Abstract
Background:
Hoffa fractures are coronal-plane fractures of the femoral condyle, which are rarer than sagittal-plane condylar fractures. This study aimed to systematically review the clinical knowledge base of Hoffa fractures to facilitate the diagnosis and management of such injuries.
Methods:
We searched Medline, Embase, Cochrane Library, Google Scholar, China National Knowledge Infrastructure, and China Biology Medicine disc, using the terms “Hoffa fracture” and “coronal fracture of femoral condyle.”
Results:
One hundred five articles on Hoffa fractures were reviewed, and the clinical knowledge base was summarized. High-energy trauma is a common cause of a Hoffa fracture, although low-energy trauma and iatrogenic injury can also lead to these fractures. Commonly used classifications include the Letenneur classification, a computed tomography (CT) classification, the AO classification, and modified AO classification. Radiography can reveal fracture lines. If radiographic findings are negative in questionable cases, CT and magnetic resonance imaging (MRI) should be performed. Nondisplaced fractures can be managed conservatively; however, they involve a high risk of redisplacement. Open reduction and internal fixation are preferred. For young patients with good compliance, simple medial or lateral condylar fractures can be treated via a medial or lateral parapatellar approach. After fracture exposure, headless compression screws can be inserted perpendicularly to the fracture line from posterior to anterior. For bicondylar fractures, a median parapatellar incision can be used. For complex fractures in patients with osteoporosis or a high body mass index, cannulated screws with antigliding plate fixation should be used.
Conclusion:
Here, we summarized the injury mechanism, diagnosis, classification, and treatment options of Hoffa fractures.
Keywords: classification, diagnosis, Hoffa fracture, injury mechanism, treatment
1. Introduction
Fractures of the distal femur typically occur in the axial and sagittal planes.[1] A Hoffa fracture, a rare fracture confined to the coronal plane of either femoral condyle, accounts for 8.7% to 13% of distal femoral fractures.[2] This fracture type was 1st described by Busch in 1869.[3,4] In 1888, Hoffa described coronal fracture of the femoral condyle but did not indicate the source of the previous reference. Following Letenneur classification of coronal fractures of the femoral condyle in the 1970s and the publication of the second version of the “Manual of Internal Fixation,” the Hoffa fracture has become more widely recognized by orthopedists. With rapid developments in transportation, construction, and industry, the incidence of Hoffa fractures has gradually increased. This article reviews the mechanism, diagnosis, classification, and treatment of Hoffa fractures.
2. Method
Medline, Embase, the Cochrane Library, Google Scholar, the China National Knowledge Infrastructure, and the China Biology Medicine disc were searched for relevant articles. We used the key words “Hoffa fracture” and “coronal fracture of femoral condyle” for the knowledge. One hundred five relevant articles were reviewed, and the clinical knowledge base was summarized.
Our hospital's institutional review board waived the need for ethical approval for this review paper.
3. Injury mechanism
The main cause of a Hoffa fracture is a high-energy injury such as those sustained in traffic collisions (80.5% of cases) and falls (9.1% of cases).[5–9] For children and individuals with osteoporosis, low-energy trauma can also lead to a Hoffa fracture.[10] Werner and Miller[11] reported that iatrogenic injury is a cause of Hoffa fracture that cannot be ignored.
3.1. High-energy trauma
The specific mechanism of a Hoffa fracture is not well understood.[12,13] Most researchers[2,7,14] currently believe that when the knee is in ≥90° of flexion and emergency braking is performed while driving a car, an axial force in either a varus or valgus direction is transferred from the proximal femur to the femoral condyle. At the same time, forces on the distal tibia are transferred to the tibial plateau, resulting in great shear stress between the femoral condyle and the tibial plateau.[15,16] These forces cause gross displacement of the condyle, which can not only rupture the quadriceps tendon but also perforate the skin, resulting in an open injury. With a lower degree of knee flexion, the extensor mechanism is damaged below the patella (patellar tendon); at higher angles, the quadriceps tendon is torn. Furthermore, a Hoffa fracture is associated with cruciate ligament injury. In these cases, avulsion of the anterior cruciate ligament along with a large chunk of bone at its insertion[17] can lead to a Hoffa fracture. When high-energy trauma involves the distal femur, the lateral condyle is often damaged[18] before the medial condyle because of the physiologic genu valgum of the knee joint.[19] Therefore, lateral condyle fracture is significantly more common than medial condyle fracture.[15,17–20] The fracture line its inclination angle of a Hoffa fracture depend on the degree of knee joint flexion at the time of trauma[18]; as the angle of knee flexion increases, the fracture line will occur farther from the posterior cortex of the femoral-condyle.[21] In contrast to unicondylar Hoffa fracture, a bicondylar Hoffa fracture is caused by a posterior and upward directed force and is not associated with knee valgus.[21,22]
In some patients, a Hoffa fracture is associated with a patellar fracture. In these cases, the associated patellar fracture results from a combination of forces: direct trauma causing the Hoffa fracture and possible indirect injuries from sudden contraction of the quadriceps muscle causing a vertical patellar fracture.[23]
3.2. Low-energy trauma
Low-energy trauma can cause Hoffa fractures in people with skeletal immaturity[24] as well as in those with low bone mass, such as patients with osteoporosis.[10] Some of these patients may have a history of poliomyelitis that predisposes individuals to osteoporosis.[25] Loss of bone matrix results in brittle, weaker bones that break rather than bend with external force. In addition to changes in bone mineral composition and a reduced proportion of bone matrix in patients with osteoporosis, changes in bone microstructure, thinning of bone cortex, and reduction in the number and size of bone trabeculae result in a decreased bone load capacity[26] and an increased risk of a Hoffa fracture with low-energy trauma.
3.3. Iatrogenic injury
Reconstruction of the anterior cruciate ligament of the knee joint can lead to iatrogenic Hoffa fracture. In anterior cruciate ligament reconstruction, an anterior medial approach to the femoral tunnel allows restoration of the position of the tendon graft and increases rotation stability when an expanded bone tunnel is used for the graft. However, if the tunnel is too close to the distal femoral articular surface and too little cartilage-covered bone is retained, either the passage of the tendon through the bone tunnel or fixation of the tendon can lead to a Hoffa fracture.[11] The presence of a thick ligament in a relatively small femur is also a risk factor for a Hoffa fracture.[27–30]
4. Classification of Hoffa fracture
The Letenneur classification, computed tomography (CT) classification, the AO classification, and the AO classification with supplement are widely used in clinics to categorize Hoffa fractures.
4.1. Letenneur classification
The widely known Letenneur classification not only clarifies the relationships between the fracture line and ligaments and soft tissue, but also has significance for clinical treatment and prognosis. The Letenneur classification[31] divides fractures into 3 types (Fig. 1). Type I, the most common classification, is a vertical fracture line parallel to the posterior cortex of the femur and involves the entire condyle. Fracture lines are often located where the anterior cruciate ligament and lateral collateral ligaments attach. In these fractures, the popliteus tendon and the lateral head of the gastrocnemius muscle remain attached to the fragment. Type II is a fracture horizontal to the base of the posterior condyle with fracture lines located posterior to the attachment point of the lateral collateral ligament. Type III is an oblique fracture of the femoral condyle with the fracture line located anterior to the joint capsule, anterior cruciate ligament, lateral collateral ligament, popliteal tendon, and the lateral head of the gastrocnemius muscle. Types I and III Hoffa fractures usually have a good prognosis because the soft tissue remains attached to the fragment, ensuring an adequate blood supply. In contrast, type II fractures have a high risk of nonhealing or delayed healing because of poor adhesion and poor blood supply. However, Gavaskar et al[2] argued that no evidence confirms this correlation.
Figure 1.
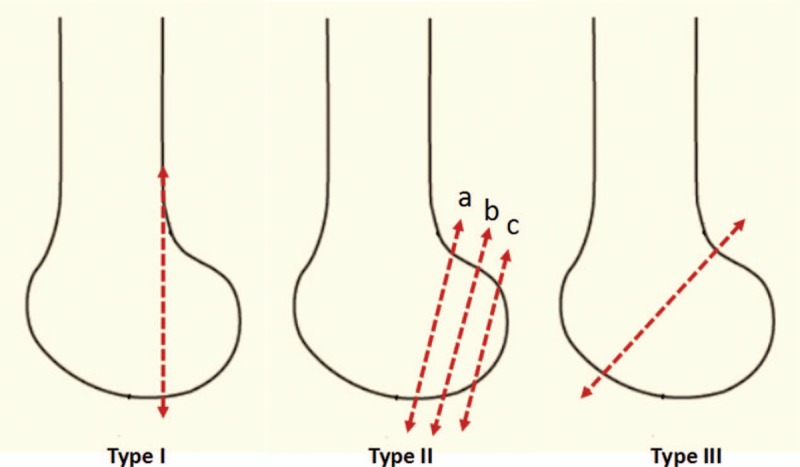
Letenneur classification of Hoffa fracture. The dotted lines represent fracture lines. In Type II fracture, the dotted lines are horizontal to the base of the posterior condyle. For fractures located posterior to dotted line a, the popliteal tendon or gastrocnemius muscle attached to the fragment. For those located posterior to dotted line b, only a part of popliteal tendon or gastrocnemius muscle attached to the fragment. There is no soft tissue attachment to the fracture fragments located posterior to dotted line c.
4.2. CT classification
The CT classification[32] uses the anatomic femoral axis and a line parallel to the posterior cortex of the femoral condyle to divide the femoral condyle into a, b, and c regions. Three types of fracture are defined based on the coronal fracture line (Fig. 2). For example, a fracture line dividing the femoral condyle surface into 2 parts is classified as type I; 2 fracture lines dividing the femoral condyle surface into 3 parts is type II; and 3 or more fracture lines dividing the femoral condyle surface into 4 or more parts is type III. This system allows the classification of comminuted femoral condyle fractures.
Figure 2.
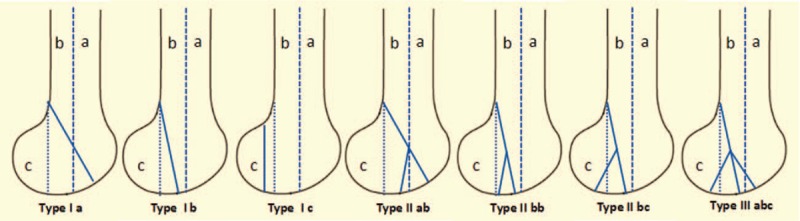
Computed tomography classification of Hoffa fracture. The anatomical femoral axis (the right dotted line) and the line parallel to the posterior cortex of the femoral condyle (the left dotted line) divided the femoral condyle into three regions (a region locates anterior to the right dotted line; b region locates between both dotted lines and c region locates posterior the left dotted line). The solid line represents fracture line.
4.3. AO classification and supplement
In the AO classification, Hoffa fracture is classified as type B3.2.[33] Dua and Shamshery[34] proposed a classification method that supplements the AO classification with proper surgical planning to optimize outcomes. In the type I, an isolated fracture is confined to the coronal plane of 1 condyle (medial or lateral). Two or 3 cancellous screws (4 or 6.5 mm) can be used to fix the fracture in an anterior-to-posterior direction. In the type II (bicondylar Hoffa fracture), both condyles are fixed with anteroposterior screws. Medial and lateral buttressing may be required if either fracture extends proximally in the same plane. In types III and IV (unicondylar coronal plane fracture with supracondylar or intercondylar distal femoral fractures, respectively), fixation is needed as for isolated Hoffa fracture in addition to stabilization with a metaphyseal bridging implant or a fixed-angle device.
5. Diagnosis
Making the diagnosis of a Hoffa fracture is challenging.[34] The clinical diagnosis of a Hoffa fracture relies on trauma history, physical examination, imaging, and other objective indicators as well as increased suspicion based on the history and positive signs.[35,36]
5.1. Medical history and local examination
Hoffa fractures are most commonly caused by traffic accidents, especially motorcycle accidents.[12,37] Orthopedic surgeons treating these patients should be vigilant in diagnosing a Hoffa fracture; patients with undiagnosed injuries experience long-term knee pain and limited knee mobility.[10,38] Local manifestations of a Hoffa fracture include knee swelling, pain, skin color changes (with or without skin defects), limited knee mobility, and a positive floating patella test.[7,10] The finding of medial or lateral stress test and anterior and posterior drawer test were reported to be positive in some patients.[39,40] Wagih[41] reported that, under general anesthesia, patients with Hoffa fracture have instability at 30° of flexion but not with leg straightened.
5.2. Imaging examination
A radiographic examination should include anteroposterior, lateral, oblique, and stress views of the knee. In the anteroposterior radiograph of the femoral condyle, the trabecular bone structure of the femoral condyles is disordered, with poor continuity of the cortex. On lateral radiographs, the normal femoral condyles overlap, and bone cortex interruption may not be visible.[7] Nondisplaced Hoffa fractures are difficult to visualize on anterior and lateral radiographs of the knee.[42] Compared with anteroposterior and lateral films, oblique radiographic views can show minimally displaced fractures better[14] and can, therefore, be used as a routine examination method for a Hoffa fracture. In addition, the Hoffa fracture line can be seen on stress films taken with the patient under general anesthesia.[43] If radiographic examination is not diagnostic but a Hoffa fracture is suspected, a CT scan, which is the gold standard for diagnosis of a Hoffa fracture, should be performed.[17,18] Magnetic resonance imaging (MRI) should be performed when injury is suspected to the meniscus, cruciate ligament, collateral ligament, or other soft tissues to determine the extent of injury,[32] develop appropriate surgical plans, and accurately assess prognosis.
5.3. Misdiagnosis
A high-energy injury resulting in a Hoffa fracture of the medial condyle is often associated with a tibia fracture,[18] a bicondylar Hoffa fracture,[44,45] a dislocation of the patella,[14] a knee dislocation,[46] intercondylar and supracondylar fractures,[9,47] and pelvic[48,49] and femoral shaft fractures.[50,51] An open supracondylar- intercondylar distal femoral fracture has a 2.8 times more chance of a Hoffa fracture than a closed distal femoral fracture.[9] The pain due to these combined injuries often exceeds that caused by the Hoffa fracture, which can lead physicians to miss the latter.[52] This fact reminds us that a Hoffa fracture evaluation should be a routine part of the lower-limb and pelvis examination with or without injury.[53] In addition, partial nondisplaced Hoffa fractures are difficult to diagnose on anteroposterior and lateral views of the knee because the fracture lines often overlaps the side or lateral condyle, which can result in a missed diagnosis in as many as 30% of cases.[9,18]
6. Treatment
6.1. Conservative treatment
Nondisplaced Hoffa fractures can be treated with cylindrical plaster cast immobilization with the knee in 10° of flexion.[54] However, popliteal and gastrocnemius muscle traction and foot or ankle movement can lead to fracture redisplacement,[55–57] which can cause delayed fracture healing, nonunion, traumatic arthritis, knee dysfunction, and other complications.[6,45,48,58–63] Therefore, we must strictly control the indications for conservative treatment.
6.2. Surgical treatment
Anatomic reduction of the articular surface, stable fixation, and early mobilization should be the aims of treatment.[64] Open reduction and internal fixation is the 1st choice for the treatment of displaced Hoffa fractures, and it is also suitable for the treatment of nondisplaced Hoffa fractures. The knee joint is placed in flexion during surgery,[65,66] placing the joint capsule and gastrocnemius in a relaxed state, which reduces the traction on the fracture and is conducive to fracture repair. The appropriate surgical plan is chosen based on the location of the Hoffa fracture, characteristics of the fracture line, fracture severity, and associated injuries.
6.3. Surgical approach
An appropriate surgical approach allowing full fracture exposure is selected based on fracture type. For simple lateral condylar Hoffa fractures, a patellar anterolateral approach is most commonly used. This approach fully exposes the fracture and does not risk damaging the nerves and blood vessels,[67] making the operation simple and safe. A lateral incision plus Gerdy tubercle osteotomy provides full exposure[68] especially in cases of coronal fracture of the lateral condyle. This approach can also be used to treat comminuted fractures or complex Hoffa fractures.[18]
For simple fractures of the medial condyle, a medial parapatellar surgical approach is most commonly used. The advantage of this approach is that it does not compromise future arthroplasty surgery; however, it does not allow visualization and treatment of any posterior comminution.[5] Viskontas et al[69] reported an extensile medial subvastus approach that allows better exposure of the surgical field and protects the blood supply of the bones comparing with the medial parapatellar approach. Gao et al[70] reported a “medial to medial-posterior distal femur approach” in which the fragments were exposed through the interval space between the gracilis muscle and medial head of the gastrocnemius and the medial collateral ligament can be clearly exposed and protected.
For bicondylar Hoffa fractures, it is necessary to simultaneously expose both condyles[71] to allow proper reduction. Lee et al[13] reported that Gerdy osteotomy combined with an anterior lateral parapatellar approach provides appropriate exposure for bicondylar Hoffa fractures. Fixation with an anti-glide plate on the lateral condyle and tibial osteotomy with two 4.5-mm screws is ideal. A swashbuckler approach[34,72] can be used to treat bicondylar Hoffa fractures because it protects the Quadriceps femoris abdomen during surgery, allowing quick postoperative recovery of muscle strength and range of motion.[73] This approach is suitable for the treatment of Hoffa fracture with patella dislocation.
Among the various types of Hoffa fractures, the Letenneur II is unique because the fragments are small and difficult to fix, and poor blood supply to the fragments impairs its healing. Kapoor et al[74] recommended a direct posterior approach and a lazy S-shaped incision to expose the fracture. In some cases, the Letenneur II fragment is small but essential for the knee join when flexed at 90° because it ensures the articular surface integrity. This method is beneficial for reducing small and rotating fragments. Tan et al[75] recommended an improved posterolateral approach starting from the space between the peroneal nerve and the biceps femoris. The risk of blood vessel damage when using this approach is minimal but the common peroneal nerve should be isolated first.
6.4. Surgical considerations
For Letenneur II and some Letenneur III fractures close to the posterior cortex of the femoral condyle, cannulated lag screw fixation is commonly used. The exposed fracture line is initially fixed with a k-wire and screws are placed perpendicular to the fracture surface. The use of several 3.5-mm-diameter screws is recommended to fix the fractures. A biomechanical study[5] shown that several smaller-diameter screws cause less damage to the joint cartilage than larger-diameter screws but that both have the same tensile force.[76,77] Fixation with 2 or more screws can prevent rotation and rotational displacement.[78] Previous studies showed the use of many screws to fix the Hoffa fracture, such as cancellous, cannulated, and headless used in a lag technique. Cancellous screws cannot achieve adequate compression[55] and require more surgical time to countersink. Headless compression screws are self-compressing and can be positioned beneath the outer cortex resulting in significantly greater axial compression, a higher load limit, and increased fracture stability.[65,67] Moreover, headless compression screws can prevent soft tissue irritation and do not need an additional countersinking procedure.[55] Onay et al[79] performed a long-term follow-up study of Hoffa fracture patients treated with screws and observed that the screws provided sufficient biomechanical stability until the fractures were healed. Somford et al[65] showed that the repair strength of absorbable screw fixation is weak, knee joint activity produces greater shear stress, and there is a risk of screw breakage; thus, careful selection of the surgical plan is recommended.
Screw insertion direction differs among operative approaches. Screws inserted from anterior to posterior induce less soft tissue dissection and carry no risk of damaging the posterior neurovascular structures.[80] From a biomechanical point of view, when the load is in the vertical direction, posteroanterior screw placement has a lower risk of shifting than anteroposterior placement.[2,77] The heads of screws placed through the articular cartilage are countersunk to prevent damage to the cartilage. Fixation with headless screws can reduce the degree of cartilage injury.[81] For patients who require a longer healing time, such as those with a higher body mass index or poor compliance, the simple application of a cannulated screw is insufficient to counter the great shearing force between condyles and the tibial plateau when the knee is in flexion.[25] A cannulated screw combined with a plate is recommended in these cases. This method is also recommended for patients with osteoporosis, metaphyseal extension, or comminuted Hoffa fractures.[82,83] A biomechanical study by Li et al[84] demonstrated that plates combined with screws more firmly fixed the femoral condyle, reducing the probability of fracture displacement. Lian and Zeng[85] and Zhao et al[86] treated Hoffa fracture patients with plates combined with screws and achieve good results. Based on plate position, screws can be combined with a lateral antigliding plate[84] or a posterior antigliding plate.[55,87]
Hoffa fractures are caused by shear stress between the femoral condyle and tibial plateau. According to the internal fixation principle, the antiglide plate should be fixed in the posterior position. However, the latest biomechanical study[88] showed that lateral antiglide plate has greater anti-shearing strength than posterior fixation. Moreover, the placement of a posterior antiglide plate with screws strips more soft tissue, especially the insertion of the gastrocnemius heads, and may destroy the blood supply to the fragments. In addition, the lateral antiglide plate can provide stable support, and in combination with autologous bone grafting can promote fracture healing,[38,55,89] which is especially useful for treating old Hoffa fractures.
Hoffa fracture with cruciate ligament, lateral collateral ligament, or meniscus injuries can be treated with arthroscopic surgery,[90] which has the advantages of minimal invasion, less of an effect on blood supply, early postoperative return to functional exercise, and effective prevention of nonunion and joint stiffness.[53,91] However, some Hoffa fractures combined with a tear of the posterolateral horn of the lateral meniscus are identified intraoperatively, and tear of the lateral meniscus can be repaired with suture anchors. Suture anchors are drilled into the posterolateral tibia to repair the meniscus to the meniscosynovial junction.[92] Moreover, if soft tissue embedded within the fracture line prevents reduction, arthroscopy can distinguish the tissues and the degree of damage to assist restoration.[93] The biggest challenge in the treatment of Hoffa fractures under arthroscopy due to the patella is dissecting the fragments for reduction[94] and placing screws perpendicularly into the fracture line.[95] Because Hoffa fractures are intra-articular, the success of anatomical reduction and firm internal fixation is closely related to postoperative complications like traumatic arthritis. Therefore, further studies are needed to improve the quality of Hoffa fracture reduction under arthroscopy.
Lax patellar attachments are thought to place adolescent boys at higher risk of patellar dislocation.[96,97] Thus, closed reduction is recommended when Hoffa fracture is accompanied by patella dislocation. A patella that is stuck between the tibia and femur can be relocated naturally by flexing of the hip joint with the knee in 110° of flexion under local anesthesia. Some patellar dislocations are difficult to treat with closed reduction because the patella is attached to the intercondylar fossa by the quadriceps femoris[98] and rotational or vertical displacement is present. Valgus strain on the knee and the continuous pull of the quadriceps causes the patella to ride against the femoral condyle, resulting in rotation around its vertical axis.[99] The patella may become incarcerated in the intercondylar fossa, wedged between the femoral condyles, or even rarely incarcerated in the Hoffa fracture. In such cases, the forces necessary for closed reduction can result in cartilage injury or a small avulsion fracture of the patella.[100,101] To avoid damaging the cartilage in these cases, it is important to reduce the patella early and restore the patellofemoral joint stability by repairing the damaged medial soft tissues.[102] Therefore, open reduction and internal fixation is recommended to minimize cartilage damage and allow appropriate treatment of the bone and soft tissues. Tsai et al[103] reported that surgical treatment is the 1st choice for Hoffa fracture accompanied by traumatic patella dislocation; if conservative treatment is adopted, the redislocation rate is as high as 40%.[104] To prevent habitual patellar dislocation, repair of the medial retinaculum complex or a combination of lateral retinacular release[14,105] and simultaneous patellar ligament insertion on the tibial tubercle is recommended. For tibial fractures, the use of bone plates or intramedullary nails is recommended if the condition of the local soft tissue is suitable. For local soft-tissue injuries, external fixation can be used, but this may delay the time to mobility restoration and affect therapeutic efficacy.
6.5. Postoperative management
On The 1st postoperative day, the injured limb should be mobilized on a continuous passive motion device. Partial weight bearing with crutches is started at 6 to 8 postoperative weeks. Weight bearing is allowed with radiographic evidence of healing, which usually occurs by 10 weeks of the postoperative period.[55]
7. Summary
Improving the accuracy and timeliness of Hoffa fracture diagnosis and improving minimally invasive treatment outcomes remain the focus of orthopedic surgeons. Familiarity with the characteristics of Hoffa fracture on various imaging modalities and an understanding of the mechanism and likelihood of combined injuries contribute to the timely and accurate diagnosis of Hoffa fracture and avoiding misdiagnosis. According to the severity of Hoffa fracture and combined injuries, a reasonable treatment plan can be developed. Further improvements in arthroscopic-assisted reduction and other minimally invasive surgery technologies will help improve patient prognosis.
Author contributions
Funding acquisition: Wei Chen.
Project administration: Wei Chen.
Supervision: Qingxian Wang, Zhiyong Hou, Wei Chen.
Writing – original draft: Yabin Zhou.
Writing – review & editing: Ying Pan.
Footnotes
Abbreviations: CT = computed tomography, MRI = magnetic resonance imaging.
YZ and YP contributed equally to this work.
This study was supported by the National Natural Science Foundation of China (grant no: 81401789) and the Top Young Talents for Hebei Province (2016–2018). The funding sources have no role in study design, literature collection, review, data analysis, and manuscript preparation.
The authors have no conflicts of interest to disclose.
References
- [1].Kumar R, Malhotra R. The Hoffa fracture: three case reports. J Orthop Surg 2001;9:47–51. [DOI] [PubMed] [Google Scholar]
- [2].Gavaskar AS, Tummala NC, Krishnamurthy M. Operative management of Hoffa fractures--a prospective review of 18 patients. Injury 2011;42:1495–8. [DOI] [PubMed] [Google Scholar]
- [3].Bartonicek J, Rammelt S. History of femoral head fracture and coronal fracture of the femoral condyles. Int Orthop 2015;39:1245–50. [DOI] [PubMed] [Google Scholar]
- [4].Heuschen UA, Gohring U, Meeder PJ. Bilateral Hoffa fracture--a rarity. Aktuelle Traumatol 1994;24:83–6. [PubMed] [Google Scholar]
- [5].Arastu MH, Kokke MC, Duffy PJ, et al. Coronal plane partial articular fractures of the distal femoral condyle: current concepts in management. Bone Joint J 2013;95-B:1165–71. [DOI] [PubMed] [Google Scholar]
- [6].Zeebregts CJ, Zimmerman KW, ten Duis HJ. Operative treatment of a unilateral bicondylar fracture of the femur. Acta Chir Belg 2000;100:104–6. [PubMed] [Google Scholar]
- [7].White EA, Matcuk GR, Schein A, et al. Coronal plane fracture of the femoral condyles: anatomy, injury patterns, and approach to management of the Hoffa fragment. Skeletal Radiol 2015;44:37–43. [DOI] [PubMed] [Google Scholar]
- [8].Cheng PL, Choi SH, Hsu YC. Hoffa fracture: should precautions be taken during fixation and rehabilitation? Hong Kong Med J 2009;15:385–7. [PubMed] [Google Scholar]
- [9].Nork SE, Segina DN, Aflatoon K, et al. The association between supracondylar-intercondylar distal femoral fractures and coronal plane fractures. J Bone Joint Surg Am 2005;87:564–9. [DOI] [PubMed] [Google Scholar]
- [10].Mootha AK, Majety P, Kumar V. Undiagnosed Hoffa fracture of medial femoral condyle presenting as chronic pain in a post-polio limb. Chin J Traumatol 2014;17:180–2. [PubMed] [Google Scholar]
- [11].Werner BC, Miller MD. Intraoperative Hoffa fracture during primary ACL reconstruction: can hamstring graft and tunnel diameter be too large? Arthroscopy 2014;30:645–50. [DOI] [PubMed] [Google Scholar]
- [12].Goel A, Sabat D, Agrawal P. Arthroscopic-assisted fixation of Hoffa fracture: a case report and description of technique. J Clin Orthop Trauma 2016;7:61–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Lee SY, Niikura T, Iwakura T, et al. Bicondylar hoffa fracture successfully treated with headless compression screws. Case Rep Orthop 2014;2014:139897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kondreddi V, Yalamanchili RK, Ravi Kiran K. Bicondylar Hoffa's fracture with patellar dislocation - a rare case. J Clin Orthop Trauma 2014;5:38–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Flanagin BA, Cruz AI, Medvecky MJ. Hoffa fracture in a 14-year-old. Orthopedics 2011;34:138. [DOI] [PubMed] [Google Scholar]
- [16].Cheng S, Zaidi SF, Linnau KF. ASER Core Curriculum Illustration Project: coronal femoral condyle (Hoffa) fracture. Emerg Radiol 2015;22:337–8. [DOI] [PubMed] [Google Scholar]
- [17].Bali K, Mootha AK, Krishnan V, et al. A rare case of bicondylar Hoffa fracture associated with ipsilateral tibial spine avulsion and extensor mechanism disruption. Chin J Traumatol 2011;14:253–6. [PubMed] [Google Scholar]
- [18].Jain A, Aggarwal P, Pankaj A. Concomitant ipsilateral proximal tibia and femoral Hoffa fractures. Acta Orthop Traumatol Turc 2014;48:383–7. [DOI] [PubMed] [Google Scholar]
- [19].Sharath RK, Gadi D, Grover A, et al. Operative treatment of isolated bicondylar Hoffa fracture with a modified Swashbuckler approach. Arch Trauma Res 2015;4:e25313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Federlin M, Krifka S, Herpich M, et al. Partial ceramic crowns: influence of ceramic thickness, preparation design and luting material on fracture resistance and marginal integrity in vitro. Oper Dent 2007;32:251–60. [DOI] [PubMed] [Google Scholar]
- [21].Ul Haq R, Modi P, Dhammi I, et al. Conjoint bicondylar Hoffa fracture in an adult. Indian J Orthop 2013;47:302–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Calmet J, Mellado JM, Garcia Forcada IL, et al. Open bicondylar Hoffa fracture associated with extensor mechanism injury. J Orthop Trauma 2004;18:323–5. [DOI] [PubMed] [Google Scholar]
- [23].Marzouki A, Zizah S, Benabid M, et al. A rare case of unicondylar medial Hoffa fracture associated with ipsilateral vertical patella fracture. J Clin Orthop Trauma 2013;4:102–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Potini VC, Gehrmann RM. Intra-articular dislocation of the patella with associated hoffa fracture in a skeletally immature patient. Am J Orthop 2015;44:E195–8. [PubMed] [Google Scholar]
- [25].Chang JJ, Fan JC, Lam HY, et al. Treatment of an osteoporotic Hoffa fracture. Knee Surg Sports Traumatol Arthrosc 2010;18:784–6. [DOI] [PubMed] [Google Scholar]
- [26].Wu P, WB, Kong LC, et al. Oral application of Qiangguyin Keli and alendronate sodium vitamin D3 tablets in postoperative anti-osteoporosis treatment in patients with primary osteoporotic hip fractured. J Trad Chin Orthop Trauma 2016;05:4. [Google Scholar]
- [27].Dave LY, Nyland J, Caborn DN. Knee flexion angle is more important than guidewire type in preventing posterior femoral cortex blowout: a cadaveric study. Arthroscopy 2012;28:1381–7. [DOI] [PubMed] [Google Scholar]
- [28].Gelber PE, Erquicia J, Abat F, et al. Effectiveness of a footprint guide to establish an anatomic femoral tunnel in anterior cruciate ligament reconstruction: computed tomography evaluation in a cadaveric model. Arthroscopy 2011;27:817–24. [DOI] [PubMed] [Google Scholar]
- [29].Busam ML, Provencher MT, Bach BR. Complications of anterior cruciate ligament reconstruction with bone-patellar tendon-bone constructs: care and prevention. Am J Sports Med 2008;36:379–94. [DOI] [PubMed] [Google Scholar]
- [30].Rue JP, Busam ML, Detterline AJ, et al. Posterior wall blowout in anterior cruciate ligament reconstruction: avoidance, recognition, and salvage. J Knee Surg 2008;21:235–40. [DOI] [PubMed] [Google Scholar]
- [31].Letenneur J, Labour PE, Rogez JM, et al. Hoffa's fractures. Report of 20 cases [in French]. Ann Chir 1978;32:213–9. [PubMed] [Google Scholar]
- [32].Li WH, LY, Wang MY. Hoffa fracture: the CT classification system. Chin J Orthop Trauma 2013;09:5. [Google Scholar]
- [33].Fracture and dislocation compendium: Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma 1996;10Suppl 1:1–54. [PubMed] [Google Scholar]
- [34].Dua A, Shamshery PK. Bicondylar Hoffa fracture: open reduction internal fixation using the swashbuckler approach. J Knee Surg 2010;23:21–4. [DOI] [PubMed] [Google Scholar]
- [35].Sasidharan B, Shetty S, Philip S, et al. Reconstructive osteotomy for a malunited medial Hoffa fracture - a feasible salvage option. J Orthop 2016;13:132–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Dhillon MS, Mootha AK, Bali K, et al. Coronal fractures of the medial femoral condyle: a series of 6 cases and review of literature. Musculoskelet Surg 2012;96:49–54. [DOI] [PubMed] [Google Scholar]
- [37].Xu Y, Li H, Yang HH, et al. A comparison of the clinical effect of two fixation methods on Hoffa fractures. Springerplus 2016;5:1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Jiang YR, Wang ZY, Zhang DB, et al. Twenty-seven-year nonunion of a Hoffa fracture in a 46-year-old patient. Chin J Traumatol 2015;18:54–8. [DOI] [PubMed] [Google Scholar]
- [39].Nandy K, Raman R, Vijay RK, et al. Non-union coronal fracture femoral condyle, sandwich technique: a case report. J Clin Orthop Trauma 2015;6:46–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ercin E, Bilgili MG, Basaran SH, et al. Arthroscopic treatment of medial femoral condylar coronal fractures and nonunions. Arthrosc Tech 2013;2:e413–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Wagih AM. Arthroscopic management of a posterior femoral condyle (Hoffa) fracture: surgical technique. Arthrosc Tech 2015;4:e299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Allmann KH, Altehoefer C, Wildanger G, et al. Hoffa fracture--a radiologic diagnostic approach. J Belge Radiol 1996;79:201–2. [PubMed] [Google Scholar]
- [43].Sahu RL, Gupta P. Operative management of Hoffa fracture of the femoral condyle. Acta Med Iran 2014;52:443–7. [PubMed] [Google Scholar]
- [44].Lal H, Bansal P, Khare R, et al. Conjoint bicondylar Hoffa fracture in a child: a rare variant treated by minimally invasive approach. J Orthop Traumatol 2011;12:111–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Papadopoulos AX, Panagopoulos A, Karageorgos A, et al. Operative treatment of unilateral bicondylar Hoffa fractures. J Orthop Trauma 2004;18:119–22. [DOI] [PubMed] [Google Scholar]
- [46].Shetty GM, Wang JH, Kim SK, et al. Incarcerated patellar tendon in Hoffa fracture: an unusual cause of irreducible knee dislocation. Knee Surg Sports Traumatol Arthrosc 2008;16:378–81. [DOI] [PubMed] [Google Scholar]
- [47].Baker BJ, Escobedo EM, Nork SE, et al. Hoffa fracture: a common association with high-energy supracondylar fractures of the distal femur. AJR Am J Roentgenol 2002;178:994. [DOI] [PubMed] [Google Scholar]
- [48].Ozturk A, Ozkan Y, Ozdemir RM. Nonunion of a Hoffa fracture in an adult. Chir Organi Mov 2009;93:183–5. [DOI] [PubMed] [Google Scholar]
- [49].Thakar C. The Hoffa fracture--a fracture not to miss. Emerg Med J 2010;27:391–2. [DOI] [PubMed] [Google Scholar]
- [50].Miyamoto R, Fornari E, Tejwani NC. Hoffa fragment associated with a femoral shaft fracture. A case report. J Bone Joint Surg Am 2006;88:2270–4. [DOI] [PubMed] [Google Scholar]
- [51].Jain A, Agrawal P, Chadha M, et al. Hoffa fracture associated with femoral shaft and proximal tibial fractures: report of two cases. Chin J Traumatol 2012;15:367–9. [PubMed] [Google Scholar]
- [52].Gong YB, Li QS, Yang C, et al. Hoffa fracture associated with ipsilateral femoral shaft fracture: clinical feature and treatment. Chin J Traumatol 2011;14:376–8. [PubMed] [Google Scholar]
- [53].Akan K, Akgun U, Poyanli O, et al. Arthroscopy-assisted treatment of Hoffa fracture associated with ipsilateral femoral shaft, tibial eminence and Malgaigne fractures. Acta Orthop Traumatol Turc 2014;48:602–6. [DOI] [PubMed] [Google Scholar]
- [54].Mak W, Hunter J, Escobedo E. Hoffa fracture of the femoral condyle. Radiol Case Rep 2008;3:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Min L, Tu CQ, Wang GL, et al. Internal fixation with headless compression screws and back buttress plate for treatment of old Hoffa fracture. Chin J Traumatol 2014;17:79–83. [PubMed] [Google Scholar]
- [56].Smith EJ, Crichlow TP, Roberts PH. Monocondylar fractures of the femur: a review of 13 patients. Injury 1989;20:371–4. [DOI] [PubMed] [Google Scholar]
- [57].McCarthy JJ, Parker RD. Arthroscopic reduction and internal fixation of a displaced intraarticular lateral femoral condyle fracture of the knee. Arthroscopy 1996;12:224–7. [DOI] [PubMed] [Google Scholar]
- [58].Tripathy SK, Aggarwal A, Patel S, et al. Neglected Hoffa fracture in a child. J Pediatr Orthop B 2013;22:339–43. [DOI] [PubMed] [Google Scholar]
- [59].Lewis SL, Pozo JL, Muirhead-Allwood WF. Coronal fractures of the lateral femoral condyle. J Bone Joint Surg Br 1989;71:118–20. [DOI] [PubMed] [Google Scholar]
- [60].Manfredini M, Gildone A, Ferrante R, et al. Unicondylar femoral fractures: therapeutic strategy and long-term results. A review of 23 patients. Acta Orthop Belg 2001;67:132–8. [PubMed] [Google Scholar]
- [61].McDonough PW, Bernstein RM. Nonunion of a Hoffa fracture in a child. J Orthop Trauma 2000;14:519–21. [DOI] [PubMed] [Google Scholar]
- [62].Iwai T, Hamada M, Miyama T, et al. Intra-articular corrective osteotomy for malunited Hoffa fracture: a case report. Sports Med Arthrosc Rehabil Ther Technol 2012;4:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Koné S, Bana A, Touré SA, et al. Hoffa fracture of medial unicondylar and bilateral in a man: a rare case. Pan Afr Med J 2015;20:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Meyer C, Enns P, Alt V, et al. Difficulties involved in the Hoffa fractures [in German]. Unfallchirurg 2004;107:15–21. [DOI] [PubMed] [Google Scholar]
- [65].Somford MP, van Ooij B, Schafroth MU, et al. Hoffa nonunion, two cases treated with headless compression screws. J Knee Surg 2013;26Suppl 1:S89–93. [DOI] [PubMed] [Google Scholar]
- [66].Kini SG, Sharma M, Raman R. A rare case of open bicondylar Hoffa fracture with extensor mechanism disruption. BMJ Case Rep 2013;2013: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Tong W, Yang J, Xu PL, et al. Efficacy of multiple Acutrak hollow head compression screws in the treatment of Hoffa fractures. J Bone Joint Surg Chin 2014;7:422–5. [Google Scholar]
- [68].Liebergall M, Wilber JH, Mosheiff R, et al. Gerdy's tubercle osteotomy for the treatment of coronal fractures of the lateral femoral condyle. J Orthop Trauma 2000;14:214–5. [DOI] [PubMed] [Google Scholar]
- [69].Viskontas DG, Nork SE, Barei DP, et al. Technique of reduction and fixation of unicondylar medial Hoffa fracture. Am J Orthop 2010;39:424–8. [PubMed] [Google Scholar]
- [70].Gao M, Tao J, Zhou Z, et al. Surgical treatment and rehabilitation of medial Hoffa fracture fixed by locking plate and additional screws: a retrospective cohort study. Int J Surg 2015;19:95–102. [DOI] [PubMed] [Google Scholar]
- [71].Agarwal S, Giannoudis PV, Smith RM. Cruciate fracture of the distal femur: the double Hoffa fracture. Injury 2004;35:828–30. [DOI] [PubMed] [Google Scholar]
- [72].Starr AJ, Jones AL, Reinert CM. The “swashbuckler”: a modified anterior approach for fractures of the distal femur. J Orthop Trauma 1999;13:138–40. [DOI] [PubMed] [Google Scholar]
- [73].Lu J, Wang PC. Progress in diagnosis and treatment of Hoffa fracture. Chin J Trauma 2013;29:806–8. [Google Scholar]
- [74].Kapoor C, Merh A, Shah M, et al. A case of distal femur medial condyle Hoffa type II(C) fracture treated with headless screws. Cureus 2016;8:e802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Tan Y, Li H, Zheng Q, et al. A modified posterolateral approach for Hoffa fracture. Eur J Orthop Surg Traumatol 2014;24:1321–3. [DOI] [PubMed] [Google Scholar]
- [76].Westmoreland GL, McLaurin TM, Hutton WC. Screw pullout strength: a biomechanical comparison of large-fragment and small-fragment fixation in the tibial plateau. J Orthop Trauma 2002;16:178–81. [DOI] [PubMed] [Google Scholar]
- [77].Jarit GJ, Kummer FJ, Gibber MJ, et al. A mechanical evaluation of two fixation methods using cancellous screws for coronal fractures of the lateral condyle of the distal femur (OTA type 33B). J Orthop Trauma 2006;20:273–6. [DOI] [PubMed] [Google Scholar]
- [78].Ostermann PA, Neumann K, Ekkernkamp A, et al. Long term results of unicondylar fractures of the femur. J Orthop Trauma 1994;8:142–6. [DOI] [PubMed] [Google Scholar]
- [79].Onay T, Gülabi D, Çolak İ, et al. Surgically treated Hoffa Fractures with poor long-term functional results. Injury 2018;49:398–403. [DOI] [PubMed] [Google Scholar]
- [80].Singh R, Singh RB, Mahendra M. Functional outcome of isolated Hoffa fractures treated with cannulated cancellous screw. Malays Orthop J 2017;11:20–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Borse V, Hahnel J, Cohen A. Hoffa fracture: fixation using headless compression screws. Eur J Trauma Emerg Surg 2010;36:477–9. [DOI] [PubMed] [Google Scholar]
- [82].Soni A, Sen RK, Saini UC, et al. Buttress plating for a rare case of comminuted medial condylar Hoffa fracture associated with patellar fracture. Chin J Traumatol 2012;15:238–40. [PubMed] [Google Scholar]
- [83].Vivek T, Saubhik Da, Sahil G, et al. Analysis of functional outcome of Hoffa fractures: a retrospective review of 32 patients. J Orthop Surg 2017;25:1–7. [DOI] [PubMed] [Google Scholar]
- [84].Li WH, Li Y, Wang MY. Antigliding plating for Letenneur type I Hoffa fractures. Chin J Orthop Trauma 2009;9:850–3. [Google Scholar]
- [85].Lian X, Zeng YJ. Meta plate and cannulated screw fixation for treatment of type Letenneur III lateral Hoffa fracture through posterolateral approach [in Chinese]. Zhongguo Gu Shang 2018;267–71. [DOI] [PubMed] [Google Scholar]
- [86].Zhao LL, Tong PJ, Xiao LW. Internal fixation with lag screws plus an antigliding plate for the treatment of Hoffa fracture of the lateral femoral condyle. Zhongguo Gu Shang 2016;29:266–9. [PubMed] [Google Scholar]
- [87].Yin TL. Treatment of Hoffa fractures with internal fixation by compressive hollow screw combined with antigliding plate. Chin J Prac Med 2013;18:27–8. [Google Scholar]
- [88].Sun H, He QF, Huang YG, et al. Plate fixation for Letenneur type I Hoffa fracture: a biomechanical study. Injury 2017;48:1492–8. [DOI] [PubMed] [Google Scholar]
- [89].Singh AP, Dhammi IK, Vaishya R, et al. Nonunion of coronal shear fracture of femoral condyle. Chin J Traumatol 2011;14:143–6. [PubMed] [Google Scholar]
- [90].Wang JY, Liu Y, Li Y, et al. Arthroscopic-assisted fixation of Hoffa fracture by plate combined with screw. Chin J Orthop Trauma 2014;16:448–50. [Google Scholar]
- [91].Atesok K, Doral MN, Whipple T, et al. Arthroscopy-assisted fracture fixation. Knee Surg Sports Traumatol Arthrosc 2011;19:320–9. [DOI] [PubMed] [Google Scholar]
- [92].Egol KA, Broder K, Fisher N, et al. Repair of displaced partial articular fracture of the distal femur: the Hoffa fracture. J Orthop Trauma 2017;31:S10–1. [DOI] [PubMed] [Google Scholar]
- [93].Jain SK, Jadaan M, Rahall E. Hoffa's fracture - lateral meniscus obstructing the fracture reduction - a case report. Injury 2015;46:419–21. [DOI] [PubMed] [Google Scholar]
- [94].Biau DJ, Schranz PJ. Transverse Hoffa's or deep osteochondral fracture? An unusual fracture of the lateral femoral condyle in a child. Injury 2005;36:862–5. [DOI] [PubMed] [Google Scholar]
- [95].Ercin E, Baca E, Kural C. Arthroscopic treatment of isolated Hoffa fractures. J Knee Surg 2017;30:842–8. [DOI] [PubMed] [Google Scholar]
- [96].Frangakis EK. Intra-articular dislocation of the patella. A case report. J Bone Joint Surg Am 1974;56:423–4. [PubMed] [Google Scholar]
- [97].Choudhary RK, Tice JW. Intra-articular dislocation of the patella with incomplete rotation--two case reports and a review of the literature. Knee 2004;11:125–7. [DOI] [PubMed] [Google Scholar]
- [98].Nanda R, Yadav RS, Thakur M. Intra-articular dislocation of the patella. J Trauma 2000;48:159–60. [DOI] [PubMed] [Google Scholar]
- [99].Lowe M, Meta M, Tetsworth K. Irreducible lateral dislocation of patella with rotation. J Surg Case Rep 2012;2012:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Chauhan A. Irreducible, incarcerated vertical dislocation of the patella into a Hoffa fracture. Indian J Orthop 2015;49:369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Vaishya R, Singh AP, Dar IT, et al. Hoffa fracture with ipsilateral patellar dislocation resulting from household trauma. Can J Surg 2009;52:E3–4. [PMC free article] [PubMed] [Google Scholar]
- [102].Soraganvi PC, Narayan Gowda B, Rajagopalakrishnan R, et al. Irreducible, incarcerated vertical dislocation of patella into a Hoffa fracture. Indian J Orthop 2014;48:525–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Tsai CH, Hsu CJ, Hung CH, et al. Primary traumatic patellar dislocation. J Orthop Surg Res 2012;7:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Maenpaa H, Huhtala H, Lehto MU. Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand 1997;68:424–6. [DOI] [PubMed] [Google Scholar]
- [105].Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am 2008;90:463–70. [DOI] [PubMed] [Google Scholar]


