Abstract
Our study aims to estimate the burden of hepatitis C virus (HCV) infection among the general population in Mainland China. We searched 4 databases for studies of the prevalence of anti-HCV antibody among the general population. Studies that met the selection criteria were included in the meta-analysis. Ninety-four studies with 10729 929 individuals were finally included. Overall, the prevalence of anti-HCV antibody among the general population in Mainland China is 0.91% (95% confidence interval, 0.81%–1.03%). The prevalence rates of anti-HCV antibody were geographically different, with a range of 0.32%–6.51%, and the East and South of China had a relatively lower prevalence. The prevalence of anti-HCV antibody increased successively from 0.16% to 3.95% with advancing age. It was noteworthy that the prevalence of anti-HCV antibody decreased continuously from 2.09% to 0.45% during 1991–2010, whereas it increased to 0.58% during 2011–2015.
Keywords: general population, hepatitis C virus infection, Mainland China, prevalence of anti-HCV antibody
Hepatitis C virus (HCV) infection is a global public health problem that can be transmitted through blood, sexual contact, and from mother to child. According to the World Health Organization (WHO) report in 2017, the global prevalence of anti-HCV antibody is around 1.0% and nearly 71 million people are chronically infected [1, 2]. Due to the lack of symptoms of HCV infection, most infected patients do not know their disease status. Thus, accurate data on the prevalence of chronic hepatitis C are not available. In 2016, the 69th World Health Assembly approved the Global Health Sector Strategy to eliminate viral hepatitis by 2030 [2]. To achieve this goal, it is essential to improve our understanding of the epidemiology of HCV infections.
Globally, in 2015, it was estimated that the Eastern Mediterranean Region had the highest prevalence of HCV RNA (2.3%) followed by the European Region (1.5%) [1]. The Western Pacific Region, where China is located, had a viremic HCV prevalence of 0.7% [1]. In China, a survey conducted in 1992 showed that the prevalence of anti-HCV antibody was 3.2% [3]. Consequently, the Chinese government made an updated policy concerning screening of blood donors. Since 1993, all blood donors have been screened for anti-HCV antibody, and this policy became law in 1998. Beginning in 2015, the screening of HCV RNA was applied in anti-HCV antibody–negative blood donors. Additionally, China has successively issued a Technical Standard for Disinfection and Standards for Nosocomial Infection Control to prevent the transmission of HCV [4]. The first guideline for the prevention and treatment of hepatitis C was issued in 2004, and it was updated in 2015 [4, 5]. After many years of efforts, the prevalence of anti-HCV antibody in China has dropped to 0.43%, according to a survey in 2006 [6]. However, the Chinese Ministry of Health reported that the number of chronically infected patients with HCV increased from 70 681 cases in 2006 to 201 622 cases in 2012 [7]. HCV infection might have increased in China in recent years. Unfortunately, there has been no nationwide HCV epidemiological survey since 2006.
To promote evidence-based policy-making and resource allocation, it is essential to estimate the burden of HCV infection in China. Thus, we conducted a systematic review to provide comprehensive and reliable epidemiological characteristics of HCV infection among the general population in Mainland China.
METHODS
Search Strategy
We searched PubMed, Embase, China National Knowledge Infrastructure (CNKI), and Wanfang Database from January 1990 to October 2016 with the following terms: hepatitis C or HCV, prevalence or epidemi*, China or Mainland China. The term “humans” was also used for a Quick Limit of PubMed searching. Our analyses were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [8].
Data Extraction and Selection Criteria
Evaluation of all articles and data extraction were completed independently by 2 reviewers, and disagreements were resolved by discussion. The following information was extracted: name of first author, year of publication, sample collection period, province of study, study area (urban or rural), sample size, number of patients positive for anti-HCV antibody, gender, age, blood donors, reagents used for testing, etc.
The inclusion criteria for study selection were (1) the study was performed in the general population in Mainland China; (2) the study had sufficient data to calculate the prevalence of anti-HCV antibody, including sample size, the number of individuals with anti-HCV antibody, and/or proportion with anti-HCV antibody. The exclusion criteria were (1) the study enrolled a high-risk population only (such as drug users, homosexuals, sex workers, sexually transmitted disease clinic clients, HIV-coinfected persons, hepatitis B virus (HBV)– or other hepatitis virus–coinfected persons, individuals with a history of paid blood donation, etc.); (2) review or meta-analysis or case report; (3) disease surveillance reports; (4) study with a sample size <50.
Statistical Analysis
Because of the low original prevalence of anti-HCV antibody in the included studies, we calculated prevalence estimates using the variance-stabilizing double arcsine transformation according to the method reported previously, and studies with a prevalence of 0% could thus be included in the analysis [9, 10]. Heterogeneity between studies was tested with Cochran’s Q test (P < .10 was considered significant heterogeneity) and the I2 statistic (values of 25%, 50%, and 75% were considered low, moderate, and high degrees of heterogeneity, respectively). Because of the high heterogeneity (>75%) between studies, a random-effects model was used for meta-analysis. Subgroup analyses classified by study area, gender, age, and the year of the study were also performed. All statistical analyses were done using Stata 13.1 (STATA Corporation, College Station, TX). ArcGIS 10.2 (ESRI, Redlands, CA) was applied for map construction.
RESULTS
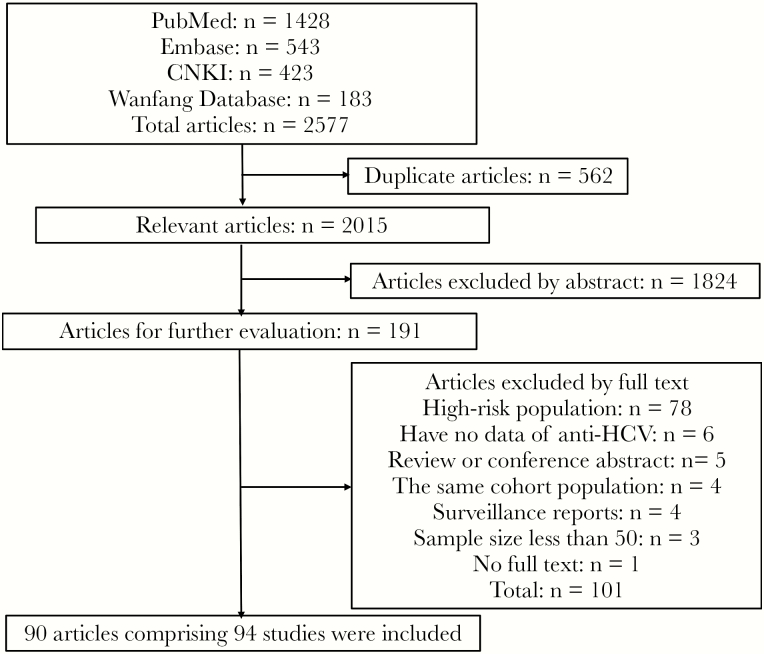
A total of 2577 articles were identified through the literature search, and 562 articles were removed for being duplicates. After initial screening, 191 articles remained for full-text evaluation. As a result, 90 articles comprising 94 studies with 10 729 929 individuals were finally included in the meta-analysis. The search results and the flowchart of selection of studies are shown in Figure 1. The characteristics of each study are summarized in Supplementary Table 1.
Figure 1.
Flow chart of the literature search and selection of studies. Abbreviation: HCV, hepatitis C virus.
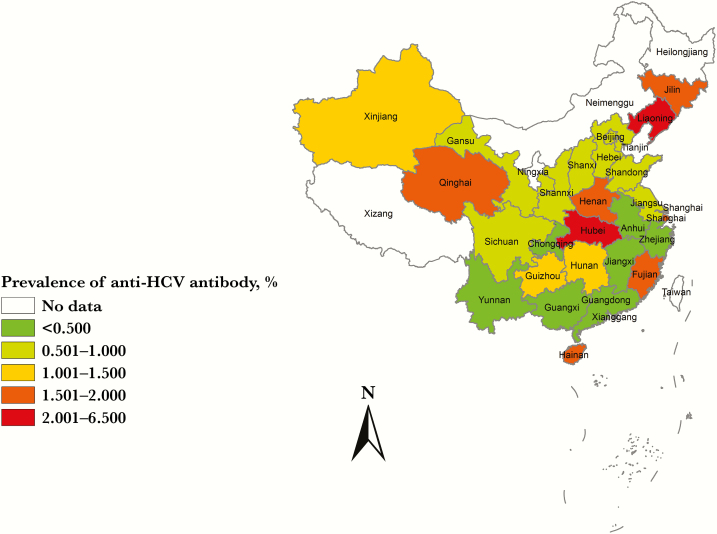
Prevalence of Anti-HCV Antibody in Different Regions of Mainland China
The prevalence of anti-HCV antibody in different provinces and geographic regions among the general population in Mainland China are shown in Table 1 and Figure 2. The prevalence of anti-HCV antibody were geographically different, with a range of 0.32% to 6.51%. The provinces with the highest prevalence of anti-HCV antibody were Hubei and Liaoning, located in Central and Northeast China, with a prevalence of 6.51% (95% confidence interval [CI], 1.72%–14.07%) and 2.88% (95% CI, 0.03%–10.17%), respectively. Most of the provinces with lower prevalence of anti-HCV antibody were located in the East and South of China, such as Jiangxi, Zhejiang, and Guangdong, with a prevalence of 0.32% (95% CI, 0.30%–0.34%), 0.43% (95% CI, 0.23%–0.69%), and 0.43% (95% CI, 0.32%–0.56%), respectively. Overall, the prevalence of anti-HCV antibody among the general population in Mainland China is 0.91% (95% CI, 0.81%–1.03%).
Table 1.
Prevalence of Anti-HCV Antibody in Different Provinces and Geographic Regions of Mainland China Among the General Population
| Area of Studies | Province or City | No. of Studies | No. of Individuals | Individuals Positive for Anti-HCV | Summary Prevalence of Anti-HCV Antibody, % | 95% CI of Prevalence of Anti-HCV Antibody, % | |
|---|---|---|---|---|---|---|---|
| North | Beijing | 6 | 308 404 | 3484 | 0.98 | 0.55 | 1.52 |
| Tianjin | 1 | 53 034 | 297 | 0.56 | 0.50 | 0.62 | |
| Hebei | 2 | 5419 | 38 | 0.77 | 0.43 | 1.22 | |
| Shanxi | 1 | 5168 | 34 | 0.67 | 0.46 | 0.91 | |
| South | Guangdong | 12 | 2 907 604 | 9783 | 0.43 | 0.32 | 0.56 |
| Guangxi | 1 | 95 645 | 478 | 0.50 | 0.45 | 0.55 | |
| Hainan | 1 | 140 | 2 | 1.76 | 0.25 | 4.57 | |
| East | Shandong | 2 | 345 396 | 2866 | 0.79 | 0.31 | 1.48 |
| Jiangsu | 8 | 361 297 | 1836 | 0.83 | 0.49 | 1.25 | |
| Anhui | 1 | 1658 | 6 | 0.39 | 0.15 | 0.75 | |
| Zhejiang | 4 | 1 636 511 | 4139 | 0.43 | 0.23 | 0.69 | |
| Fujian | 2 | 75 288 | 345 | 1.59 | 0.04 | 7.27 | |
| Shanghai | 2 | 1951 | 37 | 1.82 | 0.98 | 2.95 | |
| Jiangxi | 1 | 265 998 | 855 | 0.32 | 0.30 | 0.34 | |
| Central | Hubei | 2 | 2001 | 184 | 6.51 | 1.72 | 14.07 |
| Hunan | 6 | 236 288 | 1649 | 1.19 | 0.81 | 1.65 | |
| Henan | 6 | 591 275 | 2724 | 1.62 | 1.07 | 2.28 | |
| Northeast | Jilin | 5 | 245 730 | 6950 | 1.68 | 0.46 | 3.64 |
| Liaoning | 2 | 774 669 | 7674 | 2.88 | 0.03 | 10.17 | |
| Northwest | Xinjiang | 3 | 86 812 | 654 | 1.32 | 0.15 | 3.62 |
| Qinghai | 5 | 48 393 | 759 | 1.53 | 0.99 | 2.17 | |
| Shannxi | 3 | 730 758 | 3765 | 0.58 | 0.43 | 0.73 | |
| Gansu | 5 | 353 163 | 3158 | 0.96 | 0.70 | 1.26 | |
| Southwest | Sichuan | 6 | 691 187 | 5080 | 0.61 | 0.47 | 0.76 |
| Yunnan | 3 | 804 771 | 4315 | 0.47 | 0.35 | 0.60 | |
| Guizhou | 1 | 241 | 2 | 1.03 | 0.15 | 2.68 | |
| Chongqing | 1 | 13620 | 62 | 0.46 | 0.35 | 0.58 | |
| Multiple areas | Multiple provinces | 2 | 87508 | 366 | 0.48 | 0.31 | 0.67 |
| Total | 94 | 10729929 | 61542 | 0.91 | 0.81 | 1.03 | |
Abbreviations: CI, confidence interval; HCV, hepatitis C virus.
Figure 2.
Prevalence of anti–hepatitis C virus antibody in different provinces and geographic regions of Mainland China among the general population. Abbreviation: HCV, hepatitis C virus.
Prevalence of Anti-HCV Antibody Stratified by Gender
Twenty-eight studies with a total of 2 618 053 persons (male: 1378100; female: 1239953) compared the prevalence of anti-HCV antibody between males and females (Table 2). The pooled prevalence of anti-HCV antibody for males and females were 1.10% (95% CI, 0.84%–1.40%) and 1.19% (95% CI, 0.91%–1.53%), respectively. There was no significant difference between males and females (P = .78).
Table 2.
Prevalence of Anti-HCV Antibody Stratified by Gender
| Metaregression | |||||||
|---|---|---|---|---|---|---|---|
| Gender | No. of Studies | No. of Individuals | Individuals Positive for Anti-HCV | Summary Prevalence of Anti-HCV Antibody, % | 95% CI of Prevalence of Anti-HCV Antibody, % | Coefficient | P |
| Male | 28 | 1378100 | 11207 | 1.10 | 0.84–1.40 | 0.01 | .78 |
| Female | 1239953 | 9979 | 1.19 | 0.91–1.53 | |||
Abbreviations: CI, confidence interval; HCV, hepatitis C virus.
Prevalence of Anti-HCV Antibody Stratified by Age
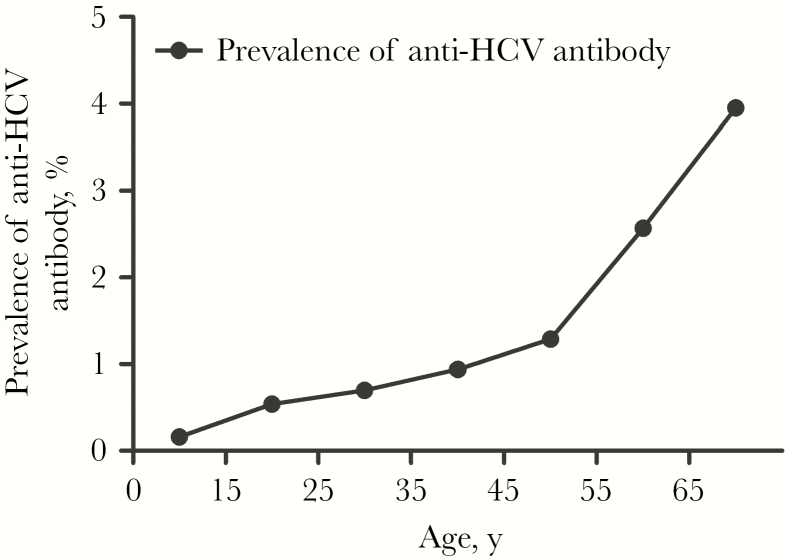
The prevalence of anti-HCV antibody among different age groups was also analyzed, as shown in Supplementary Table 2. According to the available data reported in the included studies, we divided age into 7 groups (<15, 15–25, 25–35, 35–45, 45–55, 55–65, ≥65 years of age). As a result, 14 studies with a total of 2114569 persons were included in the analysis. With advancing age, the prevalence of anti-HCV antibody increased continuously (Figure 3). Persons younger than 15 years of age had the lowest prevalence of anti-HCV antibody (0.16%), whereas people older than 65 years of age had the highest prevalence of anti-HCV antibody (3.95%).
Figure 3.
Prevalence of anti–hepatitis C virus antibody in different age groups among the general population in Mainland China. Abbreviation: HCV, hepatitis C virus.
Prevalence of Anti-HCV Antibody Stratified by Urban and Rural Areas
Eleven studies with 815940 persons investigated the prevalence of anti-HCV antibody in urban vs rural areas (Table 3). The result showed that rural areas had a relatively higher prevalence of anti-HCV antibody (2.02%; 95% CI, 0.97%–3.42%) than urban areas (1.26%; 95% CI, 0.63%–2.09%). However, the difference was not statistically significant (P = .24).
Table 3.
Prevalence of Anti-HCV Antibody Stratified by Urban and Rural Areas
| Metaregression | |||||||
|---|---|---|---|---|---|---|---|
| Location of Studies | No. of Studies | No. of Individuals | Individuals Positive for Anti-HCV | Summary Prevalence of Anti-HCV Antibody, % | 95% CI of Prevalence of Anti-HCV Antibody, % | Coefficient | P |
| Urban | 11 | 407 828 | 3879 | 1.26 | 0.63–2.09 | 0.06 | .24 |
| Rural | 408 112 | 7648 | 2.02 | 0.97–3.42 | |||
Abbreviations: CI, confidence interval; HCV, hepatitis C virus.
Prevalence of Anti-HCV Antibody Among Voluntary Blood Donors
Forty-seven studies with 7085003 persons presented the prevalence of anti-HCV antibody among voluntary blood donors, and the pooled prevalence of anti-HCV antibody was 0.66% (95% CI, 0.57%–0.76%). The distribution of HCV prevalence in different regions among the voluntary blood donors was the same as that in the total general population basically. Overall, the East and South of China had a lower prevalence of anti-HCV antibody than the other regions, and provinces with the lowest prevalence of anti-HCV antibody were Guangdong (0.27%; 95% CI, 0.18%–0.37%) and Fujian (0.27%; 95% CI, 0.24%–0.31%), respectively. In line with the results of the total general population, the provinces with the highest prevalence of anti-HCV antibody among voluntary blood donors were also Hubei (9.57%; 95% CI, 8.29%–10.93%) and Liaoning (2.88%; 95% CI, 0.03%–10.17%), respectively. In addition, the prevalence of anti-HCV antibody in the age groups of 18–25, 25–35, 35–45, and 45–55 among the voluntary blood donors were 0.55% (95% CI, 0.29%–0.88%), 0.58% (95% CI, 0.26%–1.03%), 0.68% (95% CI, 0.34%–1.12%), and 0.78% (95% CI, 0.24%–1.63%), respectively, presenting an increasing trend also.
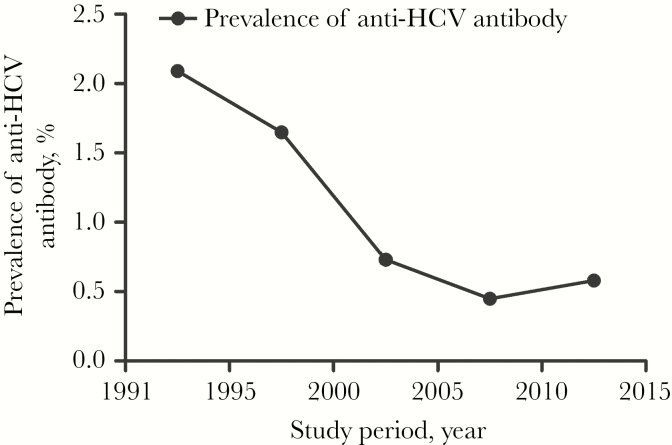
The Dynamic Changes of Prevalence of Anti-HCV Antibody Between 1991 and 2015
Changes in the prevalence of anti-HCV antibody between 1991 and 2015 were also analyzed, as shown in Supplementary Table 3. With respect to the included studies, we arranged studies into 5 time periods (1991–1995, 1996–2000, 2001–2005, 2006–2010, 2011–2015). The results demonstrated that the prevalence of anti-HCV antibody decreased successively from 2.09% to 0.45% during 1991–2010, whereas it increased to 0.58% during 2011–2015 (Figure 4).
Figure 4.
The changes of prevalence of anti–hepatitis C virus antibody among the general population between 1991 and 2015 in Mainland China. Abbreviation: HCV, hepatitis C virus.
DISCUSSION
Our meta-analysis and systematic review included 94 studies with 10729929 individuals and found an overall prevalence of 0.91% (95% CI, 0.81%–1.03%) among the general population in Mainland China from 1991 to 2015. Globally, there is heterogeneity in the prevalence of anti-HCV antibody. As Gower et al. calculated, the prevalence of anti-HCV antibody was high in Egypt (14.7%) and Pakistan (6.7%) before 2013, whereas Italy (2.0%) and Japan (1.5%) had a moderate prevalence [11]. In contrast, China (Mainland) had a low prevalence of anti-HCV antibody (0.91%). Beyond Mainland China, the prevalence of anti-HCV antibody in Taiwan appears to be substantially higher (3.28%) compared with results from this study [12], whereas the prevalence of anti-HCV antibody in Hong Kong was estimated to be as low as 0.3% in the overall population in 2017 [13]. On the other hand, it is important to note that the prevalence of HCV viremia (active HCV infection) will be lower than the result presented in this study because previously infected people who clear the virus are likely to continue to have anti-HCV positivity. However, both past and active infections are potentially infective and therefore carry a public health risk [9].
The prevalence of anti-HCV antibody was different among different geographic regions in Mainland China. Compared with other regions, the South and East of China had a relatively lower prevalence of anti-HCV antibody (e.g., 0.43% in Zhejiang and Guangdong vs 6.51% in Hubei). This finding is in accordance with other reports [6, 7, 14], and this may be associated with better implementation of preventive measures (better health education and better health care systems, etc.) in the South and East of China, where the economy is more developed than other regions of China. Moreover, as most paid blood donors were in North and Central China before 1998, the reservoir of HCV infection may be larger than that in other regions of China. At the same time, it has also been suggested that national health resources for the prevention and control of hepatitis C are more essential in the Northwest, Northeast, and Central regions of China [15]. In addition, we found that rural populations had a relatively higher prevalence of anti-HCV antibody than urban populations (2.02% vs 1.26%), although the difference was not significant (P = .24). Indeed, due to the incomplete data in most of the studies, which were not stratified by urban and rural populations, only 11 studies were included in the analysis. As a result, though the aggregated number of individuals was large, the limited number of included studies may reduce the power to observe statistical differences. Similar to our results, other studies have also revealed a higher prevalence of anti-HCV antibody in the rural population of Mainland China [7, 16–18]. This phenomenon may be related to the bad conditions of both hospitals and patients in the rural areas. In some rural clinics of China, physicians lack systematic training and may not have a thorough understanding of HCV. At the same time, sterilization procedures may not be sufficient, which may lead to HCV transmission during invasive examination and dental treatment [14]. Most people in rural areas are not well educated and do not have a good awareness of hepatitis C. For example, condom use is lower in rural areas, which may increase the chance of HCV transmission through unprotected sexual contact with HCV-infected people [19]. Health education, more thorough screening for HCV infection, and early linkage to care and treatment initiation in rural areas are critical [16].
Consistent with previous studies [6, 20, 21], we also found that there is no significant difference in the prevalence of anti-HCV antibody between males and females, which suggests that both men and women are susceptible to HCV. In agreement with the results of the national survey of HCV prevalence conducted in 2006 [6], we found that the prevalence of anti-HCV antibody increased continuously with advancing age, from 0.16% at age <15 years to 3.95% at age ≥65 years. People older than age 65 years had the highest prevalence of anti-HCV antibody (3.95%), which may have contributed to a greater chance of HCV exposure in the older population. In addition, similar to Mainland China, the prevalence of anti-HCV antibody also increased with age in Hong Kong and Taiwan, China [13, 22]. However, different regions of the world have shown differing trends of HCV prevalence associated with age. In low-income countries, children have been shown to have the highest prevalence of anti-HCV antibody, whereas in high-income countries, the adults have been shown to have the highest prevalence of anti-HCV antibody [11]. The discrepancy might due to the different risk factors for new infections (intravenous drug use in high-income countries vs nosocomial infections in low-income countries) [11].
We tried to analyze the prevalence of anti-HCV antibody among subgroup populations. The prevalence of anti-HCV antibody among voluntary blood donors was relatively lower as compared with the total general population in the current study (0.66% vs 0.91%). Before blood donation, screening (including a physical examination, alanine aminotransferase testing, detection of HBV, HCV, HIV markers, etc.) is required. Only donors who have passed the screening are allowed to donate their blood, and the blood samples from them are examined further. As most patients with liver diseases (including HCV infection) have elevated alanine aminotransferase (ALT), those with elevated ALT are excluded. Healthy people are more likely to donate blood than infected people, however, which could also result in a relatively lower prevalence of anti-HCV antibody among the voluntary blood donors as compared with the total general population. In contrast, paid blood donors had more potential infection opportunities, and the prevalence of anti-HCV antibody among them was much higher than that of voluntary blood donors (3.97% vs 0.82%) [23, 24]. Gao et al. [25] investigated the prevalence of anti-HCV antibody among all blood donors (including paid blood donors) in Mainland China between 1990 and 2010, which demonstrated a much higher HCV prevalence as compared with our study (8.68% vs 0.66%). However, paid blood donation is no longer common in China, and many studies have shown that the prevalence of anti-HCV antibody in voluntary blood donors is less than 0.4% [26–28].
The prevalence of anti-HCV antibody among the general population also appears to be changing over time. During 1991–1995, the prevalence of anti-HCV antibody was about 2.09%, and then it declined continuously to 0.45% during 2006–2010. In 2006, the national epidemiological survey found that the prevalence of anti-HCV antibody in the general population was 0.43% [6], which was basically consistent with the data of our study (0.45%). The changes in blood donors’ recruitment methods (from paid blood donation to voluntary blood donation) and other preventive measures may lead to a decline in the prevalence of anti-HCV antibody in the general population. However, the prevalence of anti-HCV antibody among the general population had an upward change, increasing to 0.58% during 2011–2015. This result was also in line with the data reported by the Chinese Ministry of Health, which indicated that the number of patients with chronic HCV infection had increased from 70681 cases in 2006 to 201622 cases in 2012 [7]. To control the epidemic of HCV infection, paid blood donation was prohibited by law in 1998 in China. Phenomena such as reuse of disposable needles among different individuals have been prohibited by the health authority [29], and HCV RNA testing for blood screening is also performed to prevent HCV transmission [4]. However, most people are not aware of the routes of HCV transmission. Currently in China, HCV transmission through blood or blood products is very low because all blood donors are screened for HCV RNA, HBV DNA, and HIV RNA by sensitive polymerase chain reaction kits. The main modes of HCV transmission are intravenous drug use, sexual contact among homosexual and heterosexual people, and iatrogenic infection (including the use of insufficient sterilization of medical instruments for invasive manipulation and dental treatment) [4]. In some areas of China, intravenous drug use–caused HCV transmission accounts for 60%–90% [4]. In addition, high-risk behaviors like razor sharing, unsafe ear piercing, and tattooing, etc., play a role in HCV transmission in China [30]. Globally, the estimated number of persons newly infected (n = 1.75 million) exceeded the estimated number of persons dying from end-stage HCV infection (n = 399000) and being cured (n = 843000) during 2015; the epidemic of HCV infection in the world may expand in magnitude [1]. Even in some areas of the world where the prevalence of anti-HCV antibody was low in 2015, such as the United States, after many years of decrease, the number of people chronically infected with HCV doubled between 2010 and 2014 [1, 31]. Our data present the same trend as that of the world. Therefore, as HCV infection may occur at any time and through various modes of transmission, it is necessary to further strengthen the prevention and treatment of HCV to reduce HCV infection.
There are some limitations of this study. First, the population included in most of the studies was not randomly selected, and the data pooled in some provinces were mainly from voluntary blood donors (9 of the 12 included studies in Guangdong province were on blood donors); thus, there is potential for selection bias. Second, substantial heterogeneity was found for studies between different regions and years of study. Therefore, a national survey is needed to further clarify the prevalence of anti-HCV antibody among the general population. Third, many studies failed to provide detailed information on the study population, which limited our assessment of the quality of studies.
In conclusion, this systematic review and meta-analysis provide comprehensive HCV prevalence data on the general population in Mainland China. The prevalence of anti-HCV antibody differed across regions, and the South and East of China had a relatively lower prevalence. Though many efforts have been made by the Chinese government to control HCV infection, the prevalence of anti-HCV antibody may present a rising trend in recent years.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
Financial support. This study was supported by a project of the Guangxi Key Laboratory for the Prevention and Control of Viral Hepatitis (Grant No. GXCDCKL201601).
Potential conflicts of interest.All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. World Health Organization. Global hepatitis report, 2017. http://www.who.int/hepatitis/publications/global-hepatitis-report2017/en/. Accessed 6 September 2018. [Google Scholar]
- 2. The Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol 2017; 2:161–76. [DOI] [PubMed] [Google Scholar]
- 3. Zhang M, Sun XD, Mark SD, et al. Hepatitis C virus infection, Linxian, China. Emerg Infect Dis 2005; 11:17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chinese Society of Hepatology and Chinese Society of Infectious Diseases, Chinese Medical Association. The guideline of prevention and treatment for hepatitis C: a 2015 update [in Chinese]. Linchuang Gandanbing Zazhi 2015; 31:1961–79. [Google Scholar]
- 5. Chinese Society of Hepatology and Chinese Society of Infectious Diseases and Parasitic Diseases, Chinese Medical Association. The guideline of prevention and treatment for hepatitis C [in Chinese]. Zhonghua Ganzanbing Zazhi 2004; 12:194–8. [Google Scholar]
- 6. Chen YS, Li L, Cui FQ, et al. A sero-epidemiological study on hepatitis C in China [in Chinese]. Zhonghua Liuxingbingxue Zazhi 2011; 32:888–91. [PubMed] [Google Scholar]
- 7. Zhang Q, Qi W, Wang X, et al. Epidemiology of hepatitis B and hepatitis C infections and benefits of programs for hepatitis prevention in northeastern China: a cross-sectional study. Clin Infect Dis 2016; 62:305–12. [DOI] [PubMed] [Google Scholar]
- 8. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009; 62:e1–34. [DOI] [PubMed] [Google Scholar]
- 9. Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis 2012; 12:859–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Freeman M, Tukey J. Transformations related to the angular and square root. Ann Math Stat 1950; 21:607–11. [Google Scholar]
- 11. Gower E, Estes C, Blach S, et al. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol 2014; 61:S45–57. [DOI] [PubMed] [Google Scholar]
- 12. Yu ML, Yeh ML, Tsai PC, et al. Huge gap between clinical efficacy and community effectiveness in the treatment of chronic hepatitis C: a nationwide survey in Taiwan. Medicine (Baltimore) 2015; 94:e690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maaroufi A, Vince A, Himatt SM, et al. Historical epidemiology of hepatitis C virus in select countries-volume 4. J Viral Hepat 2017; 24(Suppl 2):8–24. [DOI] [PubMed] [Google Scholar]
- 14. Huang P, Zhu LG, Zhai XJ, et al. Hepatitis C virus infection and risk factors in the general population: a large community-based study in eastern China, 2011–2012. Epidemiol Infect 2015; 143:2827–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sun HQ, Xiao GX, Guo Y, Yu SC, Ma JQ. Spatial clustering and changing trend of hepatitis C prevalence during 2008–2012 in China [in Chinese]. Zhongguo Gonggong Weisheng 2014; 3:286–9. [Google Scholar]
- 16. Zhou M, Li H, Ji Y, et al. Hepatitis C virus infection in the general population: a large community-based study in Mianyang, West China. Biosci Trends 2015; 9:97–103. [DOI] [PubMed] [Google Scholar]
- 17. Qin Q, Smith MK, Wang L, et al. Hepatitis C virus infection in China: an emerging public health issue. J Viral Hepat 2015; 22:238–44. [DOI] [PubMed] [Google Scholar]
- 18. Zhao Y, Shen L, Ma J, et al. Epidemiology of hepatitis C virus infection and risk factor analysis in the Hebei Province, China. PLoS One 2013; 8:e75586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang C, Li X, Su S, et al. Prevalence of HIV, syphilis, and HCV infection and associated risk factors among male clients of low-paying female sex workers in a rural county of Guangxi, China: a cross-sectional study. Sex Transm Infect 2014; 90:230–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zheng X, Ding W, Li G, et al. Seroprevalence of transfusion-transmissible infectious agents among volunteer blood donors between 2006 and 2012 in Zhejiang, China. Blood Transfus 2015; 13:401–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Song Y, Bian Y, Petzold M, Ung CO. Prevalence and trend of major transfusion-transmissible infections among blood donors in Western China, 2005 through 2010. PLoS One 2014; 9:e94528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chen CH, Yang PM, Huang GT, et al. Estimation of seroprevalence of hepatitis B virus and hepatitis C virus in Taiwan from a large-scale survey of free hepatitis screening participants. J Formos Med Assoc 2007; 106:148–55. [DOI] [PubMed] [Google Scholar]
- 23. Gao Y. Investigation of blood donors’ anti-HCV positive rate in Taiyuan, China [in Chinese]. Shanxi Linchuang Yiyao 1998; 7:44–5. [Google Scholar]
- 24. Wan CF, Wan LY, Wang BH. Investigation of anti-HCV positive rate in blood donors and plasma donors [in Chinese]. Zhongguo Shuxue Zazhi 1997; 10:41. [Google Scholar]
- 25. Gao X, Cui Q, Shi X, et al. Prevalence and trend of hepatitis C virus infection among blood donors in Chinese Mainland: a systematic review and meta-analysis. BMC Infect Dis 2011; 11:88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chen SL, Zhang X, Chen ZZ, et al. Mutual blood donation is safer at small blood collection stations in China. Transfus Apher Sci 2015; 53:315–9. [DOI] [PubMed] [Google Scholar]
- 27. Fu Y, Xia W, Wang Y, et al. The seroprevalence of hepatitis C virus (HCV) among 559,890 first-time volunteer blood donors in China reflects regional heterogeneity in HCV prevalence and changes in blood donor recruitment models. Transfusion 2010; 50:1505–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shang G, Seed CR, Wang F, Nie D, Farrugia A. Residual risk of transfusion-transmitted viral infections in Shenzhen, China, 2001 through 2004. Transfusion 2007; 47:529–39. [DOI] [PubMed] [Google Scholar]
- 29. Yin WJ, Tan C, Chen M, Liu ZG, Wang ZF. Management of disposable infusion set and injection syringe [in Chinese]. Zhonghua Yiyuan Ganranxue Zazhi 2004; 14:207–8. [Google Scholar]
- 30. He Y, Zhang J, Zhong L, et al. Prevalence of and risk factors for hepatitis C virus infection among blood donors in Chengdu, China. J Med Virol 2011; 83:616–21. [DOI] [PubMed] [Google Scholar]
- 31. C COAN, Practice BOPH, Division HAM, National Academies of Sciences EAM. Eliminating the Public Health Problem of Hepatitis B and C in the United States: Phase One Report. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.