Abstract
There has been a renewed interest in anterior cruciate ligament (ACL) repairs over the last decade with some early promising results in the right patient population. Additionally, the anterolateral ligament has been extensively studied and has recently been shown to have a protective effect on standard ACL reconstructions in a clinical trial. Given its protective effect on ACL reconstructions, we believe this phenomenon is also relevant to ACL repairs and can decrease rerupture rates. In this publication, we demonstrate a surgical technique for ACL repair using an internal brace combined with an anterolateral ligament reconstruction using a gracilis autograft.
Open primary repairs of anterior cruciate ligament (ACL) ruptures were historically abandoned due to poor functional outcomes, high rates of revision surgery, persistent instability, low rates of return to activities, and comparative studies demonstrating superior results of ACL reconstruction.1, 2, 3 The published outcomes of open ACL repair may be attributed to the morbidity of the arthrotomy, the prolonged immobilization, the imprecise indications, and the failure to comprehensively address the secondary restraint lesions that are better recognized nowadays.1, 4
Since 2008, the orthopaedic literature has shown a renewed interest in ACL repair with an emphasis on biologic process and arthroscopic procedure, rather than an open approach.3, 4, 5 DiFelice et al.4 reported promising clinical results in 10 patients with a 5-year minimum follow-up after arthroscopic primary ACL repair (9% rerupture rate, no patients with grade II/III pivot shift, and mean Lysholm score of 96). Clinical outcomes might be further improved by the use of 2 emerging concepts: a biological adjunct of a collagen-based scaffold into the notch to improve the healing potential of the ACL repair and the placement of an internal brace, which is reported to biomechanically protect the ligament during the healing phase.2, 6, 7, 8
Ferretti et al.9 demonstrated that concomitant injury to the anterolateral structures occurs in up to 90% of acute ACL-injured knees. Results may also be improved by the addition of a lateral extra-articular procedure. Sgaglione et al.10 reported good subjective, and excellent functional and objective, results in active patients who were followed for more than 3 years using the concept of “double braces” in the setting of an ACL repair. This series is the first to describe the ACL repair augmentation using a bundle of semitendinosus as an internal brace and a strip of iliotibial band as a lateral sling or “external brace.” Resurrecting this forgotten concept by using a modern device, this article describes a reemerging surgical technique for combined ACL repair and anterolateral ligament (ALL) reconstruction (Video 1).
Surgical Technique
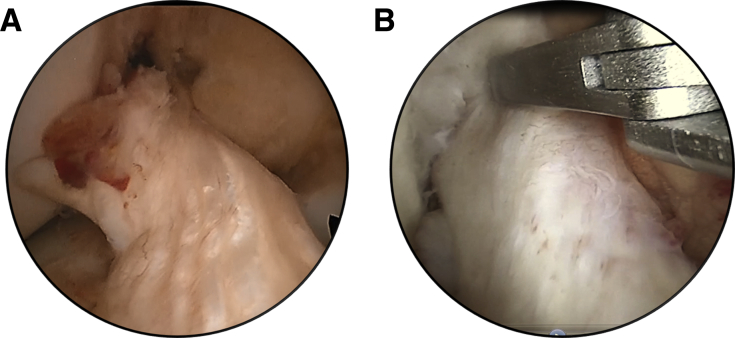
The patient is placed on an operating table in the standard arthroscopy position. After establishing high anterolateral and anteromedial portals, the feasibility of repair is determined by confirming a proximal avulsion and the quality of the remnant (Fig 1).
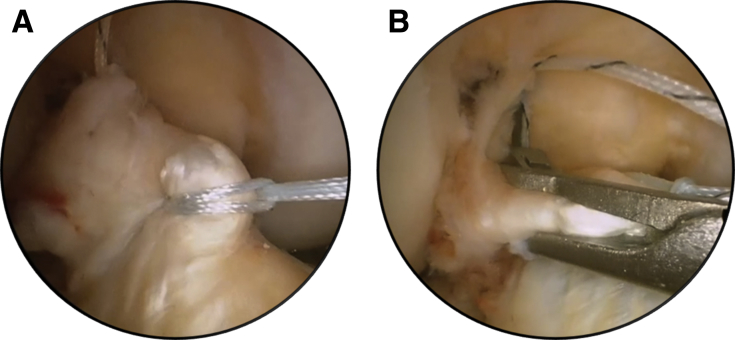
Fig 1.
Right knee. (A) Proximal rupture of the anterior cruciate ligament; (B) reapproximation of the anterior cruciate ligament remnant onto its femoral insertion is checked with an arthroscopic grasper.
ALL Tibial Tunnel Drilling
Two 4.5 × 15 mm sockets are drilled in the tibia through stab incisions placed just posterior to Gerdy's tubercle and just anterior to the fibula head, 1 cm distal to the joint line.11 These are converged into a single tunnel using a right-angled clamp. A suture (no. 2 Ethibond; Ethicon, Somerville, NJ) is then passed through the tunnel to create a loop for graft passage.
Graft Harvest and Preparation
Gracilis autograft is harvested (Pigtail Hamstring Tendon Stripper; Arthrex, Naples, FL) through a vertical incision located 1 cm medial to the tibial tuberosity. Both ends of the tendon are whipstitched using a FiberLoop suture (Arthrex).
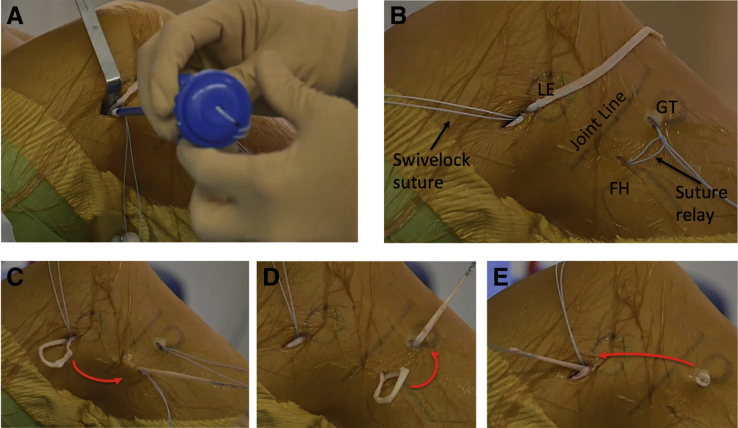
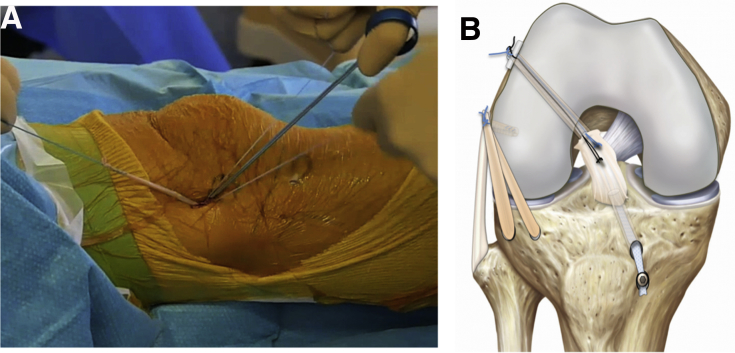
Femoral Fixation and Passage of the ALL Graft Through the Tibial Tunnel
With the knee positioned at 90° of flexion, a 2 cm incision is made, slightly posterior and proximal to the lateral epicondyle. A 4.5 × 20 mm socket is drilled through the origin of the proximal insertion of the ALL where one end of the graft is secured with a 4.75 mm SwiveLock anchor (Arthrex). The other end of the graft is shuttled deep to the iliotibial band, through the tibial tunnel, and then back again deep to the iliotibial band to the proximal incision where it will be subsequently fixed11 (Fig 2, Fig 3).
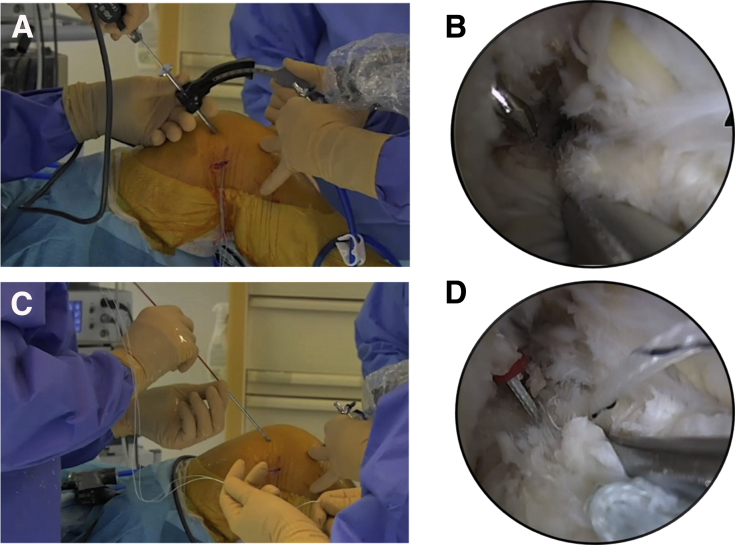
Fig 2.
Right knee. (A) Femoral fixation of one end of the gracilis with the SwiveLock anchor device. (B) One end of the gracilis is fixed in the femoral socket positioned posterior and proximal to the lateral epicondyle, and a loop of suture relay is placed through the 2 convergent transosseous tunnels positioned just below the joint line, between Gerdy's tubercle and the fibular head. (C) The free end of the gracilis is routed from the femur to the tibia deep to the iliotibial band, (D) through the tibial transosseous tunnel using the suture relay, and (E) back to the femoral incision deep to the iliotibial band. (FH, fibular head; GT, Gerdy's tubercle; LE, lateral epicondyle.)
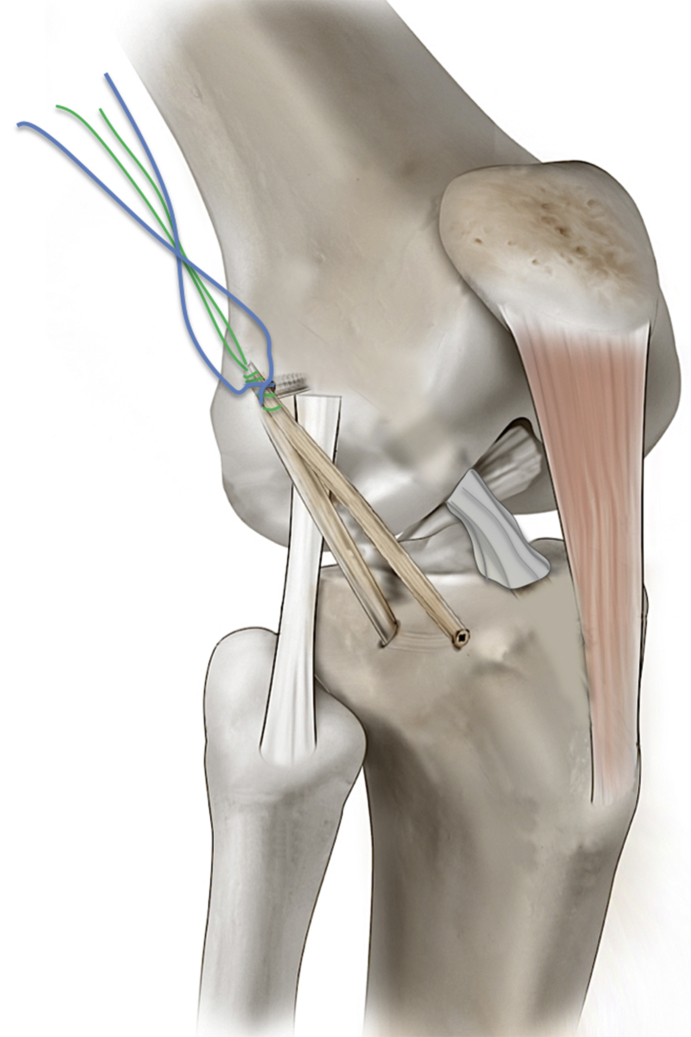
Fig 3.
Anterolateral ligament reconstruction. The free end of the gracilis will be knotted on to the femoral socket using the SwiveLock anchor suture at the end of the procedure.
Drilling of Tibial ACL Tunnel and ACL Remnant Suture
A 4 mm tibial tunnel is drilled in an ACL remnant sparing manner.12 After removal of the reamer, the guide wire is reintroduced and pushed into the remnant to emerge at its proximal end so that a path is created for suture passage. A FiberStick (Arthrex), is placed through the tibial tunnel, and the remnant and then retrieved through the anteromedial portal (Fig 4). The plastic tube is left in position to help avoid inadvertent closure of the central passage when passing 2 no. 0 FiberLink cinch sutures (Arthrex) through the remnant, at its middle and proximal parts, using the knee scorpion suture passer (Arthrex; Fig 5).
Fig 4.
Right knee. (A) Anterior cruciate ligament (ACL) tibial guide is used to position a guide pin in the center of the ACL tibial stump with the knee positioned in slight flexion. (B) Intra-articular view of ACL tibial guide positioned onto the ACL stump. (C) After drilling the tibial tunnel with a 4 mm drill, the guide pin is switched with a FiberStick. (D) The FiberStick is then retrieved with an arthroscopic suture grasper.
Fig 5.
Right knee. (A) FiberLink cinch suture at the middle part of the anterior cruciate ligament stump. (B) Placement of the proximal TigerLink cinch suture with the knee scorpion suture passer.
Drilling of the Femoral ACL Tunnel
The arthroscope is placed in the lateral gutter, and the optimal entrance point for the femoral tunnel is localized with a needle.12 The outside-in femoral guide (Arthrex) is inserted at this location and positioned at the footprint of the ACL. A 4 mm tunnel is created. A FiberStick and a TigerStick are introduced into the knee through the cannulated reamer, and one suture end from each is then retrieved from the anteromedial portal (Fig 6).
Fig 6.
Right knee. (A) Outside-in femoral guide. The femoral tunnel at the level of lateral gutter is a safe distance from the femoral socket of the anterolateral ligament reconstruction. (B) Intra-articular view of the femoral guide pin. (C) A FiberStick and a TigerStick suture are introduced in the 4 mm diameter femoral tunnel; (D) the 2 sutures are then retrieved with the arthroscopic grasper through the anteromedial portal.
Placing the Internal Brace Suture and Deploying Femoral Cortical Button
The TigerStick is linked to the FiberStick that was previously placed within the center of the ACL remnant. The latter is retrieved through the tibial tunnel, resulting in a single TigerStick passing from the tibia to the femur that will be used to shuttle the internal brace suture.
A FiberTape (Arthrex) is loaded on a TightRope button (Arthrex). The button is attached to the shuttle suture and passed through the tibial and femoral tunnels. Under arthroscopic visualization in the lateral gutter, the TightRope button is flipped onto the femoral cortex (Fig 7).
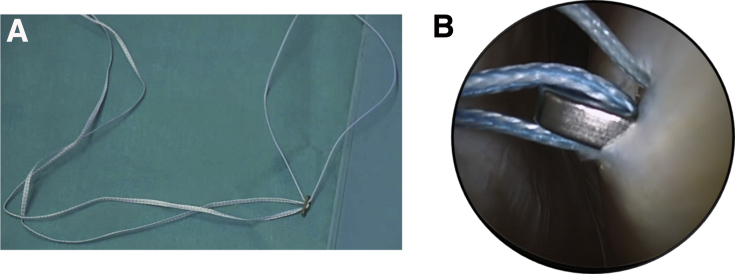
Fig 7.
(A) FiberTape loaded on the TightRope button. (B) Visualization of the button emerging from the femoral tunnel in the lateral gutter.
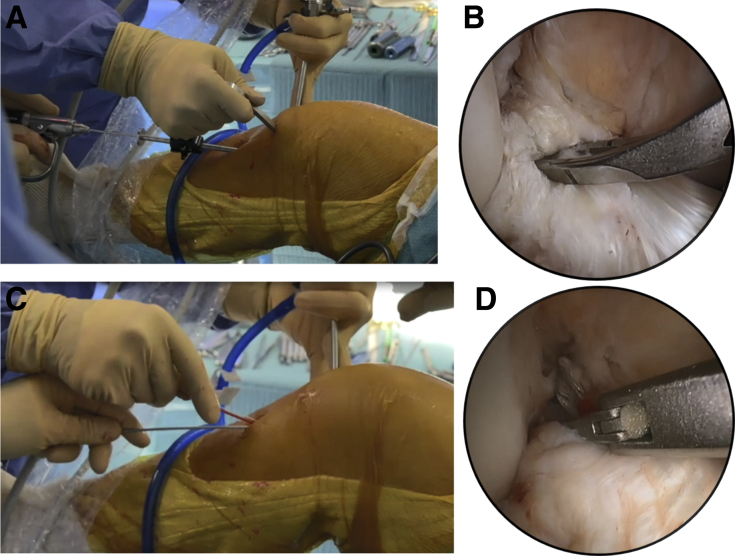
Passing and Securing the ACL Remnant Sutures
Before fixing the internal brace on the tibial side, the 2 cinch sutures placed within the ACL remnant are retrieved on the femoral side using the FiberStick that was previously passed through the femoral tunnel. The sutures are tied and secured over the TightRope button with the knee at 90° of flexion. The knee is then placed in full extension, and the internal brace is tensioned and fixed on the tibia with a 4.75 mm SwiveLock anchor (Fig 8).
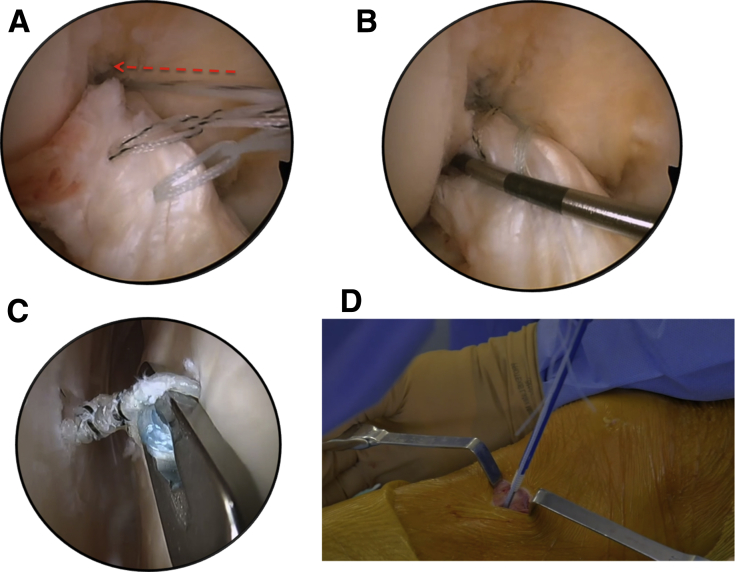
Fig 8.
Right knee. (A) The FiberLink and the TigerLink cinch sutures are pulled through the femoral tunnel. (B) Traction on the cinch sutures at the femoral side pull the anterior cruciate ligament onto its femoral insertion in the notch. (C) The limbs of the FiberLink and TigerLink are then knotted onto the TightRope button in the lateral gutter under arthroscopic control. (D) The FiberTape is tensioned and fixed on the tibia with a SwiveLock anchor with the knee in full extension.
Fixation of ALL Graft
The free end of the ALL graft is secured to the femur using the sutures of the SwiveLock anchor previously used for the first part of ALL graft fixation. This is done with the leg in full extension and neutral rotation. (Fig 9). Pearls and pitfalls of the surgical technique are given in Table 1.
Fig 9.
(A) Fixation of the free end of the anterolateral ligament graft with the knee in full extension; the suture of the SwiveLock anchor is knotted onto the free end of the graft. (B) Illustration of the combined anterior cruciate ligament repair and anterolateral ligament reconstruction.
Table 1.
Steps, Pearls, and Pitfalls of ALL Reconstruction and ACL Repair With Suture Augmentation
| Surgical Step | Pearls | Pitfalls |
|---|---|---|
| ALL tibial tunnel drilling | Use of guide wires allows precise placement and parallel orientation of sockets. | Sockets that are too close together can risk fracturing the bone bridge between them, while sockets too far apart result in difficulty in conversion to a tunnel. |
| Notch debridement | Visualize the femoral insertion without damaging the remnant. | Poor visualization may lead to inappropriate tunnel placement. |
| ACL tibial tunnel | When reaching the articular surface with the drill, slow the drill speed and perforate the cortical bone cautiously. | Lack of attention to drilling can cause iatrogenic injury to the remnant. |
| ACL suture | Keep the plastic red tube of the FiberStick within the remnant when suturing to minimize the risk of blocking the passage of the internal brace. | |
| ACL femoral tunnel | Needle localize the femoral tunnel in the lateral gutter. | If the cortical button is not directly visualized, there is a risk that the sutures placed in the remnant are not secured over it. Furthermore, a more posteriorly placed button risks collision between the ALL femoral socket and the internal brace. |
| Fixation of sutures and graft | ACL sutures are fixed with the knee flexed at 90°. The internal brace and ALL grafts are fixed in full extension. | There is a risk of knee over-constraint if the internal brace is fixed with knee in flexion. The ALL is always fixed in full extension to respect its normal nonisometry and avoid over-constraint. |
ACL, anterior cruciate ligament; ALL, anterolateral ligament.
Postoperative Course
Immediate full weight bearing without a brace and progressive range of motion exercises are allowed. Subsequent progression is milestone based.
Discussion
The main reasons to consider an ACL repair are the healing potential of the ligament and theoretical advantages including reduced morbidity, enhanced early recovery, preservation of nerves and intrinsic cell populations, the native physiology, and some of the complex biomechanical properties of the ligament.2, 7, 13 In addition, repair does not require graft integration and bone tunnels are of small diameter, which has obvious benefits if ACL rerupture occurs and a reconstruction is required. Nevertheless, clinical outcomes reported in the literature after arthroscopic ACL repair are still scarce.2 This technique remains strictly intended for patients with a proximal ACL tear with a good-quality ACL remnant, and it is important to note that there are insufficient data to dismiss historical concerns regarding the rerupture rate (Table 2).
Table 2.
Advantages and Disadvantages of the ALL Reconstruction and ACL Repair With Suture Augmentation
| Advantages | Disadvantages |
|---|---|
| Low donor site morbidity | Only suitable for proximal avulsions of the ACL. |
| Better preservation of the physiological and biomechanical properties of the ACL. | Very few published clinical results. |
| Ease of ACL revision. | |
| Faster recovery than ACL reconstruction. | |
| ACL healing protected by ligament augmentation and anterolateral ligament reconstruction. |
ACL, anterior cruciate ligament.
Although recently published midterm clinical results of arthroscopic ACL repair are promising, it is possible that these can be further improved by application of the “internal brace” suture augmentation concept that has been demonstrated in animal studies to confer improved ligament healing and protect the repair2 and in a long-term clinical study to be associated with a reduced rate of revision surgery.14
Another strategy for protecting the healing ACL repair is the addition of a lateral extra-articular procedure as was recommended by some investigators in the 1980s.2, 15 This seems all the more important today given our recently improved understanding of the anatomy and function of the ALL, and excellent clinical results of ALL reconstruction with respect to reduction in ACL graft rupture rates and improved return to sport.16
In our experience, the potential benefits of augmentation with an internal brace and an ALL reconstruction can be achieved without compromising the early enhanced recovery associated with ACL repair. Since only the gracilis tendon is harvested, donor site morbidity is minimal and the semitendinosus tendon remains available as a future autograft if necessary.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.S. receives support from Arthrex. J.B. receives support from Arthrex. B.S-C. receives support from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates the surgical technique for combined anterior cruciate ligament (ACL) repair and anterolateral ligament (ALL) reconstruction in a right-sided knee. The ALL reconstruction is performed using gracilis tendon autograft. A SwiveLock anchor is used to fix one end of the graft in a socket placed at the femoral origin of the ALL. This is located just posterior and proximal to the lateral epicondyle. The graft is passed under the iliotibial band, and from posterior to anterior, through a tibial tunnel created 1 cm below the joint line. The graft is then routed back under the iliotibial band to the femoral origin where it is fixed with the knee in full extension, after ACL repair has been completed. The ACL repair is performed with an internal brace loaded on a TightRope cortical button. One TigerLink and one Fiberlink cinch suture are placed in the ACL remnant. The limbs of these cinch sutures are passed through the femoral tunnel. Fixation of the internal brace on the tibial side is performed with a SwiveLock anchor, with the knee in full extension. The 2 limbs of the cinch sutures are then tensioned and knotted over the tightrope button. The ALL graft is then tensioned and secured at the femoral origin using a suture from the SwiveLock anchor previously placed in this location. Graft fixation is performed with the knee in full extension and neutral rotation.
References
- 1.Taylor S.A., Khair M.M., Roberts T.R., DiFelice G.S. Primary repair of the anterior cruciate ligament: A systematic review. Arthroscopy. 2015;31:2233–2247. doi: 10.1016/j.arthro.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 2.van Eck C.F., Limpisvasti O., ElAttrache N.S. Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. Am J Sports Med. 2018;46:2291–2298. doi: 10.1177/0363546517717956. [DOI] [PubMed] [Google Scholar]
- 3.Perrone G.S., Proffen B.L., Kiapour A.M., Sieker J.T., Fleming B.C., Murray M.M. Bench-to-bedside: Bridge-enhanced anterior cruciate ligament repair. J Orthop Res. 2017;35:2606–2612. doi: 10.1002/jor.23632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DiFelice G.S., van der List J.P. Clinical outcomes of arthroscopic primary repair of proximal anterior cruciate ligament tears are maintained at midterm follow-up. Arthroscopy. 2018;34:1085–1093. doi: 10.1016/j.arthro.2017.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Achtnich A., Herbst E., Forkel P. Acute proximal anterior cruciate ligament tears: Outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthroscopy. 2016;32:2562–2569. doi: 10.1016/j.arthro.2016.04.031. [DOI] [PubMed] [Google Scholar]
- 6.Murray M.M., Flutie B.M., Kalish L.A. The bridge-enhanced anterior cruciate ligament repair (BEAR) procedure: An early feasibility cohort study. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967116672176. 2325967116672176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Proffen B.L., Sieker J.T., Murray M.M. Bio-enhanced repair of the anterior cruciate ligament. Arthroscopy. 2015;31:990–997. doi: 10.1016/j.arthro.2014.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murray M.M., Martin S.D., Spector M. Migration of cells from human anterior cruciate ligament explants into collagen-glycosaminoglycan scaffolds. J Orthop Res. 2000;18:557–564. doi: 10.1002/jor.1100180407. [DOI] [PubMed] [Google Scholar]
- 9.Ferretti A., Monaco E., Fabbri M., Maestri B., De Carli A. Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament rears. Arthroscopy. 2017;33:147–154. doi: 10.1016/j.arthro.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 10.Sgaglione N.A., Warren R.F., Wickiewicz T.L., Gold D.A., Panariello R.A. Primary repair with semitendinosus tendon augmentation of acute anterior cruciate ligament injuries. Am J Sports Med. 1990;18:64–73. doi: 10.1177/036354659001800111. [DOI] [PubMed] [Google Scholar]
- 11.Sonnery-Cottet B., Daggett M., Helito C.P., Fayard J.M., Thaunat M. Combined anterior cruciate ligament and anterolateral ligament reconstruction. Arthrosc Tech. 2016;5:e1253–e1259. doi: 10.1016/j.eats.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sonnery-Cottet B., Freychet B., Murphy C.G., Pupim B.H., Thaunat M. Anterior cruciate ligament reconstruction and preservation: The single-anteromedial bundle biological augmentation (SAMBBA) technique. Arthrosc Tech. 2014;3:e689–e693. doi: 10.1016/j.eats.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nguyen D.T., Ramwadhdoebe T.H., van der Hart C.P., Blankevoort L., Tak P.P., van Dijk C.N. Intrinsic healing response of the human anterior cruciate ligament: An histological study of reattached ACL remnants. J Orthop Res. 2014;32:296–301. doi: 10.1002/jor.22511. [DOI] [PubMed] [Google Scholar]
- 14.Drogset J.O., Grontvedt T., Robak O.R., Molster A., Viset A.T., Engebretsen L. A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 2006;88:944–952. doi: 10.2106/JBJS.D.02876. [DOI] [PubMed] [Google Scholar]
- 15.Chambat P., Walch G., Deschamps G., Dejour H. [Acute lesions of the anterior cruciate ligament of the knee. Apropos of 71 follow-up cases] Rev Chir Orthop Reparatrice Appar Mot. 1984;70(Suppl 2):152–155. [PubMed] [Google Scholar]
- 16.Sonnery-Cottet B., Saithna A., Cavalier M. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: A prospective comparative study of 502 patients from the SANTI study group. Am J Sports Med. 2017;45:1547–1557. doi: 10.1177/0363546516686057. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the surgical technique for combined anterior cruciate ligament (ACL) repair and anterolateral ligament (ALL) reconstruction in a right-sided knee. The ALL reconstruction is performed using gracilis tendon autograft. A SwiveLock anchor is used to fix one end of the graft in a socket placed at the femoral origin of the ALL. This is located just posterior and proximal to the lateral epicondyle. The graft is passed under the iliotibial band, and from posterior to anterior, through a tibial tunnel created 1 cm below the joint line. The graft is then routed back under the iliotibial band to the femoral origin where it is fixed with the knee in full extension, after ACL repair has been completed. The ACL repair is performed with an internal brace loaded on a TightRope cortical button. One TigerLink and one Fiberlink cinch suture are placed in the ACL remnant. The limbs of these cinch sutures are passed through the femoral tunnel. Fixation of the internal brace on the tibial side is performed with a SwiveLock anchor, with the knee in full extension. The 2 limbs of the cinch sutures are then tensioned and knotted over the tightrope button. The ALL graft is then tensioned and secured at the femoral origin using a suture from the SwiveLock anchor previously placed in this location. Graft fixation is performed with the knee in full extension and neutral rotation.