Abstract
Background
Problematic relationship to eating and food (PREF) captures a broad range of unhealthy eating behaviors. We previously reported higher BMI is associated with PREF and graded by the number of PREF endorsed. In this study, we prospectively examined the association between PREF and metabolic syndrome and diabetes.
Methods
Eight PREF behaviors were assessed and summed to form the PREF score in 3800 black and white adults (age 27–41) in the Coronary Artery Risk Development in Young Adults Study. Diagnoses of incident metabolic syndrome and diabetes were made through 15 years of follow-up. Logistic regression estimated the association with metabolic syndrome. Proportional hazards regression estimated the association with diabetes.
Results
Odds ratio of metabolic syndrome was 1.25 per PREF point through 5 years of follow-up (95% CI: 1.17–1.34) and 1.17 per point from 5 to 10 years of follow-up (95% CI: 1.08–1.27). Hazard of diabetes was 1.20 per PREF point through 15 years of follow-up (95% CI: 1.12–1.28). Both associations attenuated after adjustment for BMI.
Discussion
Among participants with PREF, higher scores associate with metabolic syndrome and diabetes, with partial attenuation after adjustment for BMI. Early identification of PREF in middle-aged adults may reduce the burden of metabolic health outcomes.
Keywords: middle-aged, eating behavior, type 2 diabetes, metabolic syndrome, longitudinal study
INTRODUCTION
It is well-established that obesity causes metabolic health outcomes, including metabolic syndrome and diabetes (Sullivan et al., 2007). In our prior work we reported that problematic eating behaviors, including those that do not qualify as diagnosable eating disorders, were associated with substantially higher BMI (Yoon et al., 2018), but only a handful of studies have investigated the association of metabolic syndrome (Barnes et al., 2011) or diabetes (Raevuori et al., 2015) with these maladaptive eating behaviors. Most studies were limited to either clinical eating disorders (Barnes et al., 2011; Raevuori et al., 2015) or focused on certain eating behaviors (Abraham et al., 2014). Thus the long-term clinical consequences remain unclear of a broad range of eating behaviors that may not qualify as diagnosable eating disorders but that do result in excess BMI.
Thus building on prior studies, the overall purpose of this study was to examine the association between problematic eating behaviors and metabolic syndrome and diabetes. Our expectation was that problematic eating behaviors would be associated with greater risk of incident metabolic syndrome and diabetes and that these associations would be explained by BMI.
SUBJECTS AND METHODS
CARDIA is a longitudinal cohort which was established in 1985–1986 and based in 4 field centers: Birmingham AL, Chicago IL, Minneapolis MN, and Oakland CA. The CARDIA study included5,115 black and white participants aged between 18 to 30 years old at baseline (Friedman et al., 1988) who have been followed-up for 30 years. The response rates for CARDIA Years 2, 5, 7, 10, 15, 20, and 25 were 91, 86, 81, 79, 74, 72, and 72% of survivors, respectively. At each study center, the Institutional Review Board approved the study and written informed consent was obtained from each participant. Excluded from the analyses were those who did not attend the examination in Year 10 (n=1,165) and those who did not answer the Questionnaire on Eating and Weight Patterns-Revised (QEWP-R) when it was self-administered at Year 10 (n=48). In respective analyses of incidence, we further excluded those in whom metabolic syndrome was not assessed in Year 10 (n=28). Depending on the outcome variable, those with prevalent diabetes at Year 10 (n=114) or those with prevalent metabolic syndrome at Year 10 (n=996) were further excluded. Therefore, the incident metabolic syndrome and diabetes through Year 25 as a function of Year 10 PREF were analyzed among 2,878 and 3,788 participants, respectively.
Assessment of Problematic Relationship to Eating and Food (PREF)
Eight constructs related to eating and food were abstracted from the QEWP-R at Year 10 to define problematic relationship to eating and food (PREF) scores and categories (Yoon et al., 2018, Online supplement Table 1). Constructs range from weight concerns and distress about overeating and loss of control to actual overeating, anxiety surrounding food and eating, and compensatory behaviors. Endorsement of each construct was assigned 1 point (maximum 8 points), to represent a composite PREF score showing low to high involvement with these behaviors. PREF scores were further categorized into 6 groups: 0, 1, 2, 3, 4–5, and 6–8 points. While clinical eating disorder diagnosis were not assessed in CARDIA, these problematic eating behaviors may be concerning for health. PREF 6–8 points have been thought to be certainly higher risk, while the risks involved with PREF 1–5 points are less well-characterized.
Metabolic Syndrome Classification
At all CARDIA exams, metabolic syndrome was defined based on the National Cholesterol Education Program Adult Treatment Panel III guidelines (NCEP, 2001), excluding the waist circumference criterion because of its correlation of ~0.9 with BMI. Therefore, we define metabolic syndrome with those with ≥ 2 of the following four criteria: 1) elevated blood pressure, 2) elevated fasting triglyceride, 3) low high density lipoprotein cholesterol, and 4) fasting blood glucose.
Through CARDIA year 15, blood pressure was measured at 1-minute intervals using a Hawksley random zero mercury sphygmomanometer (WA Baum, Inc). Subsequently, in years 20–25, an oscillometer (Omron model HEM907XL; Omron, Mannheim, Germany) calibrated to the random zero values was used to measure blood pressure. At each visit, blood pressure was measured 3 times, and the average of the second and third measurements was used in the analyses. Elevated blood pressure was defined as systolic blood pressure ≥ 130mmHg or diastolic blood pressure ≥ 85 mmHg, or use of antihypertensive medication.
Plasma lipids were measured enzymatically by Northwest Lipids Research Laboratory at the University of Washington (Seattle, WA) (Warnick, 1986). Low density lipoprotein (LDL)-containing lipoproteins were precipitated with dextran sulphate/magnesium chloride before determining HDL-cholesterol concentrations (Warnick, 1982). Elevated fasting triglyceride was defined as level of ≥ 150 mg/dL. Low high density lipoprotein (HDL)-cholesterol was defined as <50mg/dL in women and <40 mg/dL in men. Fasting blood glucose was defined as ≥ 100mg/dL or meeting diabetes criteria.
Diabetes Classification
Fasting blood glucose concentrations were quantified in a venous blood sample using the hexokinase method and standard radioimmunoassay (Folsom et al., 1996). At all CARDIA exams, diabetes was defined as 1) self-reported use of diabetes medication or 2) fasting glucose ≥126 mg/dl. In addition to those 2 criteria, 2-hour post-challenge glucose ≥ 200mg/dl was included at Years 10, 20, and 25 and glycated hemoglobin ≥ 6.5% was added in Years 20 and 25 (Carnethon et al., 2009).
Covariates
Body weight and height were measured without shoes or excessive clothing on a calibrated scale (Friedman et al., 1988). BMI was calculated as the body weight (kg)/squared height (m2). Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) was calculated as glucose (mmol/L)*insulin (mU/L)/22.5 (Matthews et al., 1985). Educational status was quantified as the self-reported maximum number of years of school attained. Lifestyle factors, including smoking, drinking alcohol, physical activity, and medical history of taking medication for hypertension, hyperlipidemia, or diabetes were obtained by self-administered questionnaire. Smoking status was self-reported. Alcohol intake was quantified from an alcohol use questionnaire (Friedman et al., 1988). A physical activity score was derived from the CARDIA physical activity history. Total physical activity was calculated by multiplying the months of physical activity endorsed and the level of physical activity intensity, where approximately 300 exercise units is equivalent to the recommended amount of physical activity for adults (Sidney et al., 1991; Gabriel et al., 2014). The A Priori Diet Quality Score was derived from the CARDIA diet history, where greater score indicates better diet quality (Sijtsma et al., 2012).
Statistical Analysis
Person-years were calculated as the sum of individual follow-up times until the occurrence of metabolic syndrome or diabetes, censoring, or the Year 25 examination in 2010–2011. Incidence densities of metabolic syndrome and diabetes were presented by PREF points. Proportional hazards regression were modeled to calculate incidence densities of metabolic syndrome and diabetes by PREF points. However, the proportional hazard assumption, a constant hazards ratio over time, was violated for the association between PREF and metabolic syndrome. Thus with our preliminary analysis suggesting a time-dependent follow-up association for the metabolic syndrome, a logistic regression over disjoint follow-up periods was used to estimate the association of PREF with metabolic syndrome. The analysis of the association between PREF and diabetes was examined by proportional hazards models, as the hazard of diabetes was constant over time. Thus Odds Ratio (OR) from the logistic regression for PREF with metabolic syndrome and Hazard Ratio (HR) from the proportional hazards regression for the association of PREF with diabetes are provided. Statistical analysis was two-sided with a type 1 error rate of 0.05. Statistical analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC).
RESULTS
Participant characteristics
Among 2878 participants free of metabolic syndrome in CARDIA Year 10, mean age was 34.8 years, educational attainment was 15.5 years, and mean BMI was 26.3 kg/m2 (24.9 to 31.6 kg/m2 across PREF categories). As previously reported (Yoon et al., 2018), nearly 50% of participants endorsed 1–5 constructs, while only 3.6% had 6–8 PREF points. More than half of the participants were female (54.2 to 84.7% across PREF categories) and white (50.7 to 53.1% across PREF categories). Participants with PREF≥1 point had greater energy intake but also greater A Priori Diet Quality Score, suggesting excess energy, though with a healthier diet composition compared to normal eaters. Findings were similar in the 3,788 participants free of diabetes in Year 10 (details in Online supplement Table 2).
Associations between problematic relationship to eating and food, incident metabolic syndrome and incident diabetes
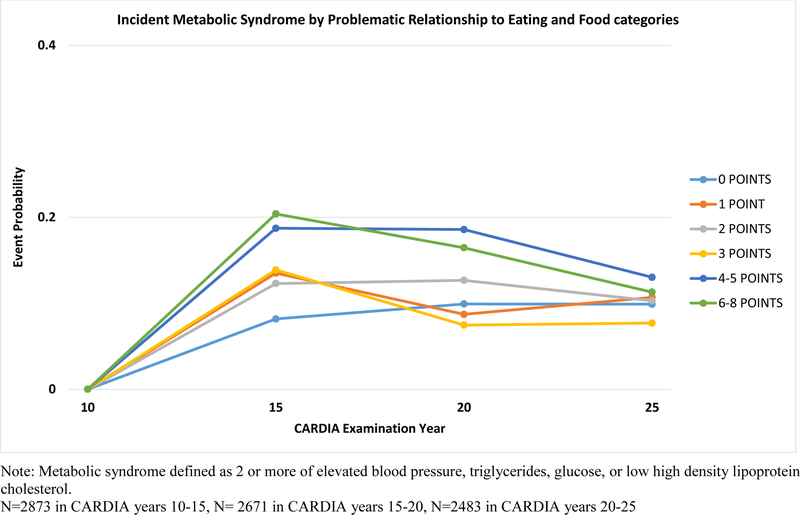
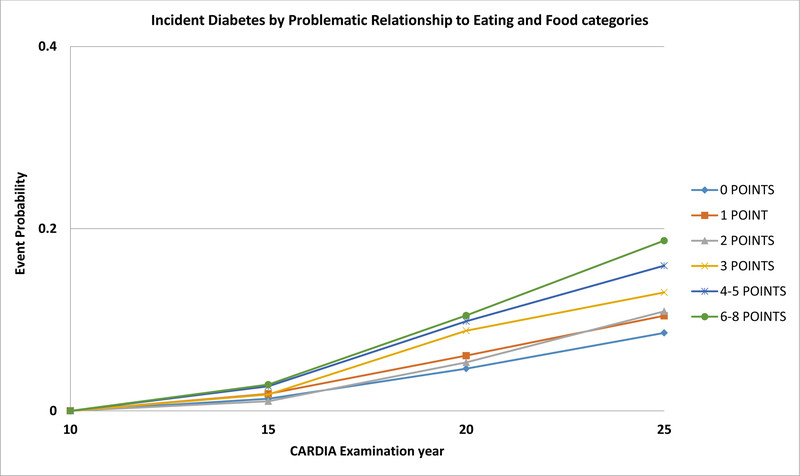
Kaplan-Meier estimates for incident metabolic syndrome according to PREF are shown in detail in Figure 1. Incidence in Years 10 to 15 and Years 15 to 20 were greater for continuous PREF after adjustment for demographics (OR 1.25 per point and 95% CI (1.17–1.34) and OR 1.17 per point and 95% CI (1.08–1.27), respectively), apparently stronger in Years 10–15 (significant OR for each PREF category compared to PREF 0 points, Online Supplement Table 3) than for Years 15–20. In both cases, findings were partially attenuated after further adjustment for baseline BMI (OR 1.10 per point, 95% CI (1.02–1.19) and OR 1.08 per point, 95% CI (0.99–1.18), for CARDIA Years 10 to 15, and Years 15 to 20, respectively). Little change was seen after further adjustments for behaviors and clinical variables. The association was not significant in Years 20 to 25. Kaplan-Meier curves for incident diabetes according to PREF are shown in Figure 2; the estimated difference among PREF categories was graded and widened with added follow-up. Hazard ratio (HR) was 1.20 (95% CI 1.12, 1.28) per PREF point after adjustment for demographics (significant for PREF categories 3+ points, Online Supplement Table 4). HR attenuated after adjusting for baseline BMI. Little to no changes were seen after further adjustments for behaviors.
Figure 1.
Kaplan-Meier Curve of Incident Metabolic Syndrome by Problematic Relationship to Eating and Food categories assessed in CARDIA Year 10 (1995–96)
Figure 2.
Kaplan-Meier Curve of Incident Diabetes by Problematic Relationship to Eating and Food categories assessed in CARDIA Year 10 (1995–96)
DISCUSSION
In this study, we assessed the association between problematic eating behaviors and metabolic syndrome and diabetes from logistic regression and proportional hazards regression, respectively. Logistic regression was modeled for the association of PREF with metabolic syndrome that was non-time dependent, while proportional hazards regression was modeled for the time-dependent association of PREF with diabetes. In this study, we confirm that participants who endorsed at least one problematic eating behavior at average age 35 years were at greater risk for metabolic syndrome and diabetes compared to normal eaters. We additionally report that both associations were attenuated after we adjusted for baseline (CARDIA year 10) BMI. Addressing PREF behaviors early in life therefore has potential to reduce clinical conditions.
Our finding of greater risk of metabolic syndrome and diabetes among participants with problematic eating behaviors is consistent with other longitudinal studies (Abraham et al., 2014). In terms of metabolic syndrome, binge eating carried 2.8 times greater risk for metabolic syndrome compared to non-binge eaters in Framingham Heart Study Third Generation and Omni 2 cohort studies after adjustment for demographics and attenuated after adjustment for BMI (Abraham et al., 2014).
In the Framingham Heart Study and Third Generation and Omni 2 cohorts, participants who engaged in binge eating were at 2.9 times greater risk for type 2 diabetes and at 3.2 times greater risk for insulin resistance compared to non-binge eating participants. Both associations were attenuated after adjustment for BMI (Abraham et al., 2014).
Our study adds to the literature showing that our definition of PREF includes behaviors and attitudes which are less likely to qualify for a diagnosable eating disorder. Regardless of whether an endorsement of a problematic eating behavior or attitude is sufficient for a formal diagnosis of an eating disorder, problematic eating behaviors and attitudes themselves may independently lead to adverse clinical consequences.
One strength of the present investigation is that the large study sample was followed for 15 years after PREF categorization, which allows clarifying the temporality between PREF and the incidence of metabolic syndrome and diabetes. Furthermore, our finding shows that, after adjustment for demographics, participants with problematic eating behaviors are at greater risk for metabolic syndrome and diabetes and the risk is graded by the number of problematic eating behaviors. In addition, the community-based samples of both black and white men and women differs from other studies with samples of adolescents and those receiving treatment for eating disorders. Therefore, this improves the generalizability of the findings. We caution that QEWP-R was only administered once in CARDIA. Because QEWP-R is not a clinical diagnostic tool and CARDIA does not collect any medical records of diagnosed eating disorders, and did not do any in-depth psychological testing, the overlap of clinically diagnosable eating disorders with PREF categories is not known. However, this point may also be viewed as a strength, as our research raises the question whether it might be generally useful to know about more modest disturbances in eating behaviors. As in the case of all observational epidemiologic studies, our study is limited by potential residual confounding from unmeasured or unknown confounders.
CONCLUSION
In our study, we confirm that endorsement of problematic eating behaviors at average age 35 years was associated with incident metabolic syndrome and diabetes. The risks were graded by PREF points and partially attenuated after adjustment of baseline BMI. These associations in this general population sample imply that the health of those with problematic relationship to eating and food are adversely affected, and in addition to what and how much people are eating, the behaviors and attitudes related to eating and food also place participants at greater risk of metabolic health consequences. A comprehensive understanding and an examination of the full spectrum of problematic eating behaviors and attitudes should be investigated through a composite score such as PREF or by counting the number of problematic eating behaviors endorsed. Because higher BMI and metabolic syndrome and diabetes are strongly associated, our finding links a highly prevalent set of problematic eating behaviors in a direct line to these metabolic disorders. Taken together, an integrated approach of early identification of subjects with problematic eating behaviors and development of interventions that focus on building a healthy relationship with eating and food could help in prevention of adverse metabolic health outcomes among middle-aged adults.
Supplementary Material
Acknowledgements:
This work was supported by the National Institutes of Health [HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, HHSN268200900041C, AG0005, and R01 HL 53560].
Footnotes
Conflict of Interest
CY, DJ, DD, DNS, LS, SM have no conflicts of interest.
REFERENCES
- Abraham TM, Massaro JM, Hoffmann DU,Yanovski JA, Fox CS. Metabolic Characterization of Adults with Binge Eating in the General Population: The Framingham Heart Study. Obesity (Sliver Spring) 2014; 22: 2441–9 doi: 10.1002/oby.20867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes RD, Boeka AG, McKenzie KC, Genao I, Garcia RL, Ellman MS, Ellis PJ,Masheb RM, Grilo CM. Metabolic syndrome in obese patients with binge-eating disorder in primary care clinics: a cross-sectional study. Prim Care Companion CNS Disord 2011;13 doi: 10.4088/PCC.10m01050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnethon MR, Sternfeld B, Schreiner PJ, Jacobs DR Jr, Lewis CE, Liu K, Sidney S. Association of 20-year changes in cardiorespiratory fitness with incident type 2 diabetes: the coronary artery risk development in young adults (CARDIA) fitness study. Diabetes Care 2009;32:1284–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Health Statistics Reports Prevalence of Metabolic Syndrome Among Adults 20 years of Age and Over, by Sex, Age, Race, and Ethnicity, and Body Mass Index: United States, 2003–2006. Internet: https://www.cdc.gov/nchs/data/nhsr/nhsr013.pdf (accessed August, 7, 2018) [PubMed]
- Folsom AR, Jacobs DR Jr, Wagenknecht LE, Winkhart SP, Yunis C, Hilner JE, Savage PJ, Smith DE, Flack JM. Increase in fasting insulin and glucose over seven years with increasing weight and inactivity of young adults. The CARDIA Study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol 1996. 1;144:235–46. [DOI] [PubMed] [Google Scholar]
- Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988; 41: 1105–111 [DOI] [PubMed] [Google Scholar]
- Gabriel KP, Sidney S, Jacobs DR Jr, Quesenberry CP Jr, Reis JP, Jiang SF, Sternfeld B. Convergent validity of a brief self-reported physical activity questionnaire. Med Sci Sports Exerc 2014. August;46(8):1570–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–419 [DOI] [PubMed] [Google Scholar]
- National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment panel III). JAMA 2001; 285: 2486–97 [DOI] [PubMed] [Google Scholar]
- Raevuori A, Suokas J, Haukka J, Gissler M, Linna M, Grainger M, Suvisaari Highly increased risk of type 2 diabetes in patients with binge eating disorder and bulimia nervosa. Int J Eat Disord 2015;48:555–62. doi: 10.1002/eat.22334. [DOI] [PubMed] [Google Scholar]
- Sidney S, Jacobs DR Jr, Haskell WL, Armstrong MA, Dimicco A, Oberman A, Savage PJ, Slattery ML, Sternfeld B, Van Horn L. Comparison of two methods of assessing physical activity in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol 1991. 15;133:1231–45. [DOI] [PubMed] [Google Scholar]
- Sijtsma FP, Meyer KA, Steffen LM, Shikany JM, Van Horn L, Harnack L, Kromhout D, Jacobs DR Jr. Longitudinal trends in diet and effects of sex, race, and education on dietary quality score change: the Coronary Artery Risk Development in Young Adults study. Am J Clin Nutr 2012;95:580–6. doi: 10.3945/ajcn.111.020719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PW, Ghushchyan V, Wyatt HR, Hill JO. The medical cost of cardiometabolic risk factor clusters in the United States. Obesity (Silver Spring) 2007;15:3150–8. doi: 10.1038/oby.2007.375. [DOI] [PubMed] [Google Scholar]
- Warnick GR, Benderson J & Albers JJ (1982) Dextran sulfate-Mg2+ precipitation procedure for quantitation of highdensity-lipoprotein cholesterol. Clin Chem 28, 1379–1388. [PubMed] [Google Scholar]
- Warnick GR (1986) Enzymatic methods for quantification of lipoprotein lipids. Methods Enzymol 129, 101–123. [DOI] [PubMed] [Google Scholar]
- World Health Organization Global Strategy on Diet, Physical Activity and Health. Obesity and Overweight. Internet: http://www.who.int/dietphysicalactivity/media/en/gsfs_obesity.pdf (accessed August, 7, 2018)
- Yoon C, Jacobs DR Jr, Duprez DA, Dutton G, Lewis CE, Neumark-Sztainer D, Steffen LM, West DS, Mason SM. Questionnaire-based problematic relationship to eating and food is associated with 25 year body mass index trajectories during midlife: The Coronary Artery Risk Development In Young Adults (CARDIA) Study. Int J Eat Disord 2018;51:10–17. doi: 10.1002/eat.22813. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.