Supplemental Digital Content is available in the text
Keywords: gout, lumbar retrolisthesis, spondylodiscitis, spondylolisthesis, urate crystals
Abstract
Rationale:
Gout occurs mainly in joints, but rarely in the spine. In the spine, urate crystals can cause intervertebral space instability but rarely lead to retrolisthesis. Here, we present an extremely rare disease with gout invaded the intervertebral disc with lumbar retrolisthesis.
Patient concerns:
A 61-years male patient with gout history has suffered from severe low back pain and intermittent claudication. Physical examination showed the level of muscle strength of his left first toe was 3/5. Images illustrated a destruction of the intervertebral space, and a retrolisthesis at L4/5 interspace and the dural sac obviously compressed.
Diagnoses:
Combining with lab examinations, imaging examinations, and histopathological results, the patient was diagnosed with gouty arthritis associated with lumbar spinal stenosis, L4–5 spondylodiscitis and L4 vertebral body retrolisthesis.
Intervention:
The patient underwent posterior decompression, reduction, and interbody fusion, and then received an aggressive postoperative rehabilitation program.
Outcomes:
The patient's low back pain was significantly alleviated after the operation. Postoperative X-ray shows the internal fixation was well placed and the sequence of spine was reconstructed. 12 weeks later, the lower limb symptoms of the patients were obviously improved, his muscle strength of the left first toe was 4/5, Japanese Orthopaedic Association (JOA) score was 19 and the improvement rate was 61.5%.
Lessons:
Gouty spondylodiscitis can cause intervertebral space instability. Sagittal imbalance and degeneration of disc with decreasing of segmental disc height are considered as the main factors of retrolisthesis. The appearance may lead to misdiagnose a patient with gout history with a destruction of the intervertebral space. Surgery is a compromise method for gouty spondylodiscitis patients with urgent neurological symptoms.
1. Introduction
Gout is a metabolic disordered and recurrent inflammatory disease; it results from the deposition of monosodium urate crystals (MSU) in tissues and is characterized by the formation of uric acid crystals as a major clinical feature. Gout is common in North America and Western European countries; the annual incidence of gout is 2.68 per 1000 persons. Gout occurs mainly in joints such as ankle and wrist, but rarely in the spine. In the spine, urate crystals occur commonly in extradural space, followed by facet joints and vertebral bodies, but rarely in discs.[1] Retrolisthesis is defined as a backward slippage of 1 vertebra on another,[2] different from anterolisthesis, retrolisthesis is unusual and the biomechanical mechanism is barely known. As the first reported case, in this article, we will discuss a patient with gout invaded the intervertebral disc with lumbar retrolisthesis.
2. Case report
A 61-year-old male was admitted to our department, suffering from low back pain for 2 months, aggravated with intermittent claudication in the last 7 days. Twenty-two years ago, the patient discovered his left ankle joint and the first metatarsophalangeal joint began to be redness and swelling (Fig. S1), then was diagnosed as “gout” and was treated with partial closure, later the condition improved. Two months before this visit, the patient appeared symptom of low back pain, which was aggravated during position transformation. During the last 7 days, intermittent claudication occurred and the symptoms were significant at the left side of lower limbs. Examination showed his muscle strength of 3/5 in the first toe on the left. The Japanese Orthopaedic Association (JOA) score was 3.
Lab examination revealed urate level of 678.40 μmol/L (reference range 180–410), C-reactive protein (CRP) of 25.28 mg/L (reference range 0–4.0), creatinine of 132.60 μmol/L (reference range 53–140). X-ray illustrated interspace between L4–5 was narrowed and obviously unstable, and showed a retrolisthesis at L4 and kyphosis in thoraco-lumbar spine. CT showed subchondral bones of L4 lower endplate and L5 upper endplate appeared as punched-out liked bone destruction with peripheral calcification, irregular erosion was found in vertebral body and lower endplate of L4, swelled articular soft tissue, and punctuate high density in bilateral yellow ligament (Fig. 1). Magnetic resonance imaging (MRI) demonstrated the offending process at L4–5 interspace and the dural sac obviously compressed. Fat-suppressed T2-weighted image (ST2WI) showed the lesion area with high signal (Fig. 2).
Figure 1.
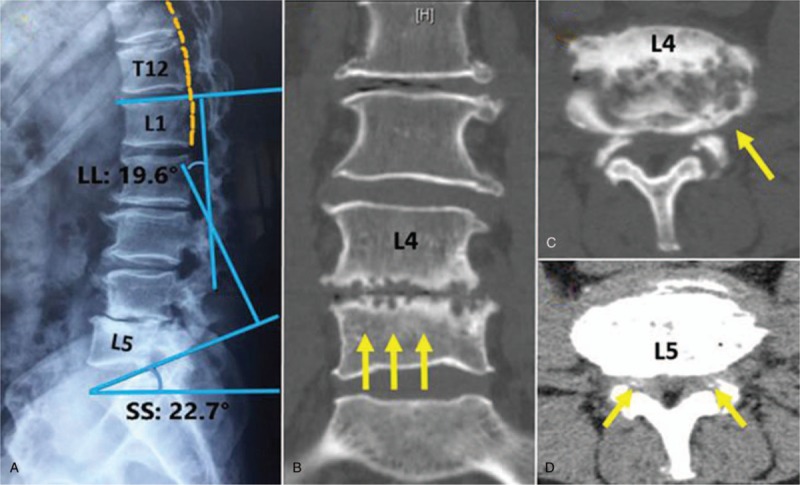
(A) X-ray shows the narrowed interspace between L4-5, retrolisthesis at L4, and kyphosis in thoraco-lumbar spine. (B) Sagittal CT illustrates subchondral bones of L4 lower endplate and L5 upper endplate appearing as punched-out liked bone destruction with peripheral calcification. (C–D) Phase axial CT shows irregular erosion in vertebral body and lower endplate of L4, swelled articular soft tissue, and punctuate high density in bilateral yellow ligament. CT = computed tomography.
Figure 2.
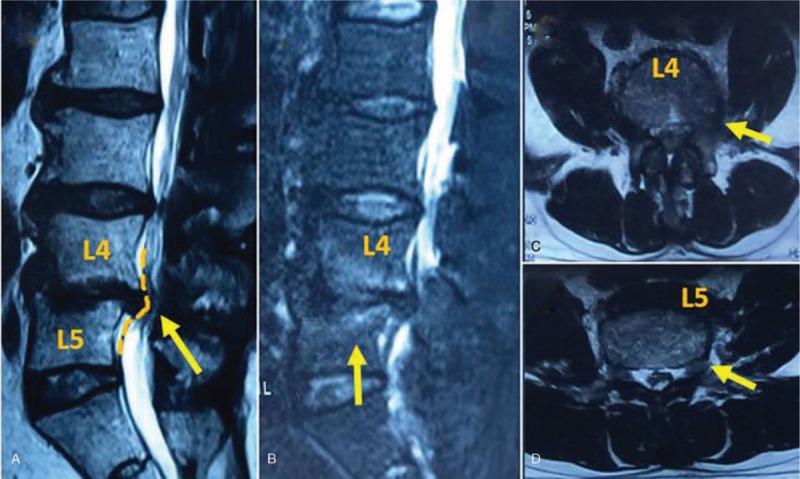
(A) MRI demonstrates the dural sac is compressed obviously. (B) Fat-suppressed T2-weighted image shows the lesion area surrounded by high signal. (C–D) Phase axial MRI illustrates the structural changes and inflammatory responses at L4-5 intervertebral disc. MRI = magnetic resonance imaging.
Based on the above examinations, the patient was diagnosed with gouty arthritis associated with lumbar spinal stenosis, L4–5 spondylodiscitis and L4 vertebral body retrolisthesis. He underwent posterior decompression, reduction, and interbody fusion. White sand-like substance was found in L4–5 intervertebral disc tissue removed during the surgery (Fig. S2). The histopathological examination showed fibroblasts, inflammatory granuloma composed of lymphocytes, and foreign body giant cells were rounded with a few urate crystals, suggesting of tophaceous gout (Fig. 3).
Figure 3.
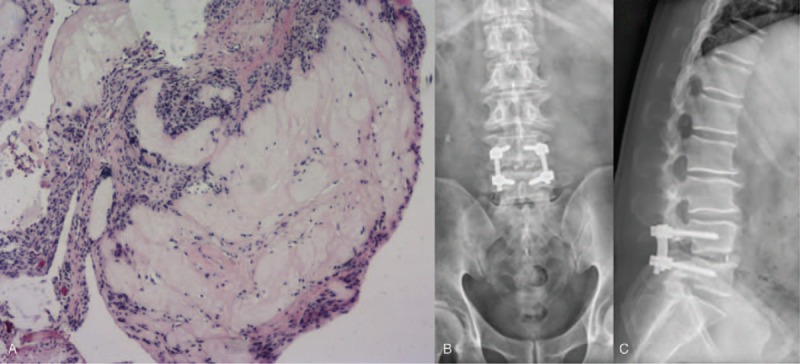
(A) Intraoperative pathology (L4-5 disc): fibroblasts, inflammatory granuloma composed of lymphocytes, and foreign body giant cells are surrounded by a few urate crystals, which suggesting tophaceous gout ((hematoxylin-eosin, × 100). (B–C) Postoperative X-ray shows the location of the internal fixation and interbody fusion cage is satisfied and the sequence of spine is well reconstructed.
The patient's low back pain was significantly alleviated after the operation. Image showed the internal fixation was well placed and the sequence of spine was reconstructed. Postoperative administration of 10 mg dexamethasone, 250 mL mannitol, and allopurinol 300 mg/day with non-steroidal anti-inflammatory drugs (NSAIDs) were given to him. 12 weeks later, the lower limb symptoms were obviously relieved, his muscle strength of the first toe on the left was 4/5, the score of JOA was 19 and the improvement rate was 61.5%.
3. Discussion
Gout is a kind of heterogeneous diseases result from the increasing of uric acid and the deposition of uric acid salt in various tissues, including joints, tendons, ligaments, kidneys, subcutaneous, and other tissues; however, rarely in the spine, especially the disc.[1,3] According to Toprover's study, among 104 patients with spinal gout, the tophus involved in the cervical spine in 32 (24.8%) cases; the thoracic spine was affected in 23 (17.8%) cases; the lumbar spine was involved in 49 (38.0%) cases;[3] but the incidence of gout invading the intervertebral disc has not been reported.
Studies demonstrated that spinal gout is common in human in range from age 35 to 75 years. The diseases can even cause incomplete paralysis (39.0%) radiculopathy (27.0%) and low back pain (18.0%).[4,5] A recent study showed that dual-energy CT (DECT) has been recognized as a newer method of imaging gout, and DECT can easily identify tophi from other types of masses.[6] Hu et al[7] found the sensitivity and specificity of DECT at 91.9% and 85.4% when identify gouty tophi. For the treatment of gout, first, education, diet and life style changes are keys to asymptomatic period patients. Second, for acute phase patients, it is aiming at symptoms conservatively control, such as colchicine, NSAIDs, and glucocorticoid. Thirdly, during intermittent and chronic periods, to develop the etiology of the disease and to prevent acute gout attacks are indispensable, the medication suggestion in this phase including allopurinol, febuxostat, and IL-1 blockers. In addition, surgery is another suitable method for patients who are ineffective with conservative treatment and suffering from the urgent neurological symptoms, especially for the spinal compression.[3,8]
In our case, the patient was attacked with typical gout, whose lab examination indicated the gout nodules in subcutaneous tissues, therefore the primary diagnose of peripheral joint gout was obvious. Moreover, according to CT examination, the endplate appeared as punched-out liked bone destruction with peripheral calcification; combining with positive the lab examination (CRP, creatinine, and urate) and the histological result, this patient was further diagnosed with gouty spondylodiscitis (L4–5). King et al[4] believed that when urate crystals are deposited around the facet joints, can cause edema; hyperemia; inflammatory reaction which can lead to necrosis around tissues; the destruction of ligaments, joints, and cartilage; acceleration of intervertebral degeneration; and resulting in segmental instability. King and Chang[4,9] supposed that cells around the disc are sensitive to extracellular PH and oxygen content, under the condition of acidic environment and hypoxia, nutrition and water content of the disc will rapidly lose, then causing or accelerating the disc degeneration, meanwhile urate crystals and uratoma are formed. In addition, proper medicine treatment is also indispensable, to prevent from kidney damage and acute kidney failure.
Retrolisthesis is defined as a backward slippage of 1 vertebra on another of more than 3 mm.[2] Different from anterolisthesis, biomechanical mechanism is barely known about the formation of retrolisthesis. Shen et al[10] supposed that retrolisthesis appears to be associated with: lumbar lordosis (LL) decrease; reduced endplate inclination; degeneration of disc; and missing of segmental disc height. More recent biomechanical researches show the association between retrolisthesis and sagittal imbalance, for example, lower pelvic incidence (PI), sacral slope (SS), LL, and thoracic lumbar kyphosis (TLK)[11]. Roussouly et al[12] believed that “patients with anterior sagittal imbalance and low PI limited the posterior excursion of the sacrum relative to the femoral heads as well as the increase of PT”, resulting in an inadequate compensatory capacity of pelvic retroversion. Therefore, retrolisthesis may plays the role of supplement for restricted pelvic retroversion and be suggested as a compensatory mechanism for sagittal imbalance. Mehta et al[13]confessed that the degenerative changes at disc and a low slip angle are leading to a compensatory retrolisthesis. While the “low slip angle” is defined as angle between the upper endplate of S1 vertebral body and the inferior endplate of L5 vertebral body.
In our case, the measurement results illustrate the patient's SS angle is 22.7° and LL angle is 19.6°, combined with Qiu's research,[14,15] the mean values of spinopelvic parameters in China is 32.5 ± 6.5° for SS and 43.2 ± 6.5° for LL (male). Besides, the X-ray image shows the patient's PI angle is small and TLK angle is significantly larger. So, we can be fairly confident of these results to be support of the above views.
4. Conclusion
Commonly, urate crystals occur mainly in peripheral joints, ligaments and subcutaneous, rarely in spine, especially the disc. Gouty spondylodiscitis leads to structural changes of intervertebral disc, structure destroys of joints and bones around the lesion, which eventually lead to the instability of the intervertebral space. Lower PI, SS, and LL, larger TLK, and degeneration of disc with decreasing of segmental disc height should be considered as main risk factors for retrolisthesis. When meet with a patient with a history of gout develops retrolisthesis, and destruction of the intervertebral space in CT image, we should alert to gouty spondylodiscitis. Surgery and anti-gout medication are the effective methods for the patient suffering from urgent neurological symptoms.
Author contributions
Investigation: Yunlong Zou, Ye Li.
Writing – original draft: Yunlong Zou.
Writing – review & editing: Jingchen Liu, Rui Gu, Boyin Zhang.
Supplementary Material
Footnotes
Abbreviations: CRP = C-reactive protein, DECT = dual-energy CT, JOA = Japanese Orthopaedic Association, LL = lumbar lordosis, NSAIDs = non-steroidal anti-inflammatory drugs, PI = pelvic incidence, SS = sacral slope, TLK = thoracic lumbar kyphosis.
Written informed consent was obtained from the guardian of the patient for publication of this case report and any accompanying images.
Bethune Project of Jilin University, 2015312; National Natural Science Foundation of China (NSFC), 81701225.
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article.
References
- [1].Mello FM, Helito PV, Bordalorodrigues M, et al. Axial gout is frequently associated with the presence of current tophi, although not with spinal symptoms. Spine 2014;39:E1531–1536. [DOI] [PubMed] [Google Scholar]
- [2].Vogt MT, Rubin DA, Palermo L, et al. Lumbar spine listhesis in older African American women. Spine J 2003;3:255–61. [DOI] [PubMed] [Google Scholar]
- [3].Toprover M, Krasnokutsky S, Pillinger MH. Gout in the spine: imaging, diagnosis, and outcomes. Curr Rheumatol Rep 2015;17:1–9. [DOI] [PubMed] [Google Scholar]
- [4].King JCJ, Nicholas C. Gouty arthropathy of the lumbar spine: a case report and review of the literature. Spine (Phila Pa 1976) 1997;22:2309–12. [DOI] [PubMed] [Google Scholar]
- [5].Hasturk AE, Basmaci M, Canbay S, et al. Spinal gout tophus: a very rare cause of radiculopathy. Eur Spine J 2012;21suppl4:S400–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Nicolaou S, Liang T, Murphy DT, et al. Dual-energy CT: a promising new technique for assessment of the musculoskeletal system. AJR Am J Roentgenol 2012;199:S78–86. [DOI] [PubMed] [Google Scholar]
- [7].Hu HJ, Liao MY, Xu LY. Clinical utility of dual-energy CT for gout diagnosis. Clin Imaging 2015;39:880–5. [DOI] [PubMed] [Google Scholar]
- [8].Ragab G, Elshahaly M, Bardin T. Gout: an old disease in new perspective—a review. J Adv Res 2017;8:495–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Chang IC. Surgical versus pharmacologic treatment of intraspinal gout. Clin Orthop Relat Res 2005;433:106–10. [DOI] [PubMed] [Google Scholar]
- [10].Michael Shen, Afshin Razi, Jon D, et al. Retrolisthesis and lumbar disc herniation: a postoperative assessment of patient function. Spine J 2007;13:406–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Zhu F, Bao H, Liu Z, et al. Lumbar retrolisthesis in aging spine: what are the associated factors. Clin Spine Surg 2017;30:E677–82. [DOI] [PubMed] [Google Scholar]
- [12].Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 2011;20:609–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mehta JS, Kochhar S, Harding IJ. A slip above a slip: retrolisthesis of the motion segment above a spondylolytic spondylolisthesis. Eur Spine J 2012;21:2128–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zhu Z, Xu L, Zhu F, et al. Sagittal alignment of spine and pelvis in asymptomatic adults: norms in Chinese populations. Spine 2014;39:1–6. [DOI] [PubMed] [Google Scholar]
- [15].Yong Q, Zhen L, Zezhang Z, et al. Comparison of sagittal spinopelvic alignment in Chinese adolescents with and without idiopathic thoracic scoliosis. Spine (Phila Pa1976) 2012;37:E714–720. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


