Abstract
The aim of this study was to evaluate the impact of home health care (HHC) for disabled patients.
We conducted a nationwide population-based retrospective cohort study. A total of 5838 disabled patients with HHC were identified to match by propensity score with 15,829 disabled patients without HHC receiving tube or catheter care (tracheostomy tube, nasogastric tube, urinary catheter, cystostomy tube, nephrostomy tube) or stage 3 or 4 pressure sore care from the Taiwanese National Health Insurance Research Database between 2005 and 2009. After 1:1 matching, 2901 subjects in the HHC group and 2901 subjects in the non-HHC group were selected and analyzed. Generalized estimating equations (GEEs) were used to compare the risk of health outcomes (rate of hospitalization and emergency services use) and the healthcare expenditure between the 2 groups.
Compared to those in the non-HHC group, the patients in the HHC group had significantly higher risk for hospitalization (odds ratio [OR] = 18.43, 95% confidence interval [CI]: 15.62–21.75, P < .001) and emergency services use (OR = 3.72, 95% CI: 3.32–4.17, P < .001) 1 year before the index date. However, 1 year after the index date, the risk for hospitalization (OR = 1.6, 95% CI: 1.41–1.83, P < .001) and emergency services use (OR = 1.16, 95% CI: 1.04–1.30, P < .05) attenuated significantly. Regarding the comparison of total healthcare expenditure 1 year before and after the index date, our study showed an insignificant decrease of US$1.5 per person per day and a significant increase of US$5.2 per person per day (P < .001) in the HHC and non-HHC groups, respectively.
The HHC for disabled patients has a potential role to reduce hospitalization and emergency services use. Besides, the improvement of healthcare quality through HHC was not accompanied by increased healthcare expenditure. The clinical impact of HHC emphasizes the importance for public health officials to promote HHC model to meet the needs of disabled patients.
Keywords: health expenditure, home health care, long-term care, quality of health care
1. Introduction
Home health care (HHC) services are important for population with severe disability. As the world's population grows older, the rates of potentially disabling diseases increase.[1] Patients with multiple chronic illness are associated with higher mortality rates and disabilities, more numbers of hospital admission and institutionalization, and increased healthcare expenditure.[2–4] “Disabled people,” defined by the International Classification of Functioning, Disability and Health (ICF), are people who have body function or structure impairment and limitations or restrictions for daily activities.[5] According to the data from World Health Organization (WHO), approximately 15% of the world's population have suffered from some forms of disability. There are unmet health care needs of people with disabilities because of their less access to healthcare services.[5] Besides, providing optimal care for elderly adults with multiple chronic diseases or comorbidities is challenging.[3] HHC services, including home nursing visits and physician visits, can make healthcare services more accessible, continuous, and comprehensive for the disabled.
The HHC programs have been established in many countries in different forms to care for patients with multiple comorbidities or disabilities. However, results of different HHC programs were controversial with insufficient data to determine the clinical impacts and economic effects.[2,6–9] It is also unclear from the available evidences that which components of HHC can contribute toward the benefit of disabled people.[7] Some studies showed that HHC after hospitalization and home-based primary care reduced risks of readmission and mortality, improved continuity of care as well as quality of life, and decreased overall costs.[2,10–12] Intensive HHC could also be an effective alternative to hospitalization for the selected elderly with acute medical conditions.[13,14] On the contrary, a Dutch randomized controlled study showed no significant difference in emergency services use and quality of life for people receiving HHC.[8] Moreover, the effectiveness of HHC in rural areas is a concern because of the higher proportion of people over 65 years of age and fewer healthcare providers in rural areas than in urban areas.[15,16] A Japanese study mentioned that HHC, compared to institutional care, increased the healthcare expenditure in rural areas.[9]
In Taiwan, HHC services for disabled patients are carried out by nurses, also acting as case managers, and physicians. In addition to these required disciplines, some HHC agencies have an interdisciplinary team, including rehabilitation therapists (physical therapists, occupational therapists, and speech/swallowing therapists), social workers, dietitians, and pharmacists. HHC services have been reimbursed by the National Health Insurance (NHI) program since 1995. The patients fulfilling the following 2 criteria are qualified for reimbursement: limited self-care ability with activities of daily living scale score <60; needs of specific medical care or skilled nursing services, including changing of catheters or tubes (urinary catheter, nasogastric tube, tracheostomy tube, nephrostomy, or cystostomy tube) and stage 3 or 4 pressure sore care.[17] Most of the patients are referred to home health care teams by medical providers due to the need of skilled nursing services. The patients can receive HHC at home, in nursing homes or long-term care facilities. The patients receiving HHC are categorized by 4 resource utilization groups (RUGs) according to the NHI reimbursement policy: RUG-1 is patients with HHC who need medical care or general nursing services only; RUG-2 to RUG-4 are groups of patients with HHC who need 1, 2, and more than 3 kinds of skilled nursing services, respectively.[17]
Previous study has assessed the type and rate of utilization of HHC services among the older population in Taiwan.[17] However, there was no study examining the impact of HHC services model in Taiwan. The aim of this study was to assess whether the HHC program, with mainly regular nursing and physician visits, was effective to improve health outcomes and reduce the healthcare expenditure.
2. Methods
2.1. Data source
In this population-based study, data were obtained from the Longitudinal Health Insurance Database 1996 to 2010, a database subset which contained the data of one million individuals randomly selected from the National Health Insurance Research Database (NHIRD) in 2010. NHIRD, a nationwide representative database, contains all original claims and registered data of reimbursement for NHI beneficiaries. Taiwan's high- performing single-payer NHI, which was launched in 1995, has provided universal health coverage for more than 99% of the population.[18] The study protocol was approved by the institutional review boards of National Health Research Institutes in Taiwan (EC1030701-E).
2.2. Design and study subjects
We conducted a population-based retrospective cohort study to compare health outcomes and the healthcare expenditure between patients with HHC and outpatient clinic patients receiving tube or catheter care (tracheostomy tube, nasogastric tube, urinary catheter, cystostomy tube, nephrostomy tube) or stage 3 or 4 pressure sore care between 2005 and 2009. We selected the patients receiving skilled nursing services at outpatient clinics as the control group (the non-HHC group) because most of the patients with HHC were referred to home health care teams by medical providers due to the need of skilled nursing services. The HHC group (n = 3835) was identified by outpatient claims with case type code 61, 66, or 67, but hospice home care (case type code 65) patients were excluded. The date of the 1st day of HHC service was defined as the index date for the HHC subjects. The non-HHC group was defined as those having the following NHI therapeutic codes: tracheostomy care (56004C), insertion or change of the nasogastric tube (47017C), urinal indwelling catheterization (47014C), urinary catheter change (50022C), and stage 3 or 4 pressure sore care (48001C, 48002C, 48003C, 48004C, 48005C) at least 2 times within 1 year (n = 15,814) at outpatient clinics. The date of the 1st day of tube or catheter care or pressure sore care was defined as the index date for the non-HHC subjects.
2.3. Assembly of study cohort: propensity score matching
To minimize bias and impacts of confounding factors, such as the disease severity of the patients, we matched patients based on their probability or propensity to receive HHC services. The propensity score (PS) is the conditional probability of receiving the HHC services given some measurable covariates.[19] Based on the comorbid status identified by the NHIRD record 1 year before the index date, we used a nonparsimonious multivariable logistic regression model to calculate the PS. The 1:1 PS method[20] was then performed by matching age, gender, index date, and comorbidities listed in the Charlson comorbidity index (CCI),[21] such as myocardial infarction, congestive heart failure, peripheral vascular disease, dementia, cerebrovascular disease, connective tissue disease, liver disease, hemiplegia, chronic renal disease, cancer, etc. After the matching procedures were complete, the numbers of subjects in HHC group (n = 2901) and non-HHC group (n = 2901) were equal. The flow chart of the study is demonstrated in Figure 1.
Figure 1.
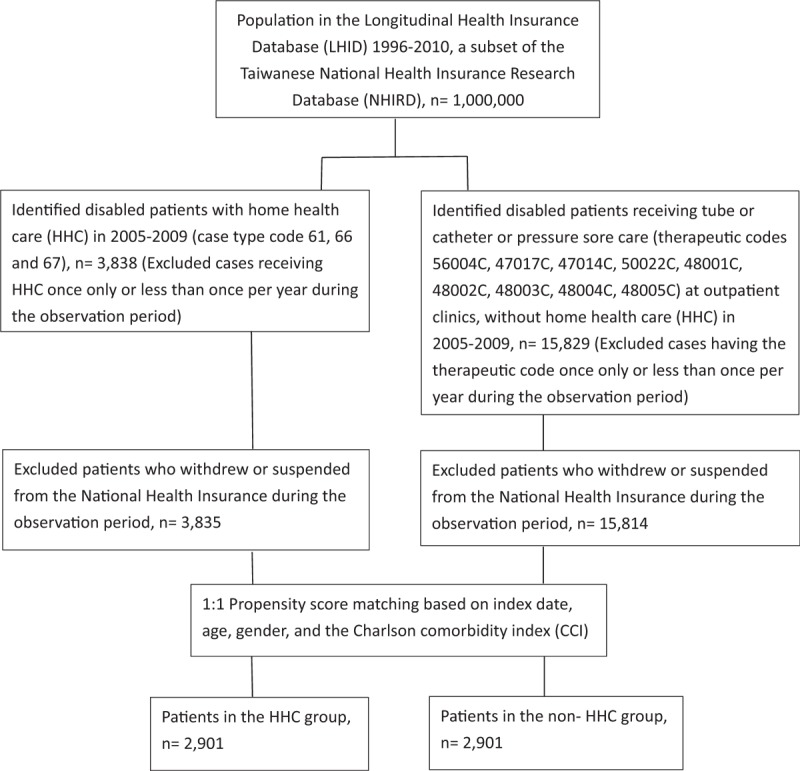
The study flow chart. The case type codes in outpatient claims were as follows: 61 (home health care [HHC] for patients living at home), 66 (HHC for patients living in nursing homes), 67 (HHC for patients living in long-term care facilities). The therapeutic codes were as follows: tracheostomy care (56004C), insertion or change of the nasogastric tube (47017C), urinal indwelling catheterization (47014C), urinary catheter change (50022C), and stage 3 or 4 pressure sore care (48001C, 48002C, 48003C, 48004C, 48005C). Index date: the date of the 1st day of HHC service was defined as the index date for the HHC subjects; the date of the 1st day of tube or catheter or pressure sore care was defined as the index date for the non-HHC subjects.
2.4. Outcomes
The health outcomes for HHC services were evaluated by the rate of hospitalization and the emergency services use 1 year before and after the index date. The healthcare expenditure (US dollars per person per day) was also calculated.
2.5. Statistical analysis
The subject data were presented by frequency, with percentages for categorical variables and the means with standard deviation for continuous variables. T tests and Chi-squared tests are used to describe the differences between the HHC and non-HHC groups for categorical variables and continuous variables, respectively. Generalized estimating equations (GEEs), assumed with a negative binomial distribution, were used to assess the adjusted odds ratio (OR) and 95% confidence interval (CI) for the risk of health outcomes. GEEs with a log-link and gamma distribution were used for the comparison of the healthcare expenditure before and after the index date in each group and the comparison of the healthcare expenditure between the HHC and non-HHC groups. All P-values were 2-sided, with the P-value <.05 was considered as a significance level. All analyses were conducted using the SAS version 9.3 (SAS Institute Inc, Cary, NC).
3. Results
3.1. Subjects characteristics
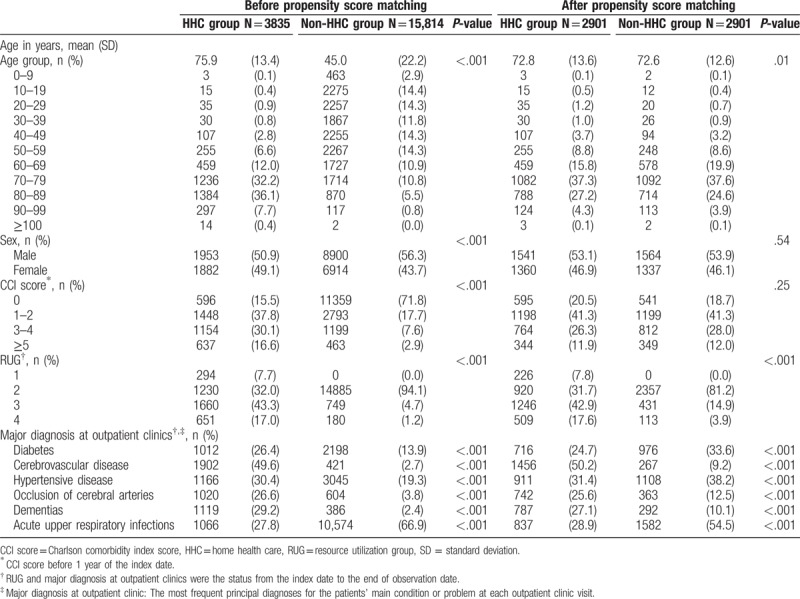
Table 1 summarizes the characteristics of the HHC and non-HHC groups before and after matching. A total of 5802 patients after matching were enrolled in the study, with 2901 subjects in each group. After matching, the HHC group had a mean age of 72.8 years and the non-HHC group had a mean age of 72.6 years (P = .01). There was no significant difference between patients of the HHC and non-HHC groups in gender and CCI. However, the patients in the HHC group were more likely to belong to the higher RUGs (P < .001) than those in the non-HHC group were.
Table 1.
Subjects characteristics of disabled patients in the HHC group and non-HHC group before and after matching.
3.2. Health outcomes in relation to HHC
The comparison of health outcomes of disabled patients with and without HHC services is shown in Table 2. Patients in the HHC group had lower risk of hospital admissions (OR = 0.2, 95% CI: 0.17–0.23, P < .001) and emergency services use (OR = 0.45, 95% CI: 0.41–0.50, P < .001) after 1 year of HHC, compared to the condition 1 year before they received HHC. In contrast, in the non-HHC group, the risk for being hospitalized (OR = 1.12, 95% CI: 1.02–1.23, P < .05) slightly increased 1 year after the index date, compared to the condition 1 year before they received tube or catheter or pressure sore care at outpatient clinics.
Table 2.
Comparison of health outcomes of disabled patients in the HHC group and non-HHC group before and after the index date.
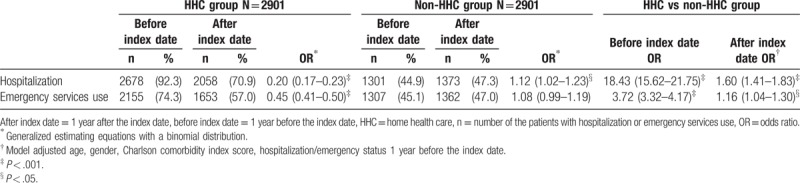
Compared to those in the non-HHC group, the patients in the HHC group had significantly higher risk for hospitalization (OR = 18.43, 95% CI: 15.62–21.75, P < .001) and emergency services use (OR = 3.72, 95% CI: 3.32–4.17, P < .001) 1 year before the index date. However, 1 year after the index date, the risk for hospitalization (OR = 1.6, 95% CI: 1.41–1.83, P < .001) and emergency services use (OR = 1.16, 95% CI: 1.04–1.30, P < .05) attenuated significantly.
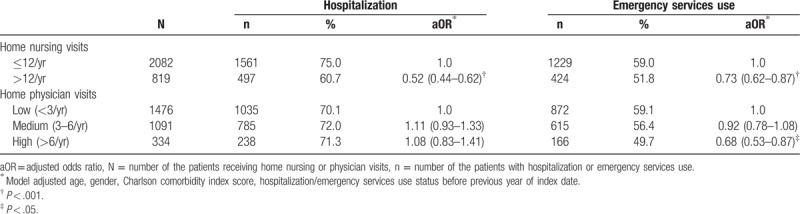
3.3. Health outcomes in relation to numbers of nursing visits and physician visits
In Table 3, for the patients with HHC receiving home nursing visits more than 12 times per year, the risk for hospitalization (OR = 0.52, 95% CI: 0.44–0.62, P < .001) and emergency services use (OR = 0.73, 95% CI: 0.62–0.87, P < .001) was lower than the risk of those receiving home nursing visits ≤12 times per year. When physician visits increased to more than 6 times per year, the risk for emergency services use was less than the risk of those receiving the home physician service <3 times per year. (OR = 0.68, 95% CI: 0.53–0.87, P < .05).
Table 3.
Comparison of health outcomes of disabled patients in relation to the frequency of home nursing visits and physician visits in the HHC group.
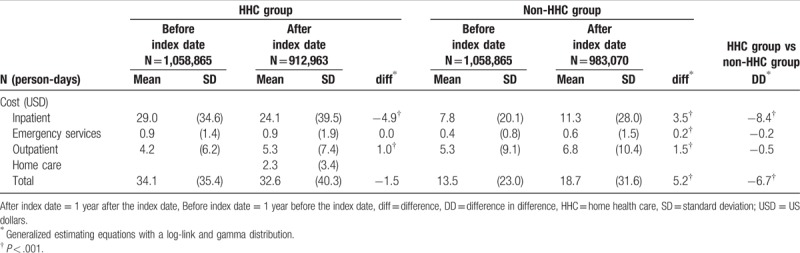
3.4. Healthcare expenditure
The comparison of the healthcare expenditure of disabled patients with and without HHC is demonstrated in Table 4. In the HHC group, the total healthcare expenditure decreased insignificantly by US$1.5 per person per day after 1-year HHC. The inpatient care cost decreased significantly by US$4.9 per person per day (P < .001), whereas the outpatient care cost increased significantly by US$1 per person per day (P < .001). In the non-HHC group, the total healthcare expenditure increased significantly by US$5.2 per person per day (P < .001). The expenditures of the inpatient care, emergency services use, and outpatient care were significantly increased by US$3.5, US$0.2, and US$1.5 per person per day (P < .001), respectively. Compared to the non-HHC group, the HHC services led to a US$6.7 per person per day decrease in the total healthcare expenditure (P < .001).
Table 4.
Comparison of the healthcare expenditure (US dollars per person per day) of disabled patients in the HHC and non-HHC groups before and after the index date.
4. Discussion and conclusion
In this study, we demonstrated that patients in the HHC group had lower risk of hospital admissions and emergency services use significantly after 1 year of HHC compared to the condition 1 year before they received HHC. Furthermore, in the HHC group, the inpatient care cost decreased significantly by US$4.9 per person per day. In the non-HHC group, the total healthcare expenditure increased significantly by US$5.2 per person per day. The expenditures of the inpatient care, emergency services and outpatient care were significantly increased by US$3.5, US$0.2, and US$1.5 per person per day, respectively. There was a US$6.7 per person per day decrease in the total healthcare expenditure of the HHC group compared to those of the non-HHC group. Our study suggested that HHC had the potential to reduce hospitalization and emergency services use. Besides, the improvement of healthcare quality through HHC was not linked to increased healthcare expenditure.
Although the patients in the HHC group were in higher RUGs (Table 1) and might be more dependent in activities of daily living, HHC was associated with a significant reduction in the risk of hospitalization and emergency services use in our study (Table 2). Similarly in the US studies, HHC could improve access to medical care and reduce hospital admissions and the healthcare expenditure.[10,11] Furthermore, a Barcelona HHC program for individuals with multimorbidities revealed a decrease of number of hospital admissions and length of stay with lower cost.[2] However, the reduction of the healthcare expenditure in our study was smaller compared with those in the US study (approximately US$42 per person per day)[11] and in the Barcelona study (approximately US$49 per person per day).[2] The reason for this difference might be because the average medical care payment in Taiwan was much lower than the payment in high-income countries. The total expenditures on health of gross domestic product were 17.1%, 9%, and 6.3% in the United States, Spain, and Taiwan, respectively.[22,23] Meanwhile, the total health expenditures per capita, purchasing power party adjusted were US$9832.3, US$3256.7, and US$2897 in the United States, Spain, and Taiwan, respectively.[22,23] Besides, the HHC program in Taiwan during the study period did not allow the home visiting physicians to prescribe medication or order tests, which may result in increased outpatient care cost due to possible outpatient clinic referrals after home visits. Further studies were necessary to clarify the possible causes.
The HHC services have the potential to improve health outcomes and reduce functional decline when based on timely multidimensional clinical assessment. However, the effects of HHC may be inconsistent and depend on the heterogeneities of programs.[24] Our study showed that higher intensity of nursing visit (more than 12 times/year) was associated with a significant reduction in the risk of hospitalization and emergency services use; while higher intensity of physician visit (more than 6 times/year) was associated with less emergency services use. In comparison to previous studies in the United States[25,26] and in Japan,[27] where the HHC programs provided nursing visits 1 to 8 times per week, the HHC program in Taiwan maximally provided nursing visits twice per month. Further studies are warranted to investigate the appropriate intensity of home care visits by different disciplines to provide cost-effective services.
There are some limitations in this study. First, although we performed PS matching to minimize the impact of measured covariates, our findings cannot demonstrate unobserved confounding factors, such as the functional status of the patients. As our study used a matched controlled cohort rather than a randomized controlled trial, the estimated ORs addressed only the correlation, not the causal relationship. However, we did demonstrate that HHC program, especially home nursing visits, was associated with risk reduction of hospitalization and emergency services use even on patients with poor functional status. Another limitation was the fact that NHIRD was an administrative database which measurement bias could happen due to the possible inaccuracy of information input. To mitigate this, we excluded some subjects whose information were against ordinary clinical practices, such as subjects receiving only annual home visit, but tube, catheter, or pressure sore cared at outpatient clinics. Furthermore, while we calculated payment reimbursed by the NHI, any expenditure incurred outside of the NHI was not available. According to the NHI policy, the frequency of physician and nursing visit reimbursed by the NHI was prescribed by the physician who assesses the patient with HHC regularly. However, when patients or families asked for more physician or nursing visits by out-of-pocket payment, the number of visits and costs could not be captured by NHIRD. Therefore, there was a possibility that the number of HHC visits and expenditure would be underestimated in this study. Nonetheless, the home health care expense only accounted for <1.7% of out-of-pocket payments in Taiwan, which would make the bias toward null.[23] Despite the limitations, the cohort was longitudinal and nationally representative. Moreover, there were very few studies investigating whether the HHC program, with mainly regular nursing and physician visits, was effective to improve health outcomes or not. To our knowledge, this is also the 1st study to demonstrate the HHC program may be cost-effective for disabled patients in the Chinese population.
In this population-based retrospective cohort study, we showed significant clinical benefits associated with HHC services for disabled patients. There was a potential for HHC with regular nursing and physician visits to reduce hospitalization and emergency services use. Besides, the improvement of healthcare quality through HHC was not accompanied by increased healthcare expenditure, suggesting a promising role for public health officials to promote HHC services for disabled patients.
Author contributions
Conceptualization: Yi-Hsuan Lee.
Data curation: Yi-Hsuan Lee, Chia-Wen Lu, Chi-Ting Huang, Hao-Hsiang Chang, Kuen-Cheh Yang, Chia-Sheng Kuo, Yu-Kang Chang, Chih-Cheng Hsu, Kuo-Chin Huang.
Formal analysis: Yi-Hsuan Lee, Chia-Wen Lu, Chi-Ting Huang, Hao-Hsiang Chang, Kuen-Cheh Yang, Chia-Sheng Kuo, Yu-Kang Chang, Chih-Cheng Hsu, Kuo-Chin Huang.
Investigation: Yi-Hsuan Lee, Chia-Wen Lu, Chi-Ting Huang, Hao-Hsiang Chang, Kuen-Cheh Yang, Chia-Sheng Kuo, Yu-Kang Chang, Chih-Cheng Hsu, Kuo-Chin Huang.
Methodology: Yi-Hsuan Lee, Chia-Wen Lu, Chi-Ting Huang, Hao-Hsiang Chang, Kuen-Cheh Yang, Chia-Sheng Kuo, Yu-Kang Chang, Chih-Cheng Hsu, Kuo-Chin Huang.
Project administration: Yi-Hsuan Lee.
Software: Chi-Ting Huang, Yu-Kang Chang.
Supervision: Chih-Cheng Hsu, Kuo-Chin Huang.
Validation: Yi-Hsuan Lee, Chia-Wen Lu, Chi-Ting Huang, Hao-Hsiang Chang, Kuen-Cheh Yang, Chia-Sheng Kuo, Yu-Kang Chang, Chih-Cheng Hsu, Kuo-Chin Huang.
Writing – original draft: Yi-Hsuan Lee.
Writing – review & editing: Yi-Hsuan Lee, Chia-Wen Lu, Chi-Ting Huang, Hao-Hsiang Chang, Kuen-Cheh Yang, Chia-Sheng Kuo, Yu-Kang Chang, Chih-Cheng Hsu, Kuo-Chin Huang.
Kuo-Chin Huang orcid: 0000-0002-6029-5520.
Footnotes
Abbreviations: CCI = Charlson comorbidity index, GEEs = generalized estimating equations, HHC = home health care, NHI = National Health Insurance, NHIRD = National Health Insurance Research Database, RUGs = resource utilization groups.
C-CH and K-CH contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Ageing, 2017. Available at: http://www.un.org/en/sections/issues-depth/ageing/ Accessed July 27, 2018. [Google Scholar]
- [2].Vila A, Villegas E, Cruanyes J, et al. Cost-effectiveness of a Barcelona home care program for individuals with multimorbidity. J Am Geriatr Soc 2015;63:1017–24. [DOI] [PubMed] [Google Scholar]
- [3].American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. Patient-centered care for older adults with multiple chronic conditions: a stepwise approach from the American Geriatrics Society: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc 2012;60:1957–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Pefoyo AJ, Bronskill SE, Gruneir A, et al. The increasing burden and complexity of multimorbidity. BMC Public Health 2015;15:415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Disability and Health, 2018. Available at: http://www.who.int/news-room/fact-sheets/detail/disability-and-health Accessed July 27, 2018. [Google Scholar]
- [6].Jackson GL, Powers BJ, Chatterjee R, et al. Improving patient care. The patient centered medical home. A systematic review. Ann Intern Med 2013;158:169–78. [DOI] [PubMed] [Google Scholar]
- [7].Tappenden P, Campbell F, Rawdin A, et al. The clinical effectiveness and cost-effectiveness of home-based, nurse-led health promotion for older people: a systematic review. Health Technol Assess 2012;16:1–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Latour CH, Bosmans JE, van Tulder MW, et al. Cost-effectiveness of a nurse-led case management intervention in general medical outpatients compared with usual care: an economic evaluation alongside a randomized controlled trial. J Psychosom Res 2007;62:363–70. [DOI] [PubMed] [Google Scholar]
- [9].Naomi A, Shiroiwa T, Fukuda T, et al. Institutional care versus home care for the elderly in a rural area: cost comparison in rural Japan. Rural Remote Health 2012;12:1817. [PubMed] [Google Scholar]
- [10].Edes T, Kinosian B, Vuckovic NH, et al. Better access, quality, and cost for clinically complex veterans with home-based primary care. J Am Geriatr Soc 2014;62:1954–61. [DOI] [PubMed] [Google Scholar]
- [11].Xiao R, Miller JA, Zafirau WJ, et al. Impact of home health care on health care resource utilization following hospital discharge: a cohort study. Am J Med 2018;131:395–407. [DOI] [PubMed] [Google Scholar]
- [12].Han SJ, Kim HK, Storfjell J, et al. Clinical outcomes and quality of life of home health care patients. Asian Nurs Res (Korean Soc Nurs Sci) 2013;7:53–60. [DOI] [PubMed] [Google Scholar]
- [13].Shepperd S, Iliffe S, Doll HA, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev 2016;9:CD007491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ticona L, Schulman KA. Extreme home makeover - the role of intensive home health care. N Engl J Med 2016;375:1707–9. [DOI] [PubMed] [Google Scholar]
- [15].Baernholdt M, Yan G, Hinton I, et al. Quality of life in rural and urban adults 65 years and older: findings from the National Health and Nutrition Examination survey. J Rural Health 2012;28:339–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hart LG, Salsberg E, Phillips DM, et al. Rural health care providers in the United States. J Rural Health 2002;18Suppl:211–32. [DOI] [PubMed] [Google Scholar]
- [17].Chang HT, Lai HY, Hwang IH, et al. Home healthcare services in Taiwan: a nationwide study among the older population. BMC Health Serv Res 2010;10:274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].2017 Taiwan Health and Welfare Report, 2018. Available at: https://www.mohw.gov.tw/cp-137-40301-2.html Accessed October 24, 2018. [Google Scholar]
- [19].Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998;17:2265–81. [DOI] [PubMed] [Google Scholar]
- [21].Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613–9. [DOI] [PubMed] [Google Scholar]
- [22].Health Expenditure and Financing, 2016. https://stats.oecd.org/Index.aspx?DataSetCode=SHA# Accessed October 13, 2018. [Google Scholar]
- [23].National Health Expenditure, 2016. Available at: https://www.mohw.gov.tw/dl-43399-3b046b4b-2b21-4cff-8166-e872c5152dae.html Accessed October 13, 2018. [Google Scholar]
- [24].Huss A, Stuck AE, Rubenstein LZ, et al. Multidimensional preventive home visit programs for community-dwelling older adults: a systematic review and meta-analysis of randomized controlled trials. J Gerontol A Biol Sci Med Sci 2008;63:298–307. [DOI] [PubMed] [Google Scholar]
- [25].O’Connor M, Bowles KH, Feldman PH, et al. Frontloading and intensity of skilled home health visits: a state of the science. Home Health Care Serv Q 2014;33:159–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Riggs JS, Madigan EA, Fortinsky RH. Home health care nursing visit intensity and heart failure patient outcomes. Home Health Care Manag Pract 2011;23:412–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Murashima S, Nagata S, Magilvy JK, et al. Home care nursing in Japan: a challenge for providing good care at home. Public Health Nurs 2002;19:94–103. [DOI] [PubMed] [Google Scholar]


