Abstract
The triad of acute pancreatitis (AP) coexisting with diabetes ketoacidosis (DKA) and hypertriglyceridemia (HTG) has been reported, but no impact on mortality has been found to date. We aim to assess if patients with this triad are at a higher inpatient mortality compared to patients with acute pancreatitis only.
Retrospective cohort. The National Inpatient Sample (NIS) database from 2003 to 2013 was queried for patients with a discharge diagnosis of AP and presence of DKA and HTG was ascertained based on International Classification of Diseases, 9th revision (ICD9) codes. Adjusted for age, gender, race, Charlson comorbidity index (CCI), median income quartile, and hospital characteristics.
Over 2.8 million AP patients were analyzed. When compared with patients with AP-only, patients with the triad of AP + DKA + HTG had higher inpatient mortality (aOR 2.8, P < .001; CI: 1.9 - 4.2), Acute Kidney Injury (AKI) (aOR 4.1, P < .001; CI: 3.6-4.6), Systemic Inflammatory Response Syndrome (SIRS) (aOR 4.9, P < .001), Shock (aOR 4.3, P < .001), Acute Respiratory Distress Syndrome (ARDS) (aOR 3.0, P < .001), sepsis (aOR 2.6, P < .001), ileus (aOR 2.1, P < .001), parenteral nutrition requirement (aOR 1.8, P < .001), inflation-adjusted hospital charges (US$ 17,704.1), and had longer length of stay (LOS) (aOR 2.0, P < .001; CI 1.8–2.3). Furthermore, when compared to AP-only, patients with AP + HTG had lower mortality, which is different from the current AP knowledge. Finally, it appears that the driving force for the increased in mortality of patients with the triad (AP, DKA, HTG) is the DKA rather than the HTG.
Patients with the triad of AP, DKA, and HTG constitute a unique subgroup of patients that has higher inpatient mortality, multi-organ failure, hospital charges, and longer hospital length of stay. Therefore, hospital protocols targeting this subgroup of AP patients could improve mortality and outcomes.
Keywords: acute Pancreatitis, diabetes ketoacidosis, diabetic acidosis, hypertriglyceridemia
1. Introduction
The triad of acute pancreatitis (AP) coexisting with diabetes ketoacidosis (DKA) and hypertriglyceridemia (HTG) has been well reported and described as the enigmatic triad due to its complexity [1]. Studies have concluded that both AP and HTG can be found as a cause or consequence of DKA. The exact pathophysiologic role of DKA in the triad is still to be determined; because whether DKA is the cause of AP (DKA→HTG→AP) or rather a complication of AP (HTG→AP→DKA) is unclear. DKA patients have dysregulated glucose and lipid metabolism that results in hypertriglyceridemia, which in fact may cause acute pancreatitis. On the other hand, diabetes is a risk factor for metabolic syndrome and development of dyslipidemia, including hypertriglyceridemia. An episode of hypertriglyceridemia acute pancreatitis may decompensate diabetes and lead to DKA. In both scenarios, the clinician can encounter the triad as a unique clinical presentation that most of the time requires intensive care unit (ICU) for the DKA and/or for the severity of AP.
The clinical significance of this unique clinical scenario is important because the triad may increase acute pancreatitis mortality. DKA patients can present with abdominal pain, nausea, and vomiting; delaying the diagnosis of AP. In addition, DKA is a condition with high mortality and requires management in the intensive care unit (ICU). A systematic review of 29 cases with the triad in 1969 concluded that AP in the setting of DKA has a mortality of 80%. More recent cohort studies that have looked to the triad of AP, HTG, and DKA did not find increased mortality. These studies could have been underpowered.[1–5]
In our population cohort study, we evaluated AP outcomes in terms of inpatient mortality, LOS, hospital charges, multi-organ failures such as AKI, ARDS, sepsis, SIRS, ileus, and parenteral nutrition requirement. We compare, patients with AP-only vs the triad (AP, HTG, DKA), AP-HTG, and AP-DKA.
2. Methods
2.1. Study setting
The National Inpatient Sample (NIS) database is under the auspices of the Healthcare Cost and Utilization Project (HCUP) and is administered by the Agency for Healthcare Research and Quality. The NIS is the largest inpatient database in the United States (US) and contains data from 20% of all hospital discharges in the US; which represents around 8 million (unweight) and approximately 40 million (weighted) hospitalizations each year that is generalizable to the American population.
The NIS contains clinical and resource utilization data but protects the privacy of patients, physicians, and hospitals. It contains over 100 clinical outcomes and non-clinical data for each hospital stay with primary and secondary diagnosis as well as baseline population characteristics, patient's comorbidity measures, total charges (US$), and hospital characteristics.[6] Institutional Review Board approved the study as required by our institution (exempt review).
2.2. Subjects
The NIS from 2003 to 2013 was queried according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CMN) for patients with a discharge diagnosis of AP (ICD-9 577.0). The presence of DKA and HTG was ascertained based on ICD9 codes (250.1, 250.12, 250.13 and 272.0, 272.1, 272.2, 272.3, 272.9 respectively).
2.3. Outcomes
Main outcome included inpatient mortality. The definition of mortality was all-cause mortality while hospitalized for an acute pancreatitis (AP) episode. Secondary outcomes included organs failure such as acute kidney injury (AKI), acute respiratory distress syndrome (ARDS) or need for mechanical ventilation, ileus, myocardial infarction (MI), stroke, shock, bacterial infection, as well as systemic inflammatory response syndrome (SIRS), needs for parenteral nutrition, imaging test need (Computed tomography, magnetic resonance cholangiopancreatography), length of hospital stay (expressed in days), hospitalization charges in United States Dollars (USD) (inflation-adjusted). Results were adjusted for age, gender, race, Charlson comorbidity index (CCI), median income quartile, and hospital characteristics (teaching, government, private).
2.4. Analysis
Data are presented as population weighted mean ± standard error for continuous variables or population weighted percent ± standard error for categorical factors. A univariate analysis was performed to assess differences between subjects with and without DKA; continuous variables were compared using t tests and categorical variables were compared using Rao-Scott chi-square tests. In addition, separate univariate and multivariable logistic regression analyses were performed to assess the association between DKA and in-hospital death and other binary outcomes of interest. Also, univariate and multivariable linear regression analyses were performed to assess the association of DKA with hospital length of stay and hospital charges. All multivariable models included DKA, age, gender, race, median income quartile, CCI, HTG, and hospital characteristics. The Deyo modification of the Charlson Comorbidity Index (CCI) was used to define severity of co-morbid conditions.
Inflation adjustment for cost analysis: Charges were adjusted for inflation to 2013 dollars using the gross domestic product deflator (Table 1.1.4 Price Indexes for Gross Domestic Product, US Department of Commerce, Bureau of Economic Analysis). The temporal trend in inflation-adjusted hospital charges in subjects with AP was assessed by linear and polynomial linear regression. The most appropriate functional form for the trend was assessed by examination of regression diagnostic plots. The interaction between DKA and year was evaluated to see differences in trends by group.
All analyses were performed using SAS (version 9.4, The SAS Institute, Cary, NC), which account for the complex sampling design of NIS and appropriately weight participants in statistical models.
3. Results
3.1. Cohort characteristics
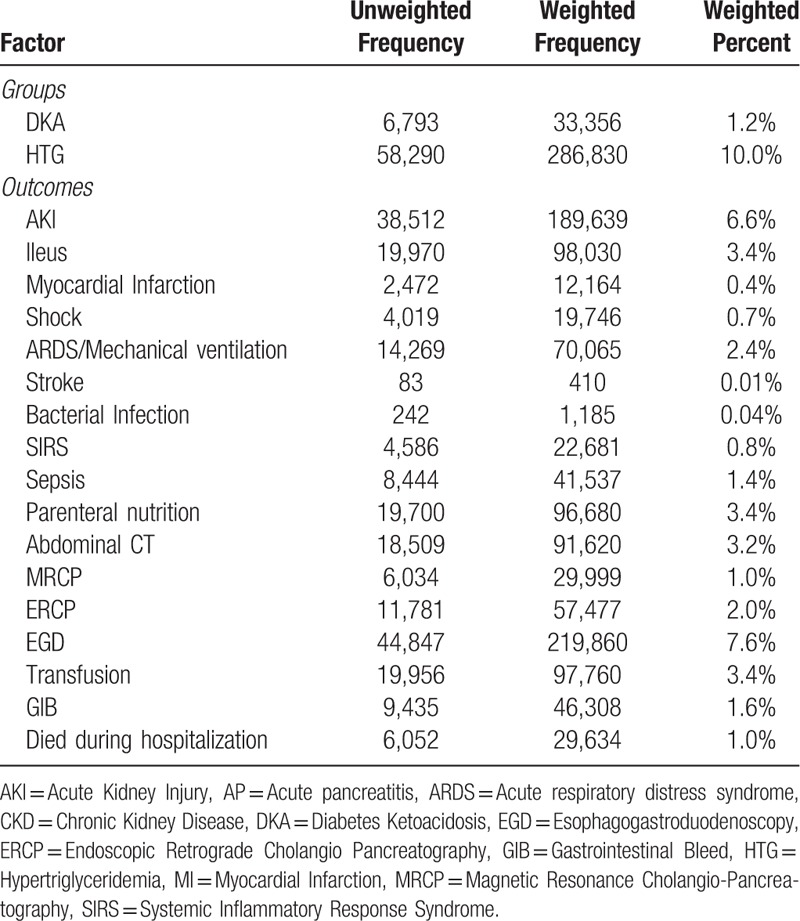
Our 10 years sample found over 2.8 million patients that were hospitalized with AP. From those, 33,356 had concomitant DKA and 286,830 had concomitant HTG. The mean age in years, according to the study groups were as follow: AP-only 52.6, AP+ HTG 52.8, AP +DKA 43.0, AP + DKA + HTG (triad) 38.8. Patients with the triad as well as those with AP+DKA were younger when compared to the AP-only group. The age of patients with AP + HTG was similar to the AP only group. Patients with the triad were predominantly men (65.3%) and obese (27.7%). Significant racial differences were found: 10.1% of patients were Hispanics in the AP-only group, compared to 23.9% (triad), 12.5% (AP + HTG) and 15.1% (AP + DKA). 14.4% were African Americans in the AP-only group, compared to 9.7% (triad), 9.1% (AP + HTG) and 18.1% (AP+DKA). We also report the frequency of the triad cases per hospital geographical region as follow: South (42.2%), West (26.9%), Midwest (18.5%) and the Northeast (12.4%) (Table 1).
Table 1.
Group and outcome prevalence in AP Cohort.
3.2. Clinical course
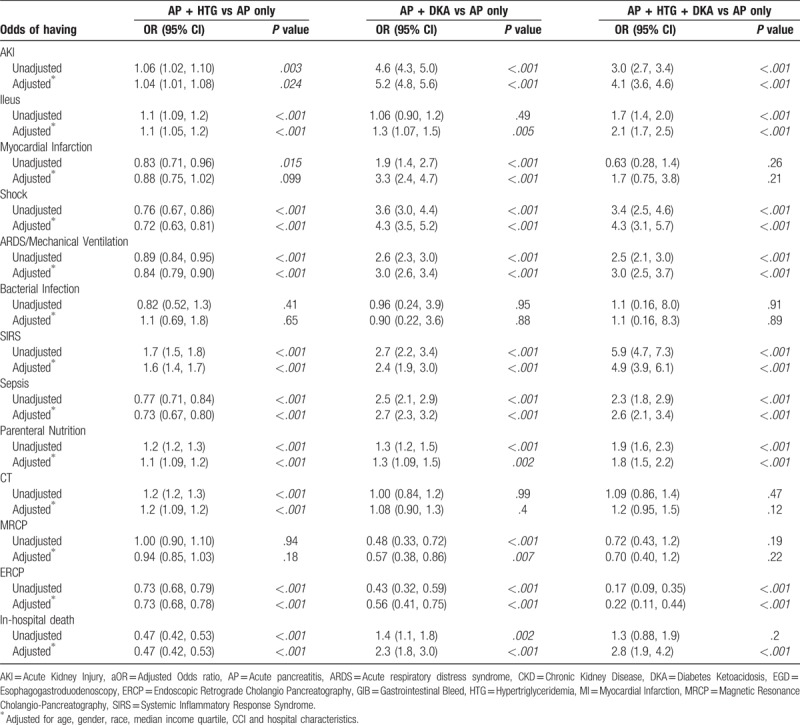
Patients with the triad had significantly higher inpatient mortality (aOR 2.8, P < .001; CI: 1.9–4.2) when compared to AP-only patients. In addition, patients with AP + DKA had also higher inpatient mortality (aOR 2.3, P < .001; CI 1.8–3.0) when compared to AP-only patients. Interestingly, patients with AP + HTG had lower mortality when compared to AP-only patients (aOR 0.47, P < .001; CI 0.42–0.53). In regards of organ failure, patients with the triad had 4 times higher odds of having AKI than those with AP-only (OR 4.1, P < .001; CI: 3.6–4.6). Although, the highest risk for developing AKI was on the AP + DKA group (aOR 5.2, P < .001; CI 4.8–5.6). There was no difference on AKI occurrence when comparing AP + HTG with AP-only patients. Moreover, the triad subjects also had higher odds of having SIRS (aOR 4.9, P < .001), shock (aOR 4.3, P < .001), ARDS (aOR 3.0, P < .001), sepsis (aOR 2.6, P < .001), ileus (aOR 2.1, P < .001) and parenteral nutrition requirement (aOR 1.8, P < .001) (Table 2). Additionally, patients with AP + DKA had higher risk for shock (aOR 4.3, P < .001), sepsis (aOR 2.7, P < .001), ARDS/Mechanical ventilation (aOR 3.0, P < .001), and myocardial infarction (aOR 3.3, P < .001) when compared to AP-only patients (Table 2).
Table 2.
Association between DKA/HTG and binary outcomes of AP.
Furthermore, patients with the triad (US$ 17,704.1) and AP + DKA (US$ 14.083.6) had higher hospital charges when compared to AP-only patients. Importantly, triad patients stayed 2 days longer in the hospital (P < .001; CI 1.8–2.3) and AP +DKA 1.8 days longer (P < .001; CI 1.5–2.1) when compared to AP-only patients’ length of stay. Contrary, AP +HTG patients had shorter length of stay (0.2 days less, P < .001) when compared to AP-only (Table 3). After adjusting for inflation, we found that hospital charges continue to rise and significant differences were also found between study groups (Fig. 1).
Table 3.
Association between DKA_HTG and continuous outcomes of AP.
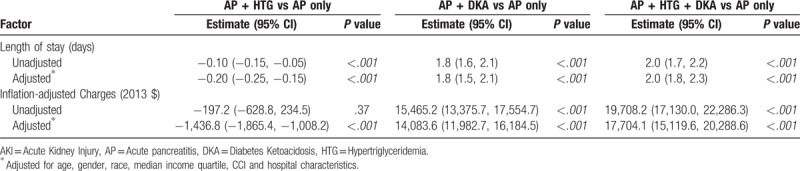
Figure 1.
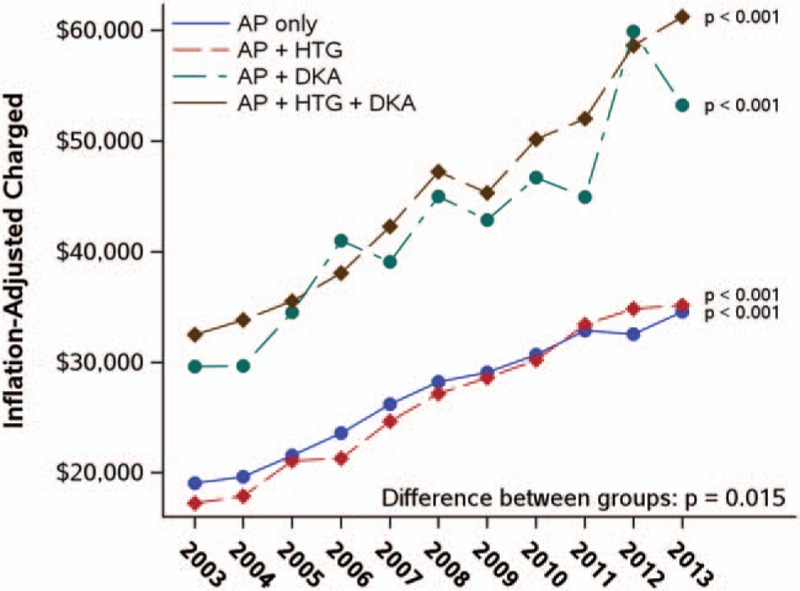
Trends in charges.
4. Discussion
In this large cohort study, we have found significantly higher inpatient mortality in AP patients with the triad (concomitant DKA and HTG) when compared to AP-only patients. Significant higher mortality was also found in patients with concomitant AP and DKA. The occurrence of the triad is uncommon, but easily overlooked due to the similarity of clinical presentation with DKA only patients. Previous studies have not been able to demonstrate a higher mortality in patients with the triad, and this was because of the small sample size (Nair et al: 11, Quintanilla et al: 8, Fernandez 54, Wang et al: 37 patients).[1–5] The presented study is a new addition to the current knowledge and merits more studies to look for what are the factors that affect the mortality in patients with the triad. In addition, DKA itself is a known life-threatening condition with high mortality that requires direct ICU admission in most cases. Our study also found that AP patients with concomitant DKA have higher mortality and this finding also reinforce the current literature on DKA. We suggest that hospitals should work on the implementation of AP-DKA management protocols to decrease mortality in this unique group patients. Furthermore, since the year 2000, DKA was found to be an independent risk factor for HTG-induced AP in a prospective assessment of 100 consecutive cases by Nair et al In the same study, the prevalence of the HTG in AP with DKA was found to be 36%. These findings are different to our study findings, 11% prevalence of AP + DKA +HTG. Prevalence of DKA in AP was found to be 10%, which correlates with the current literature.[1]
In addition, published literature have found that AP prevalence in DKA patients is about 11% and HTG is the leading etiology with 36% of cases.[1] However, no large population or epidemiologic studies exist to confirm this high prevalence of AP in DKA patients. Furthermore, a Mexican case control study of 55 hypertriglyceridemia AP patients compared patients with DKA (8) vs. Non-DKA (47). The later study did not find higher mortality in the 8 DKA patients but did find more severe AP based on Ranson criteria and APACHE II scores.[4] Although these AP severity-scoring systems are confounded by elevated glucose, base deficit and low pH that are directly influenced by DKA and not by AP and should not be used to assess AP severity and new AP severity scoring systems need to be developed for application in DKA with AP patients.[5]
Regarding hypertriglyceridemia, the authors noticed that HTG-induced AP has raised concern in recent years due to its reported higher mortality and complications; this was not the case in our study where patients with concomitant AP-HTG did not have higher mortality or organ failure incidence.
In the presented study, we found an increased mortality in patients with the triad as well as in patients with concomitant AP +DKA. Importantly, acute pancreatitis can be underdiagnosed due to the similarity of clinical presentation with DKA. Studies are needed to investigate the true prevalence of AP in patients admitted with DKA as only 1 single center study exist by Nair and Pitchumoni et al that reported 11% prevalence of AP in DKA patients (1).
The strengths of this study include: Largest patient cohort to date and results adjusted for age, gender, race, Charlson comorbidity index (CCI), median income quartile, and hospital characteristics. Nevertheless, the NIS database has limitations that impact our study. For example, it only contains inpatient data and post discharge follow up and outcomes are lacking. It also relies on administrative data and billing codes for assessment of outcomes and exposures. This is a retrospective study and there is risk for recall bias, misclassification bias and confounders. Finally, the mortality definition used was all-cause mortality, as this administrative database does not allow for specifically test for mortality due to exclusively acute pancreatitis.
5. Conclusion
In summary, our study shows that patients with the triad as well as AP-DKA patients have higher inpatient mortality., SIRS, AKI, ARDS, MI, sepsis, shock, parenteral nutrition requirement, hospital charges, and longer length of stay. Patients with the triad and with concomitant DKA constitute a unique subgroup of patients with remarkable different outcomes. Hospital protocols targeting these subgroups of AP patients to improve mortality are needed. Interestingly the patients with AP-HTG had lower mortality, which is different than the current AP knowledge and it appears that the driving force for higher mortality in our study was the DKA rather than the HTG.
5.1. Study highlights
-
1.
What is current knowledge
AP with concomitant DKA and HTG is not an infrequent presentation.
HTG is the main cause of AP with concomitant DKA
DKA itself has high mortality and warrant ICU management
Studies to date have not identified higher mortality in patients with AP + DKA +HTG
-
2.
What is new here
We have identified a higher inpatient mortality, multi-organ failure, hospital charges and longer length of stay in patients with the triad of AP + DKA + HTG.
Interestingly, patients with AP + HTG had lower mortality, which is different than the current knowledge.
In the context of AP, it appears that the driving force for higher mortality is the DKA rather than the HTG.
Author contributions
Conceptualization: Carlos Roberto Simons-Linares, Amit Bhatt, Rocio Lopez, Sunguk Jang, Madhusudan Sanaka, Tyler Stevens, John Vargo, Prabhleen Chahal.
Data curation: Carlos Roberto Simons-Linares, Rocio Lopez, Tyler Stevens, John Vargo, Prabhleen Chahal.
Formal analysis: Carlos Roberto Simons-Linares, Rocio Lopez.
Investigation: Carlos Roberto Simons-Linares, Amit Bhatt, Rocio Lopez, Sunguk Jang, Madhusudan Sanaka, Tyler Stevens, John Vargo, Prabhleen Chahal.
Methodology: Carlos Roberto Simons-Linares, Amit Bhatt, Rocio Lopez, Madhusudan Sanaka, Tyler Stevens, John Vargo, Prabhleen Chahal.
Project administration: Carlos Roberto Simons-Linares, Amit Bhatt, Rocio Lopez, Sunguk Jang, Madhusudan Sanaka, Prabhleen Chahal.
Resources: Carlos Roberto Simons-Linares.
Software: Carlos Roberto Simons-Linares, Rocio Lopez.
Supervision: Carlos Roberto Simons-Linares, Amit Bhatt, Rocio Lopez, Sunguk Jang, Madhusudan Sanaka, Tyler Stevens, John Vargo, Prabhleen Chahal.
Validation: Carlos Roberto Simons-Linares.
Visualization: Tyler Stevens, John Vargo, Prabhleen Chahal.
Writing – original draft: Carlos Roberto Simons-Linares, Amit Bhatt, Sunguk Jang, Madhusudan Sanaka, Prabhleen Chahal.
Writing – review & editing: Carlos Roberto Simons-Linares, Amit Bhatt, Sunguk Jang, Madhusudan Sanaka, Tyler Stevens, John Vargo, Prabhleen Chahal.
Carlos Roberto Simons-Linares orcid: 0000-0002-5586-3722.
Footnotes
Abbreviations: AKI = acute kidney injury, aOR = adjusted odds ratio, AP = acute pancreatitis, ARDS = acute respiratory distress syndrome, CCI = Charlson comorbidity index, CKD = chronic kidney disease, DKA = diabetes ketoacidosis, EGD = esophagogastroduodenoscopy, ERCP = endoscopic retrograde cholangio-pancreatography, GIB = gastrointestinal bleed, HTG = hypertriglyceridemia, ICD-9 = international classification of diseases (ICD), 9th revision, LOS = hospital length of stay, LPL = lipoprotein lipase, MI = myocardial infarction, MRCP = magnetic resonance cholangio-pancreatography, SIRS = systemic inflammatory response syndrome, VLDL = very-low-density lipoproteins.
All authors have no conflicts of interest to disclose.
References
- [1].Nair S, Yadav D, Pitchumoni CS. Association of diabetic ketoacidosis and acute pancreatitis: observations in 100 consecutive episodes of DKA. Am J Gastroenterol 2000;95:2795–800. [DOI] [PubMed] [Google Scholar]
- [2].Yadav D, Nair S, Norkus EP, et al. Nonspecific hyperamylasemia and hyperlipasemia in diabetic ketoacidosis: incidence and correlation with biochemical abnormalities. Am J Gastroenterol 2000;95:3123–8. [DOI] [PubMed] [Google Scholar]
- [3].Fernandez R, Misra R, Nalini R, et al. Characteristics of patients with ketosis-prone diabetes (KPD) presenting with acute pancreatitis: implications for the natural history and etiology of a KPD subgroup. Endocr Pract 2013;19:243–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Quintanilla-Flores DL, Rendon-Ramirez EJ, Colunga-Petraza PR, et al. Clinical course of diabetic ketoacidosis in hypertriglyceridemic pancreatitis. Pancreas 2015;44:615–8. [DOI] [PubMed] [Google Scholar]
- [5].Wang Y, Attar BM, Hinami K, et al. concurrent diabetic ketoacidosis in hypertriglyceridemia-induced pancreatitis: how does it affect the clinical course and severity scores? Pancreas 2017;46:1336–40. [DOI] [PubMed] [Google Scholar]
- [6].Healthcare Cost and Utilization Project (HCUP). 2011. Agency for Healthcare Research and Quality, Rockville, MD. [Google Scholar]


