Abstract
Purpose
Explore the effect of Baihe Dihuang powder on chronic stress depression rat models.
Methods
Chronic stress depression rat models were established with different stimuli for 21 days. At the same time, the drug was administered for 21 consecutive days. The animals were weighed once a week after the start of the formal experiment. On the second day after the end of drug administration, conduct sugar water consumption test and open-filed box experiment, and conduct behavioral observation; At the end of behavioral testing, blood was taken from the eyeball and plasma was separated to measure MDA level and erythrocyte SOD activity; Take brain for homogenate, then measure the contents of 5-HT, NE and DA in brain tissue homogenate; Take the thymus and spleen, stained with 10% formalin fixation, embedding and HE staining, then use microscope to observe the histopathological changes.
Results
Chronic stress depression rats model replicated successfully. Each group of given drugs could increase the weight, the consumption of sugar water, and improve the behavioral score, increase erythrocytes SOD activity and decrease MDA level of plasma, increase the content of 5-HT, NE and DA of brain homogenate, and improve the pathological changes of thymus and spleen of chronic stress depression model animals.
Conclusion
Chronic stress depression rat model replicates successfully. Baihe Dihuang powder can interfere chronic stress depression rats model through different action pathways.
Keywords: Baihe Dihuang powder, Chronic stress depression, Monoamine neurotransmitter, Action pathways
1. Introduction
Depression is a somatic syndrome characterized by persistent low mood, lack of interest, decreased voluntary activity, no pleasure experience and sleep disorder (Surget et al., 2011). Depression is expected to become the second leading cause of death and disability in humans by 2020, according to the WHO (Rutledge et al., 2017). With the understanding of depression, western medicine has put forward different hypotheses, monoamine neurotransmitter hypothesis, neurotrophic hypothesis, pituitary-hypothalamic-adrenal cortical axis disorder hypothesis and so on (Liang et al., 2018). According to different hypotheses, different types of drugs were used to treat depression, but western medicine had poor compliance and high recurrence rate of symptoms. Depression can occur alone or with a variety of diseases, such as post-stroke depression (Mattias et al., 2016), perimenopausal depression (Miao et al., 2017), and postpartum depression (Kirkan et al., 2015, Suto et al., 2016). Since depression is accompanied by varying degrees of emotional disorder, a little stimulation can aggravate mental burden and even endanger life, so it is very necessary to adopt the methods and drugs that are easy for patients to accept.
The idea of Baihe Dihuang powder in the treatment of chronic stress depression in rats was derived from Baihe Dihuang decoction recorded in Synopsis of Golden Chamber wrote by Zhang Zhongjing. In Zhang Zhong Jing's recipe, both are given as fresh juice. Traditional clinical practice is often used for the treatment of depression syndrome and lily disease (Meng et al., 2018). Ancient doctors believed that the causes of depression syndrome were quite complex, and the lesions involved the five organs and qi and blood fluid, which were caused by emotional disturbance and stagnation of qi. And the clinical manifestations of lily disease include palpitation and insomnia, loss of appetite, trance of mind and anxiety (Zhao et al., 2018). Depression is a kind of serious mental disorder, ranking first in the list of psychiatric disorders (Smith, 2014), with the psychopathic change of emotion as the main symptom, and the clinical manifestations are depression and lack of words, and the serious ones will have a strong suicidal tendency. Depression syndrome and lily disease of traditional Chinese medicine with the so-called depression of modern medicine are “different names” of the same disease. Baihe Dihuang decoction and its addition and subtraction have been widely used in the treatment of depression, but there is no research report of Baihe Dihuang powder on depression. Because powders are conducive to the realization of fresh Baihe Dihuang decoction in the treatment of depression drugs throughout the year, so our laboratory has applied for a related patent (Miao et al., 2014). Therefore, on the basis of Baihe Dihuang decoction, fresh Baihe and fresh Dihuang were beaten into powder at 1:1 ratio, so as to observe its effect on the rat models of chronic stress depression, and discuss the feasibility.
2. Experimental materials
2.1. Drugs and reagents
Fresh Dihuang, Jiaozuo Wuzhi county planting base of Huaiyao; Fresh lily bulb, Xinyang lily base provided; Identified by professor Chen Suiqing of Henan university of traditional Chinese medicine, Dihuang is the root of perennial herbs Dihuang of the scrophulariaceae; Baihe are the fleshy scales of lilies, the perennial herb of liliaceae. Baihe and Dihuang were treated by freeze-drying respectively, and then the two were powdered in a ratio of 1:1. Baihe Dihuang powder were made by pharmaceutical laboratory of Henan university of traditional Chinese medicine.
Clomipramine hydrochloride, Shanghai Xinyi Jiufu Pharmaceutical Co., Ltd. MDA, SOD detection kit, Nanjing institute of biological engineering; O-benzodiazepine, Shanghai chemical reagent procurement supplies Wulian chemical plant; Dopamine (DA), Norepinephrine (NE) and 5-hydroxytryptamine (5-HT), Sigma company; Sodium periodate, Tianjin Fuchen chemical reagent factory; EDTANa2, Bao Xin biotechnology co. LTD; Disodium hydrogen phosphate, Tianjin Kaitong chemical reagent co. LTD; Sodium dihydrogen phosphate, Tianjin Fuchen chemical reagent factory.
2.2. Experimental animals
Wistar rats, SPF level, weighing 150–180 g, male, Hebei medical laboratory animal center, license number: 701022.
2.3. Experimental apparatus
F-4500 fluorescence spectrophotometer, Hitachi LTD. FA(N)/JA(N) series electronic balance, Shanghai Minqiao precision instrument Co., Ltd. UV-2000 ultraviolet visible spectrophotometer, Uniko (Shanghai) instrument Co., LTD. TGL-16G high speed refrigerated centrifuge, Shanghai anting science instrument factory. Incubator, Beijing Yong Guangming medical instrument factory.
3. Experimental method
3.1. Molding and grouping (Yang et al., 2018, Chen et al., 2017)
After 1 week of adaptive feeding, 72 rats with similar score, weight and sugar water consumption were selected by Open field scoring. 72 rats were randomly divided into blank group, model group, clomipramine hydrochloride group (20 mg/kg) and large, middle and small dose Baihe Dihuang powder group (2. 4 g/kg, 1. 8 g/kg, 1. 2 g/kg). Except for the blank group, the other 5 groups of rats made chronic stress depression models. All rats were weighed once a week. The specific modeling method is shown in Table 1. The corresponding dosage of drugs was given on the first day of mold making. The model group and the blank group were given the same volume of saline for 21 consecutive days. Weight on day 22, did sugar water consumption test and Open-filed test, then taken blood from the orbit and separated plasma, WST-1 method determined the content of SOD in plasma (erythrocyte SOD activity) and Thibabituric Acid (TBA) method determined MDA; Preparation of brain tissue homogenate, measured the contents of 5-HT, NE and DA in brain tissue homogenate; Take thymus and spleen, 10% formalin fixation, and the effects on immune organs were observed by embedding, slicing, HE staining through microscopic examination.
Table 1.
Stimulation schedule of chronic stress depression rat model.
| Date | Stimulation | Date | Stimulation | Date | Stimulation |
|---|---|---|---|---|---|
| D1 | 2 h behavioral restrictions | D8 | Ban water for 24 h | D15 | 2 h behavioral restrictions |
| D2 | Ban water for 24 h | D9 | Clip tail for 1 min | D16 | Clip tail for 1 min |
| D3 | Forced swimming for 5 min | D10 | Shocking for 5 min | D17 | Lighting for 24 h |
| D4 | Clip tail for 1 min | D11 | Lighting for 24 h | D18 | Forced swimming for 5 min |
| D5 | Lighting for 24 h | D12 | Forced swimming for 5 min | D19 | Shocking for 5 min |
| D6 | Fasting for 24 h | D13 | Fasting for 24 h | D20 | Ban water for 24 h |
| D7 | Shocking for 5 min | D14 | Clip tail for 1 min | D21 | Fasting for 24 h |
3.2. Behavioral experimental operation
Sugar water consumption test: 1% sucrose water consumption in each group was tested in the morning 1 day before and 1 day after model preparation. Water was forbidden for 12 h before the test and sucrose water intakes were measured within 1 h.
Open-filed test (Li et al., 2017, Kuang et al., 2016): The device is a vertical square open box, 40 cm high, 80 cm long and 80 cm wide. The surrounding wall and the bottom surface are black, and the bottom surface is composed of 25 pieces of equal area, divided by white lines. At the beginning of the experiment, make rats at the center of the open box, observing rats within 3 min through bottom blocks (four claws are inside) the level of activity (crossing) score, and hind legs straight times of vertical activities (rearing) score. After each experiment, the feces were thoroughly removed. Each animal was measured once in the morning 1 day before and 1 day after the experiment, and the scores of each group were compared. The experiment was carried out in a quiet room.
4. Statistical methods
SPSS 24. 0 for Windows statistical software was used for data analysis, the measurement results were expressed as —x—x ± s. One-way anova analysis used for the comparison between groups of measurement data. The hierarchical data were analyzed using Ridit.
5. Experimental results
5.1. Effects on weight of chronic stress depression rat models
As we can see from Table 2: There was no significant difference in the initial weight of each group, indicating that the group was even. Compared with the blank group, the rats in the model group lost weight from the first week to the third week, which was obviously lower at the third week (P < 0.05); Compared with the model group, the weight of each group increased at week 1 and week 2, By week 3, the weight of Baihe Dihuang powder in the high-dose group and the low-dose group increased obviously (P < 0.05). The other groups were not statistically significant in promoting weight gain in rats.
Table 2.
Effects on weight of chronic stress depression rat models ( ± s, g).
| Group | Dose (g/kg) | Initial weight | Weight at week 1 | Weight at week 2 | Weight at week 3 |
|---|---|---|---|---|---|
| Blank group | – | 169.3 ± 12.2 | 213.8 ± 31.3 | 268.6 ± 40.3 | 300.5 ± 40.1* |
| Model group | – | 165.6 ± 8.7 | 203.5 ± 14.1 | 249.1 ± 21.4 | 272.3 ± 21.8 |
| CH group | 0.02 | 166.7 ± 9.2 | 206.2 ± 18.9 | 255.5 ± 22.7 | 288.8 ± 21.9 |
| FLR group | 2.4 | 167.4 ± 12.6 | 205.2 ± 25.4 | 261.4 ± 28.4 | 297.3 ± 28.8* |
| 1.8 | 169.6 ± 11.1 | 207.6 ± 28.1 | 260.1 ± 31.6 | 287.8 ± 30.5 | |
| 1.2 | 170.1 ± 10.2 | 211.4 ± 19.6 | 261.1 ± 29.4 | 300.2 ± 26.7* |
Note: **Represent compared to the model group P < 0.01; CH group: clomipramine hydrochloride group, FLR group: Baihe Dihuang powder group.
Represent Compared to the model group P < 0.05.
5.2. Effects on sugar water consumption of chronic stress depression rat models
As we can see from Table 3: Compared with the blank group, the consumption of sugar water was significantly reduced in the model group (P < 0.01); Compared with the model group, both the large, medium and small dose Baihe Dihuang powder group and clomipramine hydrochloride group could significantly increase the consumption of sugar water in chronic stress depression rat models (P < 0.01).
Table 3.
Effects on sugar water consumption of chronic stress depression rat models ( ± s).
| Group | Dose (g/kg) | Sugar water consumption (ml) |
|---|---|---|
| Blank group | – | 27.08 ± 7.33** |
| Model group | – | 14.75 ± 3.89 |
| CH group | 0.02 | 21.92 ± 5.71** |
| FLR group | 2.4 | 24.08 ± 6.46** |
| 1.8 | 21.92 ± 5.63** | |
| 1.2 | 20.42 ± 4.10** |
Note: *Represent Compared to the model group P < 0.05.
Represent compared to the model group P < 0.01; CH group: clomipramine hydrochloride group, FLR group: Baihe Dihuang powder group.
5.3. Effects on Open-filed test of chronic stress depression rat models
According to the experimental method prescribed by the open-filed experiment, the score of horizontal motion and vertical motion within 3 min within 1 day after the end of the experiment were observed for each group of rats. The results are shown in Table 4.
Table 4.
Effects on Open-filed test of chronic stress depression rat models ( ± s).
| Group | Dose (g/kg) | Score of horizontal motion | Score of vertical motion |
|---|---|---|---|
| Blank group | – | 30.25 ± 11.20** | 8.58 ± 1.18** |
| Model group | – | 12.00 ± 6.95 | 4.08 ± 2.19 |
| CH group | 0.02 | 22.58 ± 11.58* | 9.33 ± 5.19** |
| FLR group | 2.4 | 16.00 ± 5.08 | 6.50 ± 3.09* |
| 1.8 | 19.17 ± 8.85* | 7.17 ± 4.13* | |
| 1.2 | 25.17 ± 15.45* | 8.83 ± 3.56** |
Represent Compared to the model group P < 0.05.
Represent compared to the model group P < 0.01; CH group: clomipramine hydrochloride group, FLR group: Baihe Dihuang powder group.
As we can see from Table 4: Compared with the blank group, both horizontal and vertical motion scores of the model group significantly decreased within 3 min (P < 0.01); Compared with the model group, both the middle and small dose Baihe Dihuang powder group and clomipramine hydrochloride group could obviously increase the rats' horizontal motion score within 3 min (P < 0.01); The large and middle dose Baihe Dihuang powder group could obviously increased the score of vertical motion (P < 0.05), the small dose group and clomipramine hydrochloride group could significantly increase the score of vertical motion (P < 0.01).
5.4. Effects on plasma MDA level and erythrocyte SOD activity of chronic stress depression rat models
As we can see from Table 5: Compared with the blank group, the SOD activity of erythrocytes in the model group obviously decreased (P < 0.05), and the plasma MDA level increased. Compared with the model group, the SOD activity of erythrocytes was obviously increased in the large and middle dose Baihe Dihuang powder group (P < 0.01); The plasma MDA level of the model rats was decreased in each dose of Baihe Dihuang powder, but there was no statistical significance.
Table 5.
Effects on plasma MDA level and erythrocyte SOD activity of chronic stress depression rat models ( ± s).
| Group | Dose (g/kg) | Erythrocyte SOD activity (u/L) | MDA level (n mol/m1) |
|---|---|---|---|
| Blank group | – | 132.8 ± 24.8* | 4.71 ± 1.57 |
| Model group | – | 111.4 ± 19.8 | 5.17 ± 0.64 |
| CH group | 0.02 | 144.2 ± 15.5** | 3.91 ± 1.21** |
| FLR group | 2.4 | 131.6 ± 16.6* | 5.09 ± 1.03 |
| 1.8 | 130.9 ± 20.6* | 4.84 ± 1.04 | |
| 1.2 | 117.8 ± 22.9 | 4.35 ± 1.09 |
Represent Compared to the model group P < 0.05.
Represent compared to the model group P < 0.01; CH group: clomipramine hydrochloride group, FLR group: Baihe Dihuang powder group.
5.5. Effect on the level of monoamine neurotransmitters in brain homogenate of chronic stress and depression rats models
As we can see from Table 6: Compared with the blank group, the levels of NE, 5-HT and DA were significantly decreased in the brain tissues of the model group (P < 0.01). Compared with the model group, the levels of NE, 5-HT and DA in brain tissue of rats in the large, middle and small dose Baihe Dihuang powder group and clomipramine hydrochloride group were significantly increased (P < 0.01).
Table 6.
Effect on the level of NE, 5-HT and DA in brain homogenate of chronic stress and depression rats models ( ± s).
| Group | Dose (g/kg) | NE (μg/g) | 5-HT (μg/g) | DA (μg/g) |
|---|---|---|---|---|
| Blank group | – | 0.91 ± 0.08** | 0.74 ± 0.04** | 0.75 ± 0.04** |
| Model group | – | 0.54 ± 0.13 | 0.54 ± 0.14 | 0.47 ± 0.08 |
| CH group | 0.02 | 0.77 ± 0.08** | 0.99 ± 0.04** | 0.70 ± 0.06** |
| FLR group | 2.4 | 0.80 ± 0.06** | 0.98 ± 0.04** | 0.69 ± 0.08** |
| 1.8 | 0.71 ± 0.06** | 1.01 ± 0.03** | 0.64 ± 0.04** | |
| 1.2 | 0.77 ± 0.10** | 0.98 ± 0.09** | 0.64 ± 0.08** |
Note: *Represent Compared to the model group P < 0.05.
Represent compared to the model group P < 0.01; CH group: clomipramine hydrochloride group, FLR group: Baihe Dihuang powder group.
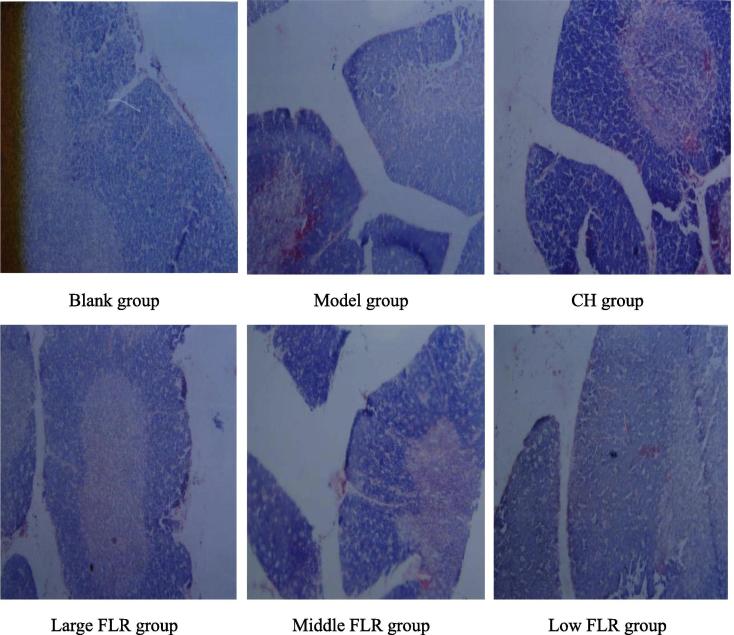
5.6. Effects on the morphology of thymus in chronic stress depressed rats
Effect on the thymus (Fig. 1): In the blank group, the parietal lobule of thymus was clear, the boundary between cortex and medulla was clear, and the cortical lymphocytes were dense; In the model group, thymus gland atrophy, cortical and medullary boundaries were not clear, cortical thinning was obvious, and lymphocyte number and density were decreased; In clomipramine hydrochloride group, the lobule of thymus gland was clear, the cortex was thicker than the model, and the cell density was increased obviously; In large, middle and low dose Baihe Dihuang powder group, the parietal lobule of thymus was clear, cortical thickness was thicker than model group, cell density and number were also increased.
Fig. 1.
Effects on the morphology of thymus in chronic stress depressed rats (HE X 100).
As we can see from Table 7: Compared with the blank group, the cortical thickness of thymus and the number of cortical cells was significantly decreased in the model group (P < 0.01). Compared with the model group, the thickness of thymus cortical cortex (P < 0.01) and the number of cortical lymphocytes (P < 0.01) were significantly increased in each drug given group (P < 0.01).
Table 7.
Effects on the morphology of thymus in chronic stress depressed rats ( ± s).
| Group | Dose (g/kg) | Thickness of the thymic cortex (μm) | Cortical cell number |
|---|---|---|---|
| Blank group | 18.3 ± 4.4** | 46.2 ± 8.4** | |
| Model group | 8.1 ± 3.1 | 17.5 ± 4.2 | |
| CH group | 0.02 | 17.4 ± 3.5** | 42.8 ± 7.4* |
| FLR group | 2.4 | 14.5 ± 3.3** | 38.2 ± 6.2** |
| 1.8 | 20.2 ± 4.3** | 50.4 ± 7.2** | |
| 1.2 | 22.4 ± 5.2** | 54.2 ± 8.7** |
Compared to the model group P < 0.05.
P < 0.01; CH group: clomipramine hydrochloride group, FLR group: Baihe Dihuang powder group.
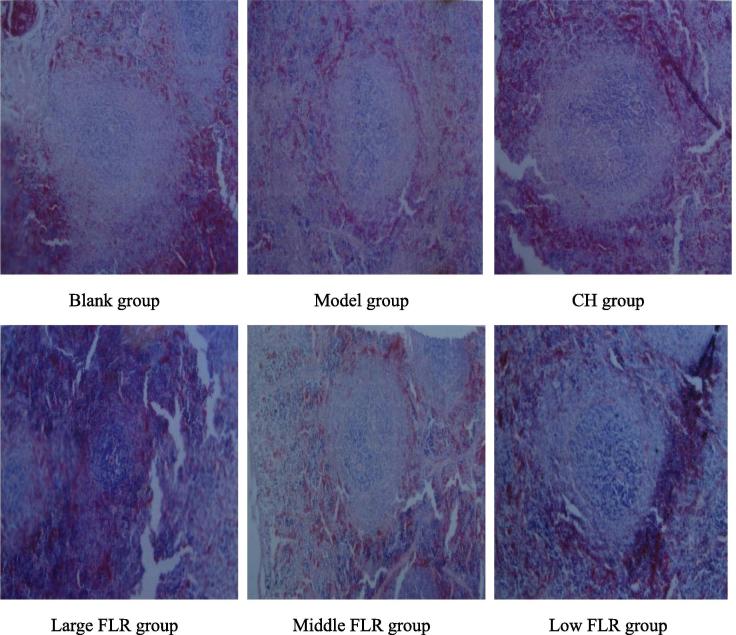
5.7. Effects on the morphology of spleen in chronic stress depressed rats
Effect on the spleen (Fig. 2): In the blank group, the spleen was clearly divided into red and white medulla boundaries, and the spleen sinus and spleen nodule were normal; In the model group, the spleen red and white medullary boundaries were not clear, the splenic nodule was significantly reduced, and the lymphocytes were significantly decreased; In clomipramine hydrochloride group, the spleen red and white medullary division was clear, and the number of splenic nodules and lymphocytes increased; In large, middle and low dose Baihe Dihuang powder group, the spleen nodules were larger than the model, the density of lymphocytes increased.
Fig. 2.
Effects on the morphology of spleen in chronic stress depressed rats (HE X 100).
As we can see from Table 8: Compared with the blank group, the spleen nodule and lymphocyte number of the model group were significantly reduced (P < 0.01); Compared with the model group, the splenic nodules and the cortical lymphocytes of the spleen increased significantly in each group (P < 0.01).
Table 8.
Effects on the morphology of thymus in chronic stress depressed rats ( ± S).
| Group | Dose (g/kg) | Splenic nodules (μm) | Cortical cell number |
|---|---|---|---|
| Blank group | – | 21.4 ± 3.1** | 42.3 ± 10.3** |
| Model group | – | 11.2 ± 2.0 | 14.6 ± 2.1 |
| CH group | 0.02 | 20.1 ± 4.2** | 38.2 ± 8.2** |
| FLR group | 2.4 | 16.2 ± 4.2** | 32.5 ± 4.3** |
| 1.8 | 18.1 ± 3.2** | 37.4 ± 3.2** | |
| 1.2 | 20.4 ± 4.3** | 40.8 ± 4.4** |
Note: *Represent Compared to the model group P < 0.05.
Represent compared to the model group P < 0.01; CH group: clomipramine hydrochloride group, FLR group: Baihe Dihuang powder group.
6. Discuss
The occurrence of depression is caused by the interaction of many factors. Genetic factors and external environment are the important factors that influence the onset of depression. Depressed patients are indifferent to feelings, lack of self-identity, and even have the idea of world-weariness, which brings heavy psychological pressure to themselves and their families. Timely and effective treatment is very necessary. The pathogenesis of depression in modern medicine mainly includes “Neurotransmitter hypothesis”, “neuroplasticity hypothesis”. As well as the patients own immune function decline and neuroendocrine dysfunction (Xu and Lee, 2014, Schatzberg, 2013). In western medicine, tricyclic antidepressants, monoamine oxidase inhibitors and selective 5-hydroxy tryptamine reuptake agents are commonly used for treatment. Although the efficacy is obvious, it is easy to cause the disorder of glucose and lipid metabolism, leading to poor patient compliance. With the increasing attention paid to the theoretical treatment of traditional Chinese medicine, the research on the treatment of depression of traditional Chinese medicine is gradually applied in clinical practice. Depression can be classified into the category of “lily disease”, “depression disease” and “dryness” in traditional Chinese medicine (Yi et al., 2017). Traditional medicine uses fresh Baihe Dihuang decoction for the treatment of “depression and lily disease”, which has been continued from ancient times till now, with positive effects. In traditional medicine, Baihe Dihuang decoction was used for the treatment of depression syndrome and lily disease. The clinical efficacy of fresh Dihunag is exact, but it is a typical seasonal medicine. Over time, there is no fresh Dihuang in the market, and there is no fresh Baihe Dihuang soup, which greatly restricts the application of fresh Dihuang, and also affects the exertion of relevant therapeutic effect. Based on this, under the inspiration of fresh Baihe Dihuang decoction, the two are mixed with powder in 1:1 ratio, and the mechanism of pharmacological effect is discussed, which will help to realize the application of Baihe Dihuang decoction in the treatment of depression drugs all year round. Therefore, this study took body weight, behavioral test, plasma oxidation index, intracerebral neurotransmitter, thymus and spleen pathological observation (immune index) as indicators to conduct the intervention effect of fresh Baihe Dihuang powder on chronic stress depression rat model, providing a basis for its application.
To a certain extent, changes in body weight can be used to evaluate the occurrence, development, prognosis and regression of diseases. In clinical practice, weight loss of most patients with depression can be generally seen, which may be related to patients' loss of appetite (Zhao et al., 2015). During the mold-making process, the weight of rats in the model group was always lower than that of normal rats, and the weight of the drug group tended to increase, indicating that fresh Baihe Dihuang powder could improve the appetite of rats. Depression often shows a certain degree of emotional indifference and laziness to exercise, sugar water consumption experiment can show a certain degree of preference, open-field experiment can show the independent activity and anxiety state of rats (Li et al., 2018, Zhang et al., 2017, Hua-wei et al., 2017). After intervention of fresh Baihe Dihuang powder, could increase the sugar intake, increase the horizontal exercise score and decrease the vertical exercise score of the model rats, indicating that it can improve the emotional and behavioral activity of the depressed rats. Oxidative stress damage involves the oxidation of proteins, nucleic acids, membrane lipids, etc. by free radicals, leading to cell degeneration and even death, which is one of the important mechanisms of depression. SOD is an important enzyme of lipid peroxidation, which can effectively eliminate superoxide anion free radicals generated by biological oxidation and has the effect of stopping the chain reaction of free radicals. MDA is one of the most important products of lipid peroxidation. Excessive accumulation of MDA can damage cell structure and function (Liu et al., 2015, Edula et al., 2017, Liu et al., 2016). Fresh Baihe Dihuang powder could decrease plasma MDA level and increase erythrocyte SOD activity of the pathological changes of spleen and thymus glands in depressed rats can be improved significantly after intervention, indicating that it can alleviate the pathological development of depression by interfering with the immune system. rat models, suggesting that it may achieve the protective effect of chronic stress depression rats through anti-oxidative stress injury. According to the “monoamine neurotransmitter hypothesis”, the occurrence of depression is mainly related to low levels of monoamine neurotransmitters such as NE, 5-HT and DA (Dou et al., 2018, Peixoto, 2018), so monoamine neurotransmitters have become the target of most traditional anti-depression drugs. However, the levels of NE, 5-HT and DA in the brain of chronic stress depression rats increased after the intervention of fresh Baihe Dihuang powder, indicating that it may achieve the therapeutic effect by regulating the content of neurotransmitter in the brain of depressed rats. The immune system is closely related to the disease, and the improvement of immune function will help patients to recover their health. Studies have shown that there is immune activation in patients with depression. Thymus and spleen are two important immune organs in the body (Wan et al., 2017, Tong, 2014, Naveed et al., 2018, Babenko et al., 2017, Pati et al., 2017, Tatar et al., 2017, Peng et al., 2017, Gao et al., 2017). The pathological changes of spleen and thymus in chronic stress depression rats can be improved significantly after intervention, indicating that it can alleviate the pathological development of depression by interfering with the immune system.
In conclusion, fresh Baihe Dihuang powder can improve the appetite, emotional cognition and behavioral preference, improve antioxidant capacity and increase the level of monoamine neurotransmitters and immune function of chronic stress depressed rats.
Acknowledgement
This research was financially supported by the National and International Cooperation Bases (2016-151) and Henan Province Results Transformation Project (142107000039).
Footnotes
Peer review under responsibility of King Saud University.
References
- Babenko D., Turmuhambetova A., Sandle T., Pestrea S.A., Moraru D., Chesca A. ACTA Med. Mediterr. 2017;33(4):607–612. [Google Scholar]
- Chen M.Z., Chen J., Huang Y.X., Cheng J., Liao W.T. Study on the effects and mechanism of total flavonoids from armeniaca mume on depression in chronic stress depression model rats. China Pharm. 2017;28(13):1758–1762. [Google Scholar]
- Dou M., Gong A.J., Hui Liang. Improvement of symptoms in a rat model of depression through combined zinc and folic acid administration via up-regulation of the Trk B and NMDA. Neurosci. Lett. 2018 doi: 10.1016/j.neulet.2018.07.036. [DOI] [PubMed] [Google Scholar]
- Edula V., Reddy P.P., Nagulu M. Antidepressant effect of ziziphus mauritania against forced swim test induced depression in wistar rats. Indo Am. J. Pharm. Sci. 2017;4(12):4226–4235. [Google Scholar]
- Gao W., Wang Y., Basavanagoud B., Jamil M.K. Saudi Pharm. J. 2017;25(4):580–586. doi: 10.1016/j.jsps.2017.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua-wei S.H.I., Rong-juan G.U.O., Zhen-wu Z.H.A.O., Hui W.A.N.G., Xiao-fei D.E.N.G., Qing-jie Y.U.A.N., Xiao G.U.O., Jian-you G.U.O., Hui W.A.N.G. Effects of Xingpi Jieyu Fang on behavior and mitochondria ultrastructure of hippocampus and skeletal muscle in depressed rats. J. Beijing Univ. Tradit. Chinese Med. 2017;40(04):284–289. [Google Scholar]
- Kirkan T.S., Aydin N., Yazici E. The depression in women in pregnancy and postpartum period: a follow-up study. Int. J. Soc. Psychiat. 2015;61(4):343–349. doi: 10.1177/0020764014543713. [DOI] [PubMed] [Google Scholar]
- Kuang S.N., Luo Y., Tian X.Y., Zhang L., Yang Y., Yang J.Q. Effect of meloxicam on CUMS-induced depressive-like behavior in rats and its preliminary mechanism. Chinese Pharmacol. Bull. 2016;32(02):263–268. [Google Scholar]
- Li Y.X., Cheng K.C., Liu K.F., Peng W.H., Cheng J.T., Niu H.S. Telmisartan activates PPAR delta to improve symptoms of unpredictable chronic mild stress-induced depression in mice. Sci. Rep. 2017 doi: 10.1038/s41598-017-14265-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T.T., Yu X.F., Li X.T., Wu T. Effects of Guipi Decoction on behavior and the level of BDNF in hippocampus CA3 area on depression model rats. China J. Tradit. Chinese Med. Pharm. 2018;33(07):2827–2831. [Google Scholar]
- Liang R., Yin J., Pan Y., Zhou H.B., Gao S.M., Yu C.Q. Effects of Jiaotai Pill on inflammatory cytokines in depression model mice with chronic unpredictable mild stress. Chinese Tradit. Herbal Drugs. 2018;49(05):1100–1105. [Google Scholar]
- Liu R., Qiu H.M., Jiang X.H., Yao X.K., Wu Y.L., Zhou Q.X. Anti-depressive effects of valproate involved in improvement of oxidative stress balance and elevation of BDNF expression in CUS-induced rat depression model. Chinese J. Clin. Pharmacol. Therap. 2015;20(05):481–485. [Google Scholar]
- Liu H.X., Wang H., Yu L.M., Guo L. The effect of hydrogen sulfideon the behavior and SOD activity and MDA content of hippocampus in rats with chronic stress depression. J. Binzhou Med. Univ. 2016;39(05) 321-323+326. [Google Scholar]
- Mattias V., Johanna M., Christa L. The influence of early depressive symptoms, social support and decreasing self-efficacy on depression 6 months post-stroke. J. Aff. Dis. 2016;20(6):252–255. doi: 10.1016/j.jad.2016.07.041. [DOI] [PubMed] [Google Scholar]
- Meng Y., Jia Y., Wu Y.F., Xiang H., Qin X.M., Tian J.S. Research progress on Baihe Dihuang Decoction in nervous-mental system. Chinese Tradit. Herbal Drugs. 2018;49(01):251–255. [Google Scholar]
- Miao, M.S., Liu, Y.M., Bai, M., 2014. Application of Baihe Dihuang powder in the preparation of drugs for depression. HeNan: CN104208383A, 2014-12-17.
- Miao M.S., Tian S., Guo L., Bai M., Fang X.Y., Liu S.Y. The effect of curculigoside on mouse model of perimenopausal depression. Saudi J. Biol. Sci. 2017;12(8):1894–1902. doi: 10.1016/j.sjbs.2017.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naveed S., Usmanghani K., Sana A., Ali H., Zafar F., Qamar F., Sarwer G., Abbas S., Alam M.T., Shinwari M.I. Pakistan J. Pharm. Sci. 2018;31(1):137–141. [PubMed] [Google Scholar]
- Pati N.B., Gupta V.R.M., Mayasa V., Velivela S.M.D., Hussain A. Indian J. Pharm. Sci. 2017;79(6):849–857. [Google Scholar]
- Peixoto M.F., Cesaretti M.L.R., Hood S.D., Tavares A. Effects of SSRI medication on heart rate and blood pressure in individuals with hypertension and depression. Clin. Exp. Hypertens. 2018:1–6. doi: 10.1080/10641963.2018.1501058. [DOI] [PubMed] [Google Scholar]
- Peng W., Li D., Zhang M., Ge S., Mo B., Li S., Ohkoshi M. Saudi J. Biol. Sci. 2017;24(2):399–404. doi: 10.1016/j.sjbs.2015.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutledge R.B., Moutoussis M., Smittenaar P. Association of neural and emotional impacts of reward prediction errors with major depression. JAMA Psych. 2017;74(8):790–797. doi: 10.1001/jamapsychiatry.2017.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatzberg Alan F. Anna-Monika Award Lecture, DGPPN Congress, 2013: the role of the hypothalamic-pituitaryadrenal (HPA) axis in the pathogenesis of psychotic major depression. World J. Biol. Psychiat.: Off. J. World Fed. Soc. Biol. Psychiat. 2015;16(1/2):2–11. doi: 10.3109/15622975.2014.916414. [DOI] [PubMed] [Google Scholar]
- Smith K. Mental health: a world of depression. Nature. 2014;515(7526):181. doi: 10.1038/515180a. [DOI] [PubMed] [Google Scholar]
- Surget A., Tanti A., Leonardo E.D. Antidepressants recruit new neurons to improve stress response regulation. Molecul. Psych. 2011;16(12):1177–1188. doi: 10.1038/mp.2011.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suto M., Isogai E., Mizutani F. Prevalence and factors associated with postpartum depression in fathers: a regional, longitudinal study in Japan. Res. Nurs. Health. 2016;39(4):253–262. doi: 10.1002/nur.21728. [DOI] [PubMed] [Google Scholar]
- Tatar S., Yontar Y., Ozmen S. Turkish J. Med. Sci. 2017;47(6):1673–1680. doi: 10.3906/sag-1701-160. [DOI] [PubMed] [Google Scholar]
- Tong H.Y., Wujisi G.L., Bai L.F., Bao W.Y., Hurile B.G., Li Q., Zhang Y. Effects of Mongolian pharmaceutical betel Shisanwei ingredients pill on nerve-endocrine-immune function in depressive rats. Chinese J. Exp. Tradit. Med. Formulae. 2014;20(09):194–198. [Google Scholar]
- Wan L., Liu J., Huang C.B., Zhang X.J., Wang Y.L., Zhang P.H., Sun Y., Liu L. Effects of triptolide on the autophagy in synovial, spleen and thymus of rats with adjuvant arthritis. J. Sichuan Univ. (Med. Sci. Ed.) 2017;48(04):520–525. [PubMed] [Google Scholar]
- Xu R.Y., Lee H.K. Application of electro-enhanced solid phase microextraction combined with gas chromatographymass spectrometry for the determination of tricyclic antidepressants in environmental water samples. J. Chromatogr., A: Including Electroph. Other Separat. Methods. 2014;1350:15–22. doi: 10.1016/j.chroma.2014.05.024. [DOI] [PubMed] [Google Scholar]
- Yang D., Yu Y., Yang P. Expression of TREK-1 and glial fiber acidic protein in hippocampus of rats with depression induced by chronic unpredictable stress and the effect of fluoxefine. Chinese J. Clin. Psychol. 2018;26(01):43–46. [Google Scholar]
- Yi B., Du Q., D J.Y., Li J.Y. Treating depression in TCM. Clin. J. Chinese Med. 2017;9(01):77–78. [Google Scholar]
- Zhang L., Zhao M.K., Sui R.B. Cerebellar fastigial nucleus electrical stimulation alleviates depressive-like behaviors in post-stroke depression rat model and potential mechanisms. Cell. Physiol. Biochem. 2017;41(4):1403–1412. doi: 10.1159/000467940. [DOI] [PubMed] [Google Scholar]
- Zhao H.M., Rong B.S., Bai Y.W. Research progress of Baihe Dihuang decoction in treating mental disease. J. Dis. Monit. Contr. 2018;12(02):149–152. [Google Scholar]
- Zhao Y., Xia C.Y., Bao Y.M., He L. The effect of Ginkgo biloba extract 50 on behavior and inflammatory cytokines levels in depressed rats. Pharmacol. Clin. Chinese Mater. Med. 2015;31(03):88–92. [Google Scholar]