Abstract
Objective:
Insomnia identity refers to the conviction that one has insomnia, which can occur independently of poor sleep. Night-to-night variability in sleep (termed intraindividual variability (IIV)) may contribute to insomnia identity yet remain undetected via conventional mean analyses. This study compared sleep IIV across four subgroups: noncomplaining good sleepers (NG), complaining poor sleepers (CP), complaining good sleepers (CG), and noncomplaining poor sleepers (NP).
Methods:
This study analyzed 14 days of sleep diary data from 723 adults. Participants were classified according to presence/absence of a sleep complaint and presence/absence of poor sleep. A 2×2 multivariate analysis of covariance (MANCOVA) was performed to explore differences on five measures of sleep IIV: intraindividual standard deviation in total sleep time (iSD TST), sleep onset latency (iSD SOL), wake after sleep onset (iSD WASO), number of nightly awakenings (iSD NWAK), and sleep efficiency (iSD SE).
Results:
MANCOVA revealed significant main effects of poor sleep, sleep complaint, and their interaction on sleep IIV. Poor sleepers exhibited greater IIV across all sleep parameters compared to good sleepers. Similarly, individuals with a sleep complaint exhibited greater IIV compared to individuals with no complaint. The interaction revealed that iSD SOL was significantly greater among CP than NP, and iSD NWAK was significantly greater among CG than NG.
Conclusions:
Greater night-to-night variability in specific sleep parameters was present among complaining versus noncomplaining sleepers in good and poor sleep subgroups. These findings suggest certain aspects of sleep consistency may be salient for treatment-seeking individuals based on their quantitative sleep status.
Keywords: Sleep, Sleep Complaint, Intraindividual Variability, Night-to-night Variability, Insomnia Identity
1. Introduction
Insomnia disorder - which is diagnosed based on a report of disturbed sleep combined with a complaint of sleep-related distress and daytime impairment - is a highly prevalent and costly sleep disorder with substantial mental and physical health consequences (American Academy of Sleep Medicine [AASM], 2014; American Psychiatric Association, [APA], 2013). Conventional wisdom may lead one to presuppose an insomnia sleep complaint necessarily results from the presence of poor sleep. However, epidemiological surveys have reported that synchrony between sleep complaint and quantitative sleep status exists among only 66% to 74% of sleepers (Lichstein, Durrence, Taylor, Bush, and Riedel, 2003; McCrae et al., 2005). Interestingly, a considerable number of individuals who endorse a sleep complaint do not display corresponding disturbance in their sleep as determined via polysomnography or sleep diaries (Edinger et al., 2000; Lichstein, 2017; Lichstein et al., 2003; McCrae et al., 2005). The converse also holds true: individuals who exhibit quantitative insomnia symptoms (i.e., sleep onset latency or wake time after sleep onset > 30 minutes per week as established in Lichstein et al., 2003; hereafter termed “poor sleep” for convenience) may or may not exhibit corresponding distress related to their sleep. As a result, individuals can be conceptualized as belonging to one of four subgroups based on the presence/absence of a sleep complaint and good/poor sleep: 1) individuals without poor sleep and without a sleep complaint (noncomplaining good sleepers, NG), 2) individuals who exhibit insomnia symptoms and endorse a sleep complaint (complaining poor sleepers, CP), 3) individuals who do not meet criteria for poor sleep but endorse a sleep complaint (complaining good sleepers, CG), and 4) individuals who meet criteria for poor sleep but deny a sleep problem (noncomplaining poor sleepers, NP).
The discordance observed between quantitative and perceived sleep is not inconsequential. The conviction that one has insomnia (termed “insomnia identity”) and the subjective distress related to this conviction have been shown to more strongly correspond to indicators of daytime impairment than actual sleep disturbance (Fichten et al., 1995; Lichstein, 2017; McCrae et al., 2003; Ustinov et al., 2010). Insomnia complaint has been associated with various domains of daytime and functional impairment - including depression, anxiety, fatigue, daytime sleepiness, insomnia impact, medical problems, and suicidality - independent of diary- or polysomnography-defined sleep parameters (Alapin et al., 2000; Edinger et al., 2000; Fichten et al., 1995; McCrae et al., 2003, 2005; Ustinov et al., 2010; Woosley, Lichstein, Taylor, Riedel, & Bush, 2016).
It is noteworthy that, in comparing the means of several objectively-measured sleep parameters, research has revealed no significant differences between complaining versus noncomplaining individuals within good or poor sleep groups (McCrae et al., 2005). A variety of subjective factors - such as attentional biases, nonrestorative sleep, or dysfunctional beliefs about sleep - may be driving the discrepancy observed between objective sleep and sleep appraisal among CG. Alternatively, intraindividual variability (IIV) in sleep - or the extent to which an individual’s sleep varies from night-to-night - may confer its own unique influence on one’s sleep appraisal yet remain undetected via conventional analyses of mean sleep parameters. Greater night-to-night variability in sleep has also been shown to contribute to objectively defined poor sleep, subjective sleep complaints, and insomnia (Bei et al., 2016; Lemola, Ledermann, & Freidman, 2013). Conventionally, IIV in sleep has been operationalized as the intraindividual standard deviation (iSD) across a single individual’s multiple nights of sleep data. Studies examining IIV emphasize the importance of characterizing sleep parameters beyond their individual means for a more comprehensive understanding of behavioral sleep/wake patterns and their impact on health and wellbeing (Bei et al., 2016). Across the age span, night-to-night differences within an individual have been reported to exceed differences between individuals (Dillon et al., 2015; Knutson, Rathouz, Yan, Liu, & Lauderdale, 2007), further supporting that IIV represents an important dimension for sleep characterization.
A recent systematic review conducted by Bei and colleagues (2016) examined a selection of 53 peer-reviewed empirical publications examining sleep/wake IIV among adults. Across these studies, greater IIV was associated with a variety of demographic, physical health, and mental health factors, including younger age, non-White race/ethnicity, depression symptomatology, and stress. Greater sleep/wake IIV has also been associated with generally higher stress, poorer objective sleep, and insomnia (Bei et al., 2016). However, to date, studies characterizing IIV in sleep among adults have focused predominantly on samples of healthy sleepers, and none have explicitly examined how IIV may contribute to worse subjective perceptions of sleep independent of poor sleep.
Given the current gaps in the existing research literature, the present study sought to explore sleep IIV as a commonly obscured factor contributing to the discordance often documented between sleep and sleep appraisal. Toward this aim, this study examined differences among four identified sleep subgroups (CG, CP, NP, NG) on five dependent measures of sleep IIV: intraindividual standard deviation in total sleep time (iSD TST), wake after sleep onset (iSD WASO), number of nightly awakenings (iSD NWAK), sleep onset latency (iSD SOL), and sleep efficiency (iSD SE). Because complaints often precede treatment seeking, whether the two complaining subgroups differ from the two noncomplaining subgroups - and also from one another - was of particular interest. We hypothesized that there would be significant independent effects of poor sleep and sleep complaint on sleep IIV. Specifically, we predicted that the combined mean iSDs for sleep parameters would be higher, indicating greater sleep IIV, for poor sleepers versus good sleepers. Additionally, we predicted that individuals with a sleep complaint would exhibit greater iSDs for sleep parameters than individuals without a sleep complaint. Mean-level differences in sleep parameters (mTST, mWASO, mNWAK, mSOL, and mSE) were also explored among the four sleep subgroups of interest to further characterize differences across these sleep subgroups.
2. Methods
2.1. Participants
This study utilized archival data from the University of Memphis Sleep Research Project epidemiological survey of sleep and daytime functioning (Lichstein, Durrence, Riedel, Taylor, & Bush, 2004). A random digit dialing procedure was used to recruit a stratified, randomly selected sample of adults from an urban county in the Southeastern United States. To ensure adequate sampling across gender and age, at least 50 men and 50 women were recruited in each age decile, beginning with ages 20 to 29 and ending with 80 and older. To broadly sample the general population, minimal eligibility criteria were utilized. For inclusion in the study, participants were required to be 1) at least 20 years of age and 2) able to read and write in English at an approximately seventh grade level. Individuals in the same household were eligible to participate in the study provided that they did not share the same bed as another participant. If an individual was a cohabitating bedpartner to a participant in the study, he/she was excluded from participation due to concern that there would exist minimal variability in bed partners’ sleep behavior. There were no further exclusion criteria.
Participation in the study required a two-week commitment, during which time participants were asked to complete daily sleep diaries as well as several self-report questionnaires sent to them via mail. Participants who completed and returned the study diaries and questionnaires received monetary compensation. All participants gave their informed consent prior to participation in the study. Original data collection and current study procedures were conducted in accordance with the ethical standards outlined by the Institutional Review Board of the University of Alabama.
Figure 1 provides a flow diagram outlining participant recruitment. A detailed overview regarding sample recruitment and methods of the survey can be found in Lichstein et al. (2004). In brief, during the three-year recruitment phase, 1,769 individuals were successfully recruited, yielding an adjusted response rate of 37.7% (Lichstein et al., 2004). Of the 1,769 recruited individuals, 859 (48.5%) returned their packets. Of the returned packets, 88 (10.2%) had extensively unclear, uninterpretable, incomplete, or duplicate data. Demographic differences between individuals who returned packets versus individuals who did not return packets were unable to be determined.
Figure 1.
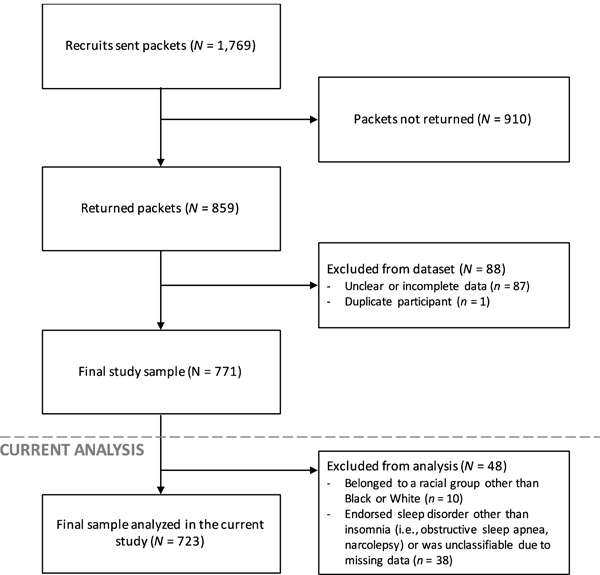
Participant recruitment for an epidemiological study of sleep.
Thus, the final sample consisted of 771 participants, who ranged in age from 20 to 98 years (M = 53.8 years, SD = 19.8 years), were primarily White (69.8%) and Black (28.9%), and were equally distributed between genders (males, 49.4%; females, 50.6%). The percentage of participants within age deciles was as follows: 20 – 29 (14%), 30 – 39 (16%), 40 – 49 (14%), 50 – 59 (15%), 60 – 69 (14%), 70 – 79 (14%), and 80 – 89+ (13%).
2.2. Measures
2.2.1. Demographics and Sleep Complaint.
Participants completed a self-reported health questionnaire, in which they reported their age, gender, and race. The presence of a sleep complaint was assessed via the following questions on the health questionnaire: “Do you have a sleep problem? If yes, describe (e.g., trouble falling asleep, long or frequent awakenings). How long have you had this sleep problem?” (Lichstein et al., 2004). Individuals who reported trouble falling asleep, staying asleep, or insomnia lasting at least 6 months were classified as having a sleep complaint. Individuals who denied a sleep problem were classified as not having a sleep complaint. Individuals with a sleep problem or complaint other than insomnia (i.e., difficulty breathing, obstructive sleep apnea, etc.) were not categorized and were excluded from analysis.
2.2.2. Sleep Diary & Quantitative Sleep Status.
Participants completed two weeks of sleep diaries. Research suggests that 14 sampling points (2 weeks) of self-reported sleep data are necessary to derive stable sleep estimates for most sleep measures (Wohlgemuth, Edinger, Fins, & Sullivan, 1999). Upon awakening, participants were asked to provide a subjective assessment of the following parameters for the previous night’s sleep: (a) bedtime (the clock time that the individual entered bed with the intent of going to sleep), (b) sleep-onset latency (SOL, number of minutes between bedtime and sleep onset), (c) wake after sleep onset (WASO, the number of minutes spent awake after sleep onset and before final awakening), (d) number of nightly awakenings (NWAK), and (e) terminal wake time (TWAK).
From these data, time in bed (TIB) and total sleep time (TST) were calculated. TIB refers to the interval of time between bedtime and rising time. To calculate TST (actual time slept), the total amount of wake time during the sleep period (SOL, WASO, TWAK) was subtracted from TIB. Sleep efficiency (SE) was calculated by dividing TST by TIB, then multiplying by 100. Intraindividual standard deviation (iSDs) for TST, NWAK, WASO, SOL, and SE were calculated across each individual’s 14 nights of data as an estimate of IIV.
Individuals’ sleep status was assessed based on their sleep diaries and empirically- supported quantitative criteria established in Lichstein et al. (2003). Individuals were considered to exhibit poor sleep if their sleep diaries indicated SOL or WASO was 31 or more minutes at least 3 nights per week for the 2 weeks of sleep diaries. Those who did not meet these criteria were classified as good sleepers. Among the epidemiological sample utilized in our current study, the selected severity criterion (≥ 31 minutes WASO and/or SOL) has been shown to maximize sensitivity and specificity between self-defined insomnia status and quantitative classification of insomnia.
2.3. Statistical Analysis
All statistical procedures were conducting using SPSS version 25.0. Two separate 2×2 multivariate analyses of covariance (MANCOVAs) were performed. The first 2×2 MANCOVA crossed sleep complaint (yes/no) and quantitative sleep status (good/poor) to explore sleep subgroup differences on five dependent measures of mean-level quantitative sleep - mTST, mWASO, mNWAK, mSOL, and mSE. The second MANCOVA crossed sleep complaint and poor sleep to explore differences on five dependent measures of sleep night-to-night variability - iSD TST, iSD WASO, iSD NWAK, iSD SOL, iSD SE. Both analyses controlled for the demographic variables of age, race, and gender. Because a significant Box’s M statistic was obtained for both analyses, the Wilks’ lambda (Λ) test statistic was reported since it is more robust to violation of the assumption of homogeneity of the covariance matrix (Field, 2009). Significant multivariate results were followed up with univariate analyses. Significant interactions were explored via simple effects testing.
3. Results
3.1. Sample Characteristics
Prior to analysis, 10 individuals who identified themselves as belonging to a racial group other than Black or White were excluded from analysis due to their limited numbers. An additional 38 individuals were excluded for other sleep disorders (i.e., obstructive sleep apnea, narcolepsy) or being unclassifiable due to missing data. The final sample size (N = 723) comprised 384 NG (50.5%), 105 NP (13.8%), 84 CG (11.0%), and 150 CP (19.7%). A total of 234 individuals reported a sleep complaint (30.7%) and 489 did not have a sleep complaint (64.3%). In terms of quantitative sleep status, 255 individuals met quantitative criteria for poor sleep (35.3%). The remaining 468 individuals (64.7%) were considered to have good sleep.
Table 1 provides a detailed summary of participant race and gender within each age decile. Despite the outlined exclusions, the sample remained generally well-balanced across age and gender. Table 2 provides descriptive statistics for demographic characteristics of the sample as a function of sleep subgroup.
Table 1.
Distribution of sample N by age, race, and gender.
| Full Sample | Black | White | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age Decade | Total | Men | Women | Total | Men | Women | Total | Men | Women |
| 20 – 29 | 99 | 48 | 51 | 39 (39%) | 17 | 22 | 60 (61%) | 31 | 29 |
| 30 – 39 | 113 | 49 | 64 | 44 (39%) | 17 | 27 | 69 (61%) | 32 | 37 |
| 40 – 49 | 95 | 49 | 46 | 32 (34%) | 18 | 14 | 63 (66%) | 31 | 32 |
| 50 – 59 | 108 | 52 | 56 | 31 (29%) | 11 | 20 | 77 (71%) | 41 | 36 |
| 60 – 69 | 103 | 52 | 51 | 27 (26%) | 9 | 18 | 76 (74%) | 43 | 33 |
| 70 – 79 | 107 | 50 | 57 | 15 (14%) | 6 | 9 | 92 (86%) | 44 | 48 |
| 80 – 89+ | 98 | 47 | 51 | 26 (27%) | 12 | 14 | 72 (73%) | 35 | 37 |
| Total | 723 | 347 | 376 | 214 (30%) | 90 | 124 | 509 (70%) | 257 | 252 |
Note: Percentages refer to proportion of Black/White participants within each age decade.
Table 2.
Descriptive statistics for demographic characteristics by sleep subgroup (N = 723).
| Good Sleep | Poor Sleep | |||
|---|---|---|---|---|
| No Complaint (n = 384) |
Complaint (n = 84) |
No Complaint (n = 105) |
Complaint (n = 150) |
|
|
Gender, n
(%) Male Female |
210 (54.7%) 174 (45.3%) |
36 (42.9%) 48 (57.1%) |
41 (39.0%) 64 (61.0 %) |
60 (40.0%) 90 (60.0%) |
|
Race, n
(%) White Black |
288 (75.0%) 96 (25.0%) |
63 (75.0%) 21 (25.0%) |
50 (47.6%) 55 (52.4%) |
108 (72.0%) 42 (28.0%) |
| Age, M (SEM) | 50.4 (0.97) | 54.5 (2.00) | 55.8 (2.04) | 61.5 (1.61) |
3.2. Differences in Mean-level Sleep Parameters by Sleep Complaint and Poor Sleep
A 2×2 MANCOVA with sleep complaint crossed with poor sleep was conducted to assess sleep subgroup differences on five dependent measures of mean-level sleep: mTST, mWASO, mNWAK, mSOL, and mSE. After controlling for age, race, and gender, multivariate analysis revealed significant main effects of poor sleep [Wilks’ Λ = .55, F (5, 712) = 115.1, p < .001, partial η2 = .447] and sleep complaint [Wilks’ Λ = .90, F (5, 712) = 15.1, p < .001, partial η2 = .096], as well as the interaction of poor sleep by sleep complaint [Wilks’ Λ = .96, F (5, 712) = 4.8, p < .001, partial η2 = .033].
3.2.1. Main effect of poor sleep.
Univariate testing indicated that the main effect of poor sleep was significant for each of the five dependent variables under investigation. Individuals with poor sleep exhibited significantly greater SOL, WASO, and NWAK and correspondingly lower TST and SE compared to individuals with good sleep. This analysis served as a manipulation check of the protocol since group assignment was based on SOL and WASO. Results of univariate analyses for the main effect of poor sleep on mean-level sleep are presented in Table 3.
Table 3.
Adjusted means, standard error, and univariate statistics for main effect of poor sleep on mean-level sleep (N = 723).
| Good Sleep (n = 468) |
Poor Sleep (n = 255) |
Univariate test | ||||
|---|---|---|---|---|---|---|
| Mean | SEM | Mean | SEM | F (1, 716) | partial η2 | |
| mTSTa | 424.86 | 4.08 | 399.12 | 4.15 | 20.18** | .027 |
| mSOLa | 16.63 | 0.92 | 37.28 | 0.94 | 254.59** | .262 |
| mWASOa | 15.01 | 1.41 | 46.11 | 1.43 | 248.59** | .258 |
| mNWAKb | 1.37 | 0.06 | 1.92 | 0.06 | 39.06** | .052 |
| mSEc | 89.09 | 0.39 | 77.93 | 0.40 | 414.69** | .367 |
Average minutes for each sleep parameter.
Average number of awakenings.
Average percentage sleep efficiency.
p < .05,
p < .001.
3.2.2. Main effect of sleep complaint.
Univariate testing indicated that the main effect of sleep complaint was significant for each of the five dependent variables under investigation. Individuals with a sleep complaint exhibited greater SOL, WASO, and NWAK as well as lower TST and SE compared to those without a complaint. Results of univariate analyses for the main effect of sleep complaint on mean-level sleep are presented in Table 4.
Table 4.
Adjusted means, standard error, and univariate statistics for main effect of sleep complaint on mean-level sleep (N = 723).
| No Complaint (n = 489) |
Complaint (n = 234) |
Univariate test | ||||
|---|---|---|---|---|---|---|
| Mean | SEM | Mean | SEM | F (1, 716) | partial η2 | |
| mTSTa | 425.56 | 3.57 | 398.42 | 4.55 | 23.08** | .031 |
| mSOLa | 23.99 | 0.81 | 29.92 | 1.03 | 21.61** | .029 |
| mWASOa | 25.38 | 1.23 | 35.74 | 1.57 | 28.34** | .038 |
| mNWAKb | 1.46 | 0.05 | 1.83 | 0.07 | 18.39** | .025 |
| mSEc | 85.49 | 0.34 | 81.53 | 0.44 | 53.77** | .070 |
Average minutes for each sleep parameter.
Average number of awakenings.
Average percentage sleep efficiency.
p < .05,
p < .001.
3.2.3. Interaction of poor sleep by sleep complaint
At the univariate level, the interaction of poor sleep by sleep complaint was significant for only the outcomes of mSOL, mWASO, and mSE. Figure 2 provides a visualization of the significant interaction of poor sleep by sleep complaint on mSOL (1a), mWASO (1b), and mSE (1c). Table 5 provides results of univariate analysis of the interaction of poor sleep by sleep complaint on mean-level sleep. To further explore the significant interaction present for mSOL, mWASO, and mSE, simple effects analyses were performed. Results of these analyses are presented in the following subsections (3.2.4 – 3.2.7). First, we compared complaining versus noncomplaining sleepers within each quantitative sleep group (poor and good sleep). Then, we compared good and poor sleepers within each sleep complaint group (complaining versus noncomplaining). Differences between good and poor sleepers within each complaint subgroup were expected since poor sleep was based on mean-level quantitative cut-offs for the parameters of SOL and WASO.
Figure 2.
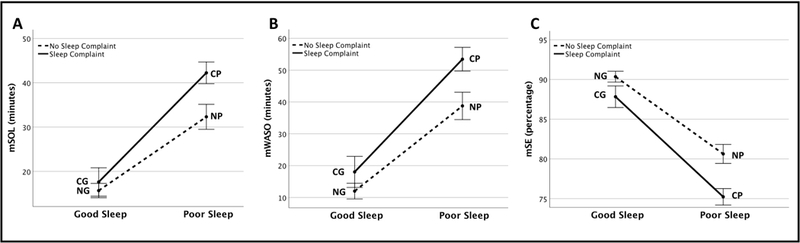
Interaction (adjusted mean ± SEM) of sleep complaint and poor sleep on (a) mSOL, (b) mWASO, and (c) mSE.
Table 5.
Adjusted means, standard error, and univariate statistics for interaction of poor sleep by sleep complaint on mean-level sleep (N = 723).
| Good Sleep | Poor Sleep | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No Complaint (n = 384) |
Complaint (n = 84) |
No Complaint (n = 105) |
Complaint (n = 150) |
Univariate test of poor
sleep x complaint |
||||||
| Mean | SEM | Mean | SEM | Mean | SEM | Mean | SEM | F (1, 716) | partial η2 | |
| mTSTa | 433.70 | 3.58 | 416.02 | 7.09 | 417.42 | 6.25 | 380.82 | 5.41 | 2.82 | .004 |
| mSOLa | 15.66 | 0.81 | 17.60 | 1.60 | 32.32 | 1.41 | 42.25 | 1.22 | 9.89** | .014 |
| mWASOa | 12.00 | 1.23 | 18.02 | 2.44 | 38.77 | 2.15 | 53.45 | 1.86 | 4.99* | .007 |
| mNWAKb | 1.14 | 0.05 | 1.61 | 0.11 | 1.78 | 0.10 | 2.05 | 0.08 | 1.45 | .002 |
| mSEc | 90.35 | 0.34 | 87.83 | 0.68 | 80.63 | 0.60 | 75.23 | 0.52 | 7.12** | .010 |
Average minutes for each sleep parameter.
Average number of awakenings.
Average percentage sleep efficiency.
p < .05,
p < .01.
3.2.4. Complaining versus noncomplaining poor sleepers (CP vs NP).
CP exhibited significantly greater mSOL and mWASO than NP [F(1, 716) = 28.5, p < .001 and F(1, 716) = 26.8, p < .001, respectively]. CP also exhibited significantly lesser mSE than NP [F(1, 716) =47.1, p < .001].
3.2.5. Complaining versus noncomplaining good sleepers (CG vs NG).
CG had significantly greater mWASO [F(1, 716) = 5.1, p < .05] and lesser mSE [F(1, 716) = 11.7, p < .01] compared to NG. CG and NG did not significantly differ on mSOL [F(1, 716) = 1.2, p = .27].
3.2.6. Good versus poor complaining sleepers (CG vs CP).
CP exhibited significantly greater mSOL and mWASO compared to CG [F(1, 716) = 156.1, p < .001 and F(1, 716) = 138.8, p < .001, respectively]. CP also exhibited significantly lesser mSE than CG [F(1, 716) = 227.4, p < .001].
3.2.7. Good versus poor noncomplaining sleepers (NG vs NP).
NP displayed significantly greater mSOL and mWASO than NG [F(1, 716) = 103.1, p < .001 and F(1, 716) = 114.7, p < .001, respectively]. NP also exhibited significantly lesser mSE than NG [F(1, 716) = 196.1, p < .001].
3.3. Differences in Sleep IIV by Sleep Complaint and Poor Sleep
A 2×2 MANCOVA with sleep complaint crossed with poor sleep was conducted to assess sleep subgroup differences on five dependent measure of sleep IIV: iSD TST, iSD WASO, iSD NWAK, iSD SOL, iSD SE. After controlling for age, race, and gender, multivariate analysis revealed significant main effects of poor sleep [Wilks’ Λ = .77, F (5, 712) = 42.2, p < .001, partial η2 = .229] and sleep complaint [Wilks’ Λ = .96, F (5, 712) = 5.7, p < .001, partial η2 = .039], as well as the interaction of poor sleep by sleep complaint [Wilks’ Λ = .98, F (5, 712) = 2.6, p < .05, partial η2 = .018].
3.3.1. Main effect of poor sleep.
Univariate testing indicated that the main effect of poor sleep was significant for each of the five dependent variables under investigation (iSD TST, iSD SOL, iSD WASO, iSD NWAK, and iSD SE). Individuals with poor sleep exhibited significantly greater night-to-night variability across all sleep parameters compared to individuals with good sleep. Results of univariate analyses for the main effect of poor sleep on sleep IIV are presented in Table 6.
Table 6.
Adjusted means, standard error, and univariate statistics for main effect of poor sleep of sleep IIV (N = 723).
| Good Sleep (n = 468) |
Poor Sleep (n = 255) |
Univariate test | ||||
|---|---|---|---|---|---|---|
| Mean | SEM | Mean | SEM | F (1, 716) | partial η2 | |
| iSD TSTa | 68.27 | 2.04 | 83.85 | 2.08 | 29.54** | .040 |
| iSD SOLa | 9.92 | 0.98 | 23.28 | 1.00 | 94.57** | .117 |
| iSD WASOa | 15.58 | 1.09 | 33.67 | 1.11 | 139.96** | .164 |
| iSD NWAKb | 0.81 | 0.03 | 0.99 | 0.03 | 19.05** | .026 |
| iSD SEc | 6.08 | 0.27 | 10.40 | 0.27 | 131.35** | .155 |
Average night-to-night variation of number of minutes for given sleep parameter.
Average night-to-night variation of number of awakenings.
Average night-to-night variation in percentage points of sleep efficiency.
p < .05,
p < .001.
3.3.2. Main effect of sleep complaint.
Univariate testing indicated that the main effect of sleep complaint was significant for the dependent variables of iSD TST, iSD SOL, iSD WASO, and iSD SE. Individuals with a sleep complaint exhibited greater night-to-night variability compared to individuals with no sleep complaint. The main effect of sleep complaint was not significant for iSD NWAK. Results of univariate analyses for the main effect of sleep complaint on sleep IIV are presented in Table 7.
Table 7.
Adjusted means, standard error, and univariate statistics for main effect of sleep complaint on sleep IIV (N = 723).
| No Complaint (n = 489) |
Complaint (n = 234) |
Univariate test | ||||
|---|---|---|---|---|---|---|
| Mean | SEM | Mean | SEM | F (1, 716) | partial η2 | |
| iSD TSTa | 71.91 | 1.79 | 80.21 | 2.28 | 8.62** | .012 |
| iSD SOLa | 14.90 | 0.86 | 18.31 | 1.09 | 6.31* | .009 |
| iSD WASOa | 21.75 | 0.95 | 27.49 | 1.22 | 14.48** | .020 |
| iSD NWAKb | 0.87 | 0.03 | 0.92 | 0.03 | 1.53 | .002 |
| iSD SEc | 7.24 | 0.24 | 9.24 | 0.30 | 28.63** | .038 |
Average night-to-night variation of number of minutes for given sleep parameter.
Average night-to-night variation of number of awakenings.
Average night-to-night variation in percentage points of sleep efficiency.
p < .05,
p < .01.
3.3.3. Interaction of poor sleep by sleep complaint.
At the univariate level, the interaction of poor sleep by sleep complaint was significant for only the outcomes of iSD SOL and iSD NWAK. Figure 3 provides a visualization of the interaction of sleep complaint and poor sleep for iSD SOL (2a) and iSD NWAK (2b). Table 8 provides results of univariate analyses of the interaction of poor sleep by sleep complaint on sleep IIV. To further explore the interaction present for iSD SOL and iSD NWAK, simple effects analyses were performed. Results of these analyses are presented in the subsequent subsections (3.3.4 – 3.3.7). First, we compared complaining versus noncomplaining sleepers within each quantitative sleep group (poor and good sleep). Then, we compared good and poor sleepers within each sleep complaint group (complaining versus noncomplaining).
Figure 3.
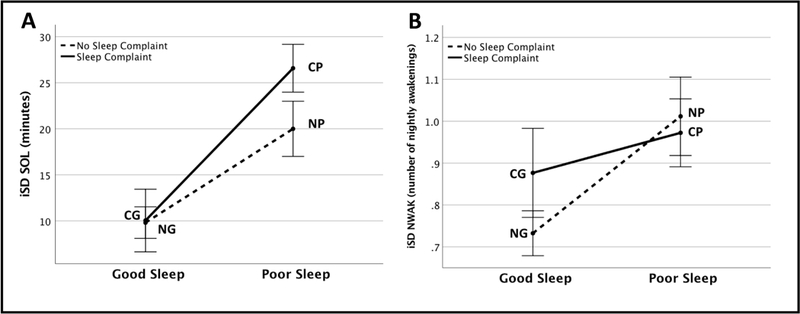
Interaction (adjusted mean ± SEM) of sleep complaint and poor sleep on (a) iSD SOL and (b) iSD NWAK.
Table 8.
Adjusted means, standard error, and univariate statistics for interaction of poor sleep by sleep complaint on sleep IIV (N = 723).
| Good Sleep | Poor Sleep | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No Complaint (n = 384) |
Complaint (n = 84) |
No Complaint (n = 105) |
Complaint (n = 150) |
Univariate test of poor
sleep x complaint |
||||||
| Mean | SEM | Mean | SEM | Mean | SEM | Mean | SEM | F (1, 716) | partial η2 | |
| iSD TSTa | 63.71 | 1.79 | 72.83 | 3.55 | 80.11 | 3.13 | 87.59 | 2.71 | 0.08 | .000 |
| iSD SOLa | 9.81 | 0.86 | 10.04 | 1.70 | 19.99 | 1.50 | 26.57 | 1.30 | 5.53* | .008 |
| iSD WASOa | 12.67 | 0.96 | 18.48 | 1.89 | 30.83 | 1.67 | 36.50 | 1.44 | 0.00 | .000 |
| iSD NWAKb | 0.73 | 0.03 | 0.88 | 0.05 | 1.01 | 0.05 | 0.97 | 0.04 | 4.74* | .007 |
| iSD SEc | 5.24 | 0.24 | 6.91 | 0.47 | 9.25 | 0.41 | 11.56 | 0.36 | 0.74 | .001 |
Average night-to-night variation of number of minutes for given sleep parameter.
Average night-to-night variation of number of awakenings.
Average night-to-night variation in percentage points of sleep efficiency.
p < .05,
p < .01.
3.3.4. Complaining versus noncomplaining poor sleepers (CP vs NP).
CP exhibited significantly greater iSD SOL compared to NP [F (1, 716) = 11.1, p < .01]. CP did not differ significantly from NP on iSD NWAK [F (1, 716) = 0.4, p = .52].
3.3.5. Complaining versus noncomplaining good sleepers (CG vs NG).
CG exhibited significantly greater iSD NWAK compared to NG [F (1, 716) = 6.2, p < .05]. CG and NG did not significantly differ from one another on iSD SOL [F (1, 716) = .02, p = .90].
3.3.6. Good versus poor complaining sleepers (CG vs CP).
CP exhibited greater iSD SOL compared to CG [F (1, 716) = 62.3, p < .001]. CP did not differ significantly from CG on iSD NWAK [F (1, 716) = 2.1, p = .14].
3.3.7. Good versus poor noncomplaining sleepers (NG vs NP)
NP exhibited significantly greater iSD SOL and iSD NWAK than NG [F (1, 716) = 34.2, p < .001 and F (1, 716) = 26.3, p < .001, respectively].
4. Discussion
The present study sought to explore sleep IIV as a commonly obscured factor contributing to the discordance often documented between sleep and sleep appraisal. Toward this aim, our findings are the first to demonstrate that IIV in certain sleep parameters may differentially contribute to negative sleep appraisal among good sleepers as well as poor sleepers (as defined based on quantitative criteria established by Lichstein et al., 2003). Specifically, night-to-night variation in SOL emerged as the only sleep IIV variable that significantly differed between complaining and noncomplaining sleepers within the poor sleep subgroup. This observation suggests that night-to-night variability in SOL may be a particularly salient factor in differentiating whether a poor sleeper adopts an insomnia identity and experiences subsequent distress related to disturbed sleep. IIV in NWAK was found to significantly differ between complaining and noncomplaining good sleepers. Furthermore, complaining good sleepers’ IIV in NWAK did not differ significantly from that of complaining poor sleepers. These findings suggest that night-to-night variability in sleep fragmentation may be an important factor driving sleep dissatisfaction among sleepers who exhibit otherwise good mean-level sleep. Treatment aimed at decreasing night-to-night variability in this sleep parameter may be one method of reducing negative sleep appraisal among individuals with quantitatively good sleep.
In the present study, poor sleepers exhibited significantly greater night-to-night variability in sleep across each of the sleep parameters investigated (iSD TST, iSD SOL, iSD WASO, iSD NWAK, and iSD SE). This finding coincides with extant research literature supporting greater night-to-night variability as a characteristic factor of insomnia. When compared to good sleepers, individuals with insomnia symptoms and poor sleep exhibited greater IIV on sleep parameters, including TST (Okun et al., 2011; Buysse et al., 2010), SOL (Buysse et al., 2010; Fichten et al., 2005; Vanderlind et al., 2014), SE (Buysse et al., 2010), and WASO (Buysse et al., 2010, Fichten et al., 2005). Based on the observation of greater IIV among poor sleepers, it has been posited that inconsistent sleep patterns may be a mechanism through which insomnia is precipitated and sustained. After a night of poor sleep, individuals may engage in maladaptive behavioral changes during the day to compensate for increased daytime impairment (i.e., taking naps, limiting activity) or during the night to “catch up” via sleeping longer. These behaviors represent a reactive approach to poor sleep that may have the unintended result of undermining the ability to initiate sleep the following night, thereby promoting a cycle of sleep inconsistency, poor sleep, and negative long-term sleep appraisals. Fortunately, a few studies of cognitive behavioral therapy for insomnia have shown that treatment produces significant reductions in IIV for the sleep diary variables of TST, SE, SOL, and WASO (Buysse et al., 2010; Edinger, Hoelscher, Marsh, Lipper, & Ionescu-Pioggia, 1992; Espie, Lindsay, Brooks, Hood, & Turvey, 1989; Sánchez-Ortuño & Edinger, 2012; Suh et al., 2012). Collectively, these findings suggest that night-to-night variability in sleep may be an important factor contributing to insomnia symptomatology, and this variability can be successfully targeted via existing interventions for insomnia. Future clinical trials assessing insomnia treatment could more thoroughly characterize the nature of treatment effects by including sleep IIV as an outcome measure in addition to mean-level sleep parameters.
Insomnia identity has been related to worse daytime functioning outcomes even after controlling for the influence of mean-level sleep parameters (Ustinov et al., 2010), signifying that there exist other unexplored or overlooked factors contributing to overall sleep wellbeing. This study is among the first to examine how night-to-night variability in several sleep parameters differs according to the presence of a sleep complaint independent of quantitative sleep status. Individuals endorsing a sleep complaint exhibited significantly greater night-to- night variability across sleep parameters of TST, SOL, WASO, and SE regardless of diary- assessed quantitative sleep status. The results of this study coincide with previous research, which has shown that greater night-to-night variability in sleep duration is related to poor subjective sleep quality as well as poor subjective wellbeing (Lemola et al., 2013). For both poor and good sleepers, greater inconsistency or irregularity in sleep from night-to-night may contribute to one’s perception of poor sleep and subsequent adoption of an insomnia identity. These findings point to sleep IIV as a potentially influential treatment target and outcome measure in clinical settings serving individuals presenting with sleep complaints regardless of whether they also exhibit corresponding disturbances in sleep.
Although sleep IIV tends to correlate with mean-level sleep (Bei et al., 2016; Dillon et al., 2015), sleep IIV quantifies the stability of sleep from night-to-night, thereby providing a more comprehensive representation of an individual’s sleep that may otherwise be obscured by mean-level analysis alone. Rather than being redundant with aggregate measures of sleep, sleep variability has been shown to confer its own unique influence on sleep quality and health outcomes independent of mean-level sleep (Bei et al., 2016). For example, greater IIV in TST has been associated with higher risk for physical health conditions and obesity after controlling for mean TST (Patel et al., 2014). Similarly, in a study of napping behavior conducted among community-dwelling older adults, daily variability in nap duration predicted medical morbidity whereas average nap duration did not (Dautovich et al., 2012). The utility of sleep IIV as a metric is particularly evident in scenarios in which mean-level sleep fails to sufficiently account for observed differences among sleep groups. For example, variability of diary-derived sleep parameters - but not conventional mean-level estimates of sleep - has been shown to differ between primary insomnia patients and comorbid insomnia patients, which helps clarify the mechanisms underlying the sleep complaint and treatment response in these two distinct patient groups (Edinger et al., 2009; Kohn and Espie, 2005; Sánchez-Ortuño & Edinger, 2012). Similarly, while several studies have demonstrated that variations in sleep constitute an important clinical feature of insomnia, this study aimed to identify characteristics of sleep variability that may underlie the discordance commonly observed between mean-level quantitative sleep and sleep appraisal.
The quantitative definition of poor sleep utilized in this study required SOL or WASO totaling 31 or more minutes at least three nights per week. This set of quantitative criteria represents one of many that have been proposed over the years (Beattie, Espie, Kyle, & Biello, 2015; Lichstein et al., 2003; Lineberger, Carney, Edinger, & Means, 2006; Natale et al., 2015). Although the current lack of consensus regarding quantitative criteria for poor sleep and insomnia represents a limitation of the current research and similar studies, the criteria utilized in the present study have been established as among the most commonly used and defensible of quantitative criteria for accurately identifying poor sleep (Lichstein et al., 2003; Schutte-Rodin et al., 2008). Among the epidemiological sample utilized in the current study, the selected severity criterion (≥ 31 minutes WASO and/or SOL) has been shown to maximize sensitivity and specificity between self-defined insomnia status and quantitative classification of insomnia. Nonetheless, it is important to acknowledge that when utilizing these criteria there still existed salient differences in mean-level sleep between complaining and noncomplaining individuals within good and poor sleep subgroups of the current study. Subjective estimates of sleep quantity (as provided in sleep diaries) have been previously shown to meaningfully differentiate between complaining and noncomplaining good sleepers but not poor sleepers in a sample of older adults (McCrae et al., 2005). Consistent with these findings, the present study revealed that mean-level sleep diary estimates of WASO and SE differed significantly between CG and NG subgroups. This finding suggests that increased time spent awake during a sleep bout, in particular, may be an important factor contributing to sleep-related distress among good sleepers. Mean-level SOL, WASO, and SE were also found to differ between CP and NP subgroups in the present study. Further research is needed to better understand how quantitative sleep parameters interact with psychosocial characteristics of the sleeper to influence sleep perception and distress. For example, relatively small differences in mean-level sleep parameters may be consequential when paired with cognitive biases characteristic of a complaining sleep group.
Several limitations of the present study warrant acknowledgement. Basing participants’ quantitative sleep status on self-report diaries introduces the likelihood of subjective bias. Future studies comparing diary-derived sleep IIV estimates with an objective measure of sleep (via polysomnography or actigraphy) would help determine if there exist differences in actual versus perceived night-to-night variability in sleep. Another limitation of the current study is mathematical in nature. In comparing poor and good sleep subgroups, it is possible that the utilized method of categorizing these sleep subgroups may have imposed an artificial ceiling/floor effect on sleep IIV among good sleepers. Nonetheless, this limitation would not influence the central comparisons made between complaining versus noncomplaining sleepers within good and poor sleep groups. Lastly, the current study relied on a relatively simplistic measure of sleep complaint that, while useful and convenient, fails to account for the likely existence of a continuum of sleep dissatisfaction and insomnia identity. Future analyses may benefit from more nuanced examination of the ways in which specific sleep symptoms and their severity influence (1) the discordance observed between sleep and sleep appraisal and (2) the impact of this discordance on related measures of daytime impairment.
The present study demonstrated that night-to-night variability in certain sleep parameters may be a meaningful factor differentially contributing to insomnia identity among good and poor sleepers, thereby suggesting a potential mechanism contributing to the discordance often documented between quantitative sleep and sleep appraisal. This study also illustrates the importance of examining quantitative sleep beyond mean-level parameters to achieve a more comprehensive view of overall sleep patterns and the influence of these patterns on sleep appraisal. These findings aim to inform which aspects of sleep and sleep consistency may be salient for treatment-seeking individuals based on their quantitative sleep status. Sleep IIV should be further investigated as a potentially useful clinical metric and novel treatment target among individuals who endorse a sleep complaint but do not exhibit corresponding dysfunction on aggregate measures of sleep. Future studies are needed to more fully clarify how sleep IIV influences negative sleep appraisal and insomnia identity, especially among CG whose complaint is uncoupled from their sleep status.
Highlights.
Insomnia identity - the belief that one has insomnia - can occur despite good sleep
Night-to-night variability in sleep may contribute to insomnia identity
For poor sleepers, complainers had more variable sleep latency than noncomplainers
For good sleepers, complainers had more variable awakenings than noncomplainers
Sleep consistency may be an important intervention target for insomnia identity
Acknowledgements:
Not Applicable.
Funding: This research was supported by the National Institute on Aging grants #AG12136 and #AG14738.
Abbreviations
- CG
Complaining Good Sleepers
- CP
Complaining Poor Sleepers
- IIV
Intraindividual Variability
- iSD
Intraindividual Standard Deviation
- MANCOVA
Multivariate Analysis of Covariance
- NG
Noncomplaining Good Sleepers
- NP
Noncomplaining Poor Sleepers
- NWAK
Number of Nightly Awakenings
- SE
Sleep Efficiency
- SEM
Standard Error of the Mean
- SOL
Sleep Onset Latency
- TIB
Time in Bed
- TST
Total Sleep Time
- TWAK
Terminal Wake Time
- WASO
Wake After Sleep Onset
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None
References
- Alapin I, Fichten CS, Libman W, Creti L, Bailes S, & Wright J (2000). How is good and poor sleep in older adults and college students related to daytime sleepiness, fatigue, and ability to concentrate? Journal of Psychosomatic Research, 49, 381 – 90. [DOI] [PubMed] [Google Scholar]
- American Academy of Sleep Medicine. (2014). International classification of sleep disorders (2nd ed.). Westchester, NY: American Academy of Sleep Medicine. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Beattie L Espie CA, Kyle SD, & Biello SM (2015). How are normal sleeping controls selected? A systematic review of cross-sectional insomnia studies and a standardized method to select healthy controls for sleep research. Sleep Medicine, 16, 669 – 77. [DOI] [PubMed] [Google Scholar]
- Bei B, Wiley JF, Trinder J, & Manber R (2016). Beyond the mean: A systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep Medicine Reviews, 28, 108 – 24. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Cheng Y, Germain A, Moul DE, Franzen PL, Fletcher M, & Monk TH (2010). Night-to-night sleep variability in older adults with and without chronic insomnia. Sleep Medicine, 11, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dautovich ND, Kay DB, Perlis ML, Dzierzewski JM, Rowe MA, & McCrae CS (2012). Day-to-day variability in nap duration predicts medical morbidity in older adults. Health Psychology, 31, 671 – 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon HR, Lichstein KL, Dautovich ND, Taylor DJ, Riedel BW, & Bush AJ (2015). Variability in self-reported normal sleep across the adult age span. The Journals of Gerontology, Series B, Psychological Sciences and Social Sciences, 70, 46 – 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinger JD, Fins AI, Glenn DM, Sullivan RJ Jr., Bastian LA, Marsh GR, ... Vasilas D (2000). Insomnia and the eye of the beholder: Are there clinical markers of objective sleep disturbances among adults with and without insomnia complaints? Journal of Consulting and Clinical Psychology, 68, 586 – 93. [PubMed] [Google Scholar]
- Edinger JD, Hoelscher TJ, Marsh GR, Lipper S, & Ionescu-Pioggia MA (1992). A cognitive-behavioral therapy for sleep maintenance insomnia in older adults. Psychology and Aging, 7, 282 – 9. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Olsen MK, Stechuchak KM, Means MK, Lineberger MD, Kirby A, & Carney CE (2009). Cognitive behavioral therapy for patients with primary insomnia or insomnia associated predominantly with mixed psychiatric disorders: a randomized clinical trial. Sleep, 32, 499 – 510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espie CA, Lindsay WR, Brooks DN, Hood EM, & Turvey TA (1989). A controlled comparative investigation of psychological treatments for chronic sleep-onset insomnia. Behaviour Research and Therapy, 27, 79 – 88. [DOI] [PubMed] [Google Scholar]
- Fichten CS, Creti L, Amsel R, Bailes S, & Libman E (2005). Time estimation in good and poor sleepers. Journal of Behavioral Medicine, 28, 537 – 53. [DOI] [PubMed] [Google Scholar]
- Fichten CS, Creti L, Amsel R, Brender W, Weinstein N, & Libman E (1995). Poor sleepers who do not complain of insomnia: Myths and realities about psychological and lifestyle characteristics of older good and poor sleepers. Journal of Behavioral Medicine, 18, 189 – 223. [DOI] [PubMed] [Google Scholar]
- Field AP (2009). Discovering statistics using SPSS. London, England: : SAGE. [Google Scholar]
- Kohn L & Espie CA (2005). Sensitivity and specificity measures of the insomnia experience: A comparative study of psychophysiologic insomnia, insomnia associated with mental disorder, and good sleepers. Sleep, 28, 104 – 12. [DOI] [PubMed] [Google Scholar]
- Knutson KL, Rathouz PJ, Yan LL, Liu K, & Lauderdale DS (2007). Intra-individual daily and yearly variability in actigraphically recorded sleep measures: The CARDIA study. Sleep, 30, 793–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemola S, Ledermann T, & Friedman EM (2013). Variability of sleep duration is related to subjective sleep quality and subjective well-being: An actigraphy study. PLoS ONE, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichstein KL (2017). Insomnia identity. Behaviour Research and Therapy, 97, 230 – 41. [DOI] [PubMed] [Google Scholar]
- Lichstein KL, Durrence HH, Riedel BW, Taylor DJ, & Bush AJ (2004).Epidemiology of sleep: Age, gender, and ethnicity. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Lichstein KL, Durrence HH, Taylor DJ, & Bush AJ, Riedel BW (2003).Quantitative criteria for insomnia. Behaviour Research and Therapy, 41, 427 – 55. [DOI] [PubMed] [Google Scholar]
- Lineberger MD, Carney CE, Edinger JD, & Means MK (2006). Defining insomnia: Quantitative criteria for insomnia severity and frequency. Sleep, 29, 479 – 85. [DOI] [PubMed] [Google Scholar]
- McCrae CS, Rowe MA, Tierney CG, Dautovich ND, Definis AL, & McNamara JP (2005). Sleep complaints, subjective and objective sleep patterns, health, psychological adjustment, and daytime functioning in community-dwelling older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 60, 182 – 89. [DOI] [PubMed] [Google Scholar]
- McCrae CS, Wilson NW, Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, & Riedel BW (2003). ‘Young old’ and ‘old old’ poor sleepers with and without insomnia complaints. Journal of Psychosomatic Research, 54, 11 – 19. [DOI] [PubMed] [Google Scholar]
- Natale V, Léger D, Bayon V, Erbacci A, Tonetti L, Fabbri M, & Martoni M (2015). The consensus sleep diary: Quantitative criteria for primary insomnia diagnosis. Psychomatic Medicine, 77, 413 – 8. [DOI] [PubMed] [Google Scholar]
- Okun ML, Reynolds CF, Buysse DJ, Monk TH, Mazumdar S, Begley A, & Hall M (2011).Sleep variability, health-related practices and inflammatory markers in a community dwelling sample of older adults. Psychosomatic Medicine, 73, 142 – 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Hayes AL, Blackwell T, Evans DS, Ancoli-Israel S, Wing YK, Stone KL, Osteoporotic Fractures in Men (MrOS), Study of Osteoporotic Fractures Research Groups. (2014). The association between sleep patterns and obesity in older adults. International Journal of Obesity, 38, 1159 – 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez-Ortuño MM, & Edinger JD (2012). Internight sleep variability: Its clinical significance and responsiveness to treatment in primary and comorbid insomnia. Journal of Sleep Research, 21, 527 – 34. [DOI] [PubMed] [Google Scholar]
- Schutte-Rodin S, Broch L, Buysse D, Dorsey C, & Sateia M (2008). Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine, 4, 487 – 504. [PMC free article] [PubMed] [Google Scholar]
- Suh S, Nowakowski S, Bernert RA, Ong JC, Siebern AT, Dowdle CL, & Manber R (2012).Clinical significance of night-to-night sleep variability in insomnia. Sleep Medicine, 13, 469–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ustinov Y, Lichstein KL, Vander Wal GS, Taylor DJ, Riedel BW, & Bush AJ (2010). Association between report of insomnia and daytime functioning. Sleep Medicine, 11, 65 – 8. [DOI] [PubMed] [Google Scholar]
- Vanderlind WM, Beevers CG, Sherman SM, Trujillo LT, McGeary JE, Matthews MD, Maddox WT, & Schnyer DM (2014). Sleep and sadness: exploring the relation among sleep, cognitive control, and depressive symptoms in young adults. Sleep Medicine, 15, 144–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohlgemuth WK, Edinger JD, Fins AI, & Sullivan RJ (1999). How many nights are enough? The short-term stability of sleep parameters in elderly insomniacs and normal sleepers. Psychophysiology, 36, 233 – 44. [PubMed] [Google Scholar]
- Woosley JA, Lichstein KL, Taylor DJ, Riedel BW, & Bush AJ (2016). Insomnia complaint versus sleep diary parameters: Predictions of suicidal ideation. Suicide and Life Threatening Behavior, 46, 88 – 95. [DOI] [PubMed] [Google Scholar]


