Abstract
Background:
Mild cognitive impairment (MCI) can be a stage of pre-dementia. Although the traditional Chinese exercise (TCE) has benefits associated with cognitive functions, the effects of the TCE on cognitive functions of older patients with MCI remain controversial. This study performs a meta-analysis to quantify the efficiency of TCE for older individuals on cognitive and psychological outcomes.
Methods:
A comprehensive database search was conducted on PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL (EBSCO), Web of Science, and four Chinese medical databases. We included trials published up to April 22, 2018, that fulfilled our inclusion and exclusion criteria. The literature was screened, the data were extracted and the methodological quality of the included trials was assessed. Meta-analyses were performed on the included data.
Results:
A total of 803 patients from 5 trials were included in our meta-analysis. Overall, there were no significant differences in global cognitive functions (P = .06), memory (P = .11), executive function (P = .74), Verbal fluency (P = .45) and depression (P = .89) between the TCE and the control groups. However, the TCE significantly improved the visuospatial function (SMD = 0.38, 95% CI = 0.22 to 0.54; P < .001) for individuals with MCI.
Conclusions:
The findings of this study suggested that the TCE was associated with significant improvement in visuospatial function but did not affect the global cognitive functions, depression and other specific cognitive domains. There is a lack of clear evidence for effects of TCE; further large, rigorously designed studies are needed.
Keywords: cognitive functions, meta-analysis, mild cognitive impairment, traditional Chinese exercise
1. Introduction
The prevalence of age-related changes in cognitive functions has steadily increased in recent decades. As a determining factor of functional disability,[1,2] the quality of cognitive functions has become a major public health concern. Nowadays, the world population of dementia is approximately 47.5 million, with 7.7 million new entrants each year. By 2030, these figures are projected to increase to 75.6 million and to 135.5 million in 2050.[3] Mild cognitive impairment (MCI) refers to the intermediate stage between the intact cognitive functioning and very early clinical dementia, which places older adults at high risk of developing dementia and contributes to increased functional disability, increased healthcare costs and decreased quality of daily-life activities.[4] Individuals with MCI are susceptible to experience diffidence, depression, anxiety and social isolation.[5] Therefore, effective treatments targeting improving cognitive health are critical for people with MCI by delaying progression to dementia.[3] However, some systematic reviews of randomized controlled trials (RCTs) suggest that there are no consensuses among medical scientists on any pharmacological treatment is recommended for MCI. Furthermore, the side effects of these drugs can cause gastro-intestinal disturbances even or unexplained increased mortality rate.[6–9] Hence, increasing advocacy of alternative medicine to maintain or enhance cognitive functions, and protect against the cognitive decline is in constant demand.[10]
Recent empirical meta-analysis has manifested that physical exercise has been investigated as a promising alternative therapy and prevents people with MCI from cognitive functions decline.[11] However, many types of physical exercise are either too intense or too monotonous, which makes it difficult for older adults to maintain long-term adherence and effective exercising.[12] Traditional Chinese exercise (TCE) is attracting worldwide attention due to tremendous benefits on health benefits, highly safe, no special equipment requirements and being easy to learn.[13] TCE was designed to improve the functional integrity of body and enhance the vitality of the energy called “Qi” and its history in the management of people with MCI has been over 2000 years.[14,15] TCE may be a reasonable adjunct to increase learning motivation and exercise persistence for those unable to engage in high intensity physical older people, because it provides light to moderate activity and strength training and the forms of TCE are various such as Tai chi, Qigong, Baduanjin, Liuzijue and so on.[16] Although certain trials on exercise programs in people with MCI have demonstrated that various forms of TCE may play positive roles on slowing down progression to dementia, yet there is also a demand for more data from further researches.[16,17] Although different types of TCE share the common traditional Chinese medicine theory focusing on a mind-body combination, each type has its unique feature. For example, Tai chi is a popular type of TCE among older people and based on yin-yang theory of traditional Chinese medicine. Tai chi exercise is characterized by gentle, graceful, smooth, coordinated and flowing movements of different body parts,[18] which make it an appropriate exercise supporting cognitive functions for older adults.[19] Furthermore, older Tai chi leaners engaging in a learning group and chatting with each other may have further benefits for cognition by enhancing mood and coping skills through social interactions and support from learning partners.[20]
Although a few systematic reviews have shown TCE and its positive role in individuals with stroke,[13] knee osteoarthritis,[18] cardiovascular diseases[14] and so on, whether TCE is more beneficial in improving cognitive functions in older patients with MCI than other exercise interventions or without treatment is presently vague. What's more, some different opinions indicated that TCE maybe make things worse because of its adverse effects.[21] Currently, there are no consensus has been reached about the benefits of TCE for the maintenance of cognitive and psychological outcomes. Hence, the objective of this systematic review is to summarize reliable evidence on the effects of TCE on cognitive and psychological outcomes, incorporate all available RCTs, and to investigate relevant subgroups. This systematic review would provide a scientific guidance for future researchers and clinicians to design effective mind-body exercise programs for boosting cognitive abilities in older people with MCI.
2. Methods
2.1. Search strategy
Relevant trials published from their inceptions to April 22, 2018 were obtained from the following databases: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL (EBSCO), Web of Science, the Chinese Biomedical Database (CBM), the China National Knowledge Infrastructure (CNKI), VIP Journal Integration Platform (from 1989), and Wanfang Med Online without language restriction. The full electronic search strategies for PubMed/MEDLINE were as follows:
-
1.
“Single-Blind Method” [Mesh] OR “Double-Blind Method” [Mesh] OR “Randomized Controlled Trials as Topic” [Mesh] OR “Randomized Controlled Trial” [Publication Type] OR “Intention to Treat Analysis” [Mesh] OR “Controlled Clinical Trials as Topic” [Mesh] OR “Clinical Trials as Topic” [Mesh] OR “Clinical Trial” [Publication Type] OR randomized controlled trial [Publication Type]
-
2.
“random∗” [Text Word] OR allocation [Text Word] OR “random allocation” [Text Word] OR placebo [Text Word] OR single blind [Text Word] OR double blind [Text Word] OR “randomized controlled trial∗” [Text Word] OR RCT [Text Word]
-
3.
1 OR 2
-
4.
animals NOT humans
-
5.
3 NOT 4
-
6.
Tai chi [Title/Abstract] OR “taiji∗” [Title/Abstract] OR qigong [Title/Abstract] OR liuzijue [Title/Abstract] OR Wuqinxi [Title/Abstract] OR yijinjing [Title/Abstract] OR baduanjin [Title/Abstract] OR “traditional exercise” [Title/Abstract] OR traditional Chinese medicine [Title/Abstract] OR “Chinese traditional exercise” OR “traditional Chinese exercise” OR “Chinese exercise”
-
7.
Alzheimer∗ [Title/Abstract] OR Alzheimer Disease OR AD [Title/Abstract] OR ”cognit∗ impair∗“[Title/Abstract] OR MCI [Title/Abstract] OR (AACI or memory or CIND or ARCD or ACMI) [Title/Abstract] OR (”N-MCI“ or ”A-MCI“ or ”M-MCI“) [Title/Abstract] OR (nMCI or aMCI or mMCI) [Title/Abstract] OR (CDR adj2 ”0.5”) [Title/Abstract]
-
8.
5 AND 6 AND 7
2.2. Inclusion criteria
-
1.
Types of studies. The RCTs were included without restriction of publication language, date or status. Theses and conference papers were excluded.
-
2.
Types of participants. The samples were older adults (≥ 60 years) with MCI. Individuals with MCI were identified by any available diagnostic criteria, such as Petersen criteria,[22] Mayo clinic criteria for amnestic mild cognitive impairment[17] and other standards and consensus. RCTs including participants with MCI for whom the cognitive deficits may be due to medical or neurological disorders (e.g., Alzheimer's disease, dementia and Parkinson's disease) were included.
-
3.
Types of interventions. Participants in the intervention groups had to have received TCE alone without other treatments. TCE including but not confined to Tai chi, Baduanjin, Qigong, Yijinjing, Liuzijue and Wuqinxi. Intervention format (individual/group), setting (community/hospital), duration, frequency were not restricted. Participants in the control group could undergo no intervention, usual care or other exercises that are different from TCE.
-
4.
Types of outcome measures. The primary outcome was global cognition functions. Secondary outcomes including 1) domain-specific cognition (e.g., memory, executive function). 2) depression.
2.3. Selection of studies
Two reviewers independently undertook a screen of titles, abstracts and full contents of all relevant records for inclusion in the review, according to the prespecified standards. Any discrepancies were settled by mutual consent. If disagreement persisted, a third author was asked to make the final decision.
2.4. Data extraction
Data were extracted by 2 authors from each article including: author, year, location, baseline participant characteristics, intervention and control, duration of treatment, outcome indicators and time point, using a standardized form. Similarly, disagreements between searchers concerning the eligibility of a trial were resolved by discussion or by consulting a third reviewer.
2.5. Quality assessment
We applied the Cochrane Risk of Bias tool[23] to evaluate the validity of the trials, focusing on sequence generation; allocation concealment; participant, personnel, and outcome assessor blinding; attrition bias; incomplete outcome data; selective outcome reporting; and other sources of bias. Two reviewers respectively judged these items as having an unclear, high or low risk of bias for each study.
2.6. Statistical analysis
If there were at least 2 trials reporting on the same outcome, the data were analyzed by a statistical meta-analysis using RevMan 5.3 software. When all trials assessed the same outcome using different scales or units, the standardized mean difference (SMD) and 95% confidence interval (CI) were present as the summary statistic for continuous data. Otherwise, the mean difference (MD) and 95% CI were used. Chi-square test and the calculating Higgins I2 values were used to determine heterogeneity. An I2 < 25% was considered to be low in statistical heterogeneity. At ∼50%, it means moderate statistical heterogeneity, and I2 > 50%, it means high statistical heterogeneity.[24] For trials with high heterogeneity (I2 > 50%), the outcome indicators were combined by a random-effects model to analysis. Otherwise a fixed-effects model was adopted.
Subgroup analyses were based on frequency, duration and geographic location of TCE to identify potential reasons for high heterogeneity. Sensitivity analysis was conducted by exclusion of each study one by one, in order to assess whether the results were stable. Potential publication bias was evaluated with a funnel plot if the group included 10 trials or more.
3. Results
3.1. Search results
Figure 1 shows the flow diagram of the screening process. A total of 877 potentially eligible records were identified in the initial literature search, 192 of which were duplicates. 661 records were removed by screening their titles and abstracts. After reviewing the full text of the records, a total of 5 records[17,22,25–27] satisfied the inclusion criteria and left in the final analysis.
Figure 1.
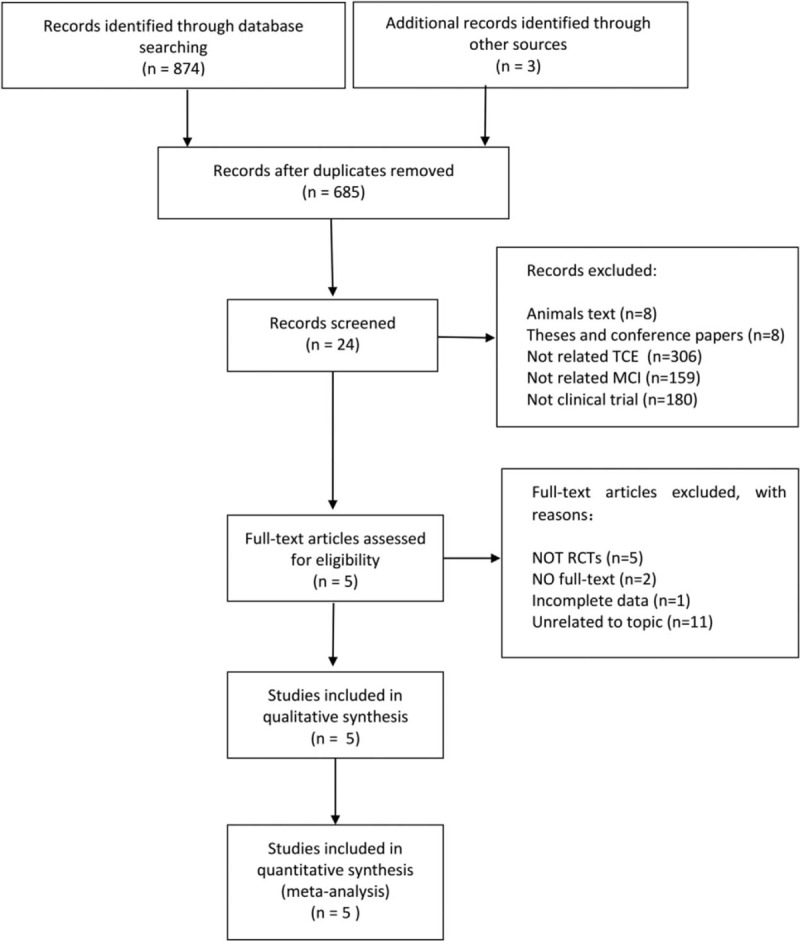
Flow chart showing the search results of the meta-analysis.
3.2. Study characteristics
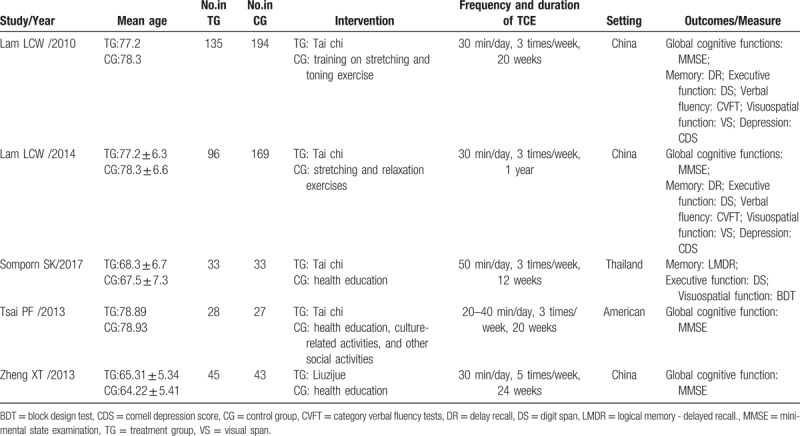
Table 1 presented study characteristics and patient demographic data of all RCTs included in this review. A total of 803 participants with cognitive impairment of mild severity (evaluated using Hoehn and Yahr stage) were covered in this review, consisting of 337 participants in the TCE group and 466 participants in the control group. One trial[27] were in Chinese, others[17,22,25,26] were in English. Trials originated from China (n = 3), the USA (n = 1) and Thailand (n = 1). Two types of exercise were used: Tai chi and Liuzijue. Of the included 5 trials, 4 adopted Tai chi,[17,22,25,26] 1 adopted Liuzijue,[27] that is widely practiced in China. TCE intervention programs (training duration ranged from 12 weeks to 1 year) varied from 20 to 50 minutes per day, 3 to 5 times weekly. The control group performed the usual physical activity and usual care, or very low intensity of activity/exercise such as relaxation exercises, stretching and toning exercise, culture-related activities and other social activities. Outcomes included global cognition functions, domain-specific cognition and depression.
Table 1.
Study Characteristics.
3.3. Quality of the evidence
Our judgments about each risk of bias domain are presented in Fig. 2. The generation of the allocation sequence was employed in all 5 trials,[17,22,25–27] and 3 trials[22,25,26] reported the allocation concealment methods. Only one trial[17] blinded the trainers, but outcome assessors who were blinded to allocation, were reported in 4 trials[17,22,25,26] (80%). In all 5 trials, 4 trials[17,22,25,26] (80%) used the intention-to-treat principle as their analysis method. With regard to selective reporting bias, we judged that expected outcomes were stated in all trials.
Figure 2.
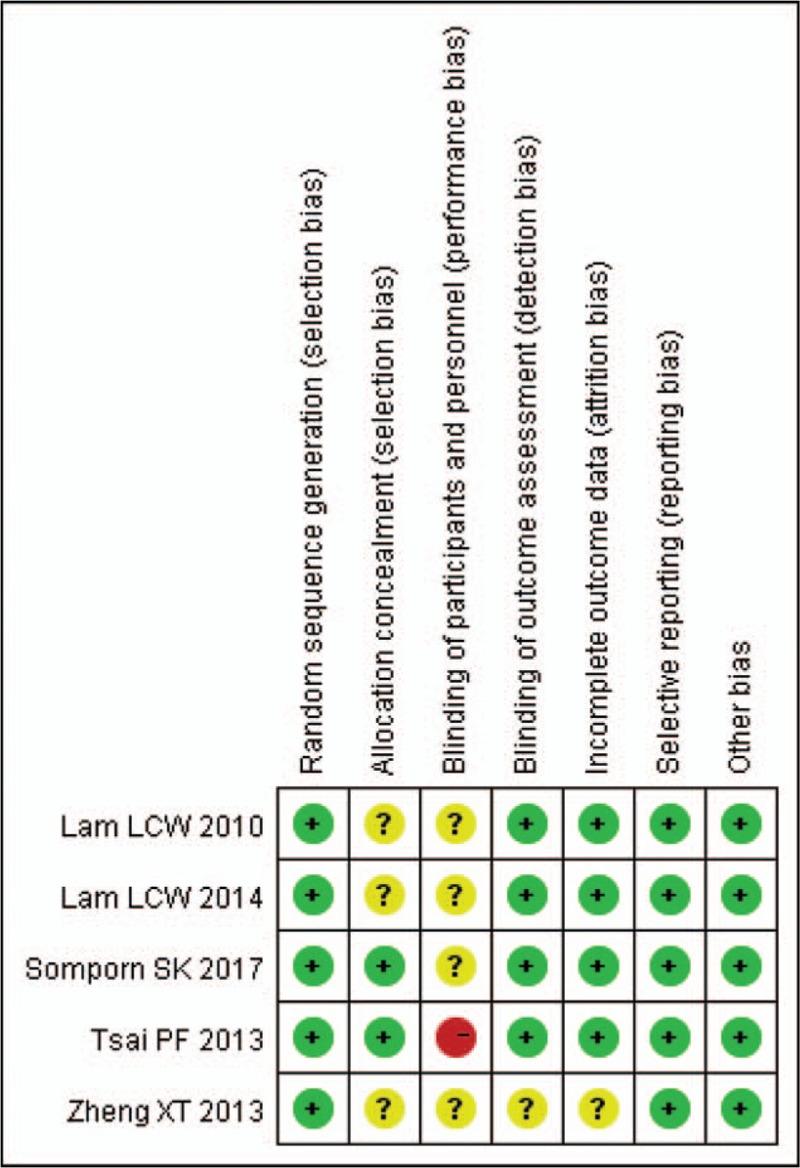
Risk of bias summary: review authors’ judgments about bias items for each included study.
3.4. Efficacy analysis
Global cognition functions, domain-specific cognition and depression were measured using various scales in the included articles. The change scores from baseline to final values were used in the final efficacy analysis.
3.4.1. Global cognition functions
737 participants in 4 trials[17,25–27] examined the effects of TCE on global cognition functions in older patients with MCI by using Mini-mental State Examination (MMSE) scores. Based on a fixed-effects model, the analysis revealed no significant effects of TCE for global cognition functions by raising MMSE scores (MD = 0.41, 95% CI = -0.01 to 0.84, P = .06; Fig. 3) with no substantial heterogeneity (I2 = 0%)
Figure 3.
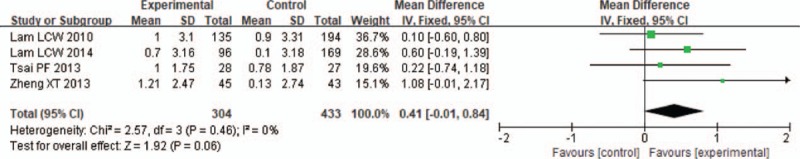
Forest plot for traditional Chinese exercise on global cognition functions.
3.4.2. Memory
Three trials[17,22,26] with data from 660 participants were included to assess the effects of the TCE on memory ability measured by 10-minute delayed recall (DC)[17,26] and Logical Memory - delayed recall (LMDC).[22] Hence SMD was used for data analysis. With a fixed-effects model, collated differences in memory ability after TCE revealed no difference between groups (SMD = 0.13, 95% CI = -0.03 to 0.28, P = .11; Fig. 4).
Figure 4.
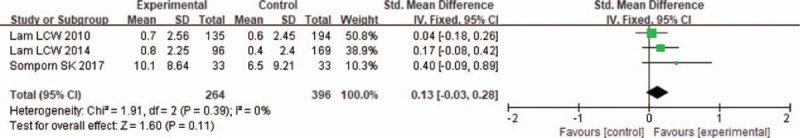
Forest plot for traditional Chinese exercise on memory.
3.4.3. Executive function
The complete Digit Span (DP)[17,22] or only the DP (backward)[26] was used to measure executive functions involving 660 patients. The collated differences from 3 trials[17,22,26] using a fixed-effects model revealed no evidence of a difference between groups (SMD = 0.03, 95% CI = -0.13 to 0.18, P = .74; Fig. 5).
Figure 5.
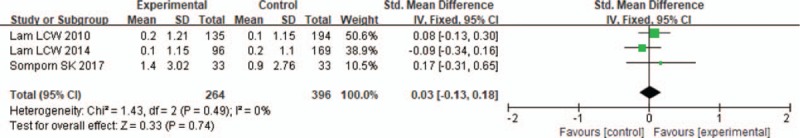
Forest plot for traditional Chinese exercise on executive function.
3.4.4. Verbal fluency
The effects of traditional Chinese exercise on verbal fluency using Category Verbal Fluency Tests (CVFT) was reported in 2 trials[17,26] with 594 patients, and data pooling indicated that no significant differences were found between the TCE and the control groups (MD = 0.47, 95% CI = -0.76 to 1.70, P = .45; Fig. 6) with a fixed-effects model.
Figure 6.
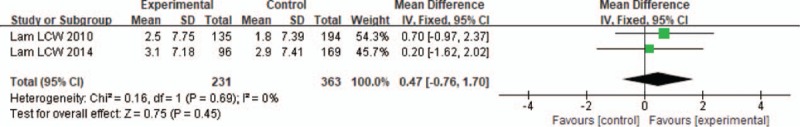
Forest plot for traditional Chinese exercise on verbal fluency.
3.4.5. Visuospatial function
Three trials in 660 patients with MCI assessed the effects of visuospatial function by Visual Span (VS)[17,26] and Block Design Test (BDT)[22]. The results showed significant effects of TCE (SMD = 0.38, 95% CI = 0.22 to 0.54, P < .001; Fig. 7) between groups based on a fixed-effects model.
Figure 7.
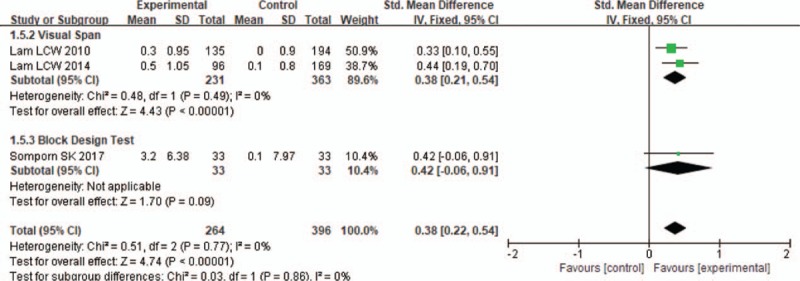
Forest plot for traditional Chinese exercise on visuospatial function.
3.4.6. Depression
The effects of depression were examined in 2 trials[17,26] containing 594 participants with Cornell Depression Score (CDS). Using a fixed-effects model, pooled results indicated significantly differences between the TCE and the control groups (MD = 0.02, 95% CI = −0.23 to 0.27, P = .89; Fig. 8).
Figure 8.
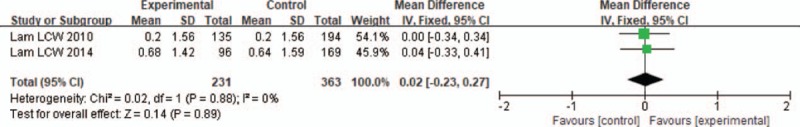
Forest plot for traditional Chinese exercise on depression.
3.5. Sensitivity analyses
A sensitivity analysis was conducted, excluding individual article one by one, to determine whether the results were stable. We found that except the outcomes of global cognition functions, the rest of the meta-analysis showed no substantial modification of the overall effect, suggesting that the outcome of global cognition functions was not stable, and the result should be interpreted with caution.
4. Discussion
To the best of our knowledge, this review is the first comprehensive synthesis of both English and Chinese language literature to ascertain the effects of TCE for improving cognitive function and depression of older individuals with MCI. Unlike prior systematic reviews[20] primarily focused more on either one type of TCE such as Tai chi, or one aspect of measures, our reviews evaluated a variety of other TCE interventions on both cognitive functions and psychological outcomes. In no cases, TCE has been associated with the adverse events in the context of improving cognition functions.
The aggregated result showed no significant benefit was found for TCE to improve global cognition functions in older individuals with MCI, as measured by MMSE scores. Thus, the results suggest that TCE produced no cognitive enhancement for individuals with MCI. This is inconsistent with the results of some single studies,[17,25] who reported that TCE might produce global cognitive enhancing effects in patients with MCI and therefore would be useful in global cognitive functions improvement. There is a similar systematic review[28] with regards to enhancing global cognitive functions in individuals following aerobic exercise, which also revealed significant improvements in global cognitive functions.
The mechanisms by which TCE might improve cognitive abilities in older adults with MCI is vague. However, it can be speculated that the following mechanism might be significant. TCE combined memorized, sequenced physical postures and movement with imagery, visualization, relaxation, and meditation, which can harmonize both physical activity and psychosocial health in older people with MCI.[3,29] And then, TCE could lead to impact on structures and functions of the central nervous system, such as increases of gray matter volume in prefrontal or medial temporal cortex and improvement of cerebral blood flow and oxygen delivery, as well as upregulation of brain-derived neurotrophic factor levels in older individuals with MCI.[30–32] This process significantly increases the establishment of brain neural networks, which may leads to increased cognitive functions.
Cognition is a complex concept that includes various sub-domains, such as memory, executive function, verbal fluency and so on.[33] Regarding the specific cognitive sub-domains, we found TCE had significant positive effects on visuospatial function. Although some publications have proposed relationship between TCE and specific cognitive domains in older adults with MCI, we identified no positive effects on memory, executive function and verbal fluency domains in this meta-analysis, which may be due to too few trials were pooled to evaluate the effects of TCE. In our meta-analysis and systematic review, the conclusions to assess the effects on specific cognitive sub-domains are from only 2 or 3 trials with small sample sizes. Therefore, the conclusions must remain uncertain.
There was also no significant improvement found in our meta-analysis and systematic review regarding depression parameter compared with the control group. Such non-significant findings are contrary to some published studies,[34] several factors such as insufficient required sample size, small number of eligible trials, intervention regimens, style of TCE adopted and the short follow-up periods may partly explain the lack of significant findings.
Our systematic review and meta-analysis included more applicable records via comprehensive literature search and critical appraisal. Also, we tried our best to improve the precision of the risk estimates with our strict inclusive criteria. What's more, we found no heterogeneity between the studies included in our systematic review and meta-analysis, which could reach statistical significance in meta-analysis. Consequently, the overall result of our systematic review is a widespread belief. There are also several limitations to our systematic review and meta-analysis should be acknowledged when attempting to make sense of the results. Firstly, and perhaps most notably, neither the sample size of treatment nor the methodological quality was poor to evaluate the effects. For example, only 3 of the included trials reported the allocation concealment in their experimental procedures, which may lead to selection bias or confounding of the final results. Moreover, it is impossible to blind patients in the TCE intervention group. Thus, performance bias may have been unavoidable. Secondly, there has been variability of interventions in the control group. Although most of the exercise in the control group were low intensity stretching exercise, some were just usual education or usual care. Given the variability of interventions in the control group, it was difficult to determine the effects of TCE intervention. Thirdly, although we searched trials from sufficient databases, most of the included trials were carried out in Chinese regions, which may result in a certain degree of selective bias. Finally, the publication bias were not conducted by funnel plot analysis on account of insufficient number of trials for each outcome. All of these limitations, and more, are very salient and require the clinician to use judgment in characterizing individuals with TCE to improve their cognitive functions. Our systematic review and meta-analysis showed that TCE training produces virtually no untoward effects and suggests that TCE could be a safe exercise for older adults with MCI. Nevertheless, it should be noted that several relevant issues need to be taken into account. Although several different types of TCE share the common traditional Chinese medicine theory, different training styles, training protocols, exercise doses, and qualifications of instructors may impact delivery and receipt of TCE. Further trials thus are urged to provide standardized exercise scheme and clear information that who took the role of the instructors. Moreover, even though it is difficult to blind subjects to some forms of interventions, using assessor blinding is important for the final result. Finally, more details such as sample size, long-term follow-up and drop-out rates were not sufficiently, researchers are urged to improve their methodological standards.
In conclusion, our systematic review and meta-analysis found that at least TCE can improve visuospatial function domain but has no effects on global cognitive functions, memory, executive function, verbal fluency domains and depression parameter. Future well-designed randomized trials with long-term follow-ups should help determine whether TCE provides cognitive benefits in older adults with MCI.
Author contributions
Conceptualization: Qi Zhang, Jianan Hu, Rui Cao, Ruishu Ma, Huimin Song, Yi Jin.
Data curation: Qi Zhang, Jianan Hu, Lijiao Wei, Yi Jin.
Formal analysis: Qi Zhang, Jianan Hu.
Methodology: Qi Zhang, Jianan Hu, Yi Jin.
Supervision: Qi Zhang.
Writing – original draft: Qi Zhang, Jianan Hu, Yi Jin.
Writing – review & editing: Lijiao Wei, Rui Cao, Ruishu Ma, Huimin Song.
Footnotes
Abbreviations: BDT = block design test, CBM = the Chinese biomedical database, CDS = cornell depression score, CENTRAL = the cochrane central register of controlled trials, CI = confidence interval, CNKI = the China National Knowledge Infrastructure, CVFT = category verbal fluency tests, DP = digit span, DR = delay recall, LMDR = logical memory - delayed recall, MCI = mild cognitive impairment, MD = mean difference, MMSE = mini-mental state examination, RCTs = randomized controlled trials, SMD = standardized mean difference, TCE = traditional Chinese exercise, VS = visual span.
The authors report no conflicts of interest.
References
- [1].Dodge HH, Kadowaki T, Hayakawa T, et al. Cognitive impairment as a strong predictor of incident disability in specific ADL–IADL tasks among community-dwelling elders: the Azuchi study. Gerontologist 2005;45:222–30. [DOI] [PubMed] [Google Scholar]
- [2].Millan-Calenti JC, Tubio J, Pita-Fernandez S, et al. Cognitive impairment as predictor of functional dependence in an elderly sample. Arch Gerontol Geriatr 2012;54:197–201. [DOI] [PubMed] [Google Scholar]
- [3].Siu MY, Lee DTF. Effects of tai chi on cognition and instrumental activities of daily living in community dwelling older people with mild cognitive impairment. Bmc Geriatr 2018;18:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Petersen RC, Caracciolo B, Brayne C, et al. Mild cognitive impairment: a concept in evolution. J Interl Med 2014;275:214–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].John Wiley & Sons, Ltd, Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer's disease and vascular dementia. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Tricco AC, Soobiah C, Berliner S, et al. Efficacy and safety of cognitive enhancers for patients with mild cognitive impairment: a systematic review and meta-analysis. CMAJ 2013;185:1393–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Raschetti R, Albanese E, Vanacore N, et al. Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomised trials. Plos Med 2007;4:e338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Birks J, Flicker L. Donepezil for mild cognitive impairment. Cochrane Database Syst Rev 2006;3:CD006104. [DOI] [PubMed] [Google Scholar]
- [9].Loy C, Schneider L. Galantamine for Alzheimer's disease and mild cognitive impairment. Cochrane Database Syst Rev 2004;28:CD001747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Teixeira CVL, Gobbi LTB, Corazza DI, et al. Non-pharmacological interventions on cognitive functions in older people with mild cognitive impairment (MCI). Arch Gerontol Geriatr 2012;54:175–80. [DOI] [PubMed] [Google Scholar]
- [11].Song D, Yu D, Li P, et al. The effectiveness of physical exercise on cognitive and psychological outcomes in individuals with mild cognitive impairment: a systematic review and meta-analysis. Int J Nurs Stud 2018;79:155–64. [DOI] [PubMed] [Google Scholar]
- [12].Liu J, Wang XQ, Zheng JJ, et al. Effects of Tai Chi versus proprioception exercise program on neuromuscular function of the ankle in elderly people: a randomized controlled trial. Evid Based Complement Alternat Med 2012;4:e1600–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ge L, Zheng QX, Liao YT, et al. Effects of traditional Chinese exercises on the rehabilitation of limb function among stroke patients: a systematic review and meta-analysis. Complement Ther Clin Pract 2017;29:35. [DOI] [PubMed] [Google Scholar]
- [14].Wang XQ, Pi YL, Chen PJ, et al. Traditional Chinese exercise for cardiovascular diseases: systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc Cardiovasc Cerebrovasc Dis 2016;5:e002562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Luo X, Zhang J, Castelberg R, et al. The effects of traditional chinese exercise in patients with chronic obstructive pulmonary disease: a meta-analysis. Plos One 2016;11:e0161564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Deschamps A, Onifade C, Decamps A, et al. Health-related quality of life in frail institutionalized elderly: effects of a cognition-action intervention and Tai Chi. J Aging Phys Act 2009;17:236–48. [DOI] [PubMed] [Google Scholar]
- [17].Lam LC, Chau RC, Wong BM, et al. Interim follow-up of a randomized controlled trial comparing Chinese style mind body (Tai Chi) and stretching exercises on cognitive function in subjects at risk of progressive cognitive decline. Int J Geriatr Psychiatry 2011;26:733–40. [DOI] [PubMed] [Google Scholar]
- [18].Zhang Y, Huang L, Su Y, et al. The effects of traditional chinese exercise in treating knee osteoarthritis: a systematic review and meta-analysis. PloS One 2017;12:e0170237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wang XQ, Pi YL, Chen PJ, et al. Traditional Chinese exercise for cardiovascular diseases: systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc 2016;5:e002562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wayne PM, Walsh JN, Taylor-Piliae RE, et al. Effect of tai chi on cognitive performance in older adults: systematic review and meta-analysis. J Am Geriatr Soc 2014;62:25–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chen B, Wang X, Zou J, et al. Effect of traditional Chinese exercise on gait and balance for stroke: systematic review and meta-analysis. PloS One 2015;10:e219–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Sungkarat S, Boripuntakul S, Chattipakorn N, et al. Effects of Tai Chi on cognition and fall risk in older adults with mild cognitive impairment: a randomized controlled trial. J Am Geriatr Soc 2017;65:721–7. [DOI] [PubMed] [Google Scholar]
- [23].Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ: Br Med J 2011;343:889–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Tsai PF, Chang JY, Beck C, et al. A pilot cluster-randomized trial of a 20-week Tai Chi program in elders with cognitive impairment and osteoarthritic knee: effects on pain and other health outcomes. J Pain Symptom Manage 2013;45:660–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Lam LCW, Chau RCM, Wong BML, et al. Interim follow-up of a randomized controlled trial comparing Chinese style mind body (Tai Chi) and stretching exercises on cognitive function in subjects at risk of progressive cognitive decline. Int J Geriatr Psychiatry 2011;26:733–40. [DOI] [PubMed] [Google Scholar]
- [27].Zhen XT, Yu J, Tu RS, et al. Rehabilitation of Liuzijue on MCI of the old-aged persons (Chinese). IntJ Trad Chin Med 2013;35:968–72. [Google Scholar]
- [28].Zheng G, Xia R, Zhou W, et al. Aerobic exercise ameliorates cognitive function in older adults with mild cognitive impairment: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med 2016;50: bjsports -2015- 095699. [DOI] [PubMed] [Google Scholar]
- [29].Miller SM, Taylor-Piliae RE. Effects of Tai Chi on cognitive function in community-dwelling older adults: A review. Geriatr Nurs 2014;35:9–19. [DOI] [PubMed] [Google Scholar]
- [30].Colcombe SJ, Kramer AF, Erickson KI, et al. The implications of cortical recruitment and brain morphology for individual differences in inhibitory function in aging humans. Psychol Aging 2005;20:363–75. [DOI] [PubMed] [Google Scholar]
- [31].Rogers RL, Meyer JS, Mortel KF. After reaching retirement age physical activity sustains cerebral perfusion and cognition. J Am Geriatr Soc 1990;38:123–8. [DOI] [PubMed] [Google Scholar]
- [32].Gold SM, Schulz KH, Hartmann S, et al. Basal serum levels and reactivity of nerve growth factor and brain-derived neurotrophic factor to standardized acute exercise in multiple sclerosis and controls. J Neuroimmunol 2003;138:99–105. [DOI] [PubMed] [Google Scholar]
- [33].McDonnell MN, Smith AE, Mackintosh SF. Aerobic exercise to improve cognitive function in adults with neurological disorders: a systematic review. Arch Phys Med Rehabil 2011;92:1044–52. [DOI] [PubMed] [Google Scholar]
- [34].Matthews MM, Williams HG. Can Tai chi enhance cognitive vitality? A preliminary study of cognitive executive control in older adults after A Tai chi intervention. J S C Med Assoc 2008;104:255–7. [PubMed] [Google Scholar]


