Abstract
Aim
Bochdalek hernias, which brought after the neonatal period, are also late-defined cases. In this study, we aimed to present the clinical characteristics of patients with late-presentation Bochdalek hernias who underwent surgery in a reference hospital and our experience regarding their diagnosis.
Material and Methods
Patients with late-presentation Bochdalek hernia who underwent surgery in our clinic between 2001 and 2016 were analyzed retrospectively in terms of the causes of the delay in diagnosis, symptoms, and radiologic and surgical results.
Results
A total of seven patients with late-presentation Bochdalek hernia underwent surgery, four males and three females. The median age was 48 months. Of the 43 patients who underwent surgery for Bochdalek hernia during the same period, 7 (16.27%) presented to hospital late. In all late-presentation Bochdalek hernia cases, the defect was on the left side. Two patients had hernia sacs, and two patients had ectopic intrathoracic left kidneys. Six of the patients presented with gastrointestinal system symptoms, and one with respiratory system symptoms. The median time between the onset of symptoms and diagnosis was 60 days. The maternal age of four patients was ≥30 years. The gestational age and birth weights of the patients were normal. In physical examination, there was a scaphoid abdomen and an increased chest anterior-posterior diameter. In chest radiographs of all patients, the appearance was consistent with intestinal gas in the left hemithorax. The transverse length of the defect in the diaphragm (median value: 5 cm) in the patients with late-presentation Bochdalek hernia was longer than that (median value: 3 cm) of patients who were diagnosed early (p=0.02). The difference was statistically significant. All patients survived, were followed up for an average of 3 years, and no relapse was observed during the follow-up period.
Conclusion
Bochdalek hernia can be diagnosed after the neonatal period. Contrary to cases diagnosed in the neonatal period, gastrointestinal system symptoms are at the forefront in these cases, and these patients have good prognosis. Congenital diaphragmatic hernia should be considered in the differential diagnosis in patients with gastrointestinal system symptoms such as recurrent nausea and vomiting.
Keywords: Bochdalek hernia, Congenital diaphragmatic hernia, child late presentation
Introduction
Congenital diaphragmatic hernia (CDH) is a closure defect of the pleuroperitoneal canal. It is characterized by herniation of the intraabdominal organs into the thorax. The most common type of congenital diaphragmatic hernia is left posterolateral Bochdalek hernia (BH) (1). Although symptoms occur in the early stage in BH, Morgagni and hiatal hernias are manifested in later stages (2). Generally, BH is one of the problems considered primarily if severe respiratory failure, tachypnea, and cyanosis are present in the neonatal period. The mortality rate in congenital diaphragmatic hernia is still high despite all medical advances (3). BH is divided into two groups as early and late presentation (4). Late-onset BH (LOBH) is the type that is detected after the neonatal period. It constitutes 5–45.5% of all CDHs (5). Its clinical signs and symptoms are different compared with early-onset BH (4). Gastrointestinal symptoms predominate in late-onset BH (2).
In this study, we aimed to present the clinical characteristics of patients with LOBH who underwent surgery in a reference center, and our clinical experiences in relation to characterization.
Material and Methods
Approval was obtained from Fırat University Noninvasive Researches Ethics Committee for this study (Decision number: 10, Date: 16/11/2017). This retrospective study has been conducted in accordance with the principles of the Helsinki Declaration. The patients who underwent surgery because of BH in our clinic between 2001 and 2016 were evaluated. Patients who were diagnosed as having BH in the neonatal period, and patients with traumatic diaphragmatic hernia, hiatal hernia, and diaphragm eventration were excluded from the study. The files of patients with late-onset BH were examined retrospectively. The age, sex, gestational age, birth weight, symptoms, maternal age, the time between the onset of symptoms and diagnosis, physical examination, accompanying anomalies, laboratory values, diagnostic and therapeutic methods, defect sizes, presence of hernia sac, hospitalization time, and complications were recorded.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) for Windows-21 (IBM Corp.; Armonk, NY, USA) program was used to record the data and for statistical analysis. Qualitative data are expressed as percentages and numeric data that did not show normal distribution are expressed as median values (minimum–maximum). In analysis of the data, the distribution of continuous variables was determined using the Kolmogorov-Smirnov and Shapiro-Wilk normality tests. The Mann-Whitney U test was used in the comparison of independent dual groups that did not show normal distribution, and p values <0.05 were considered significant.
Results
Seven (16.27%) of 43 patients who underwent surgery because of BH had LOBH. Four of the patients were male and three were female (M/F=1.3). The median age was 48 months (min: 2, max: 180). In all patients, the defect was in the left diaphragm.
Six (85.71%) of the patients had gastrointestinal system symptoms with predominance of nausea and vomiting, and one (14.29%) had respiratory system symptoms (lung infection). The median time between the onset of symptoms and diagnosis was 60 days (min: 10, max: 365). The maternal age was found as <30 years in two patients and ≥30 years in 5 patients. All patients were born at term and had normal birth weight. The physical examination was normal in four (57.15%) patients, but two (28.57%) had abdominal tenderness and one (14.28%) had scaphoid abdomen and an increased antero-posterior chest diameter. In three patients who had predominant gastrointestinal symptoms, urinary tract infection, constipation and mesenteric lymphadenitis were considered one for each. Pneumonia was considered in one patient who had predominant respiratory tract symptoms (decreased lung sounds).
Oxygen saturations measured with a pulse oximeter were within normal limits in our patients (95–100%). The blood gas values were found to be within the normal limits: pH: 7.35–7.45, PaCO2: 35–45 mm Hg, PaO2: 80–100 mm Hg, HCO3: 22–26 mEq/L.
In all patients, lung radiography revealed appearances compatible with intestinal gas in the left hemithorax (Picture 1). Previous lung radiography obtained in an external center was evaluated to be in favor of infiltration in one patient and CDH was not suspected in another patient. In the patients whose lung radiography suggested CDH, diaphragmatic defects were defined using computed thoracic tomography in five patients and thoracic magnetic resonance imaging (MRI) in two patients (Picture 2).
The diaphragmatic defect diameters ranged between 3×1 and 8×3 cm. In LOBH, the median value for the transverse length of the diaphragmatic defect was 5 cm (minimum: 3, maximum: 8) and the median value for the antero-posterior length was 2 cm (min: 1, max: 4). In the patients who had early-onset BH in the same period, the median value for the transverse length was 3 cm (min: 2, max: 8) and the median value for the antero-posterior length was 2 cm (min: 1, max: 5). In LOBH, the transverse length of the diaphragmatic defect was longer compared with early-onset BH and the difference was statistically significant (p=0.02). No statistically significant difference was found between the antero-posterior lengths (p=0.887).
Hernia sac was present in two (28.57%) patients, anectopic intrathoracic left kidney was present in two (28.57%), and a cardiac anomaly (atrial septal defect) was present in one patient (14.28%) patient.
In all patients, primary diaphragm repair was performed by way of left subcostal laparotomy. The kidneys were left in the thoracic space in two patients who had ectopic intrathoracic kidneys. Mechanical ventilation was not needed after surgery in these patients. A patient who developed ileus after surgery recovered with supportive treatment. The mean follow-up time was 3 (range, 2–5) years. No recurrence was observed in the patients. The patients’ demographic and clinical characteristics are summarized in Table 1.
Table 1.
Demographic and clinical characteristics of the patients
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| Age/Sex | 6 years | 7 years | 15 years | 2 months | 4 years | 9 months | 4 months |
| M | F | M | M | F | M | F | |
| Symptoms | GIS | GIS | GIS | GIS | GIS | GIS | RS |
| Time of onset of symptoms (days) | 365 | 60 | 365 | 10 | 10 | 60 | 90 |
| Gestational age | >36 weeks | >36 weeks | >36 weeks | >36 weeks | >36 weeks | >36 weeks | >36 weeks |
| Maternal age (years) | 30 | 35 | 40 | 35 | 30 | 28 | 28 |
| Birth weight (g) | 3000 | 3300 | 3000 | 3100 | 3000 | 3000 | 3200 |
| Physical examination | No pathology | No pathology | No pathology | Scaphoid abdomenincreased thoracic antero-posterior diameter | Abdomen tender-ness | Abdomen tenderness | No pathology |
| Hernia region and sac, defect diameter (cm) | Left PL, HS absent, 3×1 | Left PL, HS absent 8×2 | Left AL, HS absent 8×2 | Left PL HS absent, 4×4 | Left PL HS present, 8×3 | Left PL HS present, 5×3 | Left PL HS absent, 4×2 |
| Organs inside the thorax | Spleen, Stomach | Colon, Left kidney | Stomach | Spleen, Stomach | Colon | Left kidney | Spleen |
| Complication | None | None | None | Brid ileus | None | None | None |
| Hospitalization period (days) | 8 | 10 | 10 | 14 | 8 | 8 | 7 |
AL: anterolateral; M: male; GIS: Gastrointestinal system; HS: hernia sac; F: female PL: posterolateral; RS: respiratory system
Discussion
Development of acute respiratory distress in the neonatal period is a classic finding of CDH. The occurrence of symptoms after the first month is defined as late-onset CDH. The most common type is BH. It occurs with a 2-fold higher rate in boys (1, 5). In this study, the male/female ratio was found as 1.3/1. Localization on the right side occurs more commonly in patients with late-onset CDH compared with all patients with CDH. Patients with right-sided CDH become symptomatic at younger ages compared with patients with left-sided CHD (5, 6). Anterolateral CDH is localized more anteriorly in contrast to the anatomy of BH and has been defined as a type of BH (7). In contrast to the literature, six patients in our study had left posterolateral localization and one had left anterolateral localization (BH with atypical localization). Three patients were aged below one year and one patient was aged 15 years.
Forty-three percent of the patients with LOBH present with respiratory system symptoms and 33% present with gastrointestinal symptoms, 6.3–11% of the patients are asymptomatic (4, 8). It has been reported that respiratory tract symptoms occur immediately after birth and gastrointestinal symptoms are manifested at advanced ages (4). In our study, respiratory distress was present in one of three patients who were aged below one year. In six patients, gastrointestinal symptoms that were accompanied especially by nausea and vomiting predominated. The median value for the time between the onset of symptoms and diagnosis was 60 days (minimum: 10, maximum: 365). The reasons for prolongation of this time period for making the diagnosis were as follows: consideration of conditions leading to non-specific gastrointestinal symptoms including pneumonia, urinary tract infection, mesenteric lymphadenitis, constipation, and abdominal distention as prediagnoses, evaluation of X-rays as normal or inadequate interpretation of X-rays, and lack of consideration of CDH in the differential diagnosis. Gastrointestinal symptoms are observed more frequently in cases of left-sided BH (4). In this study, all patients had left-sided BH and gastrointestinal symptoms predominated. Physical examination revealed abdominal tenderness (non-specific finding) in two patients, and scaphoid abdomen and increased thoracic anteroposterior diameter suggestive of BH were present in only one patient. Four patients had no pathologic findings on physical examination.
Lung radiography is used frequently in the diagnosis. However, it has been reported that contrast- enhanced computed tomography might contribute to the differential diagnosis in suspected cases (9, 10). Treatment for pneumonia was initiated in a patient because of the appearance of infiltration on lung radiography. Treatment for urinary tract infection was given three times in a patient whose left kidney was located in the thorax because of a history of frequent urinary tract infection. The left kidney could not be seen on urinary tract ultrasonography performed during the diagnostic and therapeutic process. Renal cortex scintigraphy was performed and it was found that the left kidney was located in the left hemothorax. CDH was defined on MRI. In this study, CDH was diagnosed using computed tomography in five patients and MRI in two patients in addition to lung radiography.
Herniation of the intraabdominal organs into the thorax with increased intraabdominal pressure and reduction of the herniated organs back to the abdomen with reduction of the pressure have been reported as factors leading to the late occurrence of clinical symptoms in late-onset CDH (11). In this study, the left kidney was located inside the thorax in two patients and the spleen was located inside the thorax in three patients. It was thought that these solid organs were permanently located in the thorax independent of increased intraabdominal pressure. The literature related to increased intraabdominal pressure may apply for the intestines, which are motile organs.
In LOBH, the median value for the transverse length of the diaphragm defect was 5 cm (min: 3, max: 8) and the median value for the antero-posterior length was 2 cm (min: 1, max: 4). In the patients who had early-onset BH in the same period, the median value for the transverse length was 3 cm (min: 2, max: 8) and the median value for the antero-posterior length was 2 cm (min: 1, max: 5). In LOBH, the transverse length of the diaphragmatic defect was longer compared with early-onset BH and the difference was statistically significant (p=0.02). No statistically significant difference was found between the antero-posterior lengths (p=0.887). We think that longer transverse length of the defect in LOBH may be associated with increased defect size with growth of the patient.
A hernia sac is observed in 7.6–32.7% of patients (4, 12). It has been reported that the presence of a hernia sac may cause late onset of symptoms (5). In this study, hernia sac was present in two (28.6%) patients, one of whom was aged below one year and one was aged four years.
In the study by Kim et al. (11), it was reported that intestinal malrotation and pulmonary hypoplasia were not present in their subjects and the rate of additional anomalies was 23%. In our series, intestinal malrotation and pulmonary hypoplasia were not found. Two patients had an ectopic intrathoracic left kidney and one patient had an atrial septal defect (n=3, 42.85%). It was thought that the blood gas values were within normal limits and gastrointestinal symptoms predominated because of absence of pulmonary hypoplasia. In the literature, it has been reported that large and small intestinal hernias, stomach hernias, and splenic hernias are frequently found in left CDH (6). In our study, splenic hernia was found in three patients, stomach hernia was found in three patients and colonic hernia was found in two patients.
In cases of late-onset CDH, postoperative complications have been reported with a rate of 3.6%, recurrence has been reported with a rate of 1.9%, and the mortality rate has been reported as 3.9% (5). In this study, ileus developed in only one patient (14.28%) and recovered with supportive treatment; recurrence and mortality were not observed.
In conclusion, BH may become symptomatic in the late stage. Patients with LOBH can mostly be diagnosed with careful evaluation. LOBH is different from early-onset BH in that gastrointestinal symptoms are observed more commonly compared with respiratory tract symptoms and it has favorable prognosis. LOBH should be considered in the differential diagnosis in patients with gastrointestinal symptoms including recurrent nausea and vomiting.
Figure 1.
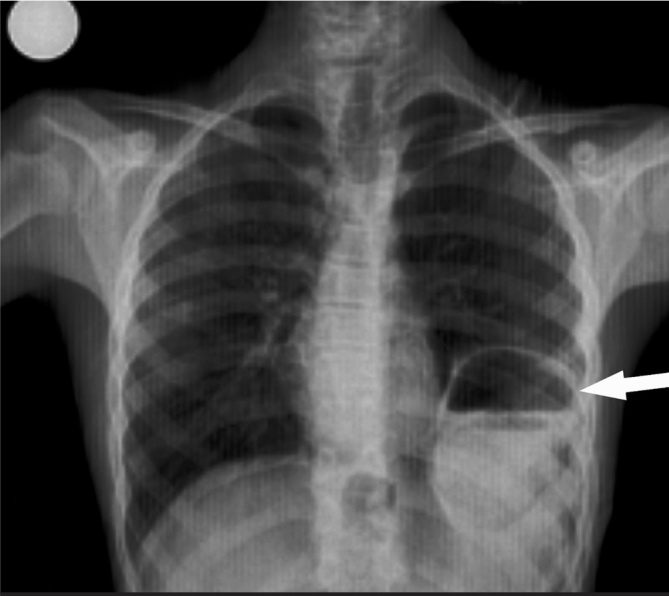
Antero-posterio lung radiography in the patient with Bochdalek hernia with late presentation
Figure 2.

Computed tomography of the thorax (coronal section) in the patient with Bochdalek hernia with late presentation
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Fırat University School of Medicine (16/11/2017-10).
Informed Consent: Informed consent was not obtained from patients due to the retrospective nature of the study.
Author Contributions: Concept - T.T.; Design - T.T., M.S.; Supervision - Ü.B., A.K., ; Data Collection and/or Processing - T.T., M.S., Ü.B.; Analysis and/ or Interpretation - T.T., A.K.; Literature Review - T.T., M.S.; Writing - T.T.; Critical Review - Ü.B., A.K.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Demirkaya A, Kaynak K. Bochdalek hernisinde tanı ve cerrahi tedavi. Turk Klin J Thorasic Surg Spec Top. 2010;3:18–22. [Google Scholar]
- 2.Çelmeli F, Palancı AN, Şahin M, Saz EU, Türkkahraman D. Late-onset congenital diaphragmatic hernia; report of three cases. J Pediatr Res. 2015;2:105–8. doi: 10.4274/jpr.64936. [DOI] [Google Scholar]
- 3.Soyer T, Hançerlioğulları Ö, Demirçeken F, Yağmurlu A, Çakmak M. Thoracoscopic diaphragmatic hernia repair in late onset congenital diaphragmatic hernia: report of a case. J Turkish Assoc Pediatr Surg. 2008;22:79–83. [Google Scholar]
- 4.Kitano Y, Lally KP, Lally PA Congenital diaphragmatic hernia study group. Late-presenting congenital diaphragmatic hernia. J Pediatr Surg. 2005;40:1839–43. doi: 10.1016/j.jpedsurg.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 5.Baglaj M. Late-presenting congenital diaphragmatic hernia in children: a clinical spectrum. Pediatr Surg Int. 2004;20:658–69. doi: 10.1007/s00383-004-1269-5. [DOI] [PubMed] [Google Scholar]
- 6.Elhalaby EA, Magda H, Sikeena A. Delayed presentation of congenital diaphragmatic hernia. Pediatr Surg Int. 2002;18:480–5. doi: 10.1007/s00383-002-0743-1. [DOI] [PubMed] [Google Scholar]
- 7.Saraç M, Bakal Ü, Tartar T, Sarı MY, Çığşar Kuzu EB, Kazez A. A rare case: atypical localized diaphragmatic hernia. F Ü Sağ Bil Tıp Derg. 2016;30:143–5. [Google Scholar]
- 8.Batts S, Thompson MW, Person DA. Late presentation of diaphragmatic hernia in a Pacific Island pediatric populatin. Hawaii Med J. 2009;68:59–61. [PubMed] [Google Scholar]
- 9.Muzzafar S, Swischuk LE, Jadhav SP. Radiographic findings in late-presenting congenital diaphragmatic hernia: helpful imaging finding. Pediatr Radiol. 2012;42:337–42. doi: 10.1007/s00247-011-2226-9. [DOI] [PubMed] [Google Scholar]
- 10.Baglej M, Dorobisz U. Late-presenting congenital diaphragmatic hernia in children: a literature review. Pediatr Radiol. 2005;34:478–88. doi: 10.1007/s00247-004-1389-z. [DOI] [PubMed] [Google Scholar]
- 11.Kim DJ, Chung JH. Late-presenting congenital diaphragmatic hernia in children: the experience of single institution in Korea. Yonsei Med J. 2013;54:1143–8. doi: 10.3349/ymj.2013.54.5.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosgor M, Karaca I, Karkiner A, et al. Associated malformations in delayed presentation of congenital diaphragmatic hernia. J Pediatr Surg. 2004;39:1073–6. doi: 10.1016/j.jpedsurg.2004.03.050. [DOI] [PubMed] [Google Scholar]


