Abstract
Aims
To compare the outcomes of partners who participated in a telephone couples behavioural intervention to improve glycaemic control in persons with Type 2 diabetes with those of untreated partners of participants in an individual intervention or education; to explore ‘ripple effects’, i.e. positive behaviour changes seen in untreated partners.
Methods
The Diabetes Support Project was a three-arm randomized telephone intervention trial comparing outcomes of couples calls (CC), individual calls (IC) and diabetes education calls (DE). Couples included one partner with Type 2 diabetes and HbA1c ≥ 58 mmol/mol (7.5%). All arms received self-management education (two calls). CC and IC participated in 10 additional behaviour change calls. CC included partners, emphasizing partner communication, collaboration and support. Blinded assessments were performed at 4, 8 and 12 months. Partner outcomes were psychosocial (diabetes distress, relationship satisfaction, depressive symptoms), medical (BMI, blood pressure) and behavioural (fat intake, activity).
Results
Partners’ (N = 268) mean age was 55.8 years, 64.6% were female and 29.9% were from minority ethnic groups. CC (vs. IC and DE) partners had greater reductions in diabetes distress, greater increases in marital satisfaction (4 and 8 months), and some improvements in diastolic BP. There were no consistent differences among arms in other outcomes. There was no evidence of a dietary or activity behaviour ripple effect on untreated partners, i.e. comparing partners in the IC and DE arms.
Conclusions
A collaborative couples intervention resulted in significant improvements in partner diabetes distress and relationship satisfaction. There were no consistent effects on behavioural or medical partner outcomes, and no evidence of diet or activity behaviour ripple effects, suggesting that partners should be targeted directly to achieve these changes. (Clinical Trial Registry No: NCT01017523)
Introduction
It is generally accepted that a person’s disease can have negative (e.g. distress) and positive (e.g. sense of purpose) effects on family members [1]. Diabetes requires that the person with diabetes make significant behavioural changes that are likely to impact family members.
A systematic review of 29 studies that assessed the effect of Type 2 diabetes on family members (2000–2011, 16 quantitative, 10 qualitative) reports that diabetes distress in family members is notable [2]. In one study, partner emotional distress was higher than patient distress [3]. Data from the DAWN2 Study, a multi-country survey that included questionnaires from 2057 family members, report that distress, especially about hypoglycaemia, was high. Examining behaviour change, some family members reported positive effects of their family member having diabetes, as it led them to make their own healthy lifestyle choices [4]. These data suggest that partners should be involved in diabetes interventions because it may benefit them too. In fact, in DAWN2, 39.4% reported that they wanted to be more involved in the care of the person with diabetes, yet only 21% report being included in even basic diabetes self-management education [5].
Interdependence theory posits that partners should provide mutual support for behaviour change and use collaborative problem-solving techniques [6,7] to help persons with diabetes make changes. This interdependence supports the potential value of couples interventions for change in the partner as well as in the person with diabetes. Other models of dyadic coping emphasize the shared realities of partners, again suggesting that an intervention involving partners will affect them as well [8,9].
We asked whether partner involvement in a behavioural intervention for adults with Type 2 diabetes may have beneficial effects on partners. The Diabetes Support Project (DSP) provided an opportunity to explore this question [10]. A few studies have compared family-based interventions with usual care for persons with diabetes [11,12], but to our knowledge, the DSP is the only one that compared a family intervention with a comparable individual intervention. This is critical to a valid assessment of the added value of involving partners. This design also allows us to assess intervention effects on partners, whether or not they participated in the intervention.
We hypothesized that partners who participated in a couples intervention would derive greater benefit than those not directly included in the treatment of the person with diabetes. Outcomes included health (obesity, BP), psychosocial (diabetes distress, depressive symptoms, relationship satisfaction) and behavioural (dietary fat intake, physical activity) measures. The primary outcome of the DSP was change in HbA1c in the person with diabetes. Details and results for the people with diabetes have been previously reported [10]. Briefly, although all groups showed decreased HbA1c, the couples intervention (vs. individual and education interventions) led to greater reduction in HbA1c for participants in the moderately high range (middle tertile) of baseline HbA1c (i.e. 67–77 mmol/mol; 8.3–9.2%), greater reduction in BMI and greater improvement in some psychosocial outcomes.
Looking at behaviour, several studies describe a ‘ripple effect,’ i.e. partners not actively involved in interventions also change their behaviour. In the LookAHEAD trial, spouses of persons with diabetes who participated in the weight loss intervention, although not participants themselves, lost significantly more weight than spouses of control participants [13]. Therefore, a secondary hypothesis was that we would find ripple effects of the individual intervention on diet and activity behaviours, and weight, of untreated partners.
Participants and methods
Trial design
The DSP, a 12-month, randomized controlled trial (RCT), involved couples in which one partner had Type 2 diabetes in poor glycaemic control (HbA1c ≥ 58 mmol/mol; 7.5%). Interventions were delivered over the telephone to increase reach. Couples were randomized to: couples intervention calls (CC; person with diabetes together with his/her partner), individual intervention calls (IC; person with diabetes alone), and individual diabetes education calls (DE; person with diabetes alone). Thus, the IC and DE arms did not provide any intervention to partners. Couples were recruited in upstate New York and northern California, enrolled by staff through chart review/recruitment letters, advertisements and community talks. Consented participants received compensation for assessment time and reimbursed transportation. The trial was approved by the Institutional Review Boards of SUNY Upstate Medical University and University of California, San Francisco.
DSP participants
Couples (self-defined as ‘in a committed relationship ≥ 1 year’) were eligible if both partners were ≥ 21 years old; the person with diabetes had been diagnosed with Type 2 diabetes > 1 year (confirmed by medical record and/or HbA1c) with baseline HbA1c ≥ 58 mmol/mol (7.5%). Both partners were able to speak/read English; had no severe medical/psychiatric conditions that might interfere with participation; had telephone access; and were willing to participate in all study-related activities. The persons with diabetes had a mean age of 56.8 years, 61.6% were male, and 30.4% were members of minority ethnic groups. Their baseline mean HbA1c was 76.0 mmol/mol (9.1%), and 62.6% reported using insulin. See Trief et al. [10] for more detailed information about the persons with diabetes, and the published CONSORT diagram for the DSP trial.
Randomization
A computer-generated random assignment scheme by region was used by the study biostatistician to assign participants to interventions. A smaller DE sample was planned to provide more power to compare CC with IC, so the biostatistician created a non-uniform random allocation ratio to assign participants to arms in the proper proportions [14]. The allocation ratio was five (CC)/five (IC)/four (DE). Arms were stratified by gender and region to strive for comparable representation.
Sample size and assessments
The minimum sample size necessary was computed based on 3-month pilot HbA1c data [15] of the persons with diabetes (thus, is less relevant to partner data). It showed that 80 participants per arm (N = 240) would exceed 80% power to detect a significant Time by Group interaction effect, and detect significant differences between CC or IC and DE on HbA1c of the person with diabetes. Because we examined subtle differences between CC and IC, and to include attrition, we aimed for a larger cohort. Participants (both the person with diabetes and his/her partner) were assessed four times (baseline, 4, 8 and 12 months). Assessments were completed at the participants’ homes or community spaces (e.g. library). Assessors were blind to the treatment group.
Interventions
The primary intervention target was improved glycaemic control of the person with diabetes. In IC and DE, persons with diabetes participated alone; in CC, the person with diabetes and his/her partner participated together. All arms received two calls covering comprehensive diabetes education. DE participants had no further intervention. CC and IC arms had 10 additional calls, content was based on social learning theory [16], which were comparable with most behavioural interventions (provision of knowledge, self-monitoring, goal-setting and behavioural contracting to promote lifestyle changes in activity, diet, blood glucose monitoring and medication adherence), focused on the effect of behaviour on glycaemic control. In CC, both partners were required to participate; if one partner was not available, the call was cancelled/rescheduled. If either partner dropped out, the intervention was terminated. The CC intervention was based on Interdependence Theory [7,8], i.e. educators were trained, and exercises designed, to help both partners recognize the effects of diabetes on both, to promote collaborative problem-solving and mutual support. Partners were actively involved in all calls and homework. The focus was consistently on how the partner could support the person with diabetes to make healthy lifestyle changes. Two calls were specific to relationships. In one, couples practised the ‘speaker–listener technique’ (one partner shares a concern, the other restates the concern until the partner feels ‘heard,’ then they switch roles). Another call focused on communication around diabetes-related conflicts. These relationship-focused calls were informed by research on relationship enhancement [17] and piloted [15]. In IC, these two calls addressed individual problem-solving.
Calls occurred weekly for 12 weeks. Trained educators followed scripts, participants had homework and workbooks (pre-call readings, diet/activity/blood glucose self-monitoring logs, goal-setting contracts). Sessions were audiotaped for supervision (until the educator was deemed competent); a random sample was reviewed by independent reviewers for quality assurance/treatment fidelity.
Partner outcomes and measures
Obesity – weight and BMI. Partners were weighed on digital scales (to the nearest 0.1 kg) wearing street clothes. Two weights were averaged. Height was measured with a stadiometer. BMI was recorded in kg/m2.
Blood pressure (BP). Three seated readings at 1-min intervals were taken using automated BP monitors. The mean of readings two and three was computed.
Diabetes distress (DD). There is no published measure of diabetes distress in partners of persons with Type 2 diabetes. A modified version of the Problem Areas in Diabetes Questionnaire (PAID) scale was used to reflect common partner concerns (Fisher L, unpublished). For example, the PAID item ‘feeling scared when you think about living with diabetes’ was changed to ‘feeling scared about my partner’s diabetes’ on the partner distress measure. Items specific to partner concerns were also added, based on qualitative interviews with patients and partners, ensuring that phrasing was clear and meaningful. This yielded a 23-item scale. Partners rate how much of a problem the issue is for them on six-point Likert scales (1 = not a problem … 6 = very serious problem). The scale was administered to 100 partners of adults with Type 2 diabetes, and report a Cronbach’s α = 0.97 [current study α = 0.95]. As with the PAID, an exploratory factor analysis identified a strong single factor (eigenvalue = 11.2, all individual item factor loadings between 0.55 and 0.78). A higher score denotes higher partner diabetes distress.
Depressive symptoms (DS). The Patient Health Questionnaire-8 (PHQ-8) was used. The PHQ-8 is a reliable, valid scale that queries the presence and severity of eight symptoms of depression, omitting the ninth symptom (suicidal ideation); its use is common in research protocols [18].
Marital satisfaction. We used the Revised Dyadic Adjustment Scale (RDAS), a 14-item self-report measure of relationship satisfaction [19], significantly correlated with the Locke–Wallace Marital Adjustment Test (r = 0.68, p < 0.01). The RDAS was reliable in the current study (Cronbach’s α= 0.84). A higher score denotes greater marital satisfaction.
- Behaviour change was measured using:
- NCI Fat Screener, a 15-item measure of the percentage of energy from the intake of fats [20]. In three validity studies, correlation between the screener estimate and estimated true intake (based on 24-h dietary recall) was 0.62–0.78.
- International Physical Activity Questionnaire (IPAQ), a seven-item self-report measure of physical activity in the past 7 days, measured as days per week and time per day that the respondent engaged in vigorous, moderate, walking and sitting activities. The IPAQ yields a value of mets/week [21]. It has been shown to be reliable, with criterion validity that is comparable with other self-report physical activity measures.
Partner involvement
Although partners did not participate directly in the IC or DE arms, ethically we could not prohibit them from involvement. In a study-developed post-intervention questionnaire to check on treatment fidelity, we asked participants with diabetes how involved their partners were (reading the materials, listening to calls, discussing the information provided). Responses were given on a four-point scale: not at all, a little, a lot and all of the time.
Statistical analysis
Mixed model linear regression was used for data analyses. The model included time as a repeated measure, treatment group and the time by treatment interaction term. Baseline scores were used as covariates in all models. The covariance structures chosen were based on best fit, which was assessed using Akaike information criterion (AIC) and Bayesian information criterion (BIC) scores; AR1 structure (decaying correlation between successive measures) provided the best fit for most variables. Between-group comparisons by assessment were conducted using planned comparisons (t-tests) of modelled means. In NCI screener analyses, the data were highly right (positive) skewed and mathematical transformations failed to normalize the distributions and correct for outliers. For the NCI regression analysis, extreme values for 14 observations were replaced with values equal to ± 3 sd from the mean of all observations. In the IPAQ data, raw IPAQ scores were highly skewed; a Log10(DV+1) transformation achieved approximate normality and was used in the regression analysis. Missing values were not imputed. Results of Little’s Missing Completely at Random (MCAR) test for the set of longitudinal dependent variables were consistent with the data being missing completely at random (P = 0.55). All analyses were conducted at the 0.05 level of significance (two-tailed), with P-values between 0.05 and 0.10 considered marginally significant. All statistical analyses were conducted using SPSS version 24 [22].
Results
Seventy (20%) of the 350 potential couples were ineligible, leaving 280 couples who completed baseline assessments and were randomized. Twelve (4.3%) did not participate in any intervention calls, thus were considered unable/unwilling to participate in study procedures, and thus as not meeting inclusion criteria. In total, 268 couples were included in intention to treat analyses.[10]
Partner participants
Table 1 shows baseline data for partner participants. The majority (64.6%) were female, 29.9% were self-described members of minority racial/ethnic groups, 54.8% were employed (full-time or part-time) and 44% reported annual household income < $50 000. For the total sample, the mean (sd) age was 55.8 (11.7) years, they had been in this committed relationship for a mean (sd) of 25.5 (14.8) years. Attrition, defined as having no assessment at each follow-up, did not differ between arms. The proportions of partners who missed assessments at 4, 8 and 12 months were 20.9%, 24.6% and 27.2%, respectively. Drop-outs, defined as having no 12-month assessment, were 26.8% (CC), 25.8% (IC) and 29.5% (DE), and did not differ by arm. Compared with completers, drop-outs were younger (49.4 vs. 57.4 years), more likely to be Hispanic (13.7% vs. 3.2%), more likely to be Asian (18.8% vs. 7.3%), less likely to be white (55.1% vs. 75.5%), less likely to be retired (13.7% vs. 36.9%), more likely to be not working (28.8% vs. 9.2%) and more likely to have no high school degree (15.3% vs. 4.6%). Comparing drop-outs with completers on dependent variables did not reveal any statistically significant differences at baseline.
Table 1.
Partner participant characteristics at baseline by intervention arm and total group
| Participant characteristic | CC | IC | DE | Total | P-value* |
|---|---|---|---|---|---|
| No. of partner participants | 97 | 93 | 78 | 268 | – |
| Gender (%) | 0.803 | ||||
| Female | 66.0 | 65.6 | 61.5 | 64.6 | |
| Ethnicity (%) | |||||
| Hispanic or Latino | 6.4 | 4.4 | 7.7 | 6.1 | 0.663 |
| Race (%) | 0.380 | ||||
| White | 72.6 | 65.6 | 72.4 | 70.1 | |
| Asian | 5.3 | 14.4 | 11.8 | 10.3 | |
| Black or African American | 16.8 | 17.8 | 13.2 | 16.1 | |
| Other | 5.3 | 2.2 | 2.6 | 3.4 | |
| Relationship status (%) | 0.089 | ||||
| Married | 88.7 | 86.0 | 83.3 | 86.2 | |
| Unmarried/living together | 10.3 | 6.5 | 6.4 | 7.8 | |
| Unmarried/not living together | 1.0 | 7.5 | 10.3 | 6.0 | |
| Education (%) | 0.158 | ||||
| Less than high school | 5.2 | 9.8 | 7.8 | 7.5 | |
| High school/GED/TECH | 16.5 | 20.7 | 19.5 | 18.8 | |
| Some college or AD | 47.4 | 37.0 | 37.7 | 41.0 | |
| Bachelors | 12.4 | 18.5 | 24.7 | 18.0 | |
| Masters or doctorate | 18.6 | 14.1 | 10.4 | 14.7 | |
| Employment status (%) | 0.293 | ||||
| Working full time | 37.1 | 41.9 | 44.9 | 41.0 | |
| Working part time | 20.6 | 9.7 | 10.3 | 13.8 | |
| Retired/on disability | 27.8 | 35.5 | 28.2 | 30.6 | |
| Not working/other | 14.4 | 12.9 | 16.7 | 14.6 | |
| Annual household income, $ (%) | 0.213 | ||||
| < 20 000 | 9.3 | 17.2 | 14.1 | 13.4 | |
| 20 000–50 000 | 20.6 | 31.2 | 26.9 | 26.1 | |
| 50 000 + | 53.6 | 41.9 | 50.0 | 48.5 | |
| Not reported | 16.5 | 9.7 | 9.0 | 11.9 | |
| Age, years, mean (sd) | 56.7 (11.8) | 54.6 (12.3) | 55.9 (11.0) | 55.8 (11.7) | 0.473 |
| Years in relationship (sd) | 26.7 (14.9) | 25.6 (14.8) | 23.9 (14.8) | 25.5 (14.8) | 0.485 |
| Systolic BP, mmHg, mean (sd) | 124.3 (17.9) | 122.8(17.4) | 121.0(17.2) | 122.8 (17.5) | 0.453 |
| Diastolic BP, mmHg, mean (sd) | 74.5 (11.3) | 74.5 (10.4) | 72.1 (11.4) | 73.8 (11.1) | 0.250 |
| Weight, kg, mean (sd) | 88.4 (28.0) | 86.7 (21.6) | 87.5 (27.5) | 87.5 (25.7) | 0.902 |
| Height, cm, mean (sd) | 166.5 (9.5) | 163.6(12.7) | 165.2 (9.7) | 165.1 (10.8) | 0.166 |
| BMI, kg/m2, mean (sd) | 31.6 (8.2) | 33.2 (15.0) | 31.8 (8.7) | 32.2 (11.1) | 0.546 |
| Diabetes Distress Scale, mean (sd) | 2.3 (1.0) | 2.4 (1.0) | 2.3 (1.0) | 2.3 (1.0) | 0.829 |
| PHQ-8, mean (sd) | 2.5 (3.0) | 3.5 (4.4) | 3.1 (4.1) | 3.0 (3.9) | 0.204 |
| RDAS, mean (sd) | 49.2 (9.3) | 50.2 (7.4) | 50.0 (9.2) | 49.8 (8.6) | 0.696 |
| IPAQ, total mets/week, mean (sd) | 90.1 (128.3) | 106.8(167.4) | 61.9 (82.9) | 87.7 (133.7) | 0.090 |
| NCI Fat Screener (%), mean (sd) | 33.9 (3.9) | 34.1 (5.2) | 35.1 (8.9) | 34.3 (6.1) | 0.404 |
Based on chi-square tests (qualitative variables) or ANOVA (quantitative variables).
CC, couples calls; IC, individual calls; DE, diabetes education calls; GED,; TECH,; AD,; PHQ-8, Patient Health Questionnaire-8; RDAS, Revised Dyadic Adjustment Scale; IPAQ, International Physical Activity Questionnaire.
Partner outcomes
Partner outcomes are detailed in Table 2.
Table 2.
Mean (se) outcomes of partners by arm: couples call intervention vs. individual call intervention vs. diabetes education call intervention
| Assessment (months) | CC | IC | DE | F-value | P-value* | |
|---|---|---|---|---|---|---|
| Weight (kg) | 0 | 88.20 (0.31) | 88.18 (0.31) | 88.19 (0.34) | 0.02 | 0.99 |
| 4 | 87.56 (0.33) | 87.66 (0.34) | 87.65 (0.37) | 0.03 | 0.98 | |
| 8 | 87.79 (0.34) | 87.88 (0.35) | 88.20 (0.39) | 0.33 | 0.72 | |
| 12 | 87.91 (0.35) | 87.53 (0.36) | 87.91 (0.40) | 0.36 | 0.70 | |
| Systolic BP (mmHg) | 0 | 123.76 (1.05) | 123.37 (1.08) | 122.92 (1.22) | 0.14 | 0.87 |
| 4 | 122.52 (1.16) | 122.96 (1.22) | 124.25 (1.31) | 0.51 | 0.60 | |
| 8 | 119.98 (1.18) | 120.91 (1.24) | 123.46 (1.37) | 1.92 | 0.15 | |
| 12 | 119.87 (1.22) | 122.88 (1.25) | 123.46 (1.39) | 2.33 | 0.10 | |
| Diastolic BP (mmHg) | 0 | 73.97 (0.66) | 73.97 (0.68) | 73.45 (0.72) | 0.17 | 0.84 |
| 4 | 71.78 (0.74)‡ | 73.37 (0.77)§ | 75.98 (0.83) | 7.20 | 0.001 | |
| 8 | 70.50 (0.68)‡ | 72.45 (0.79) | 74.40 (0.87) | 5.85 | 0.003 | |
| 12 | 70.85 (0.77)†‡ | 73.82 (0.79) | 74.23 (0.88) | 5.34 | 0.005 | |
| Diabetes Distress Scale | 0 | 2.30 (0.06) | 2.32 (0.06) | 2.29 (0.07) | 0.04 | 0.96 |
| 4 | 1.75 (0.07)†‡ | 2.12 (0.07) | 2.17 (0.08) | 10.37 | <0.001 | |
| 8 | 1.80 (0.07)†‡ | 2.16 (0.07) | 2.23 (0.08) | 11.30 | <0.001 | |
| 12 | 1.78 (0.07)†‡ | 2.03 (0.07) | 2.01 (0.08) | 3.81 | 0.02 | |
| PHQ-8 | 0 | 2.99 (0.28) | 3.12 (0.29) | 3.07 (0.32) | 0.06 | 0.95 |
| 4 | 3.13 (0.31) | 3.69 (0.33) | 3.64 (0.35) | 0.94 | 0.39 | |
| 8 | 3.08 (0.32) | 3.59 (0.33) | 3.45 (0.36) | 0.72 | 0.49 | |
| 12 | 2.85 (0.32)† | 3.99 (0.33) | 3.44 (0.37) | 3.02 | 0.05 | |
| Dyadic Adjustment Scale | 0 | 49.85 (0.41) | 49.94 (0.41) | 49.92 (0.46) | 0.01 | 0.99 |
| 4 | 51.64 (0.67)‡ | 49.87 (0.69) | 48.71 (0.77) | 4.26 | 0.01 | |
| 8 | 50.80 (0.55)†‡ | 49.19 (0.57) | 48.58 (0.63) | 3.92 | 0.02 | |
| 12 | 49.74 (0.63) | 48.28 (0.64) | 48.86 (0.72) | 1.31 | 0.27 | |
| NCI – per cent calories from fat | 0 | 33.89 (0.27) | 33.87 (0.27) | 34.02 (0.30) | 0.08 | 0.93 |
| 4 | 33.69 (0.30) | 33.13 (0.31) | 33.83 (0.33) | 1.40 | 0.25 | |
| 8 | 33.37 (0.30) | 32.91 (0.31) | 33.29 (0.34) | 0.65 | 0.52 | |
| 12 | 33.19 (0.30) | 32.96 (0.31) | 33.70 (0.34) | 1.33 | 0.27 | |
| IPAQ (mets/week) | 0 | 30.12 (0.13) | 29.20 (0.13) | 26.67 (0.14) | 0.22 | 0.80 |
| 4 | 36.67 (0.14)† | 23.60 (0.15) | 33.44 (0.16) | 2.68 | 0.07 | |
| 8 | 37.91 (0.14)† | 23.32 (0.15) | 31.06 (0.17) | 3.01 | 0.05 | |
| 12 | 26.73 (0.15) | 28.38 (0.15) | 38.92 (0.17) | 1.73 | 0.18 |
For treatment effect, derived from mix linear models
CC, couples calls; IC, individual calls; DE, diabetes education calls; PHQ-8, Patient Health Questionnaire-8; IPAQ, International Physical Activity Questionnaire.
CC vs. IC, P < 0.05;
CC vs. DE, P < 0.05;
IC vs. DE, P < 0.05.
Partner health outcomes
We found no statistically significant differences in weight/BMI among the three arms at any follow-up.
Mean diastolic BP in the CC arm was statistically significantly lower than DE at 4, 8 and 12 months (all P-values < 0.005), and statistically significantly lower than IC at 12 months (P = 0.007). The IC mean was statistically significantly lower than DE at 4 months (P = 0.022).
Partner psychosocial outcomes
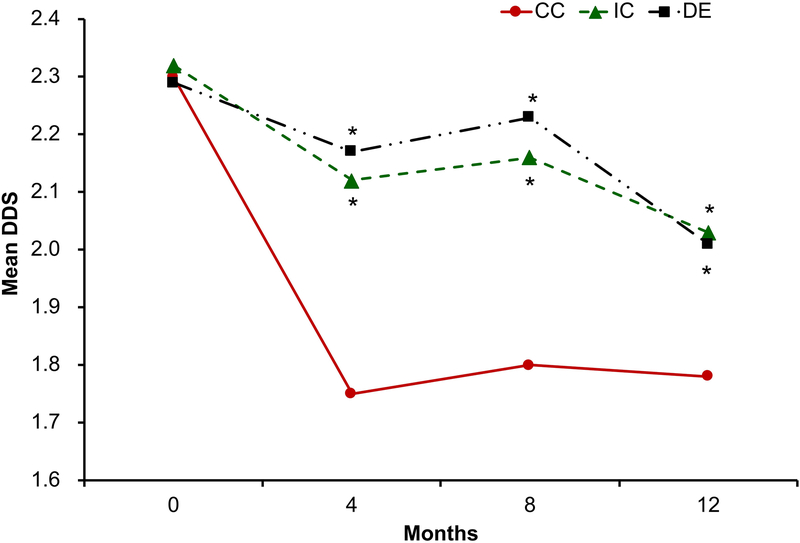
For diabetes distress, at 4, 8 and 12 months, the CC arm showed a statistically significantly lower DD score, and greater reduction in DD, than the IC and DE arms (4 and 8 months, P < 0.001; 12 month, P < 0.05) with no significant differences between the IC and DE arms (Fig. 1).
FIGURE 1.
Change in Diabetes Distress (DDS) for CC (couples call arm) vs. IC (individual call arm) vs. DE (diabetes education arm) over time.
For depressive symptoms, at 12 months, the CC arm showed a statistically significantly lower mean DS score (t = −2.50, P = 0.013) than IC and DE, this appears to reflect increases in partner DS in IC and DE arms, which did not differ. No other significant between arm differences were found.
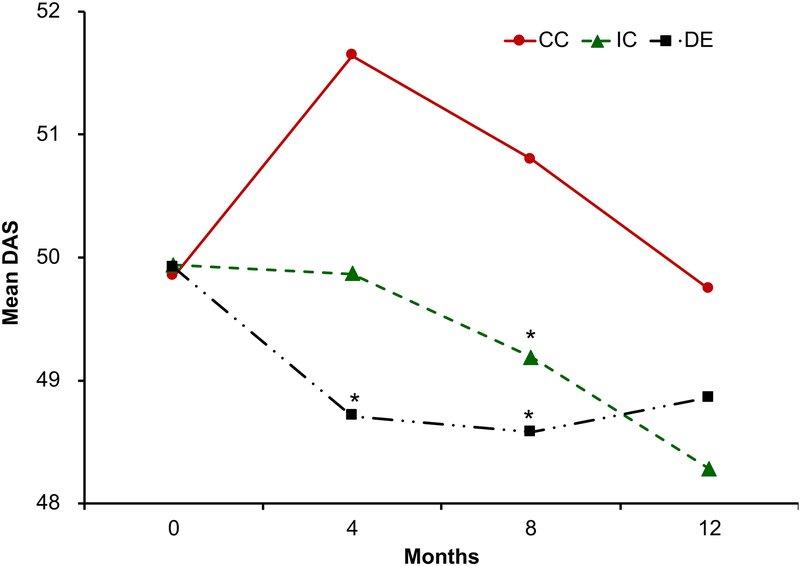
Relationship satisfaction is show in Fig. 2. The CC arm showed a statistically significantly higher, and greater increase in RS scores than the DE arm (t = 2.86, P = 0.005), and marginally higher than the IC arm (t = 1.84, P = 0.067) at 4 months. At 8 months, the CC arm showed a statistically significantly higher RS score than the IC (t = 2.03, P = 0.043) and DE arms (t = 2.64, P = 0.009); the IC and DE arms did not differ significantly at 4 or 8 months. At 12 months, there were no differences among the arms.
FIGURE 2:
Change in Marital Satisfaction (Revised Dyadic Adjustment Scale) for CC (couples call arm) vs. IC (individual call arm) vs. DE (diabetes education arm) over time.
Partner behaviour change
There were no between-arm differences in per cent of calories from fat at any of the assessments.
For activity behaviour, at 4 and 8 months, there were statistically significantly higher partner IPAQ scores in the CC compared with the IC arm (t = 2.23, P = 0.026 compared with t = 2.46, P = 0.015); this was not maintained at 12 months (t = 0.28, P = 0.768). No other between-arm differences were observed.
Partner involvement
Almost 40% of IC and DE participants reported that their partners were involved ‘a lot’ or ‘all of the time’ (e.g. listened on calls, read the materials).
Discussion
Our primary hypothesis was that partners of persons with diabetes who participated in a couples behavioural intervention would show evidence of beneficial intervention effects when compared with untreated partners of persons with diabetes who participated in a comparable individual intervention or diabetes education that did not include partner involvement. We found support for this hypothesis primarily in the psychosocial, but not the behavioural, domains. CC partners reported significantly greater reductions in diabetes distress, and improvement in relationship satisfaction, when compared with partners who did not participate in the comparable individual or briefer diabetes education interventions. CC partners also had fewer symptoms of depression at 12 months. We reported previously that both IC and CC interventions resulted in decreased diabetes distress for the persons with diabetes, although the effect was somewhat stronger for those in the CC arm [9], and here we see that this benefit extended to the participating partners too. Although high levels of partner distress have been reported [2–4], there is often concern that involving a partner will lead to more conflict and negative reactions to perceived ‘miscarried helping’ [24,25]. Our data indicate that involving the partner in an intervention may have beneficial emotional and relational effects on the partner, at least when the intervention is focused on promoting collaboration, communal coping and emotional openness.
CC partners showed improvements in diastolic, although not systolic, BP compared with the other arms. There were no significant group differences in weight loss, or diet or activity behaviours. Perhaps the unplanned partner involvement in the IC and DE arms that we identified may explain why we did not find a significant difference between CC (treated partners) and other arms on diet, activity or weight loss. This also makes the finding that the CC intervention resulted in greater reduction in partner diabetes distress and increase in partner relationship satisfaction even more compelling, as it suggests that the partner’s planned involvement in a collaborative problem-solving intervention led to these changes, compared with unplanned, somewhat tangential, involvement in partners of those in the individual-alone interventions.
Our secondary aim was to seek evidence of dietary, physical activity and weight loss ripple effects, i.e. evidence of positive behaviour change in partners of individual intervention participants, even though those partners have not participated themselves. Untreated partners have shown lowered cholesterol [25], dietary change [6], and short-term weight loss in non-diabetes samples [26]. Gorin and colleagues assessed the potential ripple effects on untreated spouses in the LookAHEAD diabetes sample [13]. Spouses of those in the lifestyle intervention arm (spouses were not involved in the intervention), lost significantly more weight and reported greater decreases in fat intake (over 1 year) than the spouses of those in the control arm, providing evidence of a dietary behaviour ripple effect. There were no differences in spouse physical activity levels. In the current analyses, we compared individual intervention (IC) arm partners to education-only control arm partners (DE), both untreated, assuming that the brief intervention was a true control, and would not have an effect on partners. [Because partners were treated in the couples arm (CC), those analyses are not relevant to the ripple effect.] There was no evidence of a dietary or physical activity ripple effect on untreated partners. One major difference between the DSP and Gorin’s work (and other studies of non-diabetes samples) is that those interventions targeted dietary change alone, whereas the DSP targeted improved glycaemic control, which can be achieved through multiple pathways, e.g. diet, activity, medication taking. Although the DSP included sessions on diet and activity, those focused primarily on their impact on glycaemic control in the person with diabetes, with much less attention to weight loss. Also, the LookAHEAD intervention was much longer (1 year vs. 4 months in the DSP). A longer intervention may have yielded evidence for ripple effects.
Strengths and limitations
The DSP trial is unique in that we engaged committed partners and included key elements of couples intervention trials; it was theoretically grounded; and it included an individual intervention comparator arm [27]. Other strengths include blinded assessments, the RCT design, a significant percentage of minority ethnic participants, and 1-year follow-up. Limitations include: data are specific to the DSP intervention, thus may not generalize to other interventions; self-report measures for diet and activity; and a sample that was older and in long-term committed relationships, thus results may not generalize to younger adults or shorter-term relationships. The percentage of people with diabetes using insulin was high, and partner behavioural changes may have been achieved in a sample who relied on oral medications only. The drop-out rate was somewhat high, and likely reflects the challenge of retaining two individuals, i.e. both partners. Finally, although some differences were statistically significant, it is not clear that they are clinically significant.
Conclusions
We have demonstrated that a couples intervention for persons with Type 2 diabetes to improve glycaemic control can have beneficial effects on partners’ diabetes distress and satisfaction with the relationship, and perhaps on depressive symptoms. Future research should explore how to enhance these positive emotional and relational changes and gain understanding of the underlying dynamics to develop tailored interventions. However, if the goal is to promote diet and activity changes that foster weight loss both in the person with diabetes and his/her partner, the intervention may need to specifically target those behaviours with the partner to be effective for them.
What’s new?
Interdependence theory suggests that couples interventions may have beneficial effects on both persons with diabetes and their participating partners, but couples interventions must be compared with equivalent individual interventions to validly assess these effects. The Diabetes Support Project (DSP) provided an opportunity to assess partner effects.
The DSP collaborative couples intervention resulted in significant improvements in partner diabetes distress and relationship satisfaction. There was no consistent effect on partner behavioural or medical outcomes.
A ‘ripple effect’ refers to a positive effect of an individual behavioural intervention on the untreated partners; we found no evidence of a dietary or activity behaviour ripple effect.
Engaging partners can benefit them emotionally and enhance the relationship. To help partners change behaviour, it may be necessary to target their behaviours directly.
Acknowledgements
We thank the late Dr Jacqueline Dimmock and Ms Pat Forken who provided expert project management for all aspects of the study. We thank the patients and partners who participated in the study. We thank the excellent educators, Pam Blackmer, Mary Griffin, Carina Lagua, Juliann Mellen, Jacqueline Pallas, Nancy Rindfuss, Christina Bellino Sullivan and Jennifer Vallone, who delivered the interventions. At SUNY Upstate Medical University, we thank Dr Roberto Izquierdo, who served as the Data and Safety Monitoring Official, and Dr Kasandra Scales, who supported all activities during the first year of the study, funded by an NIH Diversity Fellowship Supplement. At UCSF, we thank the research staff who performed assessments and recruitment activities, Ifeoma Okwu, Valerie Pintado and Tatum Toner. Finally, we thank Roche, Inc. who provided some material support.
Funding sources
This study was supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases, 1R18DK080867–01A2.
Footnotes
Parts of this study were presented in oral presentation at the Scientific Sessions of the American Diabetes Association, San Diego CA, June 2017.
Competing interests
DC, DH, JS and PMT reported no potential conflicts relevant to this article. LF reported that he serves as a consultant or member of an advisory board for Elli Lilly, Novo Nordisk and Abbott Diabetes Care. RSW reported that she receives research grant funding from Medtronic, Mylan GmbH Inc., Kowa Research Institute and Helmsley Charitable Trust/JDRF/JAEB Center for Health Research.
References
- 1.Wittenberg E, Prosser LA. Health as a family affair. N Engl J Med 2016; 374: 1804–1806. [DOI] [PubMed] [Google Scholar]
- 2.Rintala T-M, Jaatinen P, Paavilainen E, Astedt-Kurki P. Interrelation between adult persons with diabetes and their family: a systematic review of the literature. J Fam Nurs 2013; 19: 3–28. [DOI] [PubMed] [Google Scholar]
- 3.Fisher L, Chesla CA, Skaff MM, Mullan JT, Kanter RA. Depression and anxiety among partners of European-American and Latino patients with type 2 diabetes. Diabetes Care 2002; 25: 1564–1570. [DOI] [PubMed] [Google Scholar]
- 4.Kovacs Burns K, Nicolucci A, Holt RIG, Willaing I, Hermanns N, Kalra S et al. Diabetes Attitudes, Wishes and Needs second study (DAWN2): cross-national benchmarking indicators for family members living with people with diabetes. Diabet Med 2013; 30: 778–788. [DOI] [PubMed] [Google Scholar]
- 5.Stodberg R, Sunvisson H, Ahlstrom G. Lived experience of significant others of persons with diabetes. J Clin Nurs 2007; 16: 215–222. [DOI] [PubMed] [Google Scholar]
- 6.Shattuck AL, White E, Kristal AR. How women’s adopted low-fat diets affect their husbands. Am J Public Health 1992; 82: 1244–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelley HH, Thibaut TW. Interpersonal Relations: A Theory of Interdependence. New York: Wiley, 1978. [Google Scholar]
- 8.Rusbult CE, Van Lange PA. Interdependence, interaction and relationships. Annu Rev Psychol 2003; 54: 351–375. [DOI] [PubMed] [Google Scholar]
- 9.Falconier MK, Jackson JB, Hilpert P, Bodenmann G. Dyadic coping and relationship satisfaction: a meta-analysis. Clin Psychol Rev 2015; 42: 28–46. [DOI] [PubMed] [Google Scholar]
- 10.Trief PM, Fisher L, Sandberg J, Cibula DA, Dimmock J, Hessler DM et al. Health and psychosocial outcomes of a telephonic couples behavior change intervention in patients with type 2 diabetes: a randomized clinical trial. Diabetes Care 2016; 39: 2165–2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keogh KM, Smith SM, White P, McGilloway S, Kelly A, Gibney J et al. Psychological family intervention for poorly controlled type 2 diabetes. Am J Manag Care 2011; 17: 105–113. [PubMed] [Google Scholar]
- 12.Kang C-M, Chang S-C, Chen P-L, Liu P-F, Liu W-C, Chang C-C et al. Comparison of family partnership intervention care vs. conventional care in adult patients with poorly controlled type 2 diabetes in a community hospital: a randomized controlled trial. Int J Nurs Stud 2010; 47: 1363–1373. [DOI] [PubMed] [Google Scholar]
- 13.Gorin AA, Wing RR, Fava JL, Jakicic JM, Jeffery R, West DS, Brelje K et al. Weight loss treatment influences untreated spouses and the home environment: evidence of a ripple effect. Int J Obes (Lond) 2008; 32: 1678–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piantadosi S. Clinical Trials: A Methodologic Perspective. New York: Wiley, 1997. [Google Scholar]
- 15.Trief PM, Sandberg JG, Ploutz-Snyder R, Brittain R, Cibula D, Scales K et al. Promoting couples collaboration in type 2 diabetes: The Diabetes Support Project pilot data. Fam Syst Health 2011; 29: 253–261. [DOI] [PubMed] [Google Scholar]
- 16.Bandura A, Walters H. Social Learning Theory and Personality Development. New York: Wiley, 1978. [Google Scholar]
- 17.Laurenceau JP, Stanley SM, Olmos-Gallo A, Baucom B, Markman HJ. Community-based prevention of marital dysfunction: multilevel modeling of a randomized effectiveness study. J Consult Clin Psychol 2004; 72: 933–943. [DOI] [PubMed] [Google Scholar]
- 18.Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord 2009; 114: 163–173. [DOI] [PubMed] [Google Scholar]
- 19.Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and non-distressed couples: Construct hierarchy and multidimensional scales. J Marital Fam Ther 1995; 21: 289–308. [Google Scholar]
- 20.Thompson FE, Midthune D, Subar AF, Kahle LL, Schatzkin A, Kipnis V. Performance of a short tool to assess dietary intakes of fruits and vegetables, percentage of energy from fat and fibre. Public Health Nutr 2004; 7: 1097–1105. [DOI] [PubMed] [Google Scholar]
- 21.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395. [DOI] [PubMed] [Google Scholar]
- 22.IBM Corporation. IBM SPSS Statistics for Windows. Version 24.0. Armonk, NY: IBM Corporation; Released 2016. [Google Scholar]
- 23.Rook KS, August KJ, Stephens MAP, Franks MM. When does spousal control provoke negative reactions in the context of chronic illness? The pivotal role of patients’ expectations. J Pers Soc Psychol 2011; 28. doi: 10.1177/0265407510391335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tanaka R, Trief PM, Scales K, Weinstock RS. ‘Miscarried helping’ in adults with type 2 diabetes: Helping for Health Inventory-Couples. Fam Syst Health 2018; 35: 409–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sexton M, Bross D, Hebel JR, Schumann BC, Gerace TA, Lasser N et al. Risk-factor changes in wives with husbands at high risk of coronary heart disease (CHD). J Behav Med 1987; 10: 251–261. [DOI] [PubMed] [Google Scholar]
- 26.Schierberl Scherr AE, McClure Brenchley KJ, Gorin AA. Examining a ripple effect: do spouses’ behavior changes predict each other’s weight loss? J Obes 2013; 2013: 297268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell TA. Physical disorder and effectiveness research in marriage and family therapy In: Sprenkle D (ed.), Effectiveness Research in Marriage and Family Therapy. Alexandria, VA: American Association for Marriage and Family Therapy, 2002; 311–337. [Google Scholar]