Abstract
PURPOSE:
The pediatric emergency department (PED) provides care for adolescents at high risk of unintended pregnancy, but little is known regarding the efficacy of PED-based pregnancy prevention interventions. The objectives of this PED-based pilot intervention study were to (1) assess the rate of contraception initiation after contraceptive counseling and appointment facilitation in the PED during the study period (2) identify barriers to successful contraception initiation and (3) determine adolescent acceptability of the intervention.
METHODS:
This pilot intervention study included females 14–19 years of age at risk for unintended pregnancy. Participants received standardized contraceptive counseling and were offered an appointment with Gynecology. Participants were followed via electronic medical record and phone to assess contraception initiation and barriers. Chi-square tests were used to examine the association between contraception initiation and participant characteristics.
RESULTS:
One hundred forty-four patients were eligible, and 100 were enrolled. In the PED, 68% (68/100) expressed interest in initiating hormonal contraception, with 70% (48/68) of interested participants, indicating long acting reversible contraception (LARC) was their preferred method. Twenty-five percent (25/100) of participants initiated contraception during the study period, with 19 participants starting LARC. Thirty-nine percent (22/57) of participants that accepted a gynecology appointment, attended that appointment. Barriers to follow-up include transportation and inconvenient follow up times. Participants were accepting of the intervention with 93% agreeing that the PED is an appropriate place for contraceptive counseling.
CONCLUSIONS:
PED contraceptive counseling is acceptable among adolescents and led to successful contraception initiation in 25% of participants. The main barrier to contraception initiation was participant follow up with the gynecology appointment.
Keywords: Contraception, Pregnancy in adolescents, Long acting reversible contraception (LARC), Pediatric emergency medicine
Unintended teen pregnancy is a significant public health problem that affects thousands of adolescent females in the United States each year.1 Despite a decline in the teen pregnancy rate, there are still over 450,000 adolescent females who become pregnant in the U.S. annually, which is the highest teen pregnancy rate among all developed countries.2 Unintended teen pregnancy has proven negative health and social consequences for the mother, father and infant.3–5 The vast majority (75%) of teenage pregnancies are unintended, indicating a substantial unmet need for effective and reliable contraception.6 Long acting reversible contraceptives (LARC), which include intrauterine devices (IUD) and the contraceptive implant, are the most effective forms of contraception and are safe in adolescent females.7 The American College of Obstetricians and Gynecologists and the American Academy of Pediatrics both recommend that LARC be offered as first line contraception in adolescent females; however, only up to 7% of sexually active adolescents use LARC.7–9 The Contraceptive CHOICE project completed in St. Louis, Missouri showed a significant decline in teen pregnancy rates by offering no cost contraception to adolescents in the community at risk for unintended pregnancy after “LARC-first” contraceptive counseling (counseling that offers contraceptive options in order of efficacy).10
The pediatric emergency department (PED) provides care for adolescents who are at high risk for unintended pregnancy.11–13 In one study conducted in an urban PED, nearly one-third of adolescent females ages 15–19 were either pregnant or at high risk of becoming pregnant in the next year.12 Studies have also shown that adolescent females seeking care in the PED would welcome contraception counseling at the time of the PED visit.11,12,14,15 However, it is unclear if contraceptive counseling in the PED is an effective mechanism for increasing contraception initiation.
The study team, with members from pediatric emergency medicine and adolescent gynecology, worked collaboratively to address pregnancy prevention for the high risk PED population. We designed an intervention based on the contraceptive CHOICE project that involved contraceptive counseling and a facilitated gynecology follow up appointment for contraception initiation among participants with a desire to initiate contraception. Previous studies show low rates of follow up when referred from the ED.16 To our knowledge, no studies have shown rates of follow up after a PED intervention with a facilitated appointment (i.e patient given appointment date, time, and location while in PED as opposed to referral requiring the patient to call and schedule an appointment). Thus, we designed a pilot intervention study to (1) assess rates of contraception initiation after contraceptive counseling and appointment facilitation in the PED during the study period (2) identify barriers to successful initiation and (3) determine adolescent acceptability of the intervention.
METHODS
Study design and setting
This is a single site pilot quasi experimental study with no comparison group conducted at an urban Level 1 PED with approximately 60,000 annual visits. The local Institutional Review Board approved the study with a waiver of documented informed consent/assent and waiver of parental consent. Parental consent was waived because contraceptive counseling does not require parental permission outside of the research study, the study confers minimal risk to the patient, and requiring parental permission would prevent many adolescents from participating.17 We obtained verbal consent from the participant prior to enrollment. We anticipated at least one-fold increase in the rate of successful start of LARC after the intervention from the national rate of 7%, and a sample size of 100 participants will achieve over 90% power to detect a one-fold increase from the national rate (from 7% to 14%) based on two-sided binomial test.
Study participants
Participants were a non-consecutive, convenience sample of adolescent females 14–19 years of age who presented to the PED with any chief complaint and screened at risk for unintended pregnancy. Females meeting all of the following criteria on the screening survey were considered at risk for unintended pregnancy: 1) sexually active with a male partner at any point in her lifetime or intent to become sexually active with a male partner within the next 6 months, 2) no desire for pregnancy in the next 12 months 3) not currently using a LARC method and 4) not currently pregnant per patient report. These screening questions were based on the inclusion criteria used in the Contraceptive CHOICE project.10 We included patients using a Tier 2 contraceptive method (oral contraceptive pill, contraceptive patch, contraceptive vaginal ring, and depo-provera injection) since they may benefit from access to Tier 1 methods (IUD and contraceptive implant). Exclusion criteria included previous hysterectomy or sterilization procedure, altered mental status from injury or medication, developmental delay, non-English speaking, presenting for psychiatric evaluation, presenting for sexual assault, previous participation in this study, or if the screening survey could not be completed confidentially (i.e. alone in the room without family/friends present). While patients presenting for psychiatric evaluation or sexual assault may benefit from contraceptive counseling, we felt these were vulnerable populations presenting during a time of crisis and did not include them in the study. Patients were also excluded if they had a positive pregnancy test in the PED, obtained as part of their clinical care. A negative pregnancy test was not required, as pregnancy testing was completed at the Gynecology visit.
Intervention
The study intervention was a two part process consisting of a contraceptive counseling session and an appointment facilitation with Gynecology at our institution for those desiring to initiate contraception. Participants also agreed to allow the principal investigator (PI) to follow up at 60 days (± 2 weeks) via electronic medical record (EMR) and phone.
Contraceptive Counseling
The contraceptive counseling was designed based on the counseling method used in the CHOICE project, which modeled their intervention after the GATHER process for counseling.18 GATHER is a client-centered process that focuses on the woman, her needs, and concerns. The CHOICE project also used a “LARC-first” counseling method which counsels about Tier 1 methods (LARC) first, followed by Tier 2 methods. The PI reviewed the CHOICE project script, training module, and contraceptive fact sheets that were made available to the public.19 The script was modified to fit our setting and used as a guide during the counseling session. Models of the IUD, contraceptive implant, and vaginal ring were available to aid participant education. If a participant indicated a preferred method of contraception, the fact sheet on that particular method was reviewed to assess for contraindications. If the participant preferred LARC, we also reviewed information provided by our Pediatric and Adolescent Gynecology department in preparation for the procedure.
The contraceptive counseling was completed by the PI or one of two study-trained resident physicians. With the PI present, the two study-trained physicians reviewed counseling session videos provided by the CHOICE project. The PI reviewed all study procedures with both study-trained physicians and was available in the PED during their first counseling session to answer any questions in real time. The two study-trained physicians also notified the PI after every enrollment and any patient concerns or questions were addressed by the PI.
Facilitated Appointment
The second part of the intervention was appointment facilitation with our institution’s Pediatric and Adolescent Gynecology clinic for participants who desired to start contraception. The outpatient Gynecology clinic is staffed by gynecologists with specialty training in pediatric and adolescent gynecology, and they see patients by appointment only. Gynecology reserved approximately 10 appointments per month that were available to study patients and could be scheduled by the PI, regardless of the time of day the PED visit occurred. The participant was able to choose an appointment time available within the next 60 days. Ideally, appointments were scheduled within 30 days, however if there was concern for cervicitis or pelvic inflammatory disease in a patient opting for an IUD or if the participant preferred a particular date, appointments were scheduled outside of this time frame by the PI. The participant left the PED visit with an appointment time, date, and location provided on a reminder card. Gynecology was made aware of scheduled appointments by the PI on the next business day. The participant was contacted by the Gynecology staff to register for the appointment and review their policies. Per department policy, Gynecology obtains parental/guardian consent to treat and bill at all new visit appointments. Gynecology agreed to waive the cost for contraception for any uninsured patient or for patients whose insurance denied coverage.
Study procedures
All study procedures, including screening, were completed in the patient’s treatment room in the PED. Participants completed a pre-intervention questionnaire followed by the intervention and an immediate post-intervention survey. The pre-intervention questions were read to the participant and answers recorded in a REDcap database. The main goal of the pre-intervention questions was to gather information about the participant to help understand her contraceptive needs and goals in preparation for the intervention. Many of the pre-intervention survey questions were from the Youth Risk Behavioral Surveillance System.20 These specific data were not further analyzed. For participants who were not receptive to starting contraception following the counseling session, each answered open ended and multiple choice questions about reasons for refusal and barriers. At completion of the intervention, participants were given a tablet to answer three questions regarding their opinions on the intervention. All questions were developed by the study team and pilot tested to ensure adequate content validity.
We completed a review of the EMR to assess for attendance at the Gynecology appointment and contraception initiation. Participants were contacted via text and/or phone call approximately 60 days following the index PED visit. A designated study phone with a non-hospital based number was used for all participant contact. Three text/phone call attempts were made. Participants were called first. If there was no answer, participants were texted explaining what the call was about and asking them to return the call or notify us of a time they could be reached. The follow up survey was conducted using voice to voice phone contact. This survey assessed for barriers to starting contraception, and contraception initiation outside of our institution that would be missed by EMR review. We attempted to contact all participants. Those who scheduled an appointment but did not attend their appointment were asked more specific questions about reasons for not attending the appointment.
Data analysis
Our primary outcome measure, the rate of successful contraception initiation after PED-based contraceptive counseling, was defined as initiation of a Tier 1 contraceptive method, initiation of a Tier 2 method, or changing from a Tier 2 to a Tier 1 method during the study period. We included initiation of Tier 1 and Tier 2 methods in our primary outcome, as the overarching purpose of the intervention was to reduce pregnancy risk in adolescent females, which can be accomplished by both Tier 1 and Tier 2 methods. Determination of successful start was through EMR review and/or verbally from the participant at the 60 day phone follow up. Chi-Square or Fisher’s exacts were used to assess relationships between successful contraception initiation and multiple variables including age, race, chief complaint (dichotomized as non-reproductive or potentially-reproductive), relationship status, and time to appointment. Odds ratios were used to quantify the association of these variables with the successful contraception initiation. Chi-square tests were also used to assess whether there were significant differences in the successful contraception initiation among the three counselors, and analysis of variances (ANOVA) were used to test whether there was any difference in the mean length of intervention among the three counselors. Our secondary outcome measure, participant-centered barriers to initiating contraception with our intervention, are reported as descriptive data. Data were collected directly into a REDCap database, and SAS (Version 9.1.4; Cary, NC) was used to conduct data analysis.
RESULTS
Subjects were enrolled from January 2016 – March 2017. Among 388 adolescent females screened, 144 were eligible. The primary reason for ineligibility was reported lack of sexual activity (194/388; 50%). Of those eligible (n=144), 101 (70%; 101/144) agreed to participate. One potential participant left prior to completion of enrollment, thus 100 were enrolled. Table 1 shows the demographic data of our eligible (n=144) and enrolled populations (n=100). There was no significant differences between the eligible and enrolled populations. The study population had a mean age of 17 (±1.31) years and was 58% black.
Table 1:
Demographic Data of Eligible Participants Agreeing and Declining Enrollment
| Total Eligible N=144* | ||||
|---|---|---|---|---|
| Enrolled n=100 n (%) |
Declined Enrollment n=43 n(%) |
P-value | ||
| Race | Black | 58 (58) | 23(53) | 0.83 |
| White | 38(38) | 18 (42) | ||
| Other | 4 (4) | 2 (5) | ||
| Ethnicity | Hispanic | 3(3) | 0 (0) | 0.25 |
| Non-Hispanic | 97(97) | 43 (100) | ||
| Age in years | 14–15 | 14(14) | 10 (23) | 0.38 |
| 16–17 | 52 (52) | 19 (44) | ||
| 18 – 19 | 34 (34) | 14 (33) | ||
| Insurance status | Commercial | 32(32) | 15 (35) | 0.81 |
| Medicaid | 55(55) | 24 (56) | ||
| Self - Pay | 13(13) | 4 (9) | ||
| Chief complaint | Sexual Health Related |
56(56) | 20(47) | 0.29 |
| Non-Sexual Health Related |
44(44) | 23(53) | ||
1 eligible patient left prior to completion of enrollment
All 100 participants received contraceptive counseling. Sixty-eight participants expressed interest in initiating hormonal contraception after counseling, and 57 scheduled an appointment with Pediatric and Adolescent Gynecology (Figure 1). Of the 57 participants who scheduled an appointment, 22 (22/57; 39%) attended the appointment. The mean time to appointment was 20 (±18) days. Twenty-one participants who attended the appointment initiated contraception. One was pregnant at the time of the appointment, and therefore not started on contraception. Four other participants reported going to another provider and starting contraception during the study period, for a total of 25 participants with contraception initiation.
Figure 1:
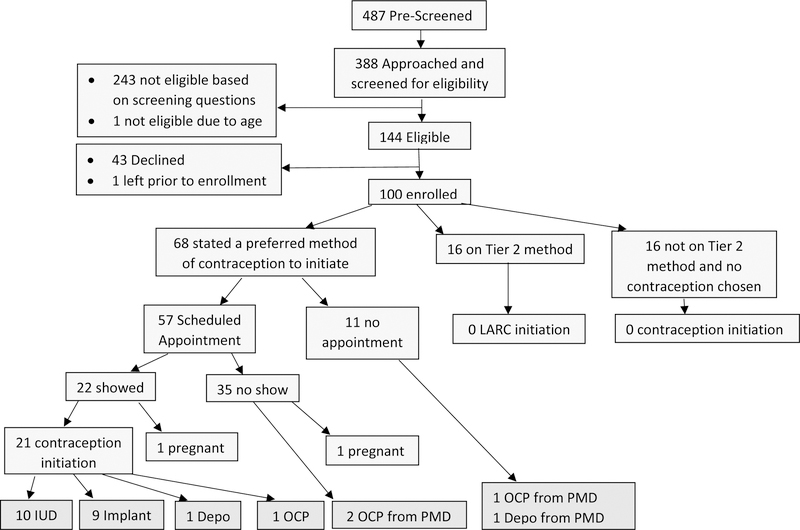
Flow Diagram of Study Recruitment and Participants.
Of the remaining 32 participants who received contraceptive counseling but did not express interest in initiating new contraception during the study period, sixteen participants were already on a Tier 2 method when they enrolled, and none of those participants opted to start LARC. The remaining 16 participants were not using a tier 2 method and chose not to start contraception and refused a gynecology appointment (Figure 1). The top barrier reported by these 16 participants was a concern about the side effects of contraception (7/16; 44%) and participant perception of low pregnancy risk (3/16; 19%). Two (2/11; 18%) participants identified the requirement for parental consent at the gynecology appointment as their main reason for not scheduling an appointment.
The majority (70%; 48/68) of those with interest in contraception initiation expressed a preference for LARC with 28 preferring hormonal IUD and 20 preferring the contraceptive implant. Nineteen adolescents completed follow up appointments and were started on LARC. The study participant rate of LARC initiation was 19%.
The bivariate analysis (Table 2) demonstrated no significant association between successful contraception initiation and age, race, relationship status, sexual health related chief complaint, insurance status, previous pregnancy, or appointment time < 14 days from index PED visit.
Table 2:
Bivariate Analysis Demonstrating Association between Variables and Successful Contraception Initiation
| Variable | Total with characteristic n= 100 |
Total with characteristic and successful start n= 25 |
Odds Ratio with 95% CI |
P- value | |
|---|---|---|---|---|---|
| Age in years | 14–15 | 14 | 3 | 1 | 0.16 |
| 16–17 | 52 | 17 | 1.78 (0.44, 7.24) | ||
| 18–19 | 34 | 5 | 0.63 (0.13, 3.10) | ||
| Race | Black | 58 | 15 | 1 | 0.99 |
| White | 38 | 9 | 0.94 (0.36, 2.44) | ||
| Other | 4 | 1 | 0.98 (0.09, 10.13) | ||
| Chief complaint | Sexual Health Related |
56 | 15 | 1.24 (0.50, 3.12) | 0.64 |
| Non-Sexual Health Related |
44 | 10 | 1 | ||
| Relationship statusa | In a relationship |
61 | 16 | 1.15 (0.45, 2.94) | 0.78 |
| Not in relationship |
38 | 9 | 1 | ||
|
Time to appointment:b |
> =14 days | 31 | 12 | 0.86 (0.30, 2.49) | 0.78 |
| < 14 days | 26 | 11 | 1 | ||
| Pregnant beforea | Yes | 13 | 1 | 0.22 (0.03, 1.75) | 0.12 |
| No | 86 | 24 | 1 | ||
| Insurance status | Commercial | 32 | 8 | 1 | 0.98 |
| Medicaid | 55 | 14 | 1.02 (0.38, 2.80) | ||
| Self-Pay | 13 | 3 | 0.90 (0.20, 4.11) | ||
n=99 due to missing data
n= 57 with characteristic of scheduling appointment, n= 23 with scheduled appointment and successful contraception initiation.(21 showed to appointment and started contraception, 2 scheduled but missed appointment and started by another provider in study period)
Contact was attempted for all 100 participants, and 70 % (70/100) were reached by phone in follow-up. Eighteen of the participants that started contraception were reached by phone and answered all follow up questions. All 18 participants were still using the form of contraception initiated and 17/18 expressed satisfaction with current method and intended continued use for one year. One participant was not satisfied due to undesired side effects.
Of the 35 participants that scheduled an appointment, but did not attend the appointment, 23 (23/35; 65%) were reached by phone and participated in the follow up survey. Transportation (8/23; 35%) was the top barrier cited as the reason for not attending the follow-up appointment. Other frequently cited barriers included inconvenient appointment times (5/23; 22%), side effect concerns (3/23; 13%), and forgotten appointments (3/23; 13%).
Participants that cited transportation as their reason for failure to show were asked if a cab voucher would have helped them in attending their chosen appointment time and all (8/8; 100%) responded yes. Participants that scheduled an appointment but did not attend were asked during phone follow up if they would have started contraception in the PED at the time of counseling if made available, and 77% (17/22) stated they would have started contraception in the PED. (One participant with missing data for this question.)
Participants were also asked three questions regarding their opinion on the intervention at completion of the survey. Almost all participants (97/100) agreed with the statement “The information that I received in the emergency room today will help me prevent pregnancy.” Additionally, 93% (93/100) agreed with the statement “I believe the emergency room is a good place to have contraceptive counseling offered to patients,” and 88% (88/100) thought pregnancy prevention counseling should be offered to all adolescent females in the emergency department regardless of chief complaint.
The mean time of the intervention was 26.9 minutes (SD ± 11.7) and the median time was 24.5 minutes (range 10 to 67 minutes). The counseling session was interrupted as needed for clinical care. Based on two-sample t-test, the mean length of the intervention was longer when a preferred contraceptive method was stated as compared to when no preferred method was identified (21.6 min vs 29.4 min, p=0.0016). There was no difference in the rate of successful contraception initiation or the mean length of intervention among the three counselors.
DISCUSSION
This study aimed to evaluate the utility of a PED contraception counseling intervention to increase contraceptive initiation among the PED population. Successful contraception initiation among 25 adolescents is of the utmost importance as it significantly decreases their individual risk for pregnancy. However, on a larger scale, this study suggests that the PED may be an important setting for pregnancy prevention services for a high-risk population.
Our rate of contraception initiation in this pilot study was higher than similar PED-based studies on pregnancy prevention.16 One such study had a 7% follow up appointment show rate after offering wallet cards advertising a family planning clinic to adolescent females at risk for pregnancy in the PED.16 The main enhancement in our intervention is the dedicated time a study-trained physician spent conducting contraception counseling and appointment facilitation.16
While our overall success rates were encouraging, we recognize that there was a no show rate of 61% (35/57). This is comparable to other show rates for PED referrals in the adolescent population21; however, this is still concerning given that the participants were all at risk for pregnancy and left the PED without contraception. The CDC recommends same day initiation of contraception whenever possible, if the provider can be reasonably certain the patient is not pregnant.22 Miller et al. found the majority (66%) of adolescents surveyed in the PED were interested in same day contraception initiation.23 Similarly, in our study, the majority of participants that did not attend their appointment stated they would have started contraception in the PED. While there are several barriers to contraception initiation in the PED, this study suggests that providing counseling and facilitation for a contraceptive initiation appointment may overcome some of these barriers and would likely benefit many young women.
As previously stated, the Pediatric and Adolescent Gynecology Division at our institution requires parental consent at initial visits, either in person or via telephone. This consent covers any testing or treatment performed at the current and future visits. While they do not require parental consent for individual contraceptive methods, there was concern that need for initial parental consent would be a barrier for patients. Only two patients that refused gynecology appointment reported the requirement for parental consent as a barrier. Many providers, including those at Title X clinics, offer confidential contraceptive services, which is imperative for many adolescents. However, the requirement for parental consent was not a significant barrier to contraception initiation in this study.
Many studies report cost concerns as a barrier to contraception initiation, especially LARC.25 Gynecology agreed to waive the cost for contraception among any uninsured patient or among those whose insurance denied coverage. Patients were informed of this process at the time of enrollment, therefore removing cost as a barrier. This study also showed that there was no association between insurance status and successful contraception initiation. However, at final review, it was noted that insurance was billed and the covered costs of contraception among all participants initiating contraception.
The study intervention was conducted by the PI or a study trained physician, rather than a physician on a clinical shift. This intervention would likely not be feasible to conduct during clinical time due to competing priorities and provider time constraints for adequate contraceptive counseling. While we believe the in-person physician intervention was a component of our success, there are other options for implementation in the PED setting, such as video-based counseling or a health promotion advocate. A recent study demonstrated the potential benefits of a health promotion advocate in the PED,26 and contraceptive counseling may be another beneficial use of an advocate.
At our institution, we are continuing to work with collaborators from the emergency department, adolescent medicine, and gynecology to address this challenge of identifying and providing contraception for adolescents at risk for pregnancy in the PED. Future interventions will be aimed at overcoming the barrier of the low attendance rate at follow up appointments identified in this study. Cab vouchers and same day/next day appointments are interventions that may improve follow up rates.
LIMITATIONS
This study is not without limitations. This is a pilot study without a control group for direct comparison, which limits our ability to draw definitive conclusions regarding efficacy. These data are specific to a single institution, thus may not be generalizable to other institutions. Also, due to the exploratory nature of the study, we did not adjust for multiple comparisons so the actual Type I error rate might be larger than the specified type I error rate of 0.05. There was no fidelity monitoring among counselors and counseling may have differed slightly among the three physicians completing contraceptive counseling in the PED; however, all were trained equally per the CHOICE project materials. The requirement for parental consent also limits the generalizability, as adolescents accepting of the need for parental consent may be different from the general population. This is a convenience sample of participants enrolled when the PI or study physician was available to complete the intervention. Participants self-selected and agreed to participate knowing that contraceptive counseling and appointment facilitation would be offered.
CONCLUSIONS
The PED providers care for a patient population at high risk for unintended pregnancy, and adolescent females are receptive to contraceptive counseling in the PED. Our intervention of contraceptive counseling and appointment facilitation led to contraception initiation in 25% of participants. The main barrier to contraception initiation was participant follow up with the scheduled Gynecology appointment. While there are many barriers to utilizing the PED for contraception initiation, this study suggests that providing contraceptive counseling and facilitation for a contraception initiation appointment may overcome those barriers and be beneficial in pregnancy prevention for many adolescents. Further research is needed to determine methods to increase contraception use among the high risk PED population in a real world clinical setting.
Acknowledgments
Funding Source: Internal funding source: Cincinnati Children’s Hospital Medical Center, Division of Emergency Medicine, Small Grant Award. Amount: $5,000. No external funding for this manuscript.
Dr. Chernick was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number KLSTR001874. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Prior Presentation: The work described in this manuscript was presented at Pediatric Academic Society meeting, San Francisco, CA in May, 2017.
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest relevant to this article to disclose.
REFERENCES
- 1.Kost K, Arpaia A. Pregnancies, Births, and Abortions Among Adolescents and Yound Women in the United States, 2013: National and State Trends by Age, Race, and Ethnicity New York: Guttmacher Institute; 2017. [Google Scholar]
- 2.Sedgh G, Finer LB, Bankole A, Eilers MA, Singh S. Adolescent pregnancy, birth, and abortion rates across countries: levels and recent trends. J Adolesc Health 2015;56:223–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen XK, Wen SW, Fleming N, Demissie K, Rhoads GG, Walker M. Teenage pregnancy and adverse birth outcomes: a large population based retrospective cohort study. Int J Epidemiol 2007;36:368–73. [DOI] [PubMed] [Google Scholar]
- 4.Hoffman S, Maynard R. Kids Having Kids: Economic Costs and Social Consequences of Teen Pregnancy Second ed: The Urban Institute Press; 2008. [Google Scholar]
- 5.Kay K, Gootman J, Ng AS & Finley C (2014. )The benfits of Birth control in America; Getting the Facts Straight Washington, DC: Power to Decide; https://powertodecide.org/what-we-do/information/resource-library/benefits-of-birth-control-in-america. [accessed 12/2017] [Google Scholar]
- 6.Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008–2011. N Engl J Med 2016;374:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Committee on Adolescent Health Care Long-Acting Reversible Contraception Working Group Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol 2012;120:983–8. [DOI] [PubMed] [Google Scholar]
- 8.Romero L, Pazol K, Warner L, et al. Vital Signs: Trends in Use of Long-Acting Reversible Contraception Among Teens Aged 15–19 Years Seeking Contraceptive Services - United States, 2005–2013. Mmwr-Morbidity and Mortality Weekly Report 2015;64:363–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Abma JC, Martinez GM. Sexual Activity and Contraceptive Use Among Teenagers in the United States, 2011–2015. Natl Health Stat Report 2017:1–23. [PubMed]
- 10.Secura GM, Madden T, McNicholas C, et al. Provision of No-Cost, Long-Acting Contraception and Teenage Pregnancy. N Engl J Med 2014;371:1316–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller MK, Pickett M, Leisner K, Sherman AK, Humiston SG. Sexual Health Behaviors, Preferences for Care, and Use of Health Services Among Adolescents in Pediatric Emergency Departments. Pediatr Emerg Care 2013;29:907–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chernick L, Kharbanda EO, Santelli J, Dayan P. Identifying adolescent females at high risk of pregnancy in a pediatric emergency department. J Adolesc Health 2012;51:171–8. [DOI] [PubMed] [Google Scholar]
- 13.Todd CS, Mountvarner G, Lichenstein FI. Unintended pregnancy risk in an emergency department population. Contraception 2005;71:35–9. [DOI] [PubMed] [Google Scholar]
- 14.Chernick L, Schnall R, Higgins T, et al. Barriers to and enablers of contraceptive use among adolescent females and their interest in an emergency department based intervention. Contraception 2015;91:217–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Solomon M, Badolato GM, Chernick LS, Trent ME, Chamberlain JM, Goyal MK. Examining the Role of the Pediatric Emergency Department in Reducing Unintended Adolescent Pregnancy. J Pediatr 2017;189:196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chernick LS, Westhoff C, Ray M, et al. Enhancing referral of sexually active adolescent females from the emergency department to family planning. J Womens Health (Larchmt) 2015;24:324–8. [DOI] [PubMed] [Google Scholar]
- 17.Reed J, Thistlethwaite J, Huppert J. STI research: Recruiting an unbiased sample. Journal of Adolescent Health 2007;41:14–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madden T, Mullersman J, Omvig K, Secura G, Peipert J. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception 2013;88:243–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.LARC First : Contraceptive Counseling, http://www.larcfirst.com/counseling.html [accessed 01/2015]
- 20.Brener ND, Kann L, Shanklin S, et al. Methodology of the Youth Risk Behavior Surveillance System−−2013. MMWR Recomm Rep 2013;62:1–20. [PubMed] [Google Scholar]
- 21.Miller MK, Champassak S, Goggin K, et al. Brief Behavioral Intervention to Improve Adolescent Sexual Health: A Feasibility Study in the Emergency Department. Pediatr Emerg Care 2016;32:17–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR Recomm Rep 2016;65:1–66. [DOI] [PubMed] [Google Scholar]
- 23.Miller MK, Randell KA, Barral R, Sherman AK, Miller E. Factors Associated With Interest in Same-Day Contraception Initiation Among Females in the Pediatric Emergency Department. J Adolesc Health 2016;58:154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Widman L, Choukas-Bradley S, Noar SM, Nesi J, Garrett K. Parent-Adolescent Sexual Communication and Adolescent Safer Sex Behavior: A Meta-Analysis. JAMA Pediatr 2016;170:52–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eisenberg D, McNicholas C, Peipert JF. Cost as a barrier to long-acting reversible contraceptive (LARC) use in adolescents. J Adolesc Health 2013;52:S59–63. [DOI] [PubMed] [Google Scholar]
- 26.Bernstein J, Dorfman D, Lunstead J, et al. Reaching Adolescents for Prevention: The Role of Pediatric Emergency Department Health Promotion Advocates. Pediatr Emerg Care 2017;33:223–9. [DOI] [PubMed] [Google Scholar]


