Abstract
Many barriers to primary healthcare accessibility in the United States exist including an increased opportunity cost associated with seeking primary care. New models of healthcare delivery aimed at addressing these problems are emerging. The potential impact that on-demand primary care physician house calls services can have on healthcare accessibility, patient care, and satisfaction by both patients and physicians is poorly characterized.
We performed a retrospective observational analysis on data from 13,849 patients who utilized Heal, Inc, an application (app)-based, on-demand house calls platform between August 2016 and July 2017. We assessed house call wait time and visit duration, diagnoses by International Classification of Diseases, tenth revision, Inc (ICD10) codes, and house call outcomes by post-visit prescription and lab requests, and patient satisfaction survey.
Patients who utilized this physician house call service had a bimodal age distribution peaking at age 1 year and 36 years. Same day acute sick exams (93.9% of pediatric (Ped) and 66.9% of adult requests) for fever and/or acute upper respiratory infection represented the most common use. The mean wait time for as soon as possible house calls were 96.1 minutes, with an overall mean house call duration of 27.1 minutes. A house call was primarily chosen over an Urgent Care Clinic or Doctor's office (46.2% and 41.6% of respondents, respectively), due to convenience or fastest appointment available (69.6% and 33.8% of respondents, respectively). Most survey respondents (94.2%) would schedule house calls again.
On-demand physician house calls programs can expand access options to primary healthcare, primarily used by younger individuals with acute illness and preference for a smartphone app-based home visit.
Keywords: healthcare delivery models, on-demand physician house calls, primary care accessibility
1. Introduction
Throughout the 20th century, the physician house call and its role in patient care have changed dramatically. In 1930, physician house calls represented 40% of physician-patient encounters.[1] A detailed analysis of house calls in 1972 found that approximately 5% of care provided by general practitioners was in their patient's homes, with two-thirds of those for patients aged greater than 55 years.[2] By 1980 house calls had decreased to less than 1% as primary care became more clinic-based.[1] Shifts in physician reimbursement patterns, patient accessibility to transportation and proximity to medical centers all contributed to the changing trend.[1]
Over time, the model of providing healthcare in the home underwent reshaping with the rise of home healthcare agencies focused on providing medical services to a population with significant limitations accessing regular medical care, such as for homebound patients, hospice services, hospital follow-up programs or concierge services.[3,4] Across the general population, however, there is a growing unmet need to address the ever-increasing sharp rise in barriers to healthcare access, primarily including cost and availability of timely care. Wait times for new patient appointments for non-emergency medical conditions continue to increase, with an average greater than 3 weeks in the United States.[5] The alternative of an emergency room (ER) visit with its wait-time and expense is seen as a major drawback for many individuals. As healthcare access worsens and given today's more consumer-driven landscape with smartphone applications (apps) and many on-demand services catering to an “I want what I want when I want it” (known as IWWIWWIWI) consumer attitude, app-based physician house calls are emerging with the goal to both meet consumer preference and facilitate more rapid access and the potential to avoid emergency or urgent care facilities.
Heal Inc is one of several new companies in the last few years offering on-demand home health care via a smartphone app service or online. Requests for same day or future house calls are made through the app, and a physician and medical assistant arrive to the patient's residence for the appointment or within 2 hours for as soon as possible (ASAP) requests. The service is focused on non-emergency, acute illness assessments as well as wellness and preventive exams, and is comparable to community-based primary care offices, retails clinics, or urgent care options including minor wound care, laboratory tests, flu shots, new prescriptions and medication refills, and imaging and specialty services referrals. Here we present data obtained during a 1-year analysis of house calls to characterize the patient population served and medical needs met through this new healthcare delivery approach.
2. Methods
We independently performed a retrospective observational analysis on data collected on Heal house calls made to 13,849 patients over 1 year from August 2016 to July 2017 from the greater Los Angeles area and additional locations as the service became available during this period including Silicon Valley, San Francisco, San Diego, Orange County, and Washington DC metropolitan areas. The database was supplied directly from Heal after undergoing frequency analysis as below using excel documents or directly from SurveyMonkey for the patient after-visit survey data. Study authors did not have access to the Heal raw database. The study underwent Scripps Health Institutional Review Board (IRB) review and exemption. Patient demographics characterized included sex, age (2 patients with invalid age data were excluded from the age analysis only), and insurance type. Physician profiles included sex, age, specialty, and number of house calls performed weekly. House calls were characterized with chief complaint, service or medication provided, billing codes, and referrals, as well as day and time when service was requested, the mean wait time for ASAP house calls, and mean house call duration. Wait time for an ASAP visit is defined as the time difference between when the service is requested from the app and when the doctor arrives at the home and starts the encounter. House call time of day requests were scheduled within 2-hour windows during 8AM to 8PM business hours, with ASAP requests booked outside of business hours timed to the first next day AM window. There were 12 pediatric (Ped) and 18 adult ASAP requests outside of business hours before the implementation of assigning the next day first AM time window which were removed from analysis due to incorrect binning. House call duration is calculated from the on-call app utilized by Heal physicians to log the encounter start and stop time. Certain data from the International Classification of Diseases, tenth revision, Inc (ICD10) code frequency analysis were subsequently pooled if they represented similar diagnoses as follows: acute upper respiratory infection (URI)/cough/pharyngitis/nasopharyngitis/nasal congestion/throat pain (J06.9, R05, J02.9, J00, R09.81, R07.0), fever/viral infection, unspecified (R50.9, B34.9), Acute Serous Otitis Media (H65.03, H65.02, H65.01), Acute Suppurative Otitis Media (H66.001, H66.003), routine health exam/encounter for immunization/general adult medical exam (Z23, Z00.129, Z00.00), Rash/Nonspecific Skin Eruption (R21), viral conjunctivitis (B30.9), streptococcal pharyngitis (J02.0), pneumonia (J18.9), acute bronchitis (J20.9), acute sinusitis (J01.80, J01.00, J01.90), allergic rhinitis/postnasal drip (R09.82, J30.9, J30.2), essential hypertension (HTN)/elevated blood pressure (BP) without HTN diagnosis (I10, R03.0), urinary tract infection (N39.0), infectious gastroenteritis and colitis, unspecified (A09). Additionally, 5296 of 6163 Ped visits and 9210 of 12,269 adult visits had at least 1 ICD10 code recorded. Visits with no recorded ICD10 code in our database resulted from a loss of data incurred from an earlier version of software used to sync the Heal database with the Heal EMR and are not included in the ICD10 analysis and noted with an asterisk. Some data were only available during the period from May 1 to June 30, 2017 and are noted with an asterisk.
2.1. Chief complaint identification
All patient-reported symptoms that were documented at the time the visit was requested were recorded. Collocation analysis was subsequently performed on this dataset using trigrams and unigrams in order to surface patterns of symptoms per published methods,[6,7] and performed by Heal. House calls without reported symptoms were not considered for analysis. Other entries for corporate visits, such as flu shot drives, were also removed. In the unigram analysis, after the data was cleaned, stop words (as defined for English in the nltk library) were removed from the descriptions. For unigrams, only frequency (defined as count/total number of house calls after cleaning) was calculated. Trigrams/Bigrams were scored by frequency, t-scores, and jaccard index. These scores were normalized, and a mean was used to identify the top trigrams/bigrams. Next, a count and frequency were calculated for these trigrams/bigrams, and the trigrams/bigrams were ranked by frequency. In another table, trigrams/bigrams containing common words (cough, sore, throat, fever ear, flu) were filtered out. A trigram/bigram containing the aforementioned words anywhere was removed so that the more uncommon trigrams could be identified. Analysis mostly involved unigrams. Additional associations with 1 or 2 more words required analysis of the bigrams or trigrams. The n-gram groups which is the union of the occurrences of each different n-grams in each n-gram group are ranked by frequency.
2.2. Survey
Patients were provided with a voluntary after visit survey using SurveyMonkey online. Survey data were collected from May 1 through June 30. Participants were asked 6 questions regarding the house call and were not required to answer all questions. The number responded to each question was recorded. Parents of minors were asked to complete the survey on their behalf.
3. Results
Heal physicians made 18,432 total combined house calls and enterprise/corporate visits to 13,849 patients between August 2016 and July 2017. Patients were nearly equally male (48.5%) versus female (51.5%). There was a predominant bimodal age distribution, with the majority of patients falling between age ranges 0 to 10 (24.3%) and 23 to 50 (60.6%), with the oldest patient seen during this time period considered for age analysis recorded at 103. The bimodal peaks were seen at age 1 year and at 36 years (Fig. 1). Patients most commonly were self-pay for the house calls (52%) or had a preferred provider organization (PPO) insurance plan (21%), or were employer self-insured (14%).
Figure 1.
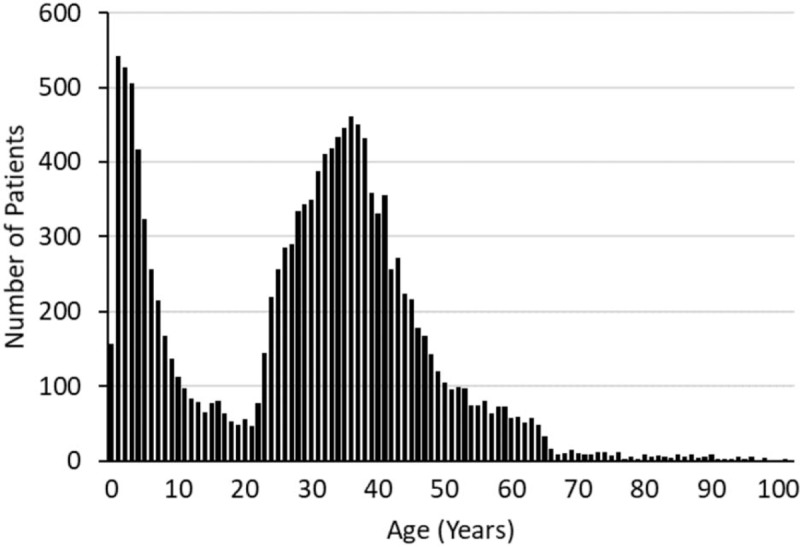
Histogram plot of patient age distribution. House calls to 13,849 patients made between August 2016 and July 2017 were analyzed for frequency of patient age.
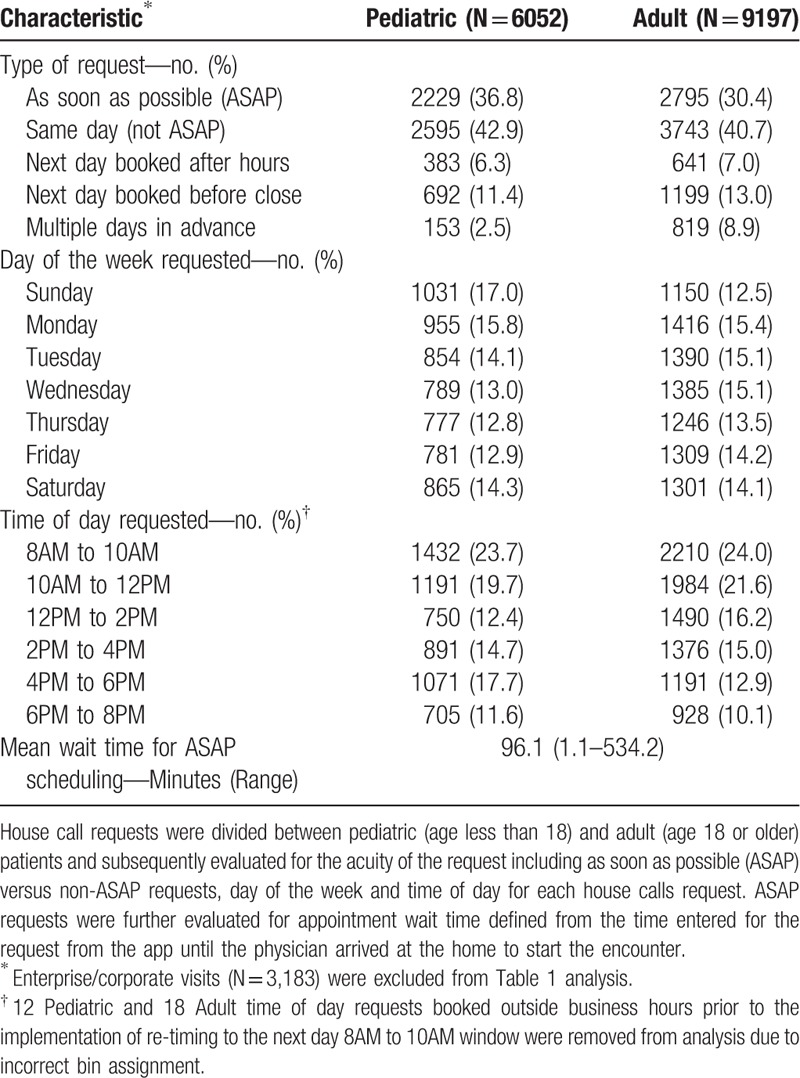
The profile of house call requests is detailed in Table 1. Enterprise/corporate visits (n = 3183) were excluded from analysis. Most patients scheduling a house call request an ASAP (Peds 36.8%, Adult 30.4%) or same day (Peds 42.9%, Adult 40.7%) appointment, with some patients requesting next day appointments (booked after hours Peds 6.3%, Adult 7.0% or before 8pm close Peds 11.4%, Adult 13.0%), and a small percentage (Peds 2.5%, Adult 8.9%) requesting house calls 2 or more days in advance. Days of the week on which house calls are requested indicate no significant difference between days, whether weekend or weekday. Time of day requested shows a trend toward AM appointment windows. (Table 1). The mean wait time from appointment request to physician arrival for ASAP house calls was 96.1 minutes (range 1.1–534.2 min).
Table 1.
House call request profile.
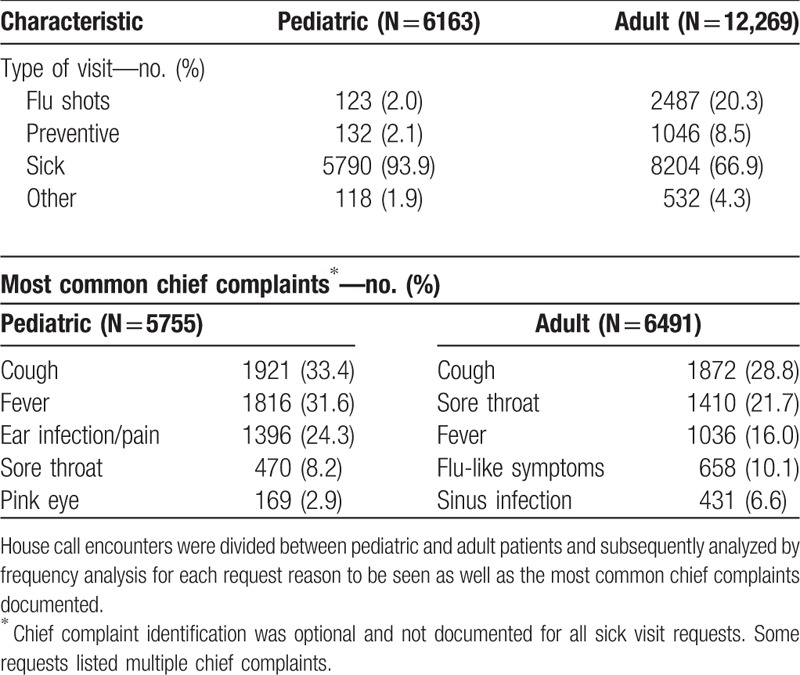
With the inclusion of enterprise visits, which were most often for influenza vaccination campaigns, most requests were for illness assessments (Peds 93.9%, Adult 66.9%), and influenza vaccination (Peds 2%, Adult 20.3%) versus preventive exams (Peds 2.1%, Adult 8.5%) (Table 2). Patients requested house calls most commonly for chief complaints including cough, fever, sore throat, ear infection, flu-like symptoms, sinus infection, or pink eye, with frequencies of the top chief complaints specifically among children versus adults indicated in Table 2. The identification of a chief complaint was optional although it was listed for 92.6% of requests.
Table 2.
Visit type and chief complaint profile.
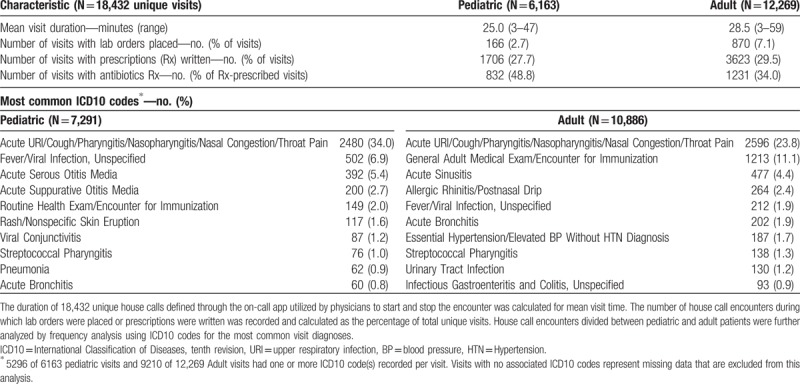
Post-house call data was collected and profiled in Table 3. The mean house call duration lasted 25 minutes for Ped visits (range 3–47 min), and 28.5 minutes for adult visits (range 3–59 minutes) with an overall mean of 27.1 minutes. After 18,432 unique visits, 166 Ped and 870 adult visits resulted with lab placement orders and 1706 Ped and 3623 adult visits resulted with medication prescription(s), within which the proportion of those including antibiotics was higher in Peds (48.8% of Peds prescriptions versus 34.0% of Adult prescriptions). The most common prescriptions overall were in decreasing frequency: Amoxicillin/Augmentin, Azithromycin, Albuterol, Cefdinir, Benzonatate, Saline drops, Ondansetron, Azelastine, or Ipratropium. Lab orders overall included complete blood or metabolic panels, lipid panels, endocrine, and vitamin level testing, sexually transmitted infection screens, upper respiratory cultures/screening tests, and urinalyses, among others. ICD10 codes were assessed to determine most common diagnoses during house calls with visits generated from physician follow-up calls excluded from analysis. ICD10 codes were most commonly characterized collectively as diagnoses of respiratory tract or ear, nose, throat (ENT) infections or allergic symptoms, unspecified fever or viral infections, and general wellness exams and immunization administration encounter. Patient referrals to specialists and follow-up Heal appointments were made after 1.8% and 2.2% of house calls, respectively; however, continuing care measures were only characterized over 2 months of the full dataset due to availability.
Table 3.
After-house call profile.
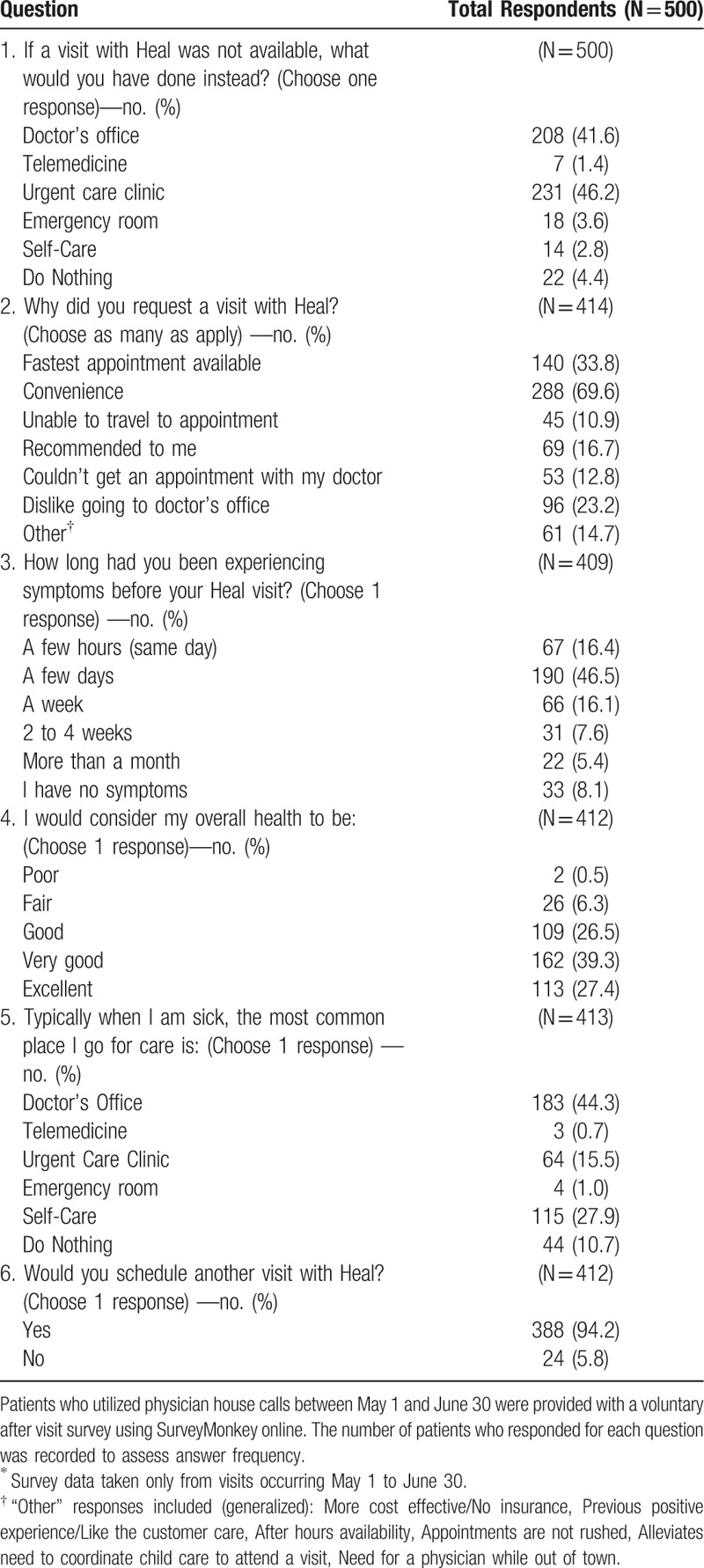
A total of 500 respondents out of 3205 visits between May 1 and June 30 answered most or all of the post-house calls online survey (Table 4). Patients were most likely to choose a house call over a visit at a Doctor's office (41.6%) or Urgent Care (46.2%), due to convenience or fast availability (69.6% and 33.8% of respondents, respectively). The majority of patients had been experiencing symptoms for no longer than 1 week (a few hours/same day 16.4%, a few days 46.5%, a week 16.1%), with 8.1% of patients booking exams with no specific symptom complaint. Patients self-report themselves to be generally in good to excellent health (poor 0.5%, fair 6.3%, good 26.5%, very good 39.3%, excellent 27.4%). Patients report in general that they typically utilize a doctor's office for sick visits (44.3%), however collectively many otherwise follow self-care (27.9%) or do nothing (10.7%) when sick, while others reported typically using an urgent care (15.5%), ER (1%), or telemedicine (0.7%). Overwhelmingly patients responded yes that they would schedule a house call again (94.2%).
Table 4.
Patient after-house call survey data∗.
Heal employed 90 physicians during this time period. Physicians were 35% females and 65% males and ranged in age from 32 to 65, with the mean physician age of 40. Physicians averaged 6.7 house calls per week, and most (75%) physicians worked part-time. Physician background training ranged from Family Practice (40%), Internal Medicine (28%), Peds (30%), and Emergency Medicine (2%).
4. Discussion
The development of mobile access platforms to support physician house calls on-demand has resulted in the return of a healthcare delivery model that has not been evaluated for over 45 years,[2] which to date has not been adequately studied. Our data indicate that the app-based house calls model is primarily utilized by younger patients, or working-aged adults, from 0 to 10 and 23 to 50 years, for ASAP or same day acute sick assessments often regarding fever or upper respiratory symptoms. Patients waited for a mean of 96.1 minutes for ASAP house calls, and the mean house calls duration lasted 27.1 minutes. Patients chose a house call most commonly over an urgent care clinic or doctor's office due to fast availability and convenience, and most would utilize the service again.
Several mobile app-based services have emerged in the past few years with variability in house calls model including whether a doctor or nurse practitioner is sent to the home and whether chief complaints are assessed first via a telemedicine-based visit, with variation in operating hours, or whether insurance is accepted, for example.[8] These services typically operate within 1 to a few major cities. Medicast was one of the first apps, starting in Miami in 2013, followed by Pager serving Manhattan in 2014.[9,10] FRND also serves New York City employing nurses for house calls, with physician video conferencing if needed. Denver-based Dispatch Health offers urgent care services either via patient mobile request or via triage of local 911 calls that may not necessitate ER transfer by bringing to the patient's home a Clinical Laboratory Improvement Amendments (CLIA)-certified lab, medications and IVs,[11] and likewise Mend and Ped-specific PediaQ offer urgent care services via house calls within the Dallas-Fort Worth area.[8] Similar to Heal, Circle Medical in San Francisco aims to extend the house calls platform from a primary urgent care focus to offering multiple primary care services including wellness exams, vaccinations, and chronic disease management.[12]
Up until these recent on-demand house calls platforms became readily accessible in many major US markets, physicians conducting house calls tended to be older and work in rural and/or solo practice settings often working together with the home health agency model of multidisciplinary medical care targeted to a typically geriatric high-risk patient population.[13–15] Patients served in this capacity include those recently discharged from the hospital, typically with multiple medical co-morbidities who have limitations in their access to regular care, those enrolled in palliative care services,[3] or necessitating acute hospital care direct to the home for select medical conditions.[16] In contrast, the data in this study reveal that younger patients requested house calls through an app, which may indicate a limited reach of newer mobile house calls platforms to the population more accustomed to arranging consumer services via smartphone. It is important to note, however, that this model may prove most adept at serving primarily acute sick visits and further studies are needed to determine if on-demand mobile health apps can address the need for continuity of care in primary care settings, including patients on Medicare, which was not accepted by Heal Inc at the time of the study however is currently an inclusion criteria. Given that these models are new, there will need to be an assessment of more longitudinal data in order to measure healthcare quality outcomes compared to office or clinic-based services. Additionally, these services are typically offered in major cities, without ameliorating the access problem in regions with less population density and rural areas. Moreover, while Heal provides services to patients regardless of language, there may be challenges to non-native English speakers in using the app. It is therefore unclear the extent to which this model addresses these potential healthcare disparities.
Mobile-based on-demand physician house calls platforms may best address the opportunity cost associated with and therefore 1 barrier to access in seeking medical care. The opportunity cost associated with an outpatient visit is significant; the mean time associated with ambulatory medical visits is 121 minutes, including 37 minutes of travel and 84 minutes at the clinic, of which face-to-face physician time is only approximately 20 minutes.[17] Of note, interventions to decrease patient waiting room time in primary care correspond to increased patient visit satisfaction.[18] Mobile-based healthcare apps offer timely medical care options with ASAP or same day house calls which circumvents the need to drive to and wait at a clinic for care, corroborated by patient post-visit survey data which indicated a house calls appointment was chosen due to convenience. Our data indicate that outside of the Ped population most patients utilizing this mobile-based service were working aged adults, and this population has previously been identified to struggle with access barriers to healthcare despite recent reforms in the healthcare insurance market.[19] Mobile-based platforms may prove adept at improving access for this population in particular, which requires further longitudinal study.
The impact of on-demand physician house calls on overall healthcare spending remains to be fully studied. Data from multiple studies reviewing multidisciplinary house calls to high risk primarily geriatric populations have indicated that enrollment in a home-based primary care practice with multiple follow-up visits is associated with fewer hospitalizations and skilled nursing facility admissions, with fewer subspecialist visits, increased independence to continue living at home, and results in overall decreased Medicare costs.[1,20–27] Nursing-based neonatal home visits have additionally been shown to be cost-effective and reduce the rate of newborn acute care visits and hospitalizations.[28,29] These data have led to Medicare-based incentives for physician house calls within this high risk older adult population, whereas conversely studies to determine cost-effectiveness of the newer mobile-based physician house calls on-demand platforms are lacking and few insurance plans currently provide coverage for these visits. Future studies are thus needed to assess whether new health systems innovation models like Heal will lead to overall healthcare savings while delivering high-quality care before any expansion of health policy incentives for physician house calls performed through these mobile app-based services. Based on survey data in this study indicating nearly half of patients would alternatively seek urgent or emergency care services, there may exist significant potential healthcare savings; this intriguing observation remains as a hypothesis requiring prospective assessment and ideally a randomized, controlled trial. The economic impact of decreased physician efficiency in time spent traveling to visits relative to cost savings associated with decreased overhead expenses on the overall cost of healthcare remains unclear. Atlanta-based MedZed is 1 technology-based house call platform that has sought to address this concern by shifting from an on-demand primarily urgent care house calls service to a chronic care house calls service allowing routine follow-up visits to be more cost-effectively performed in the home by licensed vocational and/or registered nurses with remote access to the physician.[8] Any potential healthcare policy recommendations in support of this healthcare delivery model will be dependent upon completion of a rigorous cost-effectiveness analysis.
The United States continues to experience a primary care physician shortage,[30] and many physicians-in-training reports selecting a career path based on the potential for work satisfaction and work-life balance,[31] however currently residency programs have little-dedicated instruction on physician house calls.[1,32] Heal physicians range in age from 32 to 65 years; most work part-time averaging just under 7 visits per week and have training across family practice, internal medicine, Peds, and emergency medicine. They have increased schedule flexibility and average longer visits than the national average for primary care, at 27.1 versus 18.5 minutes, respectively,[33] which may improve both physician sense of fulfillment and patient satisfaction. Importantly, however, it remains to be studied whether this model can support a physician's long-term career. Overall app-based, on-demand physician house calls represent a new model of healthcare delivery offering convenient access to primary care physicians, but with many uncertainties that require further rigorous assessment.
Author contributions
Conceptualization: Shannon Fortin Ensign, Katie Baca-Motes, Steven Steinhubl.
Data curation: Katie Baca-Motes, Steven Steinhubl.
Formal analysis: Shannon Fortin Ensign, Katie Baca-Motes, Steven Steinhubl, Eric Topol.
Funding acquisition: Steven Steinhubl, Eric Topol.
Investigation: Steven Steinhubl.
Methodology: Shannon Fortin Ensign, Steven Steinhubl, Eric Topol.
Supervision: Steven Steinhubl, Eric Topol.
Writing – original draft: Shannon Fortin Ensign, Steven Steinhubl, Eric Topol.
Writing – review & editing: Shannon Fortin Ensign, Katie Baca-Motes, Steven Steinhubl, Eric Topol.
Footnotes
Abbreviations: app = application, ASAP = as soon as possible, ER = emergency room, HTN = hypertension, ICD10 = International Classification of Diseases, tenth revision, Inc = Incorporated, Ped = pediatric.
Supported in part by the National Institutes of Health (NIH)/National Center for Advancing Translational Sciences grant UL1TR001114, a grant from the Qualcomm Foundation, and NIH training grant KL2TR001112 (SFE). We would like to acknowledge Xiaoxu Wu, Grace Zhou, and Renee Dua of Heal for their assistance in data collection and frequency analysis.
All authors had access to the data and contributed to manuscript writing. The authors have no conflicts of interests to disclose.
References
- [1].Kao H, Conant R, Soriano T, et al. The past, present, and future of house calls. Clin Geriatr Med 2009;25:19–34. [DOI] [PubMed] [Google Scholar]
- [2].Elford RW, Brown JW, Robertson LS, et al. A study of house calls in the practices of general practitioners. Med Care 1972;10:173–8. [DOI] [PubMed] [Google Scholar]
- [3].Unwin BK, Tatum PE., 3rd House calls. Am Fam Physician 2011;83:925–38. [PubMed] [Google Scholar]
- [4].Levine SA, Boal J, Boling PA. Home care. JAMA 2003;290:1203–7. [DOI] [PubMed] [Google Scholar]
- [5].Merritt Hawkins 2017 Survey of Physician Appointment Wait Times. Available at: https://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/mha2017waittimesurveyPDF.pdf [access date August 10, 2017]. [Google Scholar]
- [6].Manning CD, Schutze H. Foundations of Statistical Natural Language Processing. 1999;Cambridge, Massachusetts: The MIT Press, 149–314. [Google Scholar]
- [7].Trigram Scoring Methods. Available at: http://www.nltk.org/_modules/nltk/metrics/association.html Accessed August 28, 2017. [Google Scholar]
- [8].Chesanow N. Housecalls are back and booming. Are they a threat to PCPs? 2016. Available at: https://www.medscape.com/viewarticle/866207 Accessed December 30, 2017. [Google Scholar]
- [9].Schmidt C. Uber-inspired apps bring a doctor right to your door. 2014. Available at: www.cnn.com/2014/07/31/health/doctor-house-call-app/index.html Accessed December 28, 2017]. [Google Scholar]
- [10].Comstock J. Providence St. Joseph Health acquires Medicast, an early app-enabled house call service provider. 2016. Available at: www.mobihealthnews.com/content/providence-st-joseph-health-acquires-medicast-early-app-enabled-house-call-service-provider Accessed December 28, 2017. [Google Scholar]
- [11].Pai A. Dispatch Health raises $3.6 M for doctor house call service. 2015. Available at: www.mobihealthnews.com/46086/dispatch-health-raises-3-6m-for-doctor-house-call-service Accessed December 28, 2017. [Google Scholar]
- [12].Pai A. Circle Medical raises $2.9 M for primary care house call app. 2015. Available at: http://www.mobihealthnews.com/48745/circle-medical-raises-2-9m-for-primary-care-house-call-app Accessed December 28, 2017. [Google Scholar]
- [13].Sairenji T, Jetty A, Peterson LE. Shifting Patterns of Physician Home Visits. J Prim Care Community Health 2016;7:71–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Peterson LE, Landers SH, Bazemore A. Trends in physician house calls to Medicare beneficiaries. J Am Board Fam Med 2012;25:862–8. [DOI] [PubMed] [Google Scholar]
- [15].Meyer GS, Gibbons RV. House calls to the elderly—a vanishing practice among physicians. N Engl J Med 1997;337:1815–20. [DOI] [PubMed] [Google Scholar]
- [16].Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med 2005;143:798–808. [DOI] [PubMed] [Google Scholar]
- [17].Ray KN, Chari AV, Engberg J, et al. Opportunity costs of ambulatory medical care in the United States. Am J Manag Care 2015;21:567–74. [PMC free article] [PubMed] [Google Scholar]
- [18].Michael M, Schaffer SD, Egan PL, et al. Improving wait times and patient satisfaction in primary care. J Healthc Qual 2013;35:50–9. [DOI] [PubMed] [Google Scholar]
- [19].Kennedy J, Wood EG, Frieden L. Disparities in insurance coverage, health services use, and access following implementation of the affordable care act: a comparison of disabled and nondisabled working-age adults. Inquiry 2017;54:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].De Jonge KE, Jamshed N, Gilden D, et al. Effects of home-based primary care on medicare costs in high-risk elders. J Am Geriatr Soc 2014;62:1825–31. [DOI] [PubMed] [Google Scholar]
- [21].Wajnberg A, Wang KH, Aniff M, et al. Hospitalizations and skilled nursing facility admissions before and after the implementation of a home-based primary care program. J Am Geriatr Soc 2010;58:1144–7. [DOI] [PubMed] [Google Scholar]
- [22].Beck RA, Arizmendi A, Purnell C, et al. House calls for seniors: building and sustaining a model of care for homebound seniors. J Am Geriatr Soc 2009;57:1103–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kellogg FR, Brickner PW. Long-term home health care for the impoverished frail homebound aged: a twenty-seven-year experience. J Am Geriatr Soc 2000;48:1002–11. [DOI] [PubMed] [Google Scholar]
- [24].Melnick GA, Green L, Rich J. House calls: California program for homebound patients reduces monthly spending, delivers meaningful care. Health Aff (Millwood) 2016;35:28–35. [DOI] [PubMed] [Google Scholar]
- [25].Stuck AE, Egger M, Hammer A, et al. Home visits to prevent nursing home admission and functional decline in elderly people: systematic review and meta-regression analysis. JAMA 2002;287:1022–8. [DOI] [PubMed] [Google Scholar]
- [26].Centers for Medicare & Medicaid Services. Independence at Home Demonstration. Available at: https://innovation.cms.gov/initiatives/independence-at-home/ Accessed August 10, 2017. [Google Scholar]
- [27].Centers for Medicare & Medicaid Services. Independence at Home Demonstration Corrected Performance Year 2 Results. Available at: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2017-Fact-Sheet-items/2017-01-19.html Accessed August 10, 2017. [Google Scholar]
- [28].Braveman P, Miller C, Egerter S, et al. Health service use among low-risk newborns after early discharge with and without nurse home visiting. J Am Board Fam Pract 1996;9:254–60. [PubMed] [Google Scholar]
- [29].Paul IM, Phillips TA, Widome MD, et al. Cost-effectiveness of postnatal home nursing visits for prevention of hospital care for jaundice and dehydration. Pediatrics 2004;114:1015–22. [DOI] [PubMed] [Google Scholar]
- [30].Kozakowski SM, Travis A, Bentley A, et al. Entry of US medical school graduates into family medicine residencies: 2015–2016. Fam Med 2016;48:688–95. [PubMed] [Google Scholar]
- [31].Kernan WN, Elnicki DM, Hauer KE. The selling of primary care 2015. J Gen Intern Med 2015;30:1376–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Sairenji T, Wilson SA, D’Amico F, et al. Training family medicine residents to perform home visits: a CERA survey. J Grad Med Educ 2017;9:90–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Bruen BK, Ku L, Lu X, et al. No evidence that primary care physicians offer less care to Medicaid, community health center, or uninsured patients. Health Aff (Millwood) 2013;32:1624–30. [DOI] [PubMed] [Google Scholar]


