Abstract
Objective:
This study aimed to document population-level trends in mental health service utilization by college students.
Methods:
The study drew on 10 years of data from the Healthy Minds Study, an annual web-based survey, with a sample comprised of 155,026 students from 196 campuses. Analyses focused on past-year mental health treatment and lifetime diagnoses of a mental disorder. Changes in symptoms of depression and suicidal ideation and levels of stigma were hypothesized as potential explanatory factors.
Results:
Rates of treatment and diagnosis increased significantly. The rate of treatment increased from 19% in 2007 to 34% by 2017, while the percentage of students with lifetime diagnoses increased from 22% to 36%. The prevalence of depression and suicidality also increased, while stigma decreased.
Conclusions:
This study provides the most comprehensive evidence to date regarding upward trends in mental health service utilization on U.S. campuses over the past 10 years. Increasing prevalence of mental health problems and decreasing stigma help to explain this trend.
Keywords: Mental health service utilization, trends in diagnosis and treatment, mental health stigma, college student mental health review
Student mental health is a significant and growing concern on college campuses across the United States. An estimated one-in-three students meets criteria for a clinically significant mental health problem (1). There is limited trend data examining prevalence rates over time, but existing research suggests that there have been large increases in psychopathology among college students in recent decades (2). There is also evidence to suggest a rise in the number of students enrolling in college with preexisting mental health conditions (3). In response to the increasing severity and complexity of mental health problems, more than 95% of counseling center directors report that meeting the needs of students with significant psychological problems is a growing concern on their campus (4).
A key question is whether increasing prevalence rates translates to students’ use of mental health services. Clinical data on treatment utilization over time show steady increases in the number of students utilizing mental health care. One study found that the growth in counseling center appointments from 2009 to 2014 (30%) was six times greater than the rate of growth in institutional enrollment (5%); 88% of counseling centers reported an increase in student treatment-seeking over this five-year period (5).
Data on mental health service utilization over time have been drawn largely from clinical samples. These data are important but provide an incomplete picture, given that students use a wide variety of mental health services, including services in the communities surrounding their campuses and in their hometowns. To complement this research, there is a need to examine trends in service utilization at a population level.
Using national survey data, this study aimed to document population-level trends in mental health service utilization by college students over the past decade, as well as changes in potential explanatory factors, such as students’ symptoms and attitudes toward mental illness. This is the first paper to report national trends in mental health service utilization from the Healthy Minds Study (HMS), the largest and most comprehensive study of mental health in college populations. We discuss implications of these trends for the campus mental health system.
Methods
HMS is an annual web-based survey examining mental health, service utilization, and related factors among undergraduate and graduate students (6). In this study, we analyzed HMS data from 2007–2017. At each participating institution, our team recruited a random sample of 4,000 degree-seeking students from the full population; at smaller institutions, we recruited all students. Students had to be at least 18 years old to participate; there were no other exclusion criteria. Students were recruited via email. Upon clicking the survey link, students were presented with an informed consent page and were required to agree to the terms of participation before entering the survey. To incentivize participation, students were informed of their eligibility for one of several prizes totaling $2,000 annually.
Response rates were as follows: 43% in 2007, 42% in 2009, 25% in 2010, 26% in 2011, 23% in 2012, 29% in 2013, 23% in 2014–2015, 27% in 2015–2016, and 23% in 2016–2017. The likely reason for lower participation rates since 2009 was the discontinuation of postal mailings with $1 bills as a “pre-incentive” introducing the study; that change was made to reduce study cost. The incentive process was the only aspect of survey administration that changed; web-based data collection remained consistent across years. To adjust for potential differences between responders and nonresponders, we constructed sample probability weights. We obtained administrative data from participating institutions, including gender, race/ethnicity, academic level, and grade point average. We used this data to construct response weights, equal to 1 divided by the estimated probability of response, using a logistic regression to predict the likelihood of response associated with each variable.
HMS was approved by the institutional review boards on all campuses.
We examined four binary outcomes related to mental health service utilization: past-year therapy or counseling; past-year psychotropic medication use; past-year treatment (therapy or counseling and medication use); and lifetime diagnosis of a mental disorder. We also examined trends in location of services (on-campus; psychiatric emergency services, partial hospitalization, or inpatient psychiatric hospital; and locations not captured in the first two categories).
We examined two binary measures of mental health: depression and suicidal ideation. Symptoms of depression over the past two weeks were measured by using an adapted version of the Patient Health Questionnaire–2 (PHQ-2) (7). We used the standard PHQ-2 cutoff of ≥3 as a positive screen for depression. The PHQ-2 was added to HMS in 2009; the 2007 data were excluded from analyses involving this measure. A single question measured suicidal ideation: “In the past year, did you ever seriously think about attempting suicide?” Students answered “yes” or “no” and were categorized accordingly.
We also examined two binary measures of stigma: perceived stigma and personal stigma. Stigma was classified as a response of “strongly agree,” “agree,” or “somewhat agree” to the statement “most people think less of a person who has received mental health treatment” (perceived stigma) and “I would think less of a person who has received mental health treatment” (personal stigma).
Analyses were descriptive in nature, designed to document changes in service utilization over the past decade. We calculated service utilization rates by year, reporting the proportion of all students in a given year with past-year therapy/counseling, past-year medication use, past-year treatment, and any lifetime diagnosis of a mental disorder; we also report utilization rates by year among students with depression. Analyses were conducted by using Stata 14.2 and weighted using the weights described above.
Results
The sample is comprised 155,026 students from 196 U.S. campuses. Just over half identified as female (56.5%), two-thirds were between ages 18 and 22 (66.8%), and roughly three-quarters were white (74.0%). Overall, 26.9% screened positive for depression and 8.2% reported suicidal ideation. The proportion of students with a positive PHQ-2 score increased with each year (from a low of 24.8% in 2009 to a high of 29.9% in 2016–2017). We also found that suicidal ideation steadily increased over the past decade, from 5.8% in 2007 to 10.8% in 2016–2017.
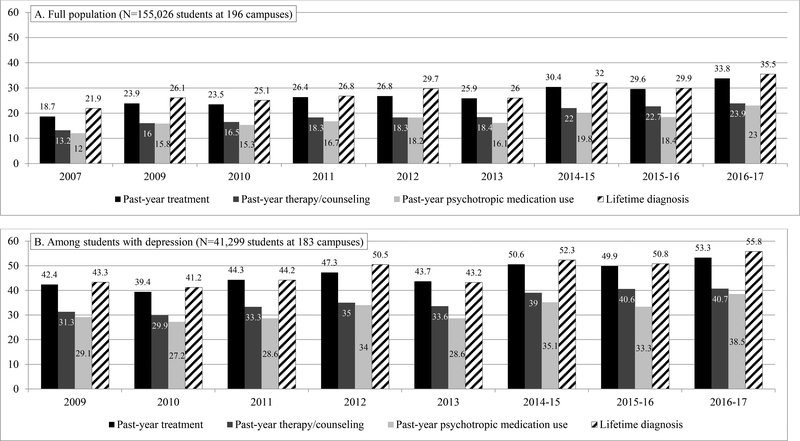
From 2007 to 2017, we found increases across all measures of service utilization, both in the full sample and among students with depression (Figure 1). Rates of past-year treatment for the full sample increased from 18.7% in 2007 to 33.8% in 2016–2017, with similar patterns for both therapy/counseling and medication use. The proportion of students with a diagnosed mental health condition increased from 21.9% in 2007 to 35.5% in 2016–2017. In later years (2014–2017), rates of both treatment and diagnosis were at or above 30% each year. Among students with depression (N=41,299), rates of past-year treatment went from 42.4% in 2009 to 53.3% in 2016–2017, and diagnosis from 43.3% to 55.8%, with rates of nearly 50% or more for both treatment and diagnosis in later years.
FIGURE 1. MENTAL HEALTH SERVICE UTILIZATION BY SURVEY YEAR (%).
Notes: Past-year treatment is any past-year therapy/counseling and/or psychotropic medication use. In Figure 1b, depression is defined as a score of ≥3 on the adapted PHQ-2; PHQ-2 data unavailable for 2007.
The most common location for receiving services was on campus, with rates increasing from 6.6% in 2007 to 11.8% in 2016–2017. Rates of psychiatric emergency service utilization showed general upward trends, with 0.3% seeking such services in 2007 and 1.0% in 2016–2017. Similarly, service use from other locations increased from 5.2% in 2007 to 8.7% in 2016–2017.
Rates of both perceived and personal stigma decreased over time, from 64.2% to 46.0% and from 11.4% to 5.7%, respectively. Among students with depression, there was no noticeable change in levels of perceived stigma over time, but personal stigma decreased from 8.2% to 5.1%.
Discussion
In this large, national sample of college students, we find that mental health service utilization has increased substantially between 2007 and 2017. Rates of past-year treatment nearly doubled during this time (from 19% to 34%). In the most recent year of data collection, more than 10% of the overall student population sought services at their campus counseling. Similarly, rates of diagnosed mental health conditions increased by approximately two-thirds, with over one-third of students reporting a diagnosed condition in 2016–2017.
Consistent with prior studies, we find that rates of depression and suicidality also increased during this time (1–3). Another factor that may help to explain the rise in treatment-seeking is that levels of stigma have notably decreased during the past decade, with levels of personal stigma much lower than perceived stigma. Prior research with college populations has revealed that personal stigma (but not perceived stigma) is associated with treatment-seeking (8, 9).
The trends revealed in this study have strained counseling centers across the country, given that many are under-resourced and operate at full capacity with waitlists for much of the year (5). There are a multitude of approaches to consider for alleviating this strain, including universal prevention programs and rapid referral to community treatment. Additionally, digital mental health programs, often delivered via mobile apps, offer the possibility of expanded treatment accessibility while circumventing barriers to traditional treatment, such as time and convenience (10, 11). Research has revealed that students hold generally favorable attitudes toward online mental health services, and a majority report willingness to use such services (12). A recent meta-analysis of digital interventions for college students found that these types of interventions can be effective in improving depression, anxiety, and stress (13). Methods for offering these types of programs independently or in conjunction with professional support through counseling centers continue to be explored as ways to engage students while minimizing burden on service delivery systems.
The implications of these findings are strengthened by the use of a large, national sample over the past 10 years, the focus on population-level data (not just clinical data), and the opportunity to explore measures of service use together with potential explanations for why rates of mental health service utilization have increased. Along with its strengths, there are several limitations to consider when interpreting results of this study. First, HMS had modest response rates, as is typical for online surveys. While sample probability weights adjusted for potential differences between responders and non-responders along known demographic and academic characteristics, these adjustments do not necessarily correct for response bias related to other characteristics, including mental health status and treatment history. Second, we cannot determine the quality of mental health services and whether they conform to evidence-based guidelines, which is an important question for additional research. Finally, we relied on a single item to measure perceived and personal stigma; these are complex constructs informed by a robust body of empirical and theoretical literature, and we recognize that our brief measures do not capture the full nature of stigma.
Conclusions
This study provides the most comprehensive evidence to date regarding population-level trends in mental health service utilization on U.S. college campuses. We find that utilization increased substantially over the past decade, with much of this burden falling to campus counseling centers. Potential explanatory factors, as identified in this study, include increased prevalence of mental health problems in college populations and decreased stigma over time. To better meet the mental health care demand from students and reduce strain on existing services, campuses may wish not only to expand capacity but also to increase the use of preventive and digital mental health services, such as those delivered via mobile apps.
Acknowledgments
Dr. Lattie is supported by a research grant from the National Institute of Mental Health (K08 MH112878) and has received consulting fees from Actualize Therapy, LLC.
Footnotes
The authors report no financial relationships with commercial interests.
Contributor Information
Sarah Ketchen Lipson, Department of Health Law Policy and Management, Boston University School of Public Health, Boston (Lipson)
Emily G. Lattie, Department of Medical Social Sciences and Department of Preventive Medicine, Northwestern University Feinberg School of Medicine, Chicago (Lattie)
Daniel Eisenberg, Department of Health Management and Policy, University of Michigan School of Public Health, and Population Studies Center, University of Michigan Institute for Social Research, Ann Arbor (Eisenberg).
References
- 1.Eisenberg D, Hunt J, Speer N: Mental health in American colleges and universities: variation across student subgroups and across campuses. J Nerv Ment Dis 2013; 201:60–67 PubMed [DOI] [PubMed] [Google Scholar]
- 2.Twenge JM, Gentile B, DeWall CN, et al. : Birth cohort increases in psychopathology among young Americans, 1938–2007: a cross-temporal meta-analysis of the MMPI. Clin Psychol Rev 2010; 30:145–154 PubMed [DOI] [PubMed] [Google Scholar]
- 3.Haas AP, Hendin H, Mann JJ: Suicide in college students. Am Behav Sci 2003; 46:1224–1240 [Google Scholar]
- 4.Mistler B, Reetz DR, Krylowicz B, et al. : The Association for University and College Counseling Center Directors Annual Survey. Indianapolis, Association for University and College Counseling Center Directors, 2012. www.aucccd.org/director-surveys-public [Google Scholar]
- 5.Xiao H, Carney DM, Youn SJ, et al. : Are we in crisis? National mental health and treatment trends in college counseling centers. Psychol Serv 2017; 14:407–415 PubMed [DOI] [PubMed] [Google Scholar]
- 6.Healthy Minds Study. Ann Arbor, MI and Boston, MA, Healthy Minds Network, 2018. healthymindsnetwork.org/research/hms [Google Scholar]
- 7.Eisenberg D, Chung H: Adequacy of depression treatment among college students in the United States. Gen Hosp Psychiatry 2012; 34:213–220 PubMed [DOI] [PubMed] [Google Scholar]
- 8.Golberstein E, Eisenberg D, Gollust SE: Perceived stigma and mental health care seeking. Psychiatr Serv 2008; 59:392–399 [DOI] [PubMed] [Google Scholar]
- 9.Lipson S, Kern A, Eisenberg D, et al. : Mental health disparities among college students of color: results from a national survey study. J Adolesc Health 2018; 63:348–356 [DOI] [PubMed] [Google Scholar]
- 10.Renton T, Tang H, Ennis N, et al. : Web-based intervention programs for depression: a scoping review and evaluation. J Med Internet Res 2014; 16:e209 PubMed [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rai M, Vigod SN, Hensel JM: Barriers to office-based mental health care and interest in e-communication with providers: a survey study. JMIR Mental Health 2016; 3:e35 PubMed [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunbar MS, Sontag-Padilla L, Kase CA, et al. : Unmet mental health treatment need and attitudes toward online mental health services among community college students. Psychiatr Serv 2018; 69:597–600 PubMed [DOI] [PubMed] [Google Scholar]
- 13.Davies EB, Morriss R, Glazebrook C: Computer-delivered and Web-based interventions to improve depression, anxiety, and psychological well-being of university students: a systematic review and meta-analysis. J Med Internet Res 2014; 16:e130 PubMed [DOI] [PMC free article] [PubMed] [Google Scholar]