Abstract
Massive irreparable rotator cuff tears in the younger, active patient can be one of the most challenging pathologies to treat in shoulder surgery. Over the last few years, the superior capsular reconstruction (SCR) technique, which has shown favorable initial clinical results, has emerged as a promising new technique that aims to restore glenohumeral mechanics and improve patient function. SCR can be technically challenging, and improvements have been made consistently to the technique. In this Technical Note, we present our knotless technique of glenoid fixation using push-in anchors and suture tapes. We believe that our procedure offers an improvement to current SCR techniques.
Treatment options for young, active patients with massive, retracted rotator cuff tears have historically been considered unpredictable and fraught with high failure rates because of tendon inelasticity and the poor tissue quality typically present in these retracted tears.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 In 2013, Mihata et al.15 described the arthroscopic superior capsular reconstruction (SCR) as a successful procedure treating massive, irreparable rotator cuff tears. In a subsequent report of clinical outcomes, Mihata et al.15 reported excellent results using a fascia lata autograft to arthroscopically reconstruct the superior capsule with significant improvements in pain, function, and range of motion in forward flexion and abduction. As this procedure has evolved, a technique of arthroscopic SCR with acellular dermal allograft has been developed as an improvement to their original technique.4, 5 In this article, we present our knotless technique of glenoid fixation using push-in anchors and suture tapes to secure the dermal allograft to the superior glenoid. We employ this technique because of its knotless construction, efficient facilitation of graft advancement into the joint with minimal suture management issues, theoretically superior biomechanical strength of tape versus suture fixation of graft,16 and the excellent fixation anchor placement into subchondral glenoid bone.
Technique Description
We perform all of these cases in the lateral decubitus position with general anesthesia and a single-shot interscalene block or single-shot block with an indwelling pain catheter (Video 1). The shoulder is examined to assess range of motion and stability and then the patient is placed in the lateral decubitus position with the arm positioned in 45° of abduction, 10° of forward flexion, and neutral rotation. A posterior glenohumeral viewing portal is created along with an anterior outflow/working portal and diagnostic arthroscopy is performed. Any intra-articular pathology is assessed and addressed appropriately. The arthroscope is then reconfigured into the subacromial space and a midlateral portal is created. Specific attention is given to the rotator cuff as it is assessed for degree of retraction, mobility, tissue quality, and atrophy. The rotator cuff is determined to be irreparable when residual rotator cuff tissue is completely mobilized through release techniques and attempts in multiple vectors to reapproximate the torn rotator cuff to the native footprint is not possible. The biceps tendon in all of our SCR procedures has been treated with biceps tenotomy and the superior labrum debrided to expose and create a bleeding bed of bone on the superior glenoid to facilitate graft healing onto the glenoid. We perform this technique with 4 portals: the midlateral portal, anterior, posterior, and juxta-acromial working portals. These are the same portals we use for performing a standard rotator cuff repair. The juxta-acromial portal is able to be used for glenoid fixation, and humeral fixation is used for graft introduction to the joint as well (Table 1). The midlateral portal is typically used as our viewing portal. The juxta-acromial portal is placed to facilitate appropriate anchor placement in the superior glenoid rim and anchor placement onto the proximal humerus for standard arthroscopic transosseous equivalent double-row fixation technique of the graft to the humerus.15 This portal is similar to a standard rotator cuff repair portal that is used for anchor placement and is accomplished using a spinal needle to assist with visualization. A flexible large-diameter cannula (Passport; Arthrex, Naples, FL) is placed in the juxta-acromial portal for graft advancement and glenoid and humeral fixation, large twist-in threaded cannulas (8.25 mm × 7 cm; Arthrex) are placed in the posterior portal, and a standard or large-threaded cannula is placed in the anterior portal to be used as working portals (Fig 1).
Table 1.
Pearls and Pitfalls of the Arthroscopic Superior Capsular Reconstruction Technique
| Pearls | Pitfalls |
|---|---|
|
|
Fig 1.
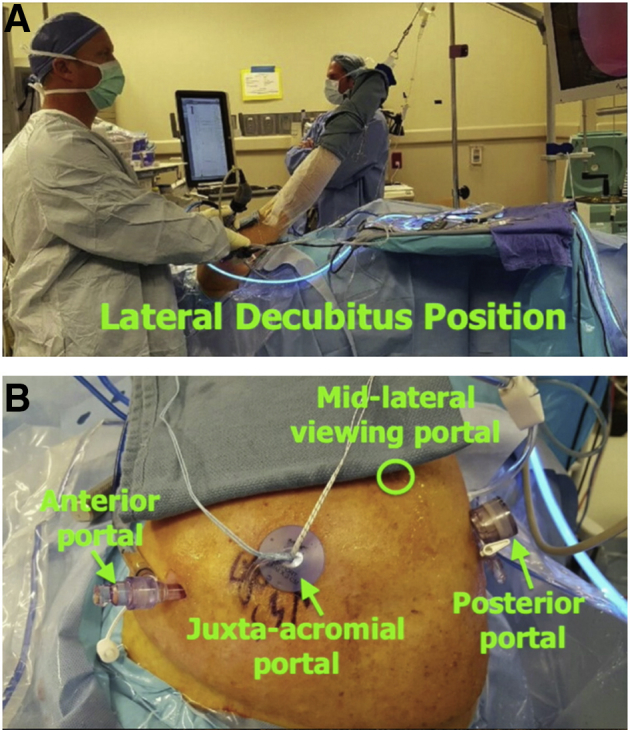
Right shoulder in a patient in the lateral decubitus position (A). Four portals are used. The arthroscope (beneath towel) is placed through a midlateral viewing portal. An 8.25 × 7–cm threaded cannula is typically placed in the posterior working portal. The juxta-acromial portal is typically placed just anterior to the anterolateral edge of the acromion and a flexible large-diameter cannula is placed in this portal. This portal is used for graft advancement as well as graft fixation onto the glenoid and humerus. The anterior portal is an additional working portal, and typically a smaller-diameter smooth clear cannula is used; however, a larger-diameter threaded cannula can be used as well. The anterior and posterior portals are mainly used for suture management and for side-to-side closure of the graft to remaining rotator cuff tissue anteriorly and posteriorly to ensure appropriate graft tensioning and facilitate force couple restoration. A surgical towel is typically placed on the arm of the patient distal to the working portals to diminish contact of the allograft with the patient's skin, thereby theoretically decreasing the infection risk for propagation of skin flora to the graft prior to implantation. Portal configuration is shown (B).
The undersurface of the acromion and the coracoacromial ligament is assessed for evidence of impingement. Any evidence of abrasion on the undersurface of the acromion is addressed with an arch-sparing/gentle subacromial smoothing procedure. The acromioclavicular joint is assessed, and if required (acromioclavicular joint tenderness), a distal clavicle excision is performed.
Our surgical technique for arthroscopic superior reconstruction largely mimics the technique described by Hirohara and Adams4 with modification to the glenoid fixation technique and graft passage. Our technique favors an advancement technique rather than double pulley used by Hirohara and Adams4 After abrasion of the superior glenoid rim and the footprint of the greater tuberosity of the humerus, drill holes are placed in the superior glenoid rim in preparation for graft fixation (Fig 2). The 2 medial row anchors (biocomposite, 4.75×19.1 mm; Arthrex) on the humerus are placed with associated suture tapes. Graft dimensions are obtained medially on the superior glenoid rim, laterally on the humeral footprint between remnant rotator cuff tissue, and anteriorly and posteriorly between the superior glenoid and the humerus.
Fig 2.
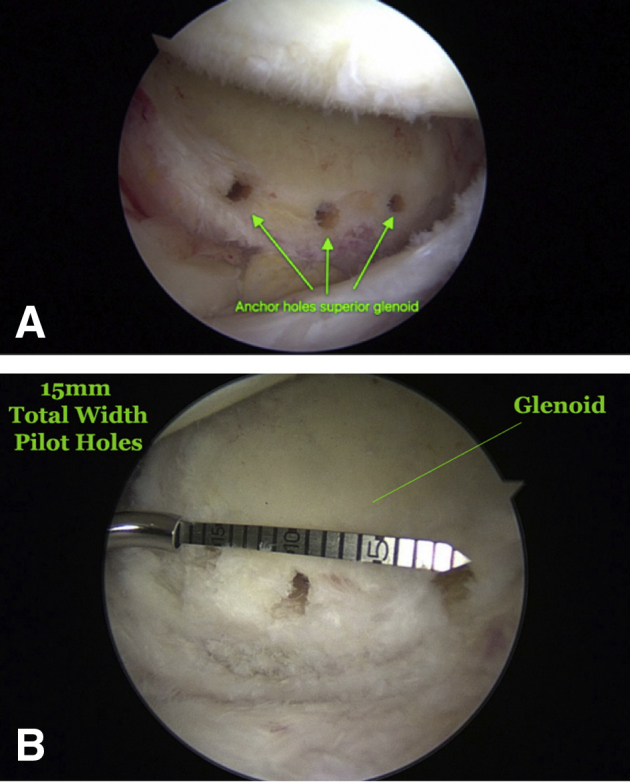
Arthroscopic view of the right shoulder in the lateral decubitus position from the midlateral viewing portal. The glenoid is at the bottom of the image and the humerus on top. The anterior side is to the right and the posterior to the left. Placement of three 2.9-mm drill holes in the superior glenoid is shown (A). These are predrilled during joint preparation for eventual use in graft fixation with push-in anchors. The anchor holes are placed along the articular margin of the superior glenoid in a similar fashion as used in labral repair. Initially, the measurement between the most anterior and the most posterior pilot holes is noted. In our patients, 15 mm, as shown, is the most common width (B).
A 3.0-mm (2.75-3.25-mm)-thick acellular dermal allograft (Lifenet, Virginia Beach, VA) is prepared using the dimensions obtained. Three suture tapes to be used for glenoid fixation are placed in the medial aspect of the graft. We mark the middle suture tape with a surgical marker at the graft–suture tape interface as well as at the free ends to facilitate identification during graft advancement and fixation (Fig 3). Two holes of sufficient diameter are drilled in the lateral aspect of the graft to allow passage of the medial row suture tapes that are in the rotator cuff anchors.
Fig 3.
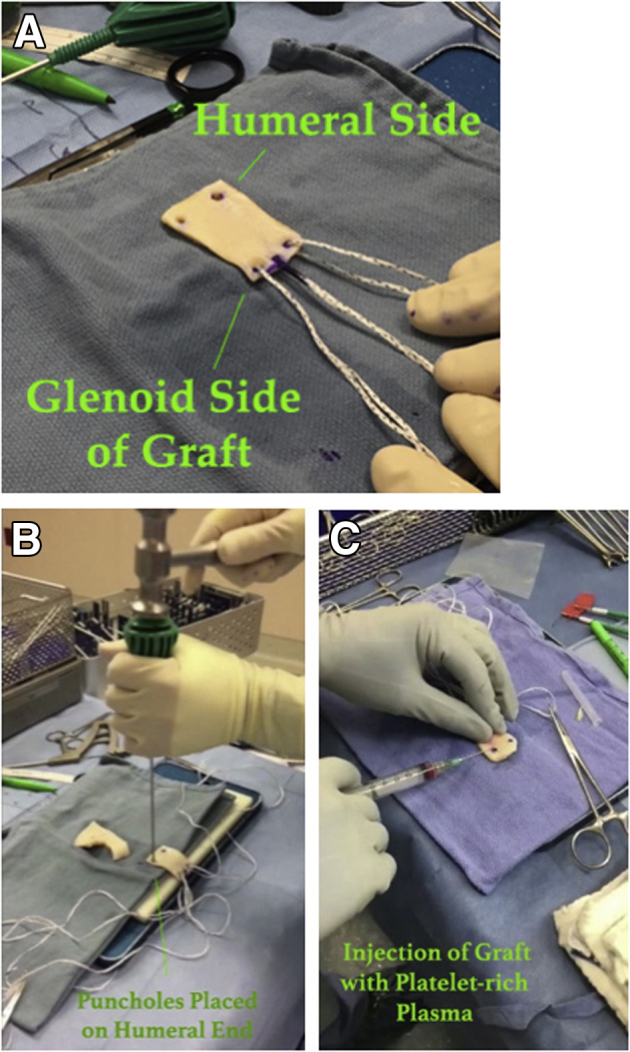
The acellular dermal allograft is prepared. In our technique, 3 separate tape sutures, which align with the 15-mm-wide intraoperative pilot holes, are shuttled through the glenoid side of the graft. The middle suture is marked with a sterile marking pen at both the graft end and the free end to more easily identify sutures during graft introduction (A). Two punch holes are placed on the humeral end to accommodate the humeral-side sutures (B). This facilitates future humeral fixation. The graft is also injected with platelet-rich plasma to theoretically improve healing (C).
Glenoid fixation modification in our technique uses a push-in anchor technique (biocomposite, 2.9×12.5 mm; Arthrex) that allows us to use the anchor suture tape–graft interface to push the graft in through the juxta-acromial portal and securely fix the graft onto the glenoid adjacent to the articular margin immediately medial to the superior articular surface of the glenoid. In our technique, this fixation is favored over the double-pulley technique because of ease of graft advancement using the anchor to advance the graft, as well as the fixation provided by the anchor being placed in the typically strong subchondral bone of the glenoid immediately adjacent to the superior glenoid rim (Table 2). This technique is also knotless, providing strong, smooth fixation of the medial aspect of the graft. Typically, we advance the graft through the juxta-acromial portal with the suture tape and anchor of the posterior superior glenoid fixation site, followed by fixation of the graft to the middle anchor of the superior glenoid, and last the anterosuperior glenoid anchor (Fig 4). In all cases that we have performed, we have used 3 push-in anchors on the glenoid. After this step, the humeral side of the graft is fixed using the suture tapes in the 2 medial-row anchors that the graft was passed over through the lateral holes placed in the graft and an additional 2 screw-in anchors (biocomposite, 4.75×19.1 mm; Arthrex) laterally to the greater tuberosity of the humerus as described in previous techniques (Fig 5). This is analogous to the arthroscopic double-row transosseous equivalent technique described by Park et al.14 Typically, 2 margin sutures were placed suturing the posterior aspect of the graft to the intact posterior rotator cuff musculature in addition to a single margin suture between the anterior aspect of the graft and the superior margin of the intact subscapularis tendon to provide appropriate graft tension. Postoperatively we treat all of these patients with a similar rehabilitation protocol with which we treat our rotator cuff repairs. This includes sling immobilization for comfort with passive range of motion for 4 weeks. Active assisted motion is commenced at 4 weeks with progression to active motion by 8 weeks postoperatively.
Table 2.
Advantages and Disadvantages of the Arthroscopic Superior Capsular Reconstruction Technique
| Advantages | Disadvantages |
|---|---|
|
|
Fig 4.
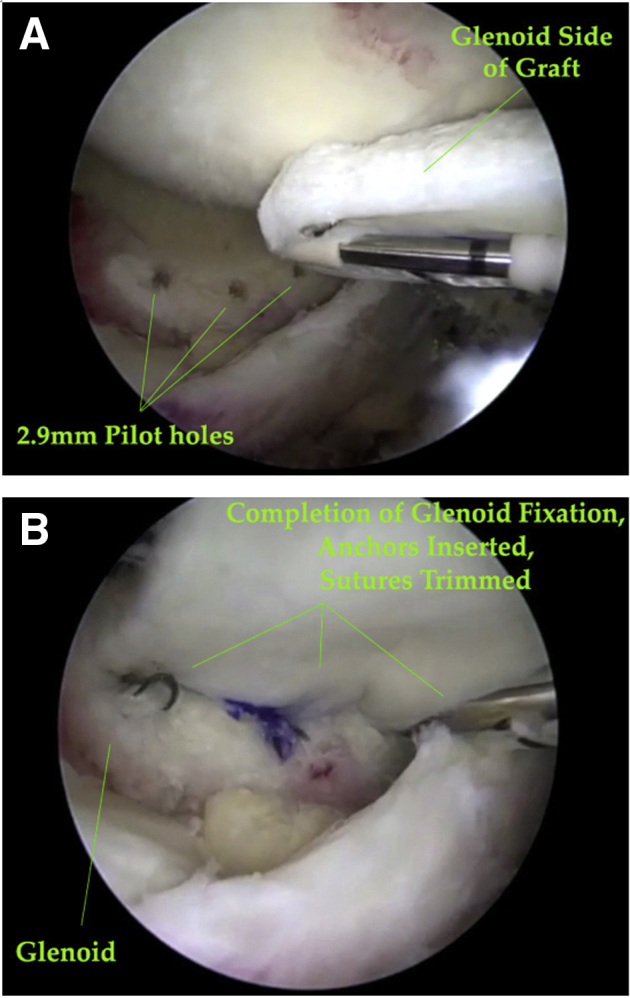
Insertion of the acellular dermal allograft into the pilot holes drilled into the superior glenoid (A). Back tension is held on all remaining sutures during advancement to avoid them getting intertwined. The posterior anchor is inserted and then pounded into place; next, the trailing suture is trimmed. This process is repeated initially for the middle anchor and then the most anterior one. Once all anchors have been inserted into the pilot holes and the trailing suture trimmed, the glenoid fixation is complete (B).
Fig 5.
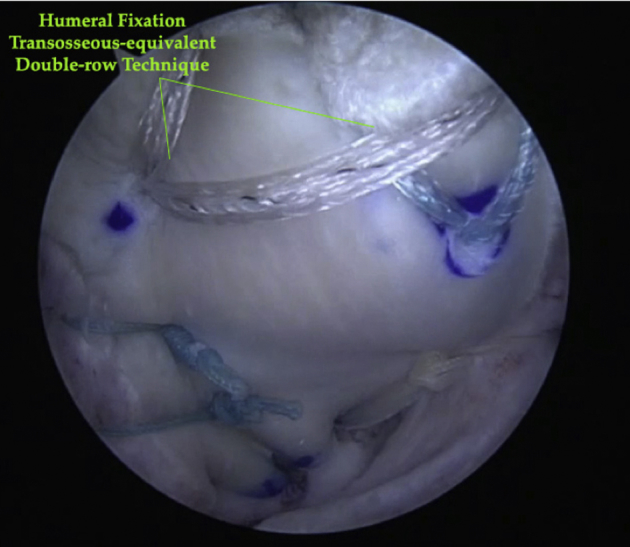
In continuing on to the humeral fixation, a transosseous-equivalent double-row technique is performed. The figure shows our humeral fixation, with side-to-side suture tapes placed between the graft and the anterior and posterior ends of the remaining rotator cuff. We typically use 2 margin sutures to suture the posterior aspect of the graft to the intact posterior remaining rotator cuff, and a single margin suture between the anterior aspect of the graft to the superior margin of the intact subscapularis tendon. This provides the appropriate amount of graft tension.
Discussion
Arthroscopic superior capsular reconstruction has gained momentum as a tool in the shoulder surgeon's armamentarium to treat this problematic patient population. Clinical outcome analyses have now consistently shown promising early results.15, 17, 18, 19 Our series of short-term results currently accepted for publication in Arthroscopy reporting 1-year follow-up on 88 shoulders and 2-year follow-up on 38 shoulders has also revealed similar favorable clinical outcomes employing this procedure with our technique of glenoid fixation.19
The majority of the risks associated with our glenoid fixation technique are inherent to the more commonly used techniques. Theoretically, there is an increased potential risk of glenoid bone stock injury because we use 3 points of anchor fixation. Considering that this is the case, a primary limitation of this technique would be poor fixation or failure of fixation in patients who have pre-existing or iatrogenic poor superior glenoid bone stock.
We present this technique of glenoid fixation of the acellular dermal allograft in superior capsular reconstruction as an efficient, secure, knotless technique that in our hands has been successfully employed in 192 procedures since February 5, 2015, using acellular dermal allografts to perform superior capsular reconstruction to restore superior capsular stability in irreparable atrophic rotator cuff tears as well as in augmentation procedures to restore superior stability in massive rotator cuff repairs when superior capsular repair was not possible with excellent results. We have not noted any cases of failure of fixation on the glenoid side on follow-up imaging in cases where advanced imaging has been performed (magnetic resonance imaging or ultrasonography, n = 45). We believe that this technique is an alternative method of fixation that is efficient, reproducible, and secure in providing glenoid fixation of the acellular dermal allograft to the glenoid in arthroscopic superior capsular reconstruction.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: W.T.P. reports personal fees from Arthrex, other from Midwest Orthopedic Specialty Hospital, other from the Surgery Center at Associated Medical and Surgical Specialists, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This is a video on the athroscopic superior capsular reconstruction using the acellular dermal allograft and push-in anchors for glenoid fixation. The video is taken on a right shoulder patient in the lateral decubitus position. Four portals are utilized - the mid-lateral viewing portal (from which the video is recorded), the posterior and anterior working portals for suture management, and the juxta-acromial portal. The juxta-acromial portal is used for eventual graft advancement and fixation of the graft to the glenoid and the proximal humerus. The video shows our procedure in a stepwise process, clearly describing our technique.
References
- 1.Le B.T., Wu X.L., Lam P.H., Murrell G.A. Factors predicting rotator cuff tears: An analysis of 1000 consecutive shoulders. Am J Sports Med. 2014;42:1134–1142. doi: 10.1177/0363546514525336. [DOI] [PubMed] [Google Scholar]
- 2.Mihata T., McGarry M., Pirolo J., Kinoshita M., Lee T. Superior capsular reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 3.Adams C.R., Denard P.J., Brady P.C., Hartzler R.U., Burkhart S.S. The arthroscopic superior capsular reconstruction. Am J Orthop. 2016;45:320–324. [PubMed] [Google Scholar]
- 4.Hirohara A.M., Adams C.R. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthroscopy Techniques. 2015;4:e637–e641. doi: 10.1016/j.eats.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerber C., Rahm S.A., Cantanzaro S., Farshad M., Moor B. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: Long-term follow-up of ten years. J Bone Joint Surg Am. 2013;95:1920–1926. doi: 10.2106/JBJS.M.00122. [DOI] [PubMed] [Google Scholar]
- 6.El-Azab H.M., Rott O., Irlenbusch U. Long term follow-up after latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J Bone Joint Surg Am. 2015;97:462–469. doi: 10.2106/JBJS.M.00235. [DOI] [PubMed] [Google Scholar]
- 7.Hanseler J.F., Nagels J., Van der Zwall P., Nelissen R.G. Teres major tendon transfer for patients with massive irreparable posterosuperior rotator cuff tears: Short term clinical results. J Bone Joint Surg Am. 2013;95:523–529. doi: 10.1302/0301-620X.95B4.30390. [DOI] [PubMed] [Google Scholar]
- 8.Kanatli U., Ozer M., Ataoglu M.B. Arthroscopic assisted latissimus dorsi tendon transfer for massive, irreparable rotator cuff tears: Technique and short-term follow-up of patients with pseuodoparalyis. Arthroscopy. 2017;33:929–937. doi: 10.1016/j.arthro.2016.09.023. [DOI] [PubMed] [Google Scholar]
- 9.Barber F.A., Burns J.P., Deutsch A., Labbe M.R., Litchfield R.B. A prospective randomized evaluation of acellular dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy. 2012;28:8–15. doi: 10.1016/j.arthro.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 10.Jones C.R., Snyder S.J. Massive irreparable rotator cuff tears: A solution that bridges the gap. Sports Med Arthroscopy. 2015;23:130–138. doi: 10.1097/JSA.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 11.Bond J.L., Dopirak R.M., Higgins J., Burns J., Snyder S.J. Arthroscopic replacement of massive, irreparable rotator cuff tears using a graft jacket allograft: Technique and preliminary results. Arthroscopy. 2008;24:403–409.e1. doi: 10.1016/j.arthro.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 12.Gupta A.K., Hug K., Boggess B., Gavigan M., Toth A.P. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: Clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med. 2013;41:872–879. doi: 10.1177/0363546512475204. [DOI] [PubMed] [Google Scholar]
- 13.Boileau P., Baque F., Valerio L., Ahrens P., Chuinard C., Trojani C. Isolated arthroscopic biceps tenotomy of tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 14.Park M.C., Elattreche N.S., Ahmad C.S., Tibone J.E. “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy. 2006;22:1360.e1–1360.e5. doi: 10.1016/j.arthro.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Liu R., Lam P.H., Shepherd H., Murrell G.A. Tape versus suture—A biomechanical and clinical analysis in arthroscopic rotator cuff repair of large tears. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117701212. 2325967117701212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirahara A.M., Anderson W.J., Panero A.J. Superior capsular reconstruction: Clinical outcomes after minimum 2-year follow-up. Am J Orthop. 2017;46:266–278. [PubMed] [Google Scholar]
- 18.Denard P.J., Brady P.C., Adams C.R., Tokish J.M., Burkhart S.S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 19.Pennington W.T., Bartz B.A., Pauli J.M., Walker C., Schmidt W. Arthroscopic superior capsular reconstruction with acellular dermal allograft for the treatment of massive irreparable rotator cuff tears: Short-term clinical outcomes and the radiographic parameter of superior capsular distance. Arthroscopy. 2018;34:1764–1773. doi: 10.1016/j.arthro.2018.01.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This is a video on the athroscopic superior capsular reconstruction using the acellular dermal allograft and push-in anchors for glenoid fixation. The video is taken on a right shoulder patient in the lateral decubitus position. Four portals are utilized - the mid-lateral viewing portal (from which the video is recorded), the posterior and anterior working portals for suture management, and the juxta-acromial portal. The juxta-acromial portal is used for eventual graft advancement and fixation of the graft to the glenoid and the proximal humerus. The video shows our procedure in a stepwise process, clearly describing our technique.


