Abstract
Post-traumatic growth in cancer patients refers to perceived positive changes following cancer diagnosis and treatment. Little is known about the status and factors related to posttraumatic growth among Chinese patients with lung cancer.
To investigate the status and factors of posttraumatic growth among Chinese patients with lung cancer.
A cross-sectional design was adopted in this study. Patients (N = 173) from the oncology unit at one teaching hospital in Sichuan were recruited. Posttraumatic growth, depression, anxiety, and coping style were self-reported by the patients. Multiple linear regression analysis was to examine factors related to posttraumatic growth.
Posttraumatic growth was a common exit in Chinese lung cancer patients. Time since cancer diagnosis, patient depression, and coping strategies are factors that affect the experience of posttraumatic growth.
Reducing depression, providing available support, and improving active coping strategies are areas to facilitate posttraumatic growth.
Keywords: Factors, lung cancer, patients, posttraumatic growth
1. Introduction
Lung cancer is a leading cancer diagnosis and leading cause of cancer-related death in China, with 605,946 new diagnoses and 486,555 identified deaths in 2010.[1] The mean cost per patient with lung cancer in China was more than $9891.[2] With the increasing ageing population, the cost of care for lung cancer has become heavier[3]; therefore, lung cancer became an important public health and social issue in China.
Patients who struggle with cancer can suffer negative consequences; however, they also report positive aspects of psychological adjustment, such as resilience and fulfilment, following their experience.[4,5] Studies on the positive changes among cancer survivors have increased in recent years. A lot of terms were used to describe the positive changes, such as posttraumatic growth, stress-related growth, and benefit findings. The “posttraumatic growth” (PTG) refers to positive psychological changes in personal growth and relationships due to the fight with traumatic experiences.[6,7] PTG is commonly found among cancer patients, with a percentage of 60% to 95%.[4] Many cancer survivors perceive personal benefits through their cancer experience, including strengthened life understanding, better relationship, and increased positive self-perception.[8]
PTG is linked to the psychological well-being of patients; therefore, investigating the factors associated with PTG is extremely important. The general factors that affect PTG are demographic characteristics (e.g., social and economic status, age, and gender), clinical characteristics (e.g., severity of disease, time following initial diagnosis, and treatments), personality (e.g., optimism and positivity), environmental aspects (e.g., support network and coping responses), and psychological characteristics (e.g., greater positive affect and less depression).[4,9] Coping efforts are essential for managing an adverse experience, which may create opportunities for personal growth by prompting revision and reframing in a positive light.[6,7] Patients who participate in active coping are associated with better health.[6,7] In addition, depression and anxiety are common psychological distress among lung cancer patients. Psychological distress is associated with poor treatment compliance, increased hospital stay, and decreased QOL.[10] Although PTG and psychological distress are both correlated with the well-being of patients, the relationship between psychological distress and PTG is debatable.[8,11–13]
PTG affirms that patients have the potential to recover and grow from traumatic events and provides a new perspective for an effective post-traumatic intervention. A deep investigation of the status and factors associated with PTG is critical to obtain an overall understanding of the psychological status of Chinese lung cancer patients and provide appropriate support for improving their psychological well-being. Despite the benefits reported among cancer patients, most of studies concentrate on the negative consequences and pathology evidence.[14] Even among positive findings on mental health specifically, the available studies are based on patients with other cancers (e.g., breast cancer and prostate cancer)[15–17] or patients with a mixed cancer diagnosis.[18,19] To our knowledge, to date, there are very few studies investigating the benefit findings among Chinese lung cancer patients. Compared to other cancers, lung cancer has a poorer prognosis[20] as well as higher rate of symptom distress,[21] unmet needs,[22] and psychological distress.[23] In addition, as a subjective concept, PTG varies from patient to patient. Thus, it is essential to investigate PTG among lung cancer patients from a Chinese perspective. The objectives of this study were to investigate the status and factors related to PCG among Chinese patients with lung cancer.
2. Measurement
2.1. Design and sample
A cross-sectional design with a convenience sampling method was adopted in this present study. Lung cancer patients were recruited from the inpatient oncology unit at a teaching hospital in Chengdu. Patients with lung cancer were recruited from a teaching hospital in Chengdu, China. The inclusion criteria were for the patients were: (1) a diagnosis of lung cancer, (2) older than 18 years old, (3) Chinese speaking, (4) able to understand the questionnaires, and (5) being informed of the cancer diagnosis. Patients who have a diagnosis of a psychiatric disorder and have severe cognitive impairment (screened by the Callahan Cognitive Screen18) were excluded.[24]
2.2. Data collection
Data collection was performed at the inpatient oncology unit of the teaching hospital prior to discharge, including patient demographic and clinical characteristics, psychological distress (depression and anxiety), PTG, and coping responses. Oncological nurses identified eligible participants in the ward according to their medical records and face-to-face interviews. Data were obtained by the medical records and patient self-reporting. The tools adopted in this study were: (1) a demographic and clinical survey, (2) Posttraumatic Growth Inventory (PTGI), (3) Hospital Anxiety and Depression Scale (HADS), and (4) simplified coping style questionnaire (SCSQ).
2.2.1. Demographic and clinical questionnaire
The demographic and clinical questionnaire included patient sex, age, education, marital status, type of cancer, stage of cancer, time since cancer diagnosis, treatment types, family monthly income, medical and other types of insurance, and employment after cancer diagnosis.
PTG was assessed by the PTGI.[7] The 21-item PTGI uses a 6-point scale ranging from 0 (I didn’t experience the change due to my cancer experience) to 5 (I experienced the change to a very high degree due to my cancer experience). A higher score is indicative of a greater growth. The PTGI has adequate reliability and validity.[7]
Patient psychological distress was assessed by the HADS.[25] The 14-item HADS consists of two subscales, including 7-item anxiety subscale and 7-item depression subscale. The 4-point HADS ranges from 0, “not present,” to 3, “considerable”. A higher score was indicative of a higher level of emotional distress. A score of 8 or above on each subscale was indicative of probable anxiety or depression. This HADS has good reliability and validity.[26] The Chinese version of the HADS has adequate scale quality among Chinese patients.[27]
The patient coping ability was assessed by the SCSQ.[28,29] The 20-item SCSQ was used to measure the coping skill of Chinese people. The SCSQ consists of 2 subscales, including a 12-item active coping subscale and 8-item negative coping subscale. The 4-point SCSQ ranged from 0 (“rarely”) to 3 (“always”). A higher score on the active coping subscale is indicative of a greater coping ability, whereas a higher score on the negative coping subscale is indicative of a poorer coping ability. Cronbach's alpha coefficients for the active and negative coping subscales were 0.84 and 0.80, respectively.
2.3. Ethical considerations
Ethical approval of this study was obtained from the Medical Ethics Committee board of the hospital and the University. Written informed consents were obtained from all enrolled patients.
2.4. Data analysis
Data analyses were performed by the SPSS 17.0 statistical analysis package (SPSS, Chicago, IL, USA). Data entry was verified by different researchers. Patient demographic and clinical data were analysed according to the descriptive statistics. The independent samples t test and analysis of variance were performed to examine the differences in the PTG scores in the subgroups of patient characteristics. The relationships between PTG and depression, anxiety, and coping skill were explored by correlation analyses. The factors related to PTG were examined by the multiple linear regression analysis.
3. Results
Among the 217 eligible patients we contacted, 10 patients declined to participate due to poor physical health, 8 patients refused to participate because of bad mood, and 26 patients refused to participate with no reason given. Thus, the final sample, consisting of 173 patients, was included for further analyses.
3.1. Sample characteristics
3.1.1. Patient demographic and clinical characteristics
As shown in Table 1, the patient mean age was 53.87 years (SD = 9.19). Most (72.8%) were less than 60 years old. A majority of patients were male (68.8%) and married (95.4%). More than half (57.8%) of the patients received a senior high school educational level or below. The majority (85.5%) had non-small cell lung cancer. The cancer stage among patients was from stage II to IV; there were 11 stage I and II patients (6.3%), 83 stage III patients (48.0%) and 79 stage IV patients (45.7%). Most patients (54.3%) had been diagnosed with lung cancer for more than 6 months. The treatment types reported by patients were concurrent chemo-radiotherapy (28.9%), chemotherapy (55.5%), sequential chemo-radiotherapy (7.5%), and targeted therapy and other treatments (8.1%). The majority (74.6%) had a family income of less than 1000 US dollars per month. Most patients (91.9%) were unemployed since cancer diagnosis. A majority (84.4%) of patients had insurance for treatment. The mean score of PTG, depression, anxiety, and coping style were shown in Table 2.
Table 1.
Demographic and clinical characteristics of patients (n = 173).
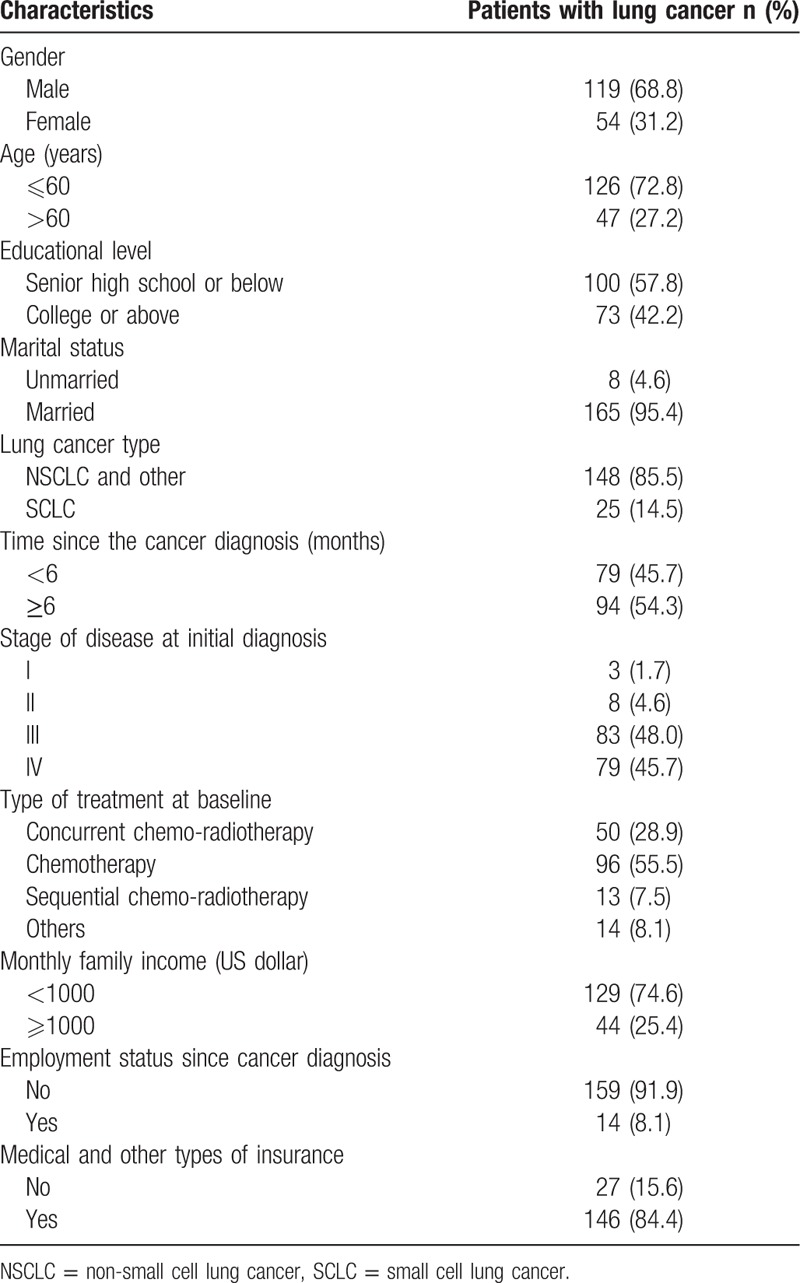
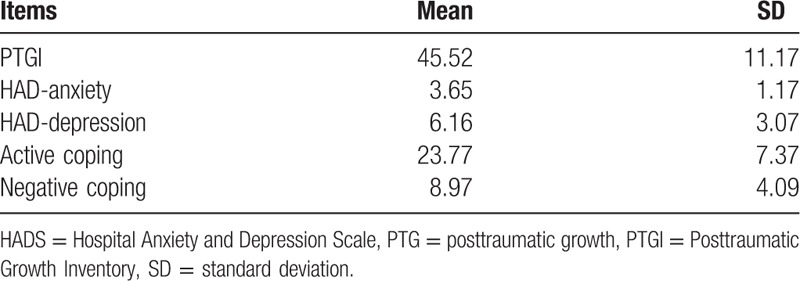
Table 2.
The PTG, depression, anxiety, and coping style among patients with lung cancer (n = 173).
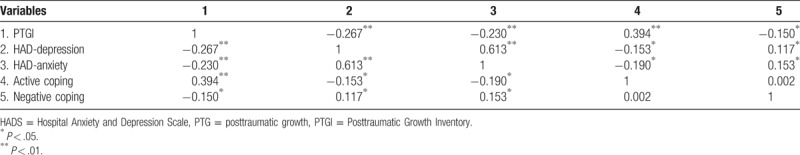
3.1.2. Relationship between the PTG, depression, anxiety and coping skill
As shown in Table 3, the Pearson correlation analyses demonstrated that PTG was inversely correlated with depression (P < .01), anxiety (P < .01), and negative coping (P < .05) and positively correlated with active coping (P < .01).
Table 3.
Relationship between the PTG, depression, anxiety, and coping style (n = 173).
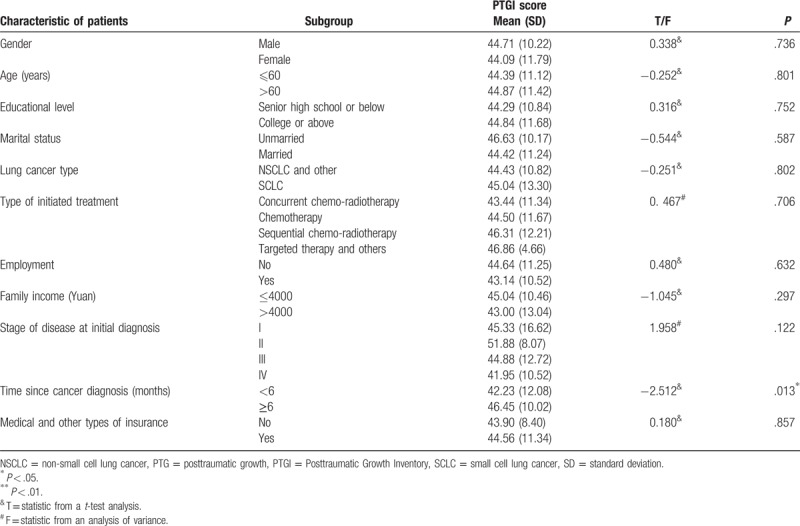
3.1.3. Factors associated with PTG in the univariate analyses
As shown in Table 4, the significant factor of the patient characteristics in univariate analyses was time since cancer diagnosis. Patients who had been diagnosed with cancer for more than 6 months demonstrated a higher level of PTG compared to those diagnosed for less than 6 months.
Table 4.
Factors related to PTG among the characteristics of patients in the univariate analysis (n = 173).
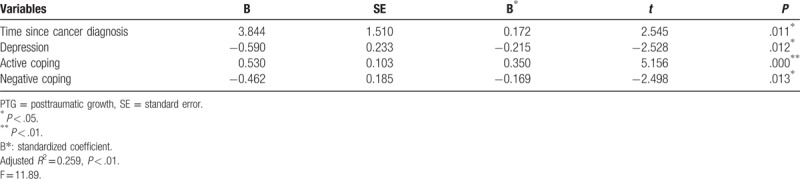
3.1.4. Factors related to PTG in multiple regression analyses
As shown in Table 5, time since cancer diagnosis (P < .05), depression (P < .05), active coping (P < .01), and negative coping (P < .05) were associated with PTG. The independent variables significantly contributed to explaining 25.9% of the variance in PTG.
Table 5.
Factors related to PTG in the multivariate analysis (n = 173).
4. Discussion
This study showed that lung cancer patients experienced benefits from their cancer experience. The factors associated with PTG among lung cancer patients were time since cancer diagnosis, depression, and coping strategies.
The PTG score in this present study was 45.52 (SD = 11.17). The findings were consistent with those of other studies, suggesting that lung cancer patients are similar to other cancer populations who perceived something positive from their traumatic experience.[8,30] However, the PTG score in this study was considerably lower than that reported in other studies.[8,30,31] For example, Cordova et al found that the mean score of PTG was 64.1 among breast cancer patients.[8] Jaarsma et al reported that the mean PTG score was 47.9 in a group of heterogeneous cancer patients.[31] The lower PTG may be related to the characteristics of lung cancer and characteristics of the sample. Lung cancer was the leading cause of cancer deaths worldwide. Compared to other cancers, lung cancer was linked to higher mortality and poorer prognosis. Patients with lung cancer showed higher levels of distress and demands than those with other cancers,[23] which might influence their perception of positive findings. In addition, the majority of patients in this sample were at stages III and IV, and the advanced stages of cancer in our sample might also contribute to the results. Consistent with the present results, Lechner et al showed that the advanced stage of the disease had an impact on the perceived growth, as the life-threatening stress from advanced cancer may overwhelm patients’ capacity to perceive benefits in the traumatic experience.[18]
We found that depression had a adverse relationship with PTG. Patients who experienced a higher level of depression perceived a lower level of PTG. Findings from previous studies in this field were inconsistent.[8,11–13] The results of some studies were consistent with those of the present study[11,12]; however, others reported that depression had no significant relationship with perceived PTG.[8,13] PTG is considered as a cognitive adaptation process that helps individuals perceive the value and meaning of the trauma in their lives.[32] The perceived benefits contribute to psychological adjustments for cancer patients by buffering the effect of psychological distress and protecting these individuals from the effects of negative perception.[33,34] The findings of the negative association between PTG and depression in the present study highlight the necessity of integrating PTG into future interventions and provide new insight for psychological interventions in programs designed to facilitate the experience of PTG, which might in turn play a positive role in depression. Strategies linked to a higher level of PTG, such as acceptance, positive reinterpretation, and active coping,[15] might be beneficial for the psychological well-being of lung cancer patients. Additional studies are essential to examine the relationship of PTG, anxiety, and depression among Chinese patients with lung cancer.
Times since cancer diagnosis and initial treatment are associated with PTG. Patients who had been diagnosed with lung cancer for less than 6 months had a lower level of PTG than those with a longer time since a cancer diagnosis. Whether time following trauma is linked to growth is not clear from previous studies.[4,9] Some studies showed no relations between PTG and time since cancer diagnosis.[14] Whereas others reported that time since cancer diagnosis is linked to an increased growth.[8,30] For example, Helgeson et al found that the relations of positive changes to outcomes were influenced by the amount of time that had passed since stressor onset.[9] The findings in this study showed that time since cancer diagnosis was actively related to PTG. PTG was linked to a cognitive processing of patients. Increased time since cancer diagnosis is related to greater PTG, as growth may take time to occur.[35] Patients diagnosed with cancer for less than 6 months may perceive less PTG due to a lack of knowledge and coping strategies related to lung cancer, thereby decreasing the perceived meanings and benefits from the cancer experience. In addition, a lower time since cancer diagnosis might also make it difficult for patients to endure psychological adjustments from a traumatic event. Therefore, more attention and support are needed for patients who have newly been diagnosed with lung cancer.
We found that active coping was positively related to PTG, whereas negative coping was adversely related to perceived growth. The results related to coping and PTG in this study were consistent with those in other studies.[16,36,37] Active coping (e.g., positive reframing, problem-solving, and approach-oriented strategies) that integrates personal mobilization and available resources facilitates active engagement in stressful events and improves positive changes.[4] Patients who adopted more active coping strategies were linked to a greater level of perceived PTG. In contrast, passive coping strategies, such as denial avoidance, tend toward an accumulation of negative emotion, then aggravate psychological distress and impede the development of positive growth.[37] Patients who adopted negative coping strategies were correlated with a lower level of PTG. Notably, Chinese families typically avoid to have a cancer-related communication with patients.[38,39] However, the active communication of thoughts and feelings may benefit for the PTG development.[35] Partners or couples who openly communicated their concerns and feeling with patients helped to promote patient growth.[30] Additionally, the more an individual actively engages in make sense of their experience following a trauma, the higher the chances for their personal growth.[6,40] In this case, “a lack of cancer-related communication” among Chinese cancer patients and their families might be an inhibitor affecting the personal growth of the patient as a result of the corresponding impact on the behaviors and cope mechanisms of the patient toward the adversity. Thus, strategies intended to improve patient-positive coping, such as self-disclosure, openly communication among the families, and pursuing approach-oriented strategies, are necessary to facilitate the development of PTG.
Several limitations in the present study should be noted. The cross-sectional design made it difficult to examine the potential causal relationships among the factors. In addition, a convenient small sample from only one hospital and the inclusion of patients who had been informed of their cancer diagnosis are other limitations that might affect the sample generalizability to other groups of lung cancer patients. Moreover, as PTG is a multidimensional concept, potential risk factors for PTG, such as support network, posttraumatic stress, and individual personalities (e.g., optimism and hope) should be included in future studies.
4.1. Implications for practice and research
The results of the present study provide new insights to completely understand the experience of cancer patients from a positive perspective. Facilitation of PTG is crucial to health providers to offer appropriate support to improve the psychological well-being of patients. Interventions that facilitate cognitive and coping efforts, including accepting the effects of the trauma, actively engaging in affective expression and communication, actively improving their circumstances, and reframing the stressor in a positive perspective, are areas that can benefit the development of PTG. In addition, given the interdependent relationship among the Chinese families, facilitation of PTG should be extended to close family members in addition to patients who are directly affected by cancer.[11]
5. Conclusion
The present study adds to the results from previous studies by identifying the status of PTG among Chinese patients with lung cancer and informs strategies to facilitate PTG. Time since cancer diagnosis, patient depression, and coping strategies are factors that are related to PTG among Chinese patients with lung cancer. These findings indicate that lung cancer patients may benefit from interventions that reduce depression, provide available support, and improve active coping strategies. More attention should be placed on patients who have been newly diagnosed with lung cancer. Additionally, the impact of the coping strategies on PTG should be highlighted and integrated into targeted interventions.
Acknowledgments
We would like to thank the executives and participating staff of the hospital for their support and assistance. Special thanks give to all participants for their understanding and cooperation.
Author contributions
Conceptualization: Yonglin Su.
Data curation: Xiaolin Hu, Yonglin Su, Wenxia Huang.
Formal analysis: Xiaolin Hu, Wenxia Huang.
Investigation: Xiaolin Hu, Yonglin Su, Wenxia Huang.
Methodology: Xiaolin Hu, Xingchen Peng.
Project administration: Xiaolin Hu, Yonglin Su, Wenxia Huang.
Resources: Xiaolin Hu, Yonglin Su, Wenxia Huang.
Software: Wenxia Huang.
Supervision: Xingchen Peng.
Writing – original draft: Xiaolin Hu, Yonglin Su.
Writing – review & editing: Xiaolin Hu, Xingchen Peng, Wenxia Huang.
Footnotes
Abbreviations: HADS = Hospital Anxiety and Depression Scale, PTG = posttraumatic growth, PTGI = Posttraumatic Growth Inventory, SCSQ= simplified coping style questionnaire, SD = standard deviation.
The authors have no conflicts of interest to disclose.
Ethical approval: This study was approved by the Ethics Committees of Sichuan University.
Funding: The study is funded by the National Natural Sciences Foundation of China (81803104), the Science and Technology Department of Sichuan Province (2016FZ0087 and 2017KZ0033), the Science and Technology Bureau of Chengdu (2018-YFYF-00122-SN), the health and family planning commission of Sichuan province (16PJ344 and 17PJ394), and the initial Science Fund of Sichuan University for the Young Teachers (2017SCU11012).
References
- [1].Chen W, Zheng R, Zeng H, et al. Epidemiology of lung cancer in China. Thorac Cancer 2015;6:209–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Huang HY, Shi JF, Guo LW, et al. Expenditure and financial burden for common cancers in China: a hospital-based multicentre cross-sectional study. Chin J Cancer 2017;36:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Mosher CE, Champion VL, Azzoli CG, et al. Economic and social changes among distressed family caregivers of lung cancer patients. Support Care Cancer 2013;21:819–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Stanton AL, Bower JE, Low CA. Calhoun LG, Tedeschi RG. Posttraumatic growth after cancer. Handbook of Posttraumatic Growth. Mahwah, NJ: Lawrence Erlbaum Associates Inc.; 2006. 138–75. [Google Scholar]
- [5].Ai AL, Park CL. Possibilities of the positive following violence and trauma: informing the coming decade of research. J Interprers Violence 2005;20:242–50. [DOI] [PubMed] [Google Scholar]
- [6].Tedeschi RG, Calhoun LG. Trauma and Transformation: Growing in the Aftermath of Suffering. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- [7].Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 1996;9:455–71. [DOI] [PubMed] [Google Scholar]
- [8].Cordova MJ, Cunningham LL, Carlson CR, et al. Posttraumatic growth following breast cancer: a controlled comparison study. Health Psychol 2001;20:176–85. [PubMed] [Google Scholar]
- [9].Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. J Consult Clini Psychol 2006;74:797–816. [DOI] [PubMed] [Google Scholar]
- [10].Pirl WF. Chabner BA, Lynch TJ, Longo DL. Depresión, ansiedad y fatiga. Harrison's Manual de Oncología. Mexico City: McGraw-Hill de Mexico; 2011. 190–6. [Google Scholar]
- [11].Ho SM, Chan CL, Ho RT. Posttraumatic growth in Chinese cancer survivors. Psychooncology 2004;13:377–89. [DOI] [PubMed] [Google Scholar]
- [12].Frazier P, Conlon A, Glaser T. Positive and negative life changes following sexual assault. J Consult Clin Psychol 2001;69:1048–55. [DOI] [PubMed] [Google Scholar]
- [13].Milam JE, Ritt-Olson A, Unger JB. Posttraumatic growth among adolescents. J Adolescent Res 2004;19:192–204. [Google Scholar]
- [14].Mystakidou K, Tsilika E, Parpa E, et al. Personal growth and psychological distress in advanced breast cancer. Breast 2008;17:382–6. [DOI] [PubMed] [Google Scholar]
- [15].Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: benefit finding, positive reappraisal coping, and posttraumatic growth in women with early-stage breast cancer. Health Psycho 2003;22:487–97. [DOI] [PubMed] [Google Scholar]
- [16].Bellizzi KM, Blank TO. Predicting posttraumatic growth in breast cancer survivors. Health Psychol 2006;25:47–56. [DOI] [PubMed] [Google Scholar]
- [17].Thornton AA, Perez MA. Posttraumatic growth in prostate cancer survivors and their partners. Psychooncology 2006;15:285–96. [DOI] [PubMed] [Google Scholar]
- [18].Lechner SC, Zakowski SG, Antoni MH, et al. Do sociodemographic and disease-related variables influence benefit-finding in cancer patients? Psychooncology 2003;12:491–9. [DOI] [PubMed] [Google Scholar]
- [19].Schulz U, Mohamed NE. Turning the tide: benefit finding after cancer surgery. Soc Sci Med 2004;59:653–62. [DOI] [PubMed] [Google Scholar]
- [20].ACS. Cancer Facts and Figures 2010. Atlanta, GA: American Cancer Society, National Home Office; 2010. [Google Scholar]
- [21].Fox SW, Lyon DE. Symptom clusters and quality of life in survivors of lung cancer. Oncol Nurs Forum 2006;33:931–6. [DOI] [PubMed] [Google Scholar]
- [22].Li J, Girgis A. Supportive care needs: are patients with lung cancer a neglected population? Psychooncology 2006;15:509–16. [DOI] [PubMed] [Google Scholar]
- [23].Zabora J, BrintzenhofeSzoc K, Curbow B, et al. The prevalence of psychological distress by cancer site. Psychooncology 2001;10:19–28. [DOI] [PubMed] [Google Scholar]
- [24].Dionne-Odom JN, Hull JG, Martin MY, et al. Associations between advanced cancer patients’ survival and family caregiver presence and burden. Cancer Med 2016;5:853–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiat Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- [26].Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res 2002;52:69–77. [DOI] [PubMed] [Google Scholar]
- [27].Qian J, Bian CD, Cui HD, et al. Comparative study of reliability and validity between several screening scales of anxiety. J Internal Med Concepts Prac 2011;6:176–9. [Chinese]. [Google Scholar]
- [28].Jie Y. Reliability and validity of the implified coping style questionnaire (SCSQ). Chin J Clin Psychol 1998;6:114–5. [Google Scholar]
- [29].Wang XD, Wang XL, Ma H. Rating Scales for Mental Health. Beijing: Chinese Mental Health Journal Press; 2009. [Google Scholar]
- [30].Manne S, Ostroff J, Winkel G, et al. Posttraumatic growth after breast cancer: patient, partner, and couple perspectives. Psychosom Med 2004;66:442–54. [DOI] [PubMed] [Google Scholar]
- [31].Jaarsma TA, Pool G, Sanderman R, et al. Psychometric properties of the Dutch version of the posttraumatic growth inventory among cancer patients. Psychooncology 2006;15:911–20. [DOI] [PubMed] [Google Scholar]
- [32].Janoff-Bulman R, Frantz CM. Power M, Brewin CR. The impact of trauma on meaning: from meaningless world to meaningful life. Wiley, The Transformation of Meaning in Psychological Therapies: Integrating Theory and Practices. New York: 1997. [Google Scholar]
- [33].Silva SM, Moreira HC, Canavarro MC. Examining the links between perceived impact of breast cancer and psychosocial adjustment: the buffering role of posttraumatic growth. Psychooncology 2012;21:409–18. [DOI] [PubMed] [Google Scholar]
- [34].Vickberg SMJ, Bovbjerg DH, DuHamel KN, et al. Intrusive thoughts and psychological distress among breast cancer survivors: global meaning as a possible protective factor. Behav Med 2000;25:152–60. [DOI] [PubMed] [Google Scholar]
- [35].Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inquiry 2004;15:1–8. [Google Scholar]
- [36].Kinsinger DP, Penedo FJ, Antoni MH, et al. Psychosocial and sociodemographic correlates of benefit-finding in men treated for localized prostate cancer. Psychooncology 2006;15:954–61. [DOI] [PubMed] [Google Scholar]
- [37].Widows MR, Jacobsen PB, Booth-Jones M, et al. Predictors of posttraumatic growth following bone marrow transplantation for cancer. Health Psychol 2005;24:266–73. [DOI] [PubMed] [Google Scholar]
- [38].Mystakidou K, Parpa E, Tsilika E, et al. The families evaluation on management, care and disclosure for terminal stage cancer patients. BMC Palliat Care 2002;1:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Caughlin JP, Mikucki-Enyart SL, Middleton AV, et al. Being open without talking about it: a rhetorical/normative approach to understanding topic avoidance in families after a lung cancer diagnosis. Commun Monogr 2011;78:409–36. [Google Scholar]
- [40].Taylor SE. Adjustment to threatening events: a theory of cognitive adaptation. Am Psychol 1983;38:1161–73. [Google Scholar]


