Abstract
Objective:
Childhood irritability is a common, impairing problem with changing agerelated manifestations that predict long-term adverse outcomes. However, more work is needed on its overall and age-specific neural correlates. Since irritable youth exhibit exaggerated responses to frustrating stimuli, we used a frustrating functional magnetic resonance imaging (fMRI) paradigm to examine associations between irritability and neural activation and tested the moderating effect of age.
Method:
We studied a transdiagnostic sample of 195 youths with varying levels of irritability (52 disruptive mood dysregulation disorder, 42 anxiety disorder, 40 attention deficit/hyperactivity disorder, and 61 healthy volunteers). Irritability was measured by parent- and child-reports on the Affective Reactivity Index. The fMRI paradigm was a cued-attention task differentiating neural activity in response to frustration (rigged feedback) from activity during attention orienting in the trial following frustration.
Results:
Whole-brain activation analyses revealed associations with irritability during attention orienting following frustration. Irritability was positively associated with frontalstriatal activation, specifically in dorsolateral prefrontal cortex, inferior frontal gyrus, and caudate (rs=.31-.40, ps<.05). Age moderated the association between irritability and activation in some frontal and posterior regions (anterior cingulate cortex [ACC], medial frontal gyrus, cuneus, precuneus, superior parietal lobule; F1,189=19.04–28.51, ps<.001, ηp2=.09-.13). Specifically, higher irritability was more strongly related to increased activation in younger relative to older youths.
Conclusions:
Following frustration, levels of irritability correlate with activity in neural systems mediating attention orienting, top-down regulation of emotions, and motor execution. While most associations were independent of age, dysfunction in ACC and posterior regions was more pronounced in young children with irritability.
Irritability can be defined as an increased propensity to experience anger and frustration, relative to peers (1). It is a serious and common mental health problem in youth (1,2). It predicts adult depressive and anxiety disorders (a genetically-mediated association) and long-term impairment e.g., high suicidality, low educational and income attainment (1–3). Irritability is also a core feature of the new DSM-5 category, disruptive mood dysregulation disorder (DMDD), which is characterized by developmentally inappropriate, frequent, and severe temper outbursts (2,4). Youth with severe irritability suffer significant impairment in multiple domains (e.g., home, school, and with peers) and have high rates of service use, hospitalization, and school suspensions (2,4). However, there are few evidence-based treatments for irritability (5). A better understanding of the pathophysiology of irritability is essential to guide the development of novel mechanism-based treatments for this common and impairing problem.
Given the increased proneness to frustration associated with irritability, and working from a translational neuroscience perspective, the neural mechanisms mediating irritability can be captured by studying an organism’s neural responses to frustrative non-reward (1,2). Originally operationalized in rodents, frustrative nonreward is the psychological state induced by the failure to receive a reward that an organism has been conditioned to expect (6). In humans, investigators can model frustrative non-reward during functional magnetic resonance imaging (fMRI) scanning by evoking frustration in real time while assessing its neural correlates (2). In a large, transdiagnostic sample, we used such methods to examine associations between irritability and neural activation during an fMRI paradigm that models frustrative non-reward.
Our second goal was to examine age-related variation in the association between irritability and neural activity. Normative responses to frustration change during development (7), yet little research examines the underlying neural mechanisms (8). Indeed, while many behavioral studies document the development of emotion regulation (9,10), neuroimaging research has just begun to elucidate the maturation of brain systems supporting such capacity (11,12). For example, the protracted development of the prefrontal cortex (PFC) has been linked to age-related improvements in attention shifting and cognitive control, which can modulate affective arousal (11–14). While agerelated brain mechanisms have been examined in some clinical populations (e.g., anxiety and depression) (15,16), little work is available in irritability (8,17,18).
Few studies have utilized frustration paradigms in youth with irritability; those that do report neural dysfunction in PFC and anterior cingulate cortex (ACC), striatum, amygdala, and parietal cortex (19–22). However, the sample sizes of these studies are insufficiently large to generate clear conclusions (23). To address this issue, we recruited a relatively large sample of 195 youth. Moreover, no prior fMRI research has dissociated neural responses to a frustrating event from the impact of frustration on the neural mechanisms mediating performance on a subsequent cognitive trial. Here, we examine the neural response to frustration and the impact of frustration on attention orienting. We define the latter as the ability to disengage attention from its current focus, move attention to a selected alternative target, and direct attention to that target (24). We chose an attention orienting task that engages frontal systems (e.g., ventral attention network) known to mediate this process (14) and adapted a frustrating task used previously (19) to track adjustments in this brain system following frustration. The task induces frustration by falsely informing subjects that they have committed errors; given the critical role of the executive attention system in adapting to errors (14), this system may thus be important in the context of frustration. Also of note, recent work has implicated attention orienting (to threat) as a potential mechanism of irritability (1, 2, 25).
Taken together, we examined associations between irritability, measured dimensionally, and neural activations during a frustrating attention orienting task. Specifically, we studied a transdiagnostic clinical sample of 195 youth with varying levels of irritability. Based on prior work (19–22), we hypothesized that irritability would be associated with perturbed activation in frontal-striatal-amygdala regions during feedback processing and during attention orienting following frustrating feedback. Additionally, given the protracted nature of PFC development (12,13), we hypothesized that associations between irritability and activation in this region would be moderated by age.
Methods
Participants
The sample included 195 8–18 year-olds (mean age=12.9, SD=2.3) with well-distributed irritability levels and a mean above the cutoff for severe irritability (26). Participants had primary diagnoses of DMDD (characterized by severe, chronic irritability; n=52), anxiety disorders (n=42), attention-deficit/hyperactivity disorder (ADHD; n=40), or no disorder (n=61) (Table 1, Supplement eTables 1 & 2). They were recruited from National Institute of Mental Health (NIMH) clinics between February 2012 and July 2016. On the Children’s Global Assessment Scale (CGAS) (27), 58% of patients had a score ≤60, indicating at least “some noticeable problems” in several areas. Most patients were seeking or receiving treatment; 48% were medicated, and half of these were taking ≥2 types of medications. Some patients with DMDD were in an inpatient treatment trial; patients with anxiety disorders were in an outpatient treatment trial. This study was approved by the NIMH IRB, and written consent/assent from parents/children was obtained. Exclusion criteria included IQ<70, pervasive developmental or neurological disorders, substance abuse within the past two months, or lifetime history of psychosis, conduct disorder, and unstable and/or chronic medical illness. See Supplement eMethods 1 for detailed diagnostic and clinical assessments and additional inclusion and exclusion criteria for the anxious group.
Table 1.
Sample Characteristics
| N (%) or Mean (SD) | |
|---|---|
| Age, mean (SD), y | 12.87 (2.35) |
| Gender, n (%) a | 98 (50.30) |
| IQ, mean (SD) b | 111.82 (13.22) |
| SES, mean (SD) c | 32.03 (17.07) |
| Motion, mean (SD) d | 0.12 (0.07) |
| CGAS (past 6 months), mean (SD) e | 57.58 (12.39) |
| Dimensional Measures, mean (SD) | |
| ARI | 3.07 (2.68) |
| SCARED | 16.55 (11.40) |
| CPRS | 59.48 (14.05) |
| Primary Diagnosis, n (%) | |
| DMDD | 52 (26.67) |
| ADHD | 40 (20.51) |
| Anxiety | 42 (21.54) |
| No diagnosis | 61 (31.28) |
| Medications, n (%) | |
| Stimulants | 45 (23.08) |
| Anti-depressants | 31 (15.90) |
| Anti-psychotics | 10 (5.13) |
Abbreviations: ADHD = Attention-Deficit/Hyperactivity Disorder; ARI = Affective Reactivity Index; CGAS = Children’s Global Assessment Scale; CPRS = Conners’ Parent Rating Scale; DMDD = Disruptive Mood Dysregulation Disorder; SCARED = Screen for Child Anxiety Related Emotional Disorders; SES = Socioeconomic status.
Coded as 0 (male) and 1 (female); n (%) is for the male.
Measured by the Wechsler Abbreviated Scale of Intelligence. Missing data for 1 participant.
Measured by the Hollingshead 2-factor index. Missing data for 25 participants.
Calculated as the mean Euclidean distance of framewise volume shift after censoring.
Data were collected for patients only. Missing data for 13 patients.
Measures
We assessed irritability using parent- and child-reports on the Affective Reactivity Index (ARI) (28). To control for co-occurring anxiety and ADHD symptoms, we collected parent- and child-reports on the Screen for Child Anxiety Related Emotional Disorders (SCARED) and parent-report on the Conners’ Parent Rating Scale-Revised: Long Form (CPRS-R: L). Total scores from child- and parent-reports were averaged for the ARI and SCARED. The ADHD-Index T-score from the CPRS was used to index ADHD symptoms. See Supplement eFigure 1 for participant distribution (by diagnosis) along these three symptom dimensions. For >90% of the sample, these measures were collected within three months of scanning. The three-month window was selected based on the stability of the measures and to maximize the sample size. These measures have been shown to be highly stable across time periods longer than three months (e.g., 28; Supplement eMethods 1).
fMRI Paradigm
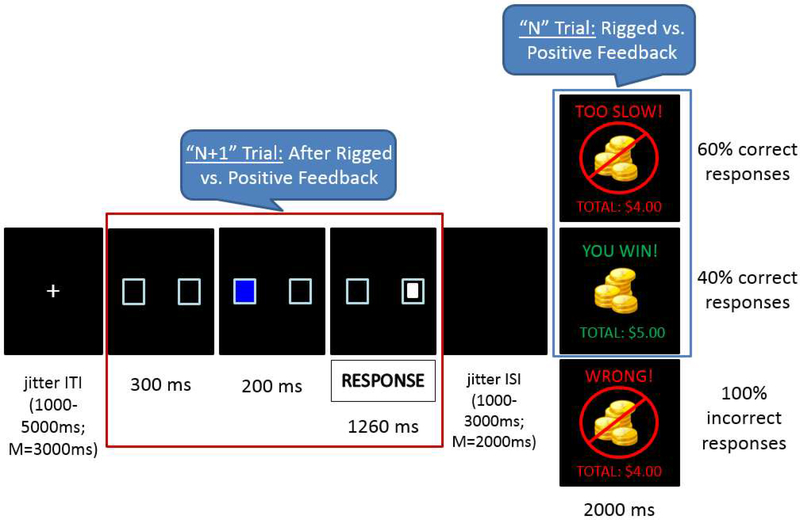
Participants completed a frustrating attention task, the Affective Posner 2 paradigm (29). This was adapted from a prior fMRI study (19) and demonstrates good reliability and validity (29). Participants were asked to identify a target following a cue by button press (left or right). For 75% of trials, the target appeared in the same location as the cue (valid trials); for 25% of trials, the target appeared in the opposite location (invalid trials). The task consisted of two non-frustration runs during which participants received accurate/positive feedback and two frustration runs during which they received rigged or positive feedback (60% and 40% of correct trials, respectively); each run lasted 8 minutes (Figure 1, Supplement eFigure 2). Imaging analyses focused on the two frustration runs. Group-level analyses were done separately for the feedback and attention portions of the task, which were separated by jitter (1000–3000ms with an average of 2000ms; Figure 1). The feedback portion (Figure 1, blue square) probed neural activity during processing of rigged vs. positive feedback. The attention portion (“N+1 trial”; Figure 1, red square) assessed neural activity during the attentional event following rigged vs. positive feedback. At the end of each run, participants rated their feelings of unhappiness and frustration on 9-point Likert scales. For more details regarding task procedures, see Supplement eMethods 2.
Figure 1 legend:
Trial Structure during Frustration Runs of the Affective Posner 2 Task
Note. ITI = inter-trial interval; ISI = inter-stimulus interval. In frustration runs, 60% of correct responses were followed by rigged feedback (“TOO SLOW”), and 40% of correct responses were followed by positive feedback (“YOU WIN”). All incorrect responses were followed by negative feedback (“WRONG”). Imaging analyses focused on the “N+1 trial” (red square) and the “feedback” (blue square) portions of the task. Neural responses for the “N+1 trial” were modeled from the onset of the two boxes for 2 seconds; neural responses for the feedback portion were modeled for the whole duration of the feedback stimulus (2000 ms). Significant associations with irritability emerged from the “N+1 trial” i.e., the attentional event following rigged vs. positive feedback (red square).
Imaging Acquisition
Neuroimaging data were acquired on a 3-T General Electric scanner using an 8channel head coil. A high-resolution anatomical scan (1-mm slices, 3-dimensional spoiled gradient-echo, 7° flip angle, minimum full echo time, 256×256 matrix, 25.6cm field of view) and gradient echo-planar imaging images were collected (repetition time [TR]=2300ms, echo time=25ms, 24cm field of view, voxel size=2.5,2.5,3 mm, 206 volumes per run, flip angle=75° [n=134] or 90° [n=61]; Supplement eMethods 3).
Imaging Preprocessing and Individual Analysis
Data were analyzed using Analysis of Functional NeuroImages (AFNI). Preprocessing included despiking, temporal alignment to the first acquired slice, coregistration, smoothing, masking, and intensity scaling. TR pairs with a Euclidean norm motion derivative >1mm were censored during linear regression. A general linear model estimated voxelwise blood oxygen level-dependent signal change (Supplement eMethods 3 and 4).
Data Analyses
Behavioral and post-hoc imaging analyses were conducted in SPSS. For behavioral results (frustration and unhappiness ratings, accuracy, reaction time), see supplement (eResults 1). Group-level whole-brain activation analyses used AFNI’s 3dMVM, a multivariate model-based analysis of covariance (ANCOVA) appropriate for our fMRI data and study design (30). Analyses examined the effects of ARI, Age, and ARI x Age, with SCARED, CPRS, and motion (for imaging data) as covariates. All variables were continuous and mean-centered to reduce multicollinearity due to testing of the interaction term (ARI x Age). Correlations between dimensional measures (rs<.54; Supplement eTable 2) had an acceptable tolerance in the model with ARI, Age, ARI x Age, SCARED, CPRS, and motion (variance inflation factors≤1.46).
Imaging data.
Imaging analyses focused on frustration runs because only these runs contained both positive and rigged feedback. We did not directly compare nonfrustration and frustration runs (e.g., on positive feedback) because there was a fundamental difference in “baselines” i.e., the baselines in frustration runs were likely more saturated and elevated. However, we also conducted a whole-brain analysis for non-frustration runs only and, relative to baseline, found no significant associations between irritability and neural activation during either positive feedback or attention orienting following positive feedback.
Only valid, correct trials were included, given insufficient numbers of other trial types. Separate analyses were conducted for the feedback portion of the “N” trial and the attentional portion of the “N+1 trial” (Figure 1). For the feedback portion of the “N” trial, an ARI × Age × Condition (rigged vs. positive feedback) ANCOVA was conducted to assess activation during processing of rigged vs. positive feedback and how it varied with irritability and age. For the “N+1 trial,” an ARI × Age × Condition (after rigged vs. positive feedback) ANCOVA was conducted to assess activation during the attentional event following rigged vs. positive feedback and how it varied with irritability and age.
Analyses used a whole-brain gray-matter mask, including voxels where data existed for ≥90% of participants, voxelwise .001 p-values, and multiple-testing correction of α=.05 via Monte Carlo cluster-size simulation. Using methods designed recently to address concerns regarding inflated false positive rates (31), 703 mm3 was set as the cluster size surviving whole-brain correction. At this threshold, we observed a large cluster of 68000 mm3 for the 3-way ARI × Age × Condition interaction and a cluster of 86281 mm3 for the 2-way ARI × Condition interaction from the N+1 analyses. To facilitate interpretation, we extracted clusters using a more stringent voxelwise p=.0001 (clusters ≥203 mm3; see Table 2). Using this threshold, we created a conjunction map of the significant 3-way and 2-way interactions and calculated the shared voxels i.e., voxels that showed significant effects for both the 3-way ARI × Age × Condition and 2-way ARI × Condition interactions. Only 8.4% of the voxels were shared, suggesting that most voxels that showed a significant ARI × Condition interaction were not moderated by age. To deconstruct significant interactions, mean activation across voxels in significant clusters were extracted via AFNI’s 3dROIstat for follow-up analyses in SPSS. For the “N” trial analyses, no significant clusters were observed i.e., ARI, Age, and their interaction were not associated with activation during processing of rigged vs. positive feedback.
Table 2.
N+1 Trial: Effect of ARI × Age × Condition and ARI × Condition from WholeBrain Activation Analysisa
| Regionsb | Size (mm3) | Peak (x, y, z)c | Analysisd |
Correlation (r)e | ||
|---|---|---|---|---|---|---|
| F1,188 | p value | ηp2 | ||||
| ARI × Age × Condition | ||||||
| R cuneus | 2563 | (9, −79, 16) | 25.25 | <.001 | .12 | – |
| R superior parietal lobule | 2563 | (31, −64, 44) | 28.51 | <.001 | .13 | – |
| L precuneus/cuneus | 1469 | (−24, −69, 24) | 22.91 | <.001 | .11 | – |
| L medial frontal gyrus/ACC | 1469 | (−9, 44, 26) | 23.94 | <.001 | .11 | – |
| R pre- and post-central gyrus | 1359 | (39, −19, 49) | 25.62 | <.001 | .12 | – |
| L precuneus | 1047 | (−14, −66, 41) | 25.15 | <.001 | .12 | – |
| L middle frontal gyrus | 641 | (−34, 11, 41) | 20.80 | <.001 | .10 | – |
| R middle occipital gyrus | 625 | (29, −84, 21) | 25.18 | <.001 | .12 | – |
| R post-central gyrus | 500 | (19, −29, 66) | 22.25 | <.001 | .11 | – |
| R superior temporal gyrus | 469 | (51, −51, 21) | 20.33 | <.001 | .10 | – |
| R superior frontal gyrus | 438 | (11, 54, 29) | 21.70 | <.001 | .10 | – |
| R lingual/fusiform gyrus | 422 | (21, −61, −4) | 21.18 | <.001 | .10 | – |
| L pre-central gyrus | 391 | (−34, −9, 44) | 21.34 | <.001 | .10 | – |
| R middle/superior frontal gyrus | 375 | (24, 24, 41) | 19.23 | <.001 | .09 | – |
| R middle frontal gyrus | 313 | (24, −6, 44) | 19.75 | <.001 | .10 | – |
| R fusiform gyrus | 297 | (36, −59, −14) | 19.41 | <.001 | .09 | – |
| L superior parietal lobule | 281 | (−29, −61, 44) | 20.58 | <.001 | .10 | – |
| L medial frontal gyrus | 234 | (−6, −11, 51) | 19.04 | <.001 | .09 | – |
| L superior frontal gyrus | 203 | (−9, 14, 54) | 20.03 | <.001 | .10 | – |
| ARI × Condition | ||||||
| L & R cingulate gyrus, R superior frontal gyrus | 13594 | (9, 19, 41) | 34.81 | <.001 | .16 | .40 |
| R middle frontal gyrus | 5844 | (36, 16, 41) | 31.63 | <.001 | .14 | .38 |
| L middle frontal gyrus | 2469 | (−31, 21, 34) | 25.85 | <.001 | .12 | .35 |
| R caudate, thalamus | 2422 | (11, −19, 19) | 27.72 | <.001 | .13 | .36 |
| R dorsolateral prefrontal cortex | 1422 | (46, 31, 26) | 29.23 | <.001 | .14 | .37 |
| R cuneus | 1250 | (9, −76, 19) | 23.65 | <.001 | .11 | .33 |
| R precuneus | 1094 | (19, −69, 41) | 25.68 | <.001 | .12 | .35 |
| L middle frontal gyrus | 1047 | (−34, −1, 46) | 22.33 | <.001 | .11 | .33 |
| R inferior frontal gyrus | 594 | (54, 26, 6) | 28.29 | <.001 | .13 | .36 |
| L pre- and post-central gyrus | 531 | (−39, −19, 39) | 20.81 | <.001 | .10 | .32 |
| L parahippocampal gyrus | 469 | (−16, −39, −4) | 23.86 | <.001 | .11 | .34 |
| L caudate | 453 | (−9, 6, 21) | 21.53 | <.001 | .10 | .32 |
| R superior temporal gyrus | 406 | (41, −49, 19) | 21.37 | <.001 | .10 | .32 |
| R pre-central gyrus | 344 | (56, 6, 6) | 21.29 | <.001 | .10 | .32 |
| L pre-central gyrus | 266 | (−61, −1, 14) | 20.85 | <.001 | .10 | .32 |
| L cingulate gyrus | 203 | (−6, −16, 41) | 20.77 | <.001 | .10 | .32 |
| L superior frontal gyrus | 203 | (−6, 11, 59) | 19.68 | <.001 | .10 | .31 |
Abbreviations: ACC = Anterior Cingulate Cortex; ARI = Affective Reactivity Index; L = Left; R = Right.
The Condition effect refers to the attention portion of the trial immediately after receiving rigged vs. positive feedback (i.e., the N+1 trial).
At voxelwise p=.001, the largest significant cluster was of 86281 mm3. To facilitate interpretation, we extracted clusters using the more stringent voxelwise p=.0001. At this threshold, clusters ≥ 203 mm3 survive whole-brain correction at α=.05. Region comprising the greatest portion of the cluster extent.
Coordinates are in Talairach space.
Post-hoc analysis of covariance (ANCOVA) on mean BOLD (blood oxygenation leveldependent) signal for extracted cluster.
Correlations between ARI and the difference in brain activation after receiving rigged vs. positive feedback (rigged minus positive), after adjusting for motion and symptoms of anxiety and attention-deficit/hyperactivity disorder. Note that these correlations may be inflated given that they were computed based on extracted signal change from voxels that survived whole-brain correction (40).
To address concerns regarding threshold-based cluster forming and replicability of imaging findings, we re-analyzed our data using the Threshold-Free Cluster Enhancement approach (32), with familywise error rate correction level of 0.05, via permutation testing (eResults 8 and eFigure 9). Results were largely consistent with the original analysis in AFNI, except that two small clusters for the ARI × Condition effect (left caudate and pre-central gyrus) became non-significant (right caudate remains significant).
Results
Imaging Data
Significant findings emerged from the N+1 analysis, in the comparison of neural activity occurring after rigged vs. positive feedback during the frustration runs (Figure 1, red square). Specifically, we report interactions involving Condition (after rigged vs. positive feedback) and ARI (dimensional measure of irritability) i.e., ARI × Age × Condition and ARI × Condition.
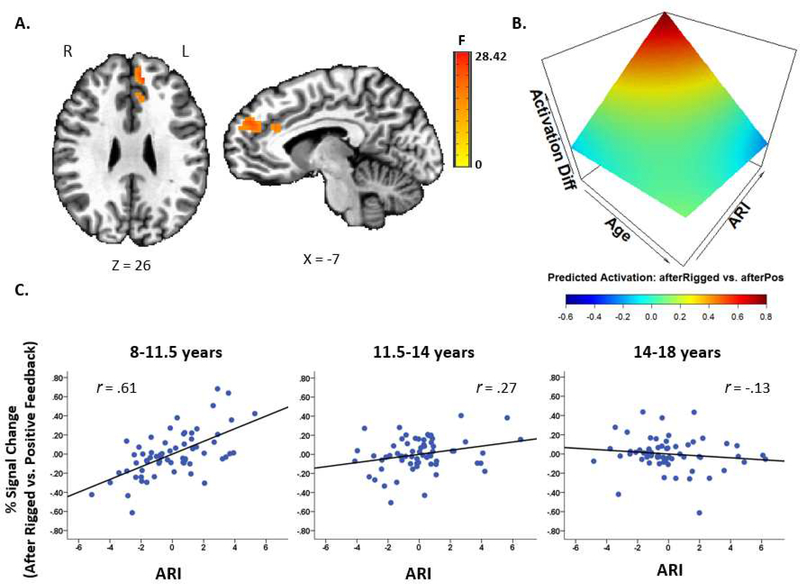
ARI × Age × Condition.
During the attentional event immediately following rigged vs. positive feedback, activation in several posterior and frontal regions varied with levels of irritability and as a function of participant age. These regions include cuneus, precuneus, superior parietal lobule, medial frontal gyrus, and ACC (Table 2, Figure 2, Supplement eFigure 3). Across these regions, higher irritability was more strongly related to increased activation in younger relative to older youths. Specifically, higher irritability was significantly related to increased activation in young children (aged 8–11.5 years) and younger adolescents (aged 11.5–14 years), with the strongest correlation in young children. However, irritability was not related to activation in older adolescents (aged 14–18 years) (Figure 2 depicts finding in medial PFC/ACC).
Figure 2 legend:
Age Moderating the Association between Irritability and Activation in Medial Prefrontal Cortex/Anterior Cingulate Cortex during Attention Orienting Following Rigged vs. Positive feedback
A. Left medial prefrontal cortex extending to the anterior cingulate cortex from the whole-brain N+1 trial activation analysis. During the attentional portion of the trial, activation after receiving rigged vs. positive feedback varied with irritability (i.e., Affective Reactivity Index, ARI, scores) and age.
B. Associations among ARI, age, and brain activation (all variables were continuous). The BOLD % signal change for this cluster was extracted for each condition (the N+1 trial after rigged and after positive feedback) for each subject. These values were entered in the same ANCOVA model (controlling for symptoms of anxiety and attention-deficit/hyperactivity disorder and motion) as in the main analysis, and predicted % signal changes were generated. The differences between the predicted % signal changes after rigged vs. positive feedback were plotted. The 3-D graph shows that, after receiving rigged vs. positive feedback, younger youth with high irritability exhibited increased activation.
C. Partial regression plots (controlling for symptoms of anxiety and attention-deficit/hyperactivity disorder and motion) by age tertiles (n=65 for each age group) depict individual data points and the association between ARI (mean-centered) and the % signal change difference between trials occurring after rigged vs. after positive feedback. Age was treated as a continuous variable in the analyses. The age tertiles here were used for visualization only. Higher irritability was more strongly related to increased activation on this contrast in early childhood (age 8–11.5 years) than in early adolescence (age 11.5–14 years); irritability was not related to activation in late adolescence (age 14–18 years). Note that these correlations may be inflated given that they were computed based on extracted signal change from voxels that survived whole-brain correction (40).
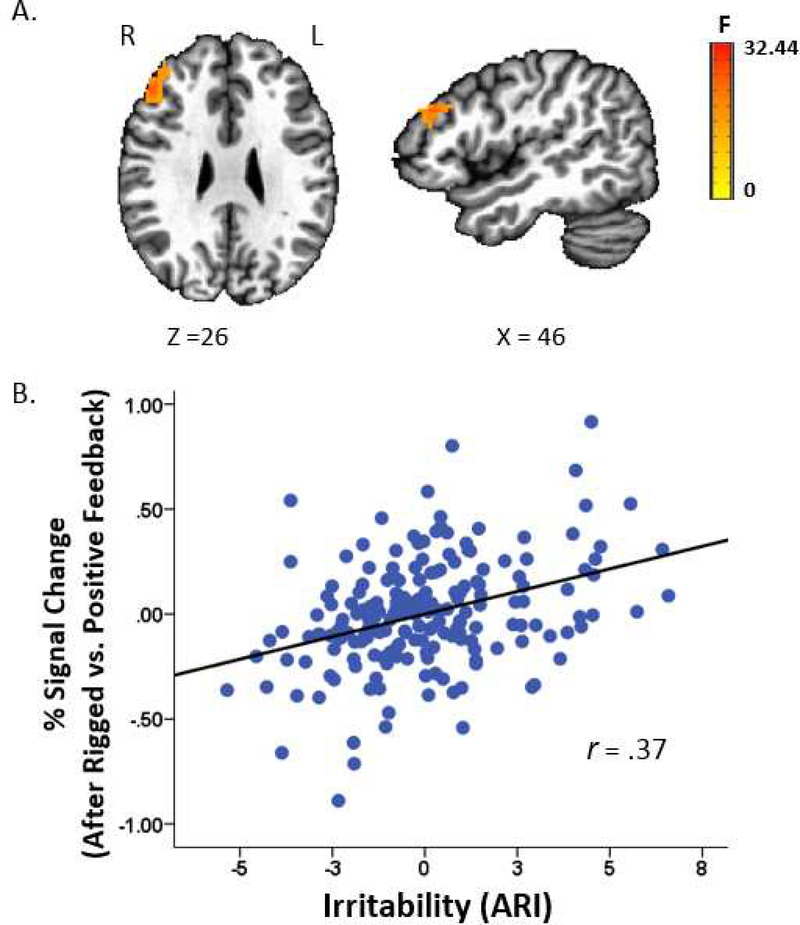
ARI × Condition.
This 2-way interaction yielded significant findings in bilateral cingulate gyrus, middle frontal gyrus, caudate, dorsolateral prefrontal cortex (dlPFC), cuneus, precuneus, and inferior frontal gyrus (IFG) (Table 2, Figure 3, Supplement eFigure 4). Most (91.6%) significant voxels in these regions did not overlap with the significant voxels for the 3-way interaction described above. The few overlapping regions included bilateral cingulate gyrus, middle frontal gyrus, cuneus, and precuneus. Given that these regions were qualified by a 3-way interaction of ARI × Age × Condition, we do not interpret them here. Regions showing a significant ARI × Condition effect without a qualifying 3-way interaction included dlPFC (Figure 3), caudate (extending to thalamus), and IFG, among others (Table 2, Supplement eFigure 4). Across these regions, higher irritability was related to increased activation following rigged vs. positive feedback.
Figure 3 legend:
Association between Irritability and Dorsolateral Prefrontal Cortex (dlPFC) Activation during Attention Orienting Following Rigged vs. Positive feedback
A. dlPFC from the whole-brain N+1 trial activation analysis. During the attentional portion of the trial, activation after receiving rigged vs. positive feedback varied with irritability (i.e., Affective Reactivity Index, ARI, scores).
B. Partial regression plots (controlling for symptoms of anxiety and attention-deficit/hyperactivity disorder and motion) depicted individual data points and the association between ARI (mean-centered) and the % signal change difference between trials occurring after rigged vs. positive feedback. Higher irritability was related to more activation on this contrast. Note that these correlations may be inflated given that they were computed based on extracted signal change from voxels that survived whole-brain correction (40).
Post-hoc Analyses: Depressive Symptoms, Frustration and Unhappiness Ratings, Medication, DSM-5 Diagnosis, and Gender
Given the longitudinal link between childhood irritability and depression later in life (3), we evaluated the effect of depression by conducting whole-brain analyses with depressive symptoms (measured by self-rated Children’s Depression Inventory) as the main dimension. There were no significant associations between depressive symptoms and neural activations (threshold voxelwise p=.001, cluster extent ≥703 mm3). Depressive symptoms were evaluated this way and not treated as a covariate in the main analyses (as anxiety and ADHD symptoms were) because 28 participants had missing data.
We also conducted analyses to examine the effects of “state irritability” measured by self-ratings of frustration and unhappiness obtained at the end of each of the two frustration runs (Supplement eResults 2). The only significant finding was a positive association between unhappiness and activation in the right superior temporal gyrus during processing of rigged vs. positive feedback. These analyses have limitations because of the problems associated with the state measures (Supplement eResults 2). Nonetheless, they suggest that the neural substrates underlying transient, subjective feelings of frustration and unhappiness may differ from the neural substrates mediating trait irritability.
We evaluated the confounding effect of medications by iteratively excluding participants by medication class (stimulants, anti-depressants, antipsychotics; Supplement eTable 3 and eTable 4). All significant findings remained. Also, analyses comparing medicated (n=25) vs. unmedicated (n=100) participants on the day of the scan did not reveal significant between-group differences on the imaging findings.
Categorical analyses using diagnoses instead of symptom dimensions yielded null results in whole-brain activation but a few findings in functional connectivity (for details, see Supplement eResults 3).
We also examined the moderating effect of gender and found that most of the main imaging results were not moderated by gender. However, in inferior parietal lobule, pre- and post-central gyrus, and insula, irritability was related to increased activation in younger boys and decreased activation in older boys (Supplement eResults 4).
Additional Region-of-Interest and Functional Connectivity Analyses
Region-of-interest analyses in amygdala and striatum revealed positive associations between ARI and striatal activity during the N+1 trial but not during feedback (age moderated some associations; Supplement eResults 5). We also analyzed functional connectivity with IFG and amygdala seeds (Supplement eResults 6 & 7, eTable 5 & 6, eFigure 5–8). Notably, we found that higher irritability was related to decreased functional connectivity between left IFG and periaqueductal gray (extending to culmen) during the N+1 trial (Supplement eFigure 6).
Discussion
This study investigates the neural correlates of attention orienting following frustration in a large, transdiagnostic sample i.e., 195 youth with varying levels of irritability. We used a novel paradigm to model the frustration that irritable youth are prone to experience, particularly when rewards are withheld and they are frustrated and asked to adjust their behaviors (e.g., stop playing video games and start homework instead). We found that irritability was associated with neural activation during attention orienting following a frustrating event, but not during processing of the frustrating feedback itself. Two specific findings emerged. First, higher irritability was related to increased activation in multiple frontal-striatal regions independent of age. Second, in other regions, associations between irritability and activation were moderated by age, such that associations were stronger in younger relative to older children. These findings suggest that promising treatments for irritability may target frontal-striatal regions and that interventions could be prioritized for younger youth with high irritability.
Irritability was associated with dysfunction in PFC, ACC (20–22,33,34), and striatum (19,33). This is consistent with previous research in youth and adults with irritability or related phenotypes (anger, trait aggression) (19–22,33,34). Specifically, while engaged in the attentional part of the task after being frustrated, highly irritable youth exhibited increased activation in multiple frontal regions (ACC, dlPFC, IFG) implicated in cognitive control, executive attention, and attention orienting (35,36). Highly irritable youth also showed increased activation in striatum, which has a regulatory influence on cortex and is involved in motor and eye-movements and in set shifting (37).
Notably, irritability was not associated with performance deficits (e.g., poor accuracy, slower reaction time). Thus, the observed increased activation may reflect a compensatory mechanism i.e., compared to healthy youth, irritable youth may require more robust recruitment of these regions following frustration to regulate their negative affect, focus on the task at hand, and meet task demands. Importantly, our finding is best explained by irritability, and not better attributed to co-occurring anxiety, ADHD, or depressive symptoms. Furthermore, we found no associations between irritability and activation during non-frustration runs. This observation suggests that trait-specific neural correlates manifest in irritable youth when they are frustrated. Such context specificity is consistent with our event-related analysis contrasting activity during performance of the attention orienting task following frustrating vs. non-frustrating feedback. Because of the insufficient number of incorrect trials, we were unable to examine the neural responses to errors (where reward is omitted and not expected). An interesting and important question is whether irritability has similar associations with responses to errors, responses to “pure” frustrative non-reward (i.e., where reward is expected and omitted because of changed contingencies), and responses to frustrative non-reward due to deception (rigged feedback).
Despite comparable performance on a simple attention task, irritable youth exhibited heightened frontal activation following frustration, suggesting a requirement for greater PFC engagement to adjust to frustration and achieve performance comparable to that of less irritable youth. Many everyday tasks (e.g., schoolwork, homework, or transitions between activities) are much more cognitively demanding than laboratory tasks, such as the one used here. Therefore, inefficiency in systems that facilitate postfrustration adjustment could lead irritable youth to struggle in daily life. Moreover, while many irritable youth in our sample were medicated, the impact of medications on their brain function was not evident in our analysis. This suggests that current medications may fail to normalize the particular neural dysfunction reported here. There is clearly a need for new treatments including non-pharmacological approaches (e.g. real-time fMRI neurofeedback or transcranial magnetic stimulation targeting frontal-striatal regions). Additionally, given that neural dysfunction associated with irritability was found during attentional processes following frustration, intervention efforts might target strategies that help irritable children allocate attention effectively.
Age moderated the association between irritability and brain activation during attention orienting following frustration in several frontal and posterior regions (ACC, medial frontal gyrus, cuneus, precuneus). Specifically, higher irritability was related to increased activation in children and younger adolescents but not older adolescents; the association was particularly strong in young children. This finding is inconsistent with the only previous study that examined the interacting effect of age and irritability and found that, as age increased, higher irritability was associated with more frontal-striatalthalamic activation (17). This discrepancy could be explained by differences in sample size (N=30 vs. 195 here); sample characteristics e.g., age (4–12 vs. 8–18 years here) and the nature of the sample (non-clinical vs. clinical sample here); and fMRI paradigm (viewing of emotionally- or neutrally-valenced video clips vs. frustrating cued-attention task here). Young and highly irritable children may be most susceptible to affectivelycharged stimuli and may have the greatest difficulty disengaging attention from negatively-arousing stimuli. While these youth did not show performance deficits, their ability to perform the task despite immature neural circuitry may have required prolonged and inefficient computational processes that generated increased regional neural activity (38). Indeed, the increased ACC activation seen in young children, as compared to older youth or adults, may reflect neural inefficiency in cognitive control (38).
Contrary to some previous studies, we did not find an association between irritability and amygdala activation in response to a frustrating event (19,34). This could be due to differences in frustration paradigms i.e., block (34) vs. event-related design and/or no jitter (19) vs. jitter between attentional and feedback portions of the task (the latter allows for separation of attention orienting and feedback processing). Alternatively, the unreliability of amygdala activation may hamper replication (39). Notably, our null amygdala finding is consistent with a recent study that also adopted a dimensional approach to examine irritability and brain function during frustration (20).
Limitations
First, our findings may apply only to the disorders sampled (DMDD, anxiety disorders, ADHD) and not to other disorders (e.g., depression, bipolar disorder) where irritability is also common. Second, given the high correlation between chronological age and puberty status, we used age as a proxy for development. Future work is needed to directly examine the effect of puberty. Third, although our cross-sectional design is a helpful starting point to understand brain function over development, only longitudinal studies can elucidate individual differences in developmental trajectories. Fourth, as in most studies with severely impaired youth, medication may confound the results; however, post-hoc analyses do not support this. Finally, this study used raw, reported scores of irritability symptoms. Other phenotyping approaches (e.g., latent variable modeling) may provide additional perspectives.
Conclusions
In a sample characterized by a mix of mood, anxiety, and ADHD symptoms in the clinically-impairing range, we found unique associations of irritability with neural systems mediating attention orienting, top-down regulation of emotions, and motor execution following frustrative non-reward. These associations were not attributed to co-occurring ADHD, anxiety, or depressive symptoms. While most associations were independent of age, dysfunction in ACC and some posterior regions was more pronounced in young children with irritability. The neural dysfunction did not seem to be altered by medications, highlighting a need for new treatments, including nonpharmacological approaches, that target the common and impairing symptom of irritability. Since associations between irritability and brain function were found during attentional processes following frustration, intervention efforts might target strategies helping irritable children regulate the negative affect and arousal elicited by frustrating events and flexibly shift their attention to focus on the task at hand.
Supplementary Material
Acknowledgements
We thank the children and families who participated in this study as well as the staff of the Emotion and Development Branch and the Scientific and Statistical Computing Core at the NIMH. In particular, we would like to thank Anderson Winkler, MD, DPhil (Emotion and Development Branch) for assistance on Permutation Analysis of Linear Models (PALM) and threshold-free cluster enhancement analysis; Dan Barlow for programming support; and Gang Chen, PhD, for imaging statistics guidance. This research used the computational resources of the NIH HPC Biowulf cluster (http://hpc.nih.gov). All authors have no conflicts of interest or outside financial support to report.
Funding/Support: This study was supported by the Intramural Research Program of the NIMH, and it was conducted under projects ZIA-MH002778 (clinical protocol NCT00006177), ZIA-MH-002781 (NCT00018057), and ZIA44 MH002786 (NCT00025935).
Contributor Information
Wan-Ling Tseng, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Christen M. Deveney, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Joel Stoddard, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Katharina Kircanski, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Anna E. Frackman, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Jennifer Y. Yi, Mses., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Derek Hsu, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Elizabeth Moroney, Mses., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Laura Machlin, Mses., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Laura Donahue, Mses., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Alexandra Roule, Mses., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Gretchen Perhamus, Mses., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Richard C. Reynolds, Mr., Scientific and Statistical Computing Core, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Roxann Roberson-Nay, Dr., Department of Psychiatry and the Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, Virginia
John M. Hettema, Dr., Department of Psychiatry and the Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, Virginia
Kenneth E. Towbin, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Argyris Stringaris, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Daniel S. Pine, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Melissa A. Brotman, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
Ellen Leibenluft, Dr., Emotion and Development Branch, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, Bethesda, MD
References
- 1.Brotman MA, Kircanski K, Stringaris A, et al. : Irritability in youth: A translational model. Am J Psychiatry 2017; 174:520–532 [DOI] [PubMed] [Google Scholar]
- 2.Leibenluft E: Pediatric irritability: A systems neuroscience approach. Trends Cogn Sci 2017; 21:277–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vidal-Ribas P, Brotman MA, Valdivieso I, et al. : The status of irritability in psychiatry: A conceptual and quantitative review. J Am Acad Child Adolesc Psychiatry 2016; 55:556–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roy AK, Lopes V, Klein RG: Disruptive mood dysregulation disorder (DMDD): A new diagnostic approach to chronic irritability in youth. Am J Psychiatry 2014; 171:918–924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stringaris A, Vidal-Ribas P, Brotman MA, et al. : Practitioner review: Definition, recognition, and treatment challenges of irritability in young people. J Child Psychol Psychiatry 2018; 59:721–739 [DOI] [PubMed] [Google Scholar]
- 6.Amsel A: The role of frustrative nonreward in noncontinuous reward situations. Psychol Bull 1958; 55:102–119 [DOI] [PubMed] [Google Scholar]
- 7.Wakschlag LS, Estabrook R, Petitclerc A, et al. : Clinical implications of a dimensional approach: The normal:abnormal spectrum of early irritability. J Am Acad Child Adolesc Psychiatry 2015; 54:626–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pagliaccio P, Pine DS, Barch DM, et al. : Irritability trajectories, cortical thickness, and clinical outcomes in a sample enriched for preschool depression. J Am Acad Child Adolesc Psychiatry 2018; 57:336–342.e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.John OP, Gross JJ: Healthy and unhealthy emotion regulation: Personality processes, individual differences, and life span development. J Pers 2004; 72:1301–1333 [DOI] [PubMed] [Google Scholar]
- 10.Posner MI, Rothbart MK, Sheese BE, et al. : Developing attention: Behavioral and brain mechanisms. Adv Neurosci 2014; 2014:405094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen AO, Breiner K, Steinberg L, et al. : When Is an adolescent an adult? Assessing cognitive control in emotional and nonemotional contexts. Psychol Sci 2016; 27:549–562 [DOI] [PubMed] [Google Scholar]
- 12.Ahmed SP, Bittencourt-Hewitt A, Sebastian CL: Neurocognitive bases of emotion regulation development in adolescence. Dev Cogn Neurosci 2015; 15:11–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ordaz SJ, Foran W, Velanova K, et al. : Longitudinal growth curves of brain function underlying inhibitory control through adolescence. J Neurosci 2013; 33:18109–18124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petersen SE, Posner MI: The attention system of the human brain: 20 years later. Annu Rev Neurosci 2012; 35:73–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luby JL, Agrawal A, Belden A, et al. : Developmental trajectories of the orbitofrontal cortex and anhedonia in middle childhood and risk for substance use in adolescence in a longitudinal sample of depressed and healthy preschoolers. Am J Psychiatry, in press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tamnes CK, Walhovd KB, Torstveit M, et al. : Performance monitoring in children and adolescents: A review of developmental changes in the error-related negativity and brain maturation. Dev Cogn Neurosci 2013; 6:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karim HT, Perlman SB: Neurodevelopmental maturation as a function of irritable temperament: Insights from a naturalistic emotional video viewing paradigm. Hum Brain Mapp 2017; 38:5307–5321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wakschlag LS, Perlman SB, Blair RJ, et al. : The neurodevelopmental basis of early childhood disruptive behavior: Irritable and callous phenotypes as exemplars. Am J Psychiatry 2018; 175:114–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deveney CM, Connolly ME, Haring CT, et al. : Neural mechanisms of frustration in chronically irritable children. Am J Psychiatry 2013; 170:1186–1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grabell AS, Li Y, Barker JW, et al. : Evidence of non-linear associations between frustration-related prefrontal cortex activation and the normal:abnormal spectrum of irritability in young children. J Abnorm Child Psychol 2018; 46:137–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perlman SB, Jones BM, Wakschlag LS, et al. : Neural substrates of child irritability in typically developing and psychiatric populations. Dev Cogn Neurosci 2015; 14:71–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rich BA, Carver FW, Holroyd T, et al. : Different neural pathways to negative affect in youth with pediatric bipolar disorder and severe mood dysregulation. J Psychiatr Res 2011; 45:1283–1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poldrack RA, Baker CI, Durnez J, et al. : Scanning the horizon: towards transparent and reproducible neuroimaging research. Nat Rev Neurosci 2017; 18:115–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Posner MI, Walker JA, Friedrich FJ, et al. : Effects of parietal injury on covert orienting of attention. J Neurosci 1984; 4:1863–1874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kircanski K, White LK, Tseng WL, et al. : A latent variable approach to differentiating neural mechanisms of irritability and anxiety in youth. JAMA Psychiatry 2018; 75:631–639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kircanski K, Zhang S, Stringaris A, et al. : Empirically derived patterns of psychiatric symptoms in youth: A latent profile analysis. J Affect Disord 2017; 216:109–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaffer D, Gould MS, Brasic J, et al. : A children’s global assessment scale (CGAS). Arch Gen Psychiatry 1983; 40:1228–1231 [DOI] [PubMed] [Google Scholar]
- 28.Stringaris A, Goodman R, Ferdinando S, et al. : The Affective Reactivity Index: A concise irritability scale for clinical and research settings. J Child Psychol Psychiatry 2012; 53:1109–1117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tseng W-L, Moroney E, Machlin L, et al. : Test-retest reliability and validity of a frustration paradigm and irritability measures. J Affect Disord 2017; 212:38–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen G, Adleman NE, Saad ZS, et al. : Applications of multivariate modeling to neuroimaging group analysis: A comprehensive alternative to univariate general linear model. Neuroimage 2014; 99:571–588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cox RW, Chen G, Glen DR, et al. : FMRI clustering in AFNI: False-positive rates redux. Brain Connect 2017; 7:152–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith SM, Nichols TE: Threshold-free cluster enhancement: Addressing problems of smoothing, threshold dependence and localization in cluster inference. Neuroimage 2009; 44:83–98 [DOI] [PubMed] [Google Scholar]
- 33.Abler B, Walter H, Erk S: Neural correlates of frustration. Neuroreport 2005; 16:669–672 [DOI] [PubMed] [Google Scholar]
- 34.Pawliczek CM, Derntl B, Kellermann T, et al. : Anger under control: Neural correlates of frustration as a function of trait aggression. PLoS One 2013; 8:e78503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MacDonald AW 3rd, Cohen JD, Stenger VA, et al. : Dissociating the role of the dorsolateral prefrontal and anterior cingulate cortex in cognitive control. Science 2000; 288:1835–1838 [DOI] [PubMed] [Google Scholar]
- 36.Corbetta M, Shulman GL: Control of goal-directed and stimulus-driven attention in the brain. Nat Rev Neurosci 2002; 3:201–215 [DOI] [PubMed] [Google Scholar]
- 37.Ravizza SM, Ciranni MA: Contributions of the prefrontal cortex and basal ganglia to set shifting. J Cogn Neurosci 2002; 14:472–483 [DOI] [PubMed] [Google Scholar]
- 38.Luna B, Padmanabhan A, O’Hearn K: What has fMRI told us about the development of cognitive control through adolescence? Brain Cogn 2010; 72:101–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Den Bulk BG,Koolschijn PCMP,Meens PHF, et al. : How stable is activation in the amygdala and prefrontal cortex in adolescence? A study of emotional face processing across three measurements. Dev Cogn Neurosci 2013; 4:65–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vul E, Harris C, Winkielman P, et al. : Puzzlingly high correlations in fMRI studies of emotion, personality, and social cognition. Perspect Psychol Sci 2009; 4:274–290 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.