipping and the consequences of a fall may be particularly severe if open slippers are worn as they can prevent evasive action, such as stepping, which would reduce potential injuries from falls. Therefore, managers and nursing staff should work together to assess the safety of the living environment of the elderly to eliminate risk factors. The quality of life of the elderly can be improved and the risk of falling can be reduced by changing the living environment in LTC facilities.
Previous studies have reported that a lack capability to perform self-care is associated with a fear of falling. This fear represents another barrier for elderly individuals who are seeking to regain their self-care capability.[37,39] Older adults tend to reduce daily activities due to the fear of falling, and this contributes to a growing weakness in the lower limb muscles.[34] It has been reported that low physical activity levels are associated with a reduced quality of life and higher rates of morbidity and mortality.[40] Even when in poor health, some elderly adults are unwilling to rely on others for assistance. These individuals may even feel uncomfortable calling for necessary help, which may contribute to accidents. Thus, nursing staff should increase the frequency of inspections and master the knowledge and skills necessary to understand the physical and psychological traits of older adults.
The majority of elderly people in LTC institutions suffer from chronic diseases such as hypertension, heart disease, diabetes, joint or muscular diseases and require long-term medication.[41] With age, physiological decline of the elderly including musculoskeletal disorders, gait instability, visual acuity, hearing loss and injured lower limbs, even fractures, leads to a significant increase in the risk of falls.[42] Effective fall prevention nursing assessment and management can minimize the risk of falls and thus improve the quality of care to protect the safety of the elderly.
There are several limitations associated with this study. First, the data were derived from a cross-sectional survey and this limited the interpretation of our results, making it hard to draw causal conclusions. Second, the participants were sampled from one city in China, and the sample size of this study was relatively small, which may not be representative of the situation nationwide, causing some bias in interpretation. Third, due to the data limitations of LTC institutions, we were unable to obtain detailed epidemiological information on all the falls that occurred in elderly residents over a year. Fourth, fall could be considered a marker of care quality, therefore if the number of assistants or nurses or medical staff could influence this marker. In the follow-up of this study, the number and quality of caregivers will be considered. Fifth, the revised FROP-com scale needs to be further tested and evaluated in this study. Therefore, large-scale longitudinal studies are required to assess the effects of fall prevention measures in LTC institutions. In particular, we hope to further explore the effectiveness of different interventions in different types of LTC institutions in the future.
5. Conclusions
In conclusion, elderly people living in LTC facilities fall more often than those living in the community. Most falls were not witnessed. Factors influencing falls were: ADL, balance and gait, medical conditions, cognitive status, living environment, feet and footwear, and sensory loss. Targeted interventions should be taken to reduce the fall rate of each institution. First, we need to enhance and modify private and rural nursing facilities, focusing on women, the poor self-care ability and those with cognitive impairment. Furthermore, the managers of LTC institutions should widen the monitoring of falls among the elderly through smart wearable devices or emergency buttons within institutions and establish relevant contingency plans. Third, nursing facilities need to focus on strengthening cognitive interventions, exercising to improve balance, correct gait, enhancing the comfort and fitness of shoes, and management of medication for the elderly, in addition to developing environmental programs such as adding nonslip mats and handrails to bathrooms. Last but not the least, LTC institutions should establish an ability assessment system of the elderly, including incapacitation and evaluation of falls. In addition, an LTC insurance system should be established to reduce the burden of disability caused by falls.
5.1. Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author contributions
Conceptualization: Liangwen Zhang.
Formal analysis: Liangwen Zhang.
Funding acquisition: Yanbing Zeng, Ya Fang.
Investigation: Liangwen Zhang, Chenziheng Weng, Jiajin Yan.
Methodology: Liangwen Zhang.
Writing – original draft: Liangwen Zhang.
Writing – review & editing: Liangwen Zhang, Yanbing Zeng, Ya Fang.
Footnotes
Abbreviations: ADL = activity of daily living, DGI = dynamic gait index, FROP-Com = Falls Risk for Older People-Community setting, LTC = long-term care, MMSE = Mini-Mental State Examination, OR = odds ratios, SOP = standard operating procedure, WHO = World Health Organization.
LZ and YZ contributed to the work equally and should be regarded as co-first authors.
This research was supported by the Project of Fujian Province Natural Science Fund (Ref. 2017J01133), the Project of National Natural Science Fund (Ref. 71874147), and the Project of National Natural Science Fund (Ref. 81573257) in China.
The authors have no conflicts of interest to disclose.
References
- [1].Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006;35suppl 2:ii37–41. [DOI] [PubMed] [Google Scholar]
- [2].Stevens JA, Mack KA, Paulozzi LJ, et al. Self-reported falls and fall-related injuries among persons aged ≥65 years—United States, 2006. J Safety Res 2008;39:345–9. [DOI] [PubMed] [Google Scholar]
- [3].Morrison A, Fan T, Sen SS, et al. Epidemiology of falls and osteoporotic fractures: a systematic review. Clin Outcomes Res 2013;5:9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hartholt KA, van Beeck EF, Polinder S, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma 2011;71:748–53. [DOI] [PubMed] [Google Scholar]
- [5].Gill TM, Murphy TE, Gahbauer EA, et al. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol 2013;178:418–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Davis JC, Robertson MC, Ashe MC, et al. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int 2010;21:1295–306. [DOI] [PubMed] [Google Scholar]
- [7].Buckinx F, Reginster JY, Petermans J, et al. Relationship between frailty, physical performance and quality of life among nursing home residents: the SENIOR cohort. Aging Clin Exp Res 2016;28:1149–57. [DOI] [PubMed] [Google Scholar]
- [8].Centers for Disease Control and Prevention. Falls among older adults: an overview. Home and Recreational Safety Web site. Available at: http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html. [Google Scholar]
- [9].Vellas BJ, Wayne SJ, Romero LJ, et al. Fear of falling and restriction of mobility in elderly fallers. Age Ageing 1997;26:189–93. [DOI] [PubMed] [Google Scholar]
- [10].Scott V, Votova K, Scanlan A, et al. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing 2007;36:130–9. [DOI] [PubMed] [Google Scholar]
- [11].Rosendahl E, Lundinolsson L, Kallin K, et al. Prediction of falls among older people in residential care facilities by the Downton index. Aging Clin Exp Res 2003;15:142–7. [DOI] [PubMed] [Google Scholar]
- [12].Coutinho ES, Bloch KV, Rodrigues LC. Characteristics and circumstances of falls leading to severe fractures in elderly people in Rio de Janeiro, Brazil. Cadernos De Saúde Pública 2009;25:455–9. [DOI] [PubMed] [Google Scholar]
- [13].Deandrea S, Bravi F, Turati F, et al. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta-analysis. Arch Gerontol Geriatr 2013;56:407. [DOI] [PubMed] [Google Scholar]
- [14].Botwinick I, Johnson JH, Safadjou S, et al. Geriatric nursing home falls: a single institution cross-sectional study. Arch Gerontol Geriatr 2016;63:43. [DOI] [PubMed] [Google Scholar]
- [15].Hartog LC, Cizmar-Sweelssen M, Knipscheer A, et al. The association between orthostatic hypotension, falling and successful rehabilitation in a nursing home population. Arch Gerontol Geriatr 2015;61:190–6. [DOI] [PubMed] [Google Scholar]
- [16].Angelousi A, Girerd N, Benetos A, et al. Association between orthostatic hypotension and cardiovascular risk, cerebrovascular risk, cognitive decline and falls as well as overall mortality: a systematic review and meta-analysis. J Hypertens 2014;32:1562. [DOI] [PubMed] [Google Scholar]
- [17].Rapp K, Becker C, Cameron ID, et al. Epidemiology of falls in residential aged care: analysis of more than 70,000 falls from residents of Bavarian nursing homes. J Am Med Dir Assoc 2012;13: 187.e1–187.e6. [DOI] [PubMed] [Google Scholar]
- [18].Lai ZM, Zhang CF, Chen QL, et al. Investigation on the incidence of falls among the elderly in nursing homes in Nanhai District, Foshan City. China Minkang Med 2007;19:83–4. [Google Scholar]
- [19].Zhao M, Wang H, He Y, et al. Analysis of epidemiological characteristics and risk factors of falls in elderly people in old-age care institutions. Chin J Emergency Med 2016;25:654–8. [Google Scholar]
- [20].The National Ageing Research Institute. 2015. Available at: https://www.nari.net.au/resources/health-professionals/falls-and-balance. [Google Scholar]
- [21].Elliott SJ, Ivanescu A, Leland NE, et al. Feasibility of interdisciplinary community-based fall risk screening. Am J Occup Ther 2012;66:161. [DOI] [PubMed] [Google Scholar]
- [22].Ding YY, He GR, Chen Y, et al. Analysis on status quo of falls of the elderly in pension institutions. General Nurs 2014;2883–4. [Google Scholar]
- [23].Chen W, Fang Y, Mao F, et al. Assessment of disability among the elderly in Xiamen of China: a representative sample survey of 14,292 older adults 2015;10:e0131014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Nukala B, Rodriguez A, Tsay J, et al. Evaluating Optimal Placement of Real-Time Wireless Gait Analysis Sensor with Dynamic Gait Index (DGI)[C]//IEEE Cisti. IEEE 2014. [Google Scholar]
- [25].Trivedi D. Cochrane Review Summary: Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Primary Health Care Res Dev 2017;1. [DOI] [PubMed] [Google Scholar]
- [26].Zhang L, Weng CS, Wang QH. Effect of vestibular sense, proprioception, and vision on fall risk in elderly. Chin J Rehabil Theory Pract 2010. [Google Scholar]
- [27].Kwan, et al. J Am Geriatr Soc 2011;59:536–43. [DOI] [PubMed] [Google Scholar]
- [28].Schoene D, Valenzuela T, Lord SR, et al. The effect of interactive cognitive-motor training in reducing fall risk in older people: a systematic review. BMC Geriatr 2014;14:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Stenhagen M, Ekström H, Nordell E, et al. Falls in the general elderly population: a 3- and 6- year prospective study of risk factors using data from the longitudinal population study “Good ageing in Skane”. BMC Geriatr 2013;13:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Kosse NM, de Groot MH, Vuillerme N, et al. Factors related to the high fall rate in long-term care residents with dementia. Int Psychogeriatr 2015;27:803–14. [DOI] [PubMed] [Google Scholar]
- [31].Jefferis Barbara J, Iliffe S, Kendrick D, et al. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr 2014;14:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Schwartz AV, et al. Older women with diabetes have a higher risk of falls. Diabetes Care 2002;25:1749–54. [DOI] [PubMed] [Google Scholar]
- [33].Tayama M, Moriguchi K, Asada T. The relationship between memory of falling and cognitive function in nursing home residents. Alzheimers Dementia 2010;6:S316–1316. [Google Scholar]
- [34].Delbaere K, Crombez G, Vanderstraeten G, et al. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing 2004;33:368e73. [DOI] [PubMed] [Google Scholar]
- [35].Büchele G, Becker C, Cameron ID, et al. Predictors of serious consequences of falls in residential aged care: analysis of more than 70,000 falls from residents of Bavarian nursing homes. J Am Med Directors Assoc 2014;15:559. [DOI] [PubMed] [Google Scholar]
- [36].Shafer K, Pace GT. Gender differences in depression across parental roles. Soc Work 2015;60:115–25. [DOI] [PubMed] [Google Scholar]
- [37].Sharifi F, Fakhrzadeh H, Memari A, et al. Predicting risk of the fall among aged adult residents of a nursing home. Arch Gerontol Geriatr 2015;61:124–30. [DOI] [PubMed] [Google Scholar]
- [38].Becker C, Rapp K. Fall prevention in nursing homes. Clin Geriatr Med 2010;26:693. [DOI] [PubMed] [Google Scholar]
- [39].Chang SH. Beliefs about self-care among nursing home staff and residents in Taiwan. Geriatr Nurs 2009;30:90–8. [DOI] [PubMed] [Google Scholar]
- [40].Nguyen AM, Arora KS, Swenor BK, et al. Physical activity restriction in age-related eye disease: a cross-sectional study exploring fear of falling as a potential mediator. BMC Geriatr 2015;15:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].El-Khoury F, Cassou B, Charles MA, et al. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ 2013;347:f6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Scott V, Votova K, Scanlan A, et al. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing 2007;36:130–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


