Abstract
Emerging CVD risk factors (e.g. HDL function and central haemodynamics) may account for residual CVD risk experienced by individuals who meet LDL-cholesterol and blood pressure (BP) targets. Recent evidence suggests that these emerging risk factors can be modified by polyphenol-rich interventions such as soya, but additional research is needed. This study was designed to investigate the effects of an isoflavone-containing soya protein isolate (delivering 25 and 50g/d soya protein) on HDL function (i.e. ex vivo cholesterol efflux), macrovascular function and blood markers of CVD risk. Middle-aged adults (n 20; mean age = 51.6 (SEM 6.6) years) with moderately elevated brachial BP (mean systolic BP = 129 (SEM 9) mmHg; mean diastolic BP = 82.5 (SEM 8.4)mmHg) consumed 0 (control), 25 and 50g/d soya protein in a randomised cross-over design. Soya and control powders were consumed for 6 weeks each with a 2-week compliance break between treatment periods. Blood samples and vascular function measures were obtained at baseline and following each supplementation period. Supplementation with 50 g/d soya protein significantly reduced brachial diastolic BP (−2.3 mmHg) compared with 25 g/d soya protein (Tukey-adjusted P = 0.03) but not the control. Soya supplementation did not improve ex vivo cholesterol efflux, macrovascular function or other blood markers of CVD risk compared with the carbohydrate-matched control. Additional research is needed to clarify whether effects on these CVD risk factors depend on the relative health of participants and/or equol producing capacity.
Keywords: HDL function, Central blood pressure, Arterial stiffness, Augmentation index
Assessment of emerging CVD risk factors may improve risk prediction and treatment strategies as many individuals continue to experience residual CVD risk despite meeting current LDL-cholesterol and blood pressure targets. For instance, HDL functionality (i.e. cholesterol efflux) has recently been proposed as a more informative marker of CVD risk than HDL-cholesterol(1,2) due to the lack of benefit on hard endpoints in trials of pharmacological HDL-cholesterol raising agents(3–5). Similarly, central blood pressure and related indices of arterial stiffness have been shown to better predict cardiovascular events(6) and are more sensitive predictors of disease severity(7) compared with brachial pressures. Plant-based whole foods are recommended for reducing CVD risk(8) but it has yet to be conclusively established whether cholesterol efflux and/or macrovascular function can be modified by polyphenol-rich plant-based foods/beverages.
Previous studies have demonstrated promising results for these outcomes with certain interventions (e.g. berries, red wine and cocoa), but evidence is limited. For instance, ex vivo cholesterol efflux has been shown to increase following supplementation with extra virgin olive oil(9) and coffee(10), as well as resveratrol(11) and anthocyanins(12), which are found in red wine and berries. However, other studies have produced mixed results(13) and other polyphenol-rich interventions have yet to be investigated. Improvements in central blood pressure and other measures of macrovascular function have also been found following supplementation with polyphenol-rich berries(14,15), grapefruit(16), watermelon(17,18) and isoflavone-enriched chocolate(19), but results have been inconsistent for other interventions(20–23). In addition, many of these findings were specific to postmenopausal women(16,17,19) or normotensive individuals(14,20–23).
Soyabeans provide plant protein as well as numerous polyphenols and other bioactive compounds, including isoflavones(24,25). Consuming 25 g/d soya protein (as part of a diet low in saturated fat and cholesterol) may reduce the risk of heart disease by lowering blood cholesterol(26), and epidemiological evidence suggests that greater soya protein intake may be related to reduced CVD risk(27,28), particularly in postmenopausal women(29). However, much less is known about the effects of soya on cholesterol efflux and macrovasculature function. Notably, many previous studies have been limited to isolated soya isoflavones, despite pre-clinical evidence that cardiovascular benefits may only be achieved when isoflavones are administered in conjunction with soya protein(30–34) With regard to HDL function, to our knowledge no studies have been conducted using a soya protein isolate with naturally occurring isoflavones. Supplementation with isolated soya isoflavones did not elicit any change in ex vivo cholesterol efflux in postmenopausal women following 3 months of supplementation(33,34). Initial evidence for the effect of soya isoflavones on macrovascular function has been promising(35,36); however, few studies have investigated soya protein with endogenous isoflavones and results have been inconsistent(37–39). Furthermore, no studies have evaluated potential dose-response effects of an isoflavone-containing soya protein isolate on these risk factors.
The present study was designed to investigate the dose- response effects of a soya protein isolate (delivering 25 and 50g/d soya protein) containing endogenous isoflavones on HDL function (i.e. ex vivo cholesterol efflux), central blood pressure, indices of arterial stiffness and other blood markers of CVD risk in adults with moderately elevated resting blood pressure. Our primary hypothesis was that supplementation with an isoflavone-containing soya protein isolate would increase ex vivo cholesterol efflux compared with the placebo control. In addition, we hypothesised that soya supplementation would improve vascular function, indices of arterial stiffness, and blood markers of CVD risk in a dose-dependent manner relative to the control.
Methods
Study population
Men and women who were 35–60 years of age, had moderately elevated resting blood pressure (systolic blood pressure ≥120 mmHg and/or diastolic blood pressure ≥80 mmHg and <160/100 mmHg), and were otherwise free of any serious illness were recruited for the study. Other inclusion criteria consisted of: following a typical American diet (i.e. not vegetarian, not engaged in a structured diet plan or attempting to lose weight, and not frequently consuming soya products), BMI of 18–39 kg/m2, fasting TAG <3 95mmol/l, and fasting LDL-cholesterol <4 14mmol/l. Exclusion criteria included: smoking and/or use of other tobacco products; a history of diabetes, autoimmune disorders, and heart, liver, kidney or thyroid disease; pregnancy, lactation or a desire to become pregnant during the study; chronic use of non-steroidal anti-inflammatories or medications/supplements for elevated lipids, blood pressure or glucose; lactose intolerance; and excessive alcohol consumption (>14 standard drinks per week).
Participant recruitment
Participants were recruited from March 2014 to June 2015 via fliers in the community, campus email lists and a university research website. Potential subjects emailed or called to indicate interest in participating in the study and were then given additional information about the study. If interested, they were asked a series of medical history and lifestyle questions to screen for eligibility. A schematic of participant recruitment for the study is provided in Fig. 1. Of the 170 initial respondents who provided contact information, 149 elected to complete the initial screening questions by telephone. In all, forty-eight of these volunteers met study criteria and completed a screening appointment at the Pennsylvania State University Clinical Research Center (CRC) to verify eligibility. After written informed consent was obtained, a urine pregnancy test was performed for women of child-bearing potential, and blood pressure was measured according to JNC 7 guidelines(40). In brief, after a 5-min seated rest, three readings were taken by nurses in a controlled environment using a calibrated mercury sphygmomanometer. The average of the last two readings was used to determine eligibility. If an individual’s blood pressure met the study inclusion criteria, body weight and height were measured (without shoes and in light clothing) to calculate BMI. A blood sample was then drawn for a complete blood count and standard chemistry profile (lipid panel, glucose, liver and kidney function) to rule out the presence of illness (autoimmune disease, cancer and immunodeficiency). Of the forty-eight individuals who were screened, twenty-three met eligibility criteria and were enrolled in the study. Three participants withdrew during the study. Thus, data are reported for twenty participants (nine men, eleven women). The screening characteristics of the twenty participants who completed the study are available in the online Supplementary Table S1.
Fig. 1.
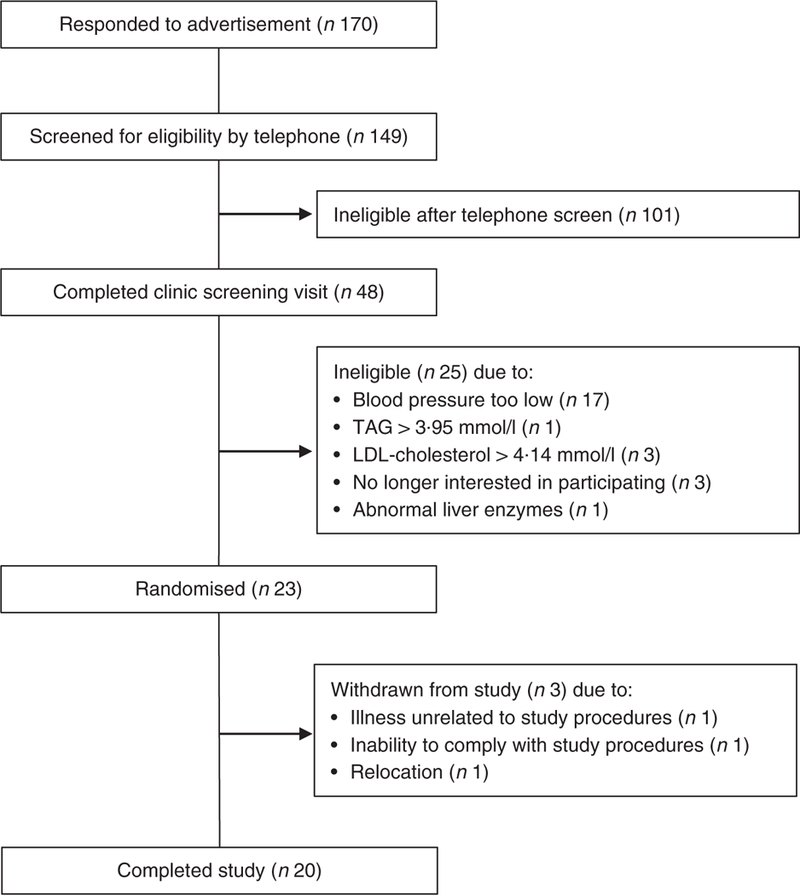
Flow diagram of participant recruitment. Soya protein, HDL function and blood pressure
A balanced randomisation scheme with a block size of six was developed in advance (by A. C. S.-R.) using an online randomisation generator, and subjects were assigned to a treatment sequence at enrolment (by C. J. L.). Sample size was determined based on a power calculation, with ex vivo cholesterol efflux as the primary outcome. In all, twenty participants were estimated to provide 80 % power to detect a 2 percentage point change in cholesterol efflux with a significance level of 0.05, based on the variability of cholesterol efflux values in our previous work(41). This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Board of the Pennsylvania State University. Written informed consent was obtained from all participants. The study was registered at https://clinicaltrials.gov as NCT02180841.
Study design and intervention
This was a randomised, placebo-controlled, three-period crossover study with 6-week treatment periods separated by an approximate 2-week compliance break. Treatment periods were extended by up to 2 weeks (8 weeks total) in the case of illness, injury or scheduling difficulties. During the treatment periods, participants received 50, 25 or 0g/d (control) soya protein delivered as an unfractionated soya protein isolate (isolate contained 87.4 % protein by total weight) that contained naturally occurring isoflavones, in random order. Treatments consisted of dry blended beverage powders provided as two identical sachets per day during all three periods. Treatments were matched to coded alphanumeric identifiers so that the researchers and participants were blinded to treatment assignment. The soya and control powders were formulated to be matched for carbohydrate and mineral (Na+, K+, Ca2+ and Mg2+) content, and differed mainly in the amount of soya protein provided (Table 1). The control beverage powders contained maltodextrin in place of the protein, and also contained approximately 1 % (w/w) total hydrocolloids (xanthan and carageenan; DuPont™ Danisco® Grinsted®) to provide a similar mouthfeel as the protein-containing beverages and maintain blinding. The soya protein isolate was prepared from defatted soyabean flakes by standard isoelectric precipitation, followed by partial protein hydrolysis with food enzymes and agglomeration for quicker dispersion into liquid. The soya protein isolate was analysed for isoflavone content by Nestlé Purina Analytical Laboratories and was determined to contain 1.7 mg of isoflavones (expressed as aglycone units) per g of protein, consisting of genistein, daidzein and glycitein (0.55:1.09:0.06 mg/g protein, respectively). All treatment powders were provided in individual sachets that were identical in appearance. Powders were also matched for taste and appearance to maintain the blinding of participants and researchers to treatment sequence. All study powders were formulated and provided by DuPont Nutrition and Health and analysed by Nestlé Purina Analytical Laboratories.
Table 1.
Nutrient profile of the control and isoflavone-containing soya protein supplements*
| 0 g/d soya protein (control) |
25 g/d soya protein |
50 g/d soya protein |
|
|---|---|---|---|
| Serving size (g) | 40 | 64 | 92 |
| Energy content (kJ) | 586 | 1004 | 1506 |
| Energy content (kcal) | 140 | 240 | 360 |
| Fat (g) | 2 | 2 | 4 |
| Protein (g) | 0 | 25 | 50 |
| Carbohydrate (g) | 34 | 30 | 30 |
| Na (mg) | 475 | 500 | 535 |
| K (mg) | 804 | 715 | 751 |
| Ca (mg) | 109 | 65 | 31 |
| Mg (mg) | 41 | 43 | 43 |
| Isoflavones (mg expressed as aglycone units) | 0 | 42.5 | 85 |
Values are based on analyses conducted on the final products by Nestlé Purina Analytical Laboratories and represent the averages of the vanilla and chocolate flavours that were provided for each treatment period.
Participants were instructed to consume two sachets per day during each treatment period by mixing the study powders with milk, water or food. They were provided with 1 week’s worth of treatment powders at a time. Participants were asked to incorporate the study powders into their habitual diet and maintain their normal dietary intake and physical activity. In addition, participants were instructed to avoid all other soya products for the duration of the study. A 3-d food record (2 weekdays and 1 weekend day) was completed at baseline and during the final week of each treatment period to confirm that dietary habits remained stable throughout the study and that soya-containing foods were avoided. Participants reported to the Metabolic Diet Center on a weekly basis. At this time, a member of the research team who was not involved in the statistical analyses provided participants with additional study powder and reviewed their body weight and treatment powder consumption logs.
Blood sampling and vascular testing was performed at baseline and following each 6-week supplementation period. All study procedures were conducted at the Pennsylvania State University CRC according to standardised protocols. During the 48 h before testing visits, participants were instructed to: avoid high antioxidant foods (berries, cocoa/chocolate), strenuous exercise and alcohol; refrain from taking pain relievers, vitamins or minerals; and limit their intake of coffee and tea to no more than one cup per day. Testing visits were conducted following an overnight fast (no food or drink other than water for 12 h). At each visit, vascular function testing was performed before blood sampling. All study procedures were completed by December 2015.
Vascular function measures
Vascular function, in terms of central blood pressure and arterial stiffness indices, was assessed using the SphygmoCor System pulse waveform analysis (AtCor Medical). All measurements were performed in a temperature-controlled, quiet, dimly lit room.
Pulse wave analysis: central (aortic) blood pressure and augmentation index.
Following a 5 min seated rest, central pressures and wave reflection characteristics (i.e. augmentation pressure and the augmentation index (AI)) were derived from brachial pressure waveforms using a generalised transfer function that is considered by the US Food and Drug Administration to be substantially equivalent to generalised transfer functions for radial tonometry that have been validated against an indwelling catheter(42–44). At each visit, three pulse wave analysis (PWA) measurements were taken, following JNC 7 blood pressure guidelines(40), with 1 min between each reading. The last two PWA results were averaged and used for analysis. The AI was standardised to a heart rate of 75 beats per min (AI@75) to correct for the independent inverse effect of heart rate on augmentation of the pulse wave form(45).
Pulse wave velocity.
Aortic stiffness was assessed by carotid-femoral pulse wave velocity (PWV). Carotid and femoral arterial pressure waveforms were measured simultaneously via an applanation tonometry sensor manually held in place above the right common carotid artery and a blood pressure cuff placed on the right femoral artery. Distance measurements were taken from the sternal notch to the carotid artery, from the sternal notch to the top of the femoral cuff, and from the femoral artery to the top of the femoral cuff. Based on these measurements, the SphygmoCor System automatically calculates the distance travelled by the pulse wave from the carotid artery to the femoral artery. Transit time between the carotid and femoral pressure waves is determined by the SphygmoCor System using the foot-to-foot method(46). PWV is then calculated as distance over transit time. At each visit, three PWV measurements were obtained in the supine position, with 1 min between readings. The last two PWV results were averaged for analysis.
Blood sample collection and assay methods
Blood drawn into anticoagulant-coated tubes containing lithium heparin or EDTA was immediately centrifuged for 15 min at 1500 g. Blood drawn into serum separator tubes was allowed to clot for 30 min before centrifugation. Total cholesterol and TAG were measured by enzymatic procedures (Quest Diagnostics; CV <2% for both). HDL-cholesterol was estimated according to the modified heparin-manganese procedure (Quest Diagnostics; CV <2 %). LDL-cholesterol was calculated using the Friedewald equation (LDL-cholesterol = total cholesterol −(HDL-cholesterol +TAG/5)). Glucose was determined by Spectrophotometry procedures (Quest Diagnostics). Insulin was measured by RIA using 125I-labelled human insulin and a human insulin antiserum (Quest Diagnostics). Serum high-sensitivity C-reactive protein (CRP) was measured by latex-enhanced immunonephelometry (Quest Diagnostics; assay CV <8 %). For other endpoints, aliquots of serum and plasma were immediately stored at −80°C for batch analysis.
Cholesterol efflux.
Cholesterol efflux capacity was quantified in serum samples using a validated ex vivo assay (Vascular Strategies LLC). J774 mouse macrophage cells were grown and maintained in Roswell Park Memorial Institute (RPMI) 1640 medium containing 10% fetal bovine serum (FBS) and 0.5% gentamycin and incubated at 37°C in a humidified incubator (95% air and 5% CO2). Cells were then plated in growth medium in 24-well tissue culture plates at a density of 150 000 cells/well for 24 h and grown to 80−90% confluence. Subsequently, cells were washed three times with HEPES-buffered minimum essential medium (MEM) and labelled with 2 μCi/ml [1,2-3H]cholesterol for 24 h in RPMI medium containing 5% FBS. After labelling, cells were washed with MEM−HEPES twice and RPMI 1640 medium containing 0.2% bovine serum albumin plus 0.3mM-8-(4-cholorophenyl-thio)-cyclic AMP was added to the cells for 16 h to up-regulate ATP-binding cassette transporter 1 (ABCA1). After ABCA1 up-regulation, cells were washed with MEM-HEPES, and efflux of [3H]free cholesterol (FC) was initiated by incubating the cells for 4h with 2.5% apoB-depleted serum from the study subjects. After the media was collected and filtered, 0.2 ml was used to calculate efflux by measuring the release of [3H]FC into the medium. Experiments were performed with the presence of acetyl-CoA acetyltransferase (ACAT) inhibitor, Sandoz 58–035 to ensure that essentially all of the labelled cholesterol and cholesterol mass was present as FC. Cholesterol efflux was quantified as the percentage of radiolabel in the media compared with that present in the cells before incubation with cholesterol acceptors. The amount of radiolabel present in the cells was determined by extracting cell lipids with isopropanol and measuring the [3H] cholesterol in the lipid extraction by liquid scintillation counting. Samples were analysed in triplicate, with a mean CV <5 %.
Statistical analyses
All statistical analyses were performed using SAS (version 9.4; SAS Institute). Only participants who completed all three supplementation periods were included in analyses. Differences between male and female participants at baseline were assessed by an independent two-sample t test (PROC TTEST). Change scores for end of treatment values were calculated by subtracting study-entry baseline values from each post-supplementation measure. Outcome variables were checked for normality (PROC UNIVARIATE) and positively skewed variables (skew >1; TAG, CRP and insulin) were logarithmically transformed. Participants with acutely elevated CRP (i.e. CRP ≥10.5 mg/l) at the end of a treatment period (n 2 for 50g/d treatment period), which is indicative of acute inflammation, were excluded from all analyses for that treatment period. This was done to ensure that the analysis was performed on the target population of healthy adults with moderately elevated blood pressure. For end of treatment values, the mixed models procedure (PROC MIXED) in SAS was used to test the effects of treatment, period and treatment by period interactions for each outcome. Baseline values were included as covariates. Because there was a trend for a significant period effect for the change in weight over the course of the study (P = 0.07; −0.2, +0.3 and+0.9 kg for periods 1, 2 and 3, respectively), change in weight was included as a covariate in all models. Subject was treated as a random effect and the remaining factors were fixed effects. When period and treatment by period interactions were non-significant, they were removed from the model. For all outcomes, no treatment by period effect was found. When period effects were significant, they were retained in the final model of treatment effects. Tukey−Kramer-adjusted P values were used for post hoc comparisons between the three groups. Values that were measured in duplicate on separate days (i.e. body weight and lipids) were averaged before analysis. Means are reported as least squares means with their standard errors unless otherwise specified. For all tests, α was set at 0.05.
Results
Of the twenty participants that completed the study, all were middle-aged, seven were normal weight (BMI 18.5 to <25 kg/m2), nine were overweight (BMI >25 and <30 kg/m2), and four were obese (BMI >30 kg/m2) at baseline (Table 2). All had moderately elevated resting systolic and diastolic blood pressure (Table 2). At baseline, LDL-cholesterol was optimal (<2.6 mmol/l) in two subjects, above optimal (2.6–3.3 mmol/l) in fourteen subjects, and borderline high (3.4–4.1 mmol/l) in four subjects. At baseline, male participants had significantly lower total cholesterol (TC), HDL-cholesterol, LDL-cholesterol, non-HDL-cholesterol, augmentation pressure, AI and heart rate compared with female participants (Table 2); otherwise, male and female participants who completed the study were not different from one another at baseline. No sex differences were found for any outcome variables in exploratory subgroup analyses (data not shown). Participants were compliant with the study intervention based on completion of self-reported daily consumption logs.
Table 2.
Baseline characteristics of participants who completed the study (Mean values with their standard errors, and ranges; n 20)
| Male (n 9) |
Female (n 11) |
|||||
|---|---|---|---|---|---|---|
| Mean | SEM | Range | Mean | SEM | Range | |
| Age (years) | 50.4 | 2.4 | 39−59 | 52.5 | 1.9 | 40−60 |
| BMI (kg/m2) | 26.4 | 0.9 | 23.6−31.0 | 26.6 | 1.0 | 22.1−32.6 |
| Glucose (mmol/l) | 4.9 | 0.1 | 4.6−5.3 | 4.9 | 0.1 | 4.3−5.5 |
| Insulin (μIU/I) | 5.2 | 0.7 | 2.2−9.0 | 5.6 | 0.7 | 3.0−11 |
| TC (mmol/l)* | 4.5 | 0.1 | 4.0−5.0 | 5.6 | 0.2 | 4.7−6.6 |
| HDL-cholesterol (mmol/l)* | 1.2 | 0.1 | 0.8−1.7 | 1.6 | 0.1 | 1.3−2.1 |
| TC:HDL | 4.1 | 0.4 | 2.5−6.2 | 3.5 | 0.2 | 2.9−4.8 |
| LDL-cholesterol (mmol/l)* | 2.7 | 0.1 | 2.0−3.2 | 3.4 | 0.1 | 2.9−4.3 |
| Non-HDL-cholesterol (mmol/l)* | 3.3 | 0.2 | 2.4−4.2 | 4.0 | 0.2 | 3.2−5.0 |
| TAG (mmol/l) | 1.3 | 0.2 | 0.7−3.0 | 1.3 | 0.1 | 0.7−2.2 |
| CRP (mg/l) | 1.9 | 0.5 | 0.2−4.0 | 2.6 | 0.9 | 0.3−10.4 |
| Brachial SBP (mmHg) | 128.4 | 2.8 | 116.5−139.5 | 130.2 | 3.1 | 120.5−147 |
| Brachial DBP (mmHg) | 83.2 | 1.9 | 75−92.5 | 81.9 | 3.1 | 59−93.5 |
| Central SBP (mmHg) | 118.4 | 2.8 | 107−127 | 121.1 | 3.1 | 107.5–136 |
| PP (mmHg) | 34.6 | 1.6 | 29−44.5 | 38.8 | 2.4 | 25−50.5 |
| AP (mmHg)* | 8.2 | 1.2 | 3.5−13.5 | 13.0 | 1.2 | 4.5–20 |
| AI@75 (%)* | 15.8 | 33 | 2.0−28 | 32 | 2.6 | 20−44.5 |
| HR (beats per min)* | 55.1 | 1.5 | 49−64.5 | 66.5 | 3.4 | 51.5–85 |
| PWV (m/s) | 8.0 | 0.2 | 6.4−8.9 | 7.6 | 0.3 | 6.5−9.3 |
TC, total cholesterol; CRP, C-reactive protein; SBP, systolic blood pressure; DBP diastolic blood pressure; PP, pulse pressure; AP, augmentation pressure; AI@75, augmentation index normalised to 75 beats per min; HR, heart rate; PWV, pulse wave velocity.
Significant difference between male and female participants (P< 0 05).
Effect of soya supplementation on ex vivo cholesterol efflux
There were no significant treatment effects for any measures of ex vivo cholesterol efflux (Table 3). ABCA1-specific efflux was significantly reduced from baseline following supplementation with the control (−12.7%; P = 0.02), but this change was not significant compared with ABCA1 efflux following 50 g/d of soya protein (P = 0.4).
Table 3.
Measures of ex vivo cholesterol efflux following supplementation with 50g/d isoflavone-containing soya protein compared with the control† (Mean values with their standard errors; n 20)
| Baseline |
0g/d soya protein (control) |
50 g/d soya protein‡ |
P for treatment effect | ||||
|---|---|---|---|---|---|---|---|
| Mean | SEM | Mean | SEM | Mean | SEM | ||
| ABCA1 (% efflux/4 h) | 3.46 | 0.34 | 3.02* | 0.18 | 3.15 | 0.18 | 0.39 |
| Global efflux (+cAMP) (% efflux/4 h) | 9.47 | 0.47 | 8.92 | 0.27 | 9.06 | 0.28 | 0.57 |
| Global efflux (−cAMP) (% efflux/4 h) | 6.00 | 0.26 | 5.89 | 0.18 | 5.91 | 0.18 | 0.93 |
ABCA1, ATP-binding cassette transporter 1; cAMP, cyclic AMP; CRP, C-reactive protein.
Significant change from baseline:
P = 0.02.
ABCA1-specific efflux was calculated as the difference between cAMP-stimulated and non-stimulated (−cAMP) efflux. Values were compared using the MIXED procedure (SAS version 9.4; SAS Institute Inc.). Period effects were universally non-significant (P> 0.05).
Data represent eighteen participants; two were excluded from analyses for this treatment period due to acutely elevated CRP concentrations (i.e. CRP ≥10.5 mg/l).
Effect of soya supplementation on vascular function
Post-supplementation values for blood pressure (brachial and central), AI and PWV are presented in Table 4. There was a significant treatment effect for brachial diastolic blood pressure (P = 0.04); however, in post hoc comparisons, the 2.3 mmHg reduction in brachial diastolic blood pressure following supplementation with 50 g/d soya protein was only significant compared with 25 g/d supplementation (Tukey-adjusted P = 0.03) (Fig. 2). There was a trend towards a significant treatment effect for central systolic blood pressure (P = 0.12); however, the only post hoc comparison that neared significance was 50 g/d soya protein v. 25 g/d (1.6% decrease v. 0.8% increase, respectively; unadjusted P = 0.05). There were no significant treatment effects for any other outcomes. There was a trend for a 3.1 and 2.8 point increase in AI@75 from baseline following supplementation with 50 g/d soya protein and 0 g/d (P = 0.07 and P = 0.09, respectively), but these changes were not significantly different from one another.
Table 4.
Measures of vascular function and indices of arterial stiffness following each 6-week treatment period* (Mean values with their standard errors; n 20)
| Baseline |
0 g/d soya protein (control) |
25 g/d soya protein |
50 g/d soya protein† |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SEM | Mean | SEM | Mean | SEM | Mean | SEM | Pfor treatment effect | |
| Brachial SBP (mmHg) | 129.4 | 2.1 | 128.2 | 2.1 | 130.5 | 2.1 | 127.4 | 2.2 | 0.18 |
| Brachial DBP (mmHg) | 82.5 | 1.9 | 82.0 | 1.2 | 83.6 | 1.2 | 80.5 | 1.2 | 0.04‡ |
| Central SBP (mmHg) | 119.9 | 2.1 | 119.1 | 1.9 | 120.9 | 1.9 | 118.0 | 2.0 | 0.12 |
| Central PP (mmHg) | 36.9 | 1.5 | 36.6 | 1.2 | 36.6 | 1.2 | 37.0 | 1.3 | 0.89 |
| AP (mmHg) | 10.9 | 1.0 | 11.6 | 0.9 | 11.1 | 0.9 | 11.9 | 0.9 | 0.47 |
| AI@75 (%) | 24.7 | 2.7 | 27.2 | 1.6 | 26.1 | 1.6 | 27.5 | 1.6 | 0.59 |
| HR (beats per min) | 61.4 | 2.3 | 62.4 | 1.0 | 64.3 | 1.0 | 62.6 | 1.1 | 0.25 |
| PWV (m/s) | 7.8 | 0.2 | 7.7 | 0.2 | 7.8 | 0.2 | 7.8 | 0.2 | 0.84 |
SBP, systolic blood pressure; DBP, diastolic blood pressure; PP, pulse pressure; AP, augmentation pressure; AI@75, augmentation index normalised to 75 beats per min; HR, heart rate; PWV, pulse wave velocity; CRP, C-reactive protein.
Values were compared using the MIXED procedure (SAS version 9.4; SAS Institute Inc.). Period effects were universally non-significant (P> 0.05).
Data represent eighteen participants; two were excluded from analyses for this treatment period due to acutely elevated CRP concentrations (i.e. CRP ≥10.5 mg/l).
Only 25 g/d soya protein v. 50 g/d was significant in post hoc comparisons (Tukey-adjusted P = 0.03).
Fig. 2.
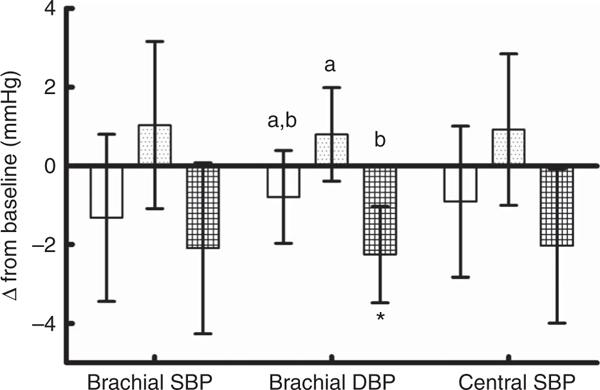
Changes in brachial and central blood pressures from baseline following 6 weeks of control and soya protein supplementation. Values are means (n 20), with their standard errors represented by vertical bars. SBP systolic blood pressure; DBP, diastolic blood pressure; □, 0g/d; ▦, 25g/d; ▦50g/d. Change scores were calculated by subtracting the baseline pre-supplementation value from post-supplementation values, and were compared using the MIXED procedure (SAS version 9.4; SAS Institute Inc.).a,b Mean values with unlike letters were significantly different. * Trend towards a significant difference from baseline (P = 0.07).
Effect of soya supplementation on lipids/lipoproteins and other blood markers of CVD
Post-supplementation values for lipids/lipoproteins, glucose metabolism and inflammatory markers are presented in Table 5. There were no significant treatment effects for any outcomes. Significant period effects were found for TAG, non-HDL- cholesterol and CRP. In post hoc comparisons, period 1 values were significantly lower than period 3 values for TAG (geometric means: 1.09 mmol/l (95% CI 0.89, 1.320) v. 1.32 mmol/l (95% CI 1.11, 1.57)) and non-HDL-cholesterol (means: 3.40 (SEM 0.09) v. 3.68 (SEM 0.09) mmol/l), whereas period 1 CRP values (geometric mean: 1.8 mg/l (95% CI 1.1−2.9)) were significantly higher than period 2 (geometric mean: 1.2 mg/l (95 % CI 0.7−2.0)) and period 3 values (geometric means: 1.2mg/l (95% CI 0.7−2.1)). Significant changes from baseline were found following soya supplementation for glucose and total cholesterol but no post hoc comparisons between treatment groups were significant.
Table 5.
Blood markers of CVD risk following each 6-week treatment period* (Mean values with their standard errors; n 20)
| Soya protein |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
0 g/d (control) |
25 g/d |
50 g/d† |
P |
||||||
| Mean | SEM | Mean | SEM | Mean | SEM | Mean | SEM | For treatment effect | For period effect | |
| Glucose (mmol/l) | 4.9 | 0.1 | 5.0 | 0.1 | 5.1 | 0.1 | 5.1 | 0.1 | 0.14 | 0.15 |
| log Insulin (μIU/I) | 0.70 | 0.04 | 0.73 | 0.04 | 0.69 | 0.04 | 0.73 | 0.04 | 0.74 | 0.43 |
| TC (mmol/l) | 5.1 | 0.2 | 4.9 | 0.1 | 5.0 | 0.1 | 4.9 | 0.1 | 0.64 | 0.06 |
| HDL-cholesterol (mmol/l) | 1.4 | 0.1 | 1.4 | 0.04 | 1.4 | 0.04 | 1.4 | 0.4 | 0.26 | 0.25 |
| TC:HDL-cholesterol | 3.8 | 0.2 | 3.8 | 0.1 | 3.7 | 0.1 | 3.7 | 0.1 | 0.57 | 0.87 |
| LDL-cholesterol (mmol/l) | 3.1 | 0.1 | 3.0 | 0.1 | 3.0 | 0.1 | 2.9 | 0.1 | 0.85 | 0.40 |
| log TAG (mmol/l) | 2.0 | 0.04 | 2.0 | 0.03 | 2.0 | 0.03 | 2.0 | 0.03 | 0.75 | 0.003a |
| Non-HDL-cholesterol (mmol/l) | 3.7 | 0.2 | 3.5 | 0.1 | 3.6 | 0.1 | 3.6 | 0.1 | 0.67 | 0.02b |
| log CRP (mg/l) | 0.16 | 0.10 | 0.11 | 0.07 | 0.18 | 0.07 | 0.11 | 0.07 | 0.36 | 0.02c |
TC, total cholesterol; CRP, C-reactive protein.
Period 1 values significantly lower than period 3 values in post hoc comparisons (Tukey-adjusted P = 0.002);
period 1 values significantly lower than period 3 values in post hoc comparisons (Tukey-adjusted P = 0.02);
period 1 values significantly higher than period 2 and period 3 values in post hoc comparisons (Tukey-adjusted P = 0.03 and 0.05, respectively).
Values were compared using the MIXED procedure (SAS version 9.4; SAS Institute Inc.).
Data represent eighteen participants; two were excluded from analyses for this treatment period due to acutely elevated CRP concentrations (i.e. CRP ≥10.5 mg/l).
Discussion
This study investigated the effects of a soya protein isolate containing endogenous isoflavones on HDL function and vascular function in adults with moderately elevated resting blood pressure. We found no significant treatment effects of soya supplementation for ex vivo cholesterol efflux or other blood markers of CVD risk. Brachial diastolic blood pressure was significantly reduced following consumption of 50 g/d of soya protein, but this 2.3 mmHg decrease was significant only when compared with the non-significant increase following supplementation with 25g/d soya protein. No other measures of vascular function were significantly altered by the study treatments.
Previous studies have shown that HDL function, in terms of ex vivo cholesterol efflux, can be improved by polyphenol-rich interventions such as extra virgin olive oil(9) and coffee(10), but little is known about soya. To our knowledge, the effect of an isoflavone-containing soya protein isolate on HDL function − rather than isolated soya isoflavones − has not previously been studied. The two previous studies of isolated soya isoflavones found that 3 months of supplementation had no effect on ex vivo cholesterol efflux in postmenopausal women(33,34). Pre-clinical evidence suggests that the provision of isoflavones in combination with soya protein may be necessary to elicit significant changes(30–32). The lack of effect on HDL efflux in the current study, using a soya protein isolate with isoflavones, may be due to the relatively short plasma half-life of soya iso-flavones(47–49), as soya isoflavones may not have been at peak concentrations during the time of the fasting blood sample. Alternatively, a longer supplementation period (e.g. 3 months) may be needed for other components of soya (i.e. soya protein) to have a sustained effect on ex vivo cholesterol efflux. Further research is needed to determine whether soya supplementation, either acute or longer-term, has the potential to improve HDL function. In addition, other tests of HDL function are also available and may provide further insight as a single assay may not be an ideal surrogate measure of HDL function.
Polyphenol-rich interventions have also been shown to improve central blood pressure and other measures of macro-vascular function, but results have been inconsistent. For instance, significant benefits have been achieved with water-melon(17,18), cranberry juice(15) and isoflavones(19,35), whereas no changes were found with spinach(20), cherry juice(21) or blueberries(50). These disparate results may be due in part to differences in study design (e.g. duration of supplementation) or the relative health of participants (e.g. individuals with elevated blood pressure v. normotensive individuals), but are also likely dependent on the unique profile of bioactive compounds provided by each intervention. Current understanding of the effects of soya on macrovascular function are similarly inconsistent and limited to a relatively small number of studies(37–39,47,51). Although significant reductions in PWV have been found using a synthetic isoflavone metabolite(37) and isolated red clover isoflavones(35), no significant changes in central PWV or AI were found following supplementation with a soya cereal (40 g soya protein)(38) or soya protein isolates (40 and 52 g soya protein)(39,51). Thus, our results are consistent with previous findings of no effect on PWV and/or AI. The cause of this incongruity between the vascular effects of isolated isoflavones v. soya protein is unknown as the studies were conducted in similar populations and the interventions provided similar amounts of isoflavones(35,37–39,51); however, this may be related to differences in the bioavailability of isoflavones from different food sources(52).
LDL-cholesterol and blood pressure are the primary modifiable CVD risk factors, and the potential hypocholesterolaemic effects of soya have been extensively investigated. Based largely on a 1995 meta-analysis(53) in which soya protein consumption (47g/d) reduced LDL-cholesterol by 13%, the US Food and Drug Administration issued a health claim stating that 25 g/d of soya protein (as part of a diet low in saturated fat and cholesterol) may reduce the risk of heart disease(26). However, more recent studies of soya protein have found much smaller LDL-cholesterol reductions (3–6%)(24,54–56). LDL-cholesterol reduction may also be greater in individuals with hyper-cholesterolaemia and/or elevated LDL-cholesterol at base- line(53,54,57); thus, the lack of LDL-cholesterol reduction in our study may have been due to the relatively normal TC (mean TC = 5.12mmol/l) and LDL-cholesterol (mean LDL-cholesterol = 3.10mmo]/l) of our participants at baseline, and is not unprecedented. Studies investigating the effects of soya on brachial blood pressure are more limited, but evidence suggests that soya supplementation may improve systolic and diastolic blood pressure; however the magnitude of effects may depend on the baseline blood pressure of participants and the type of control(58). The 2–3mmHg reduction in diastolic blood pressure that we observed with the 50 g/d dose is consistent with previous findings for individuals with moderately elevated resting blood pressure; however, it should be noted that this change was only significant compared with the change following the 25g/d dose.
In addition to the duration of supplementation, our null results may also be explained by the capacity of our participants to produce equol. In approximately 25–30% of individuals in Western countries, the parent isoflavone compound daidzein undergoes intestinal bacterial metabolism to form equol(59). Because equol and other isoflavone metabolites have more potent oestrogenic and antioxidant properties, it has been suggested that the beneficial effects of soya are dependent upon this conversion, and thus may occur only in equol producers(60). For instance, in older men with moderate 10-year CVD risk, only equol producers experienced acute improvements in arterial stiffness following the consumption of isolated isoflavones(47). However, the role of equol in eliciting the cardiovascular benefits of soya remains unclear since not all studies have shown differential effects in equol producers and non-equol producers(33,51,61) In addition, in most cases these were exploratory analyses and the studies were not designed to analyse differences between equol producers and non-equol producers. We did not assess equol production in our participants. However, given the prevalence of equol producers in the general US population, it is likely that many of our participants were non-equol producers and this may have influenced our results. Future soya protein supplementation studies should prospectively examine potential differences in effects between equol producers and non-equol producers to clarify the role of equol in achieving any physiological changes.
We further speculate that any beneficial effects of soya may depend on additional concomitant dietary changes. In the current study, the soya intervention, which provided both protein and isoflavones, was incorporated into the background diet without otherwise altering dietary habits. Participants significantly increased their protein intake during the 25 and 50 g/d soya protein supplementation periods (+17 and +44g/d, respectively; P< 0.0001), but the intake of energy content and other macronutrients was unchanged throughout the study and soya protein supplementation did not result in significant weight gain. In many of the studies demonstrating the LDL-lowering ability of soya, soya protein was compared with casein, milk or mixed animal proteins(24), whereas a carbohydrate-matched control was used in the current study. We noted that the carbohydrate control led to similar nonsignificant reductions in total and LDL-cholesterol compared with the soya protein treatments. It is possible that the cholesterol lowering effect from the control was due to a substitution effect of reducing fat energy content with energy content from carbohydrates, and/or the prebiotic effect of maltodextrin with the added hydrocolloids. Therefore, improvements in cholesterol efflux and macrovascular function following consumption of a soya protein isolate may similarly depend on the type of control and/or whether it replaces another component of the diet (e.g. animal protein, refined carbohydrates, added sugars, etc.). In addition, it is possible that the processing techniques used to produce the soya protein isolate and make it more dispersible in beverages (agglomeration) may have altered essential attributes of the protein or isoflavones that are necessary for their physiological actions. Future studies are needed to investigate whether processing techniques can alter the physiological effects of soya protein isolates. If future research confirms that soya products effectively modify CVD risk factors, incorporating them into an overall healthy dietary pattern is likely to achieve the greatest benefit.
Strengths and limitations
The cross-over design of this study allowed participants to act as their own controls and decreased potential sources of error by minimising the influence of between-subject variability when analysing treatment effects. Our participants had moderately elevated resting blood pressure but were otherwise generally healthy and representative of the general population. Our study population was also well-balanced with regard to male and female participants; however, our sample size was relatively small and additional studies with larger participant populations are needed. Moreover, we did not determine the equol producing capability of our participants, which may influence whether soya supplementation elicits significant health benefits(59). The soya protein isolate intervention was incorporated into the normal dietary habits of participants, making it more reflective of ‘real world’ implementation. The carbohydrate content of the soya and control powders was closely matched, and the amount of soya protein and isoflavones provided by the interventions was consistent previous studies(33,34,37,39,51). The consumption logs and 3-d food recalls indicate that participants consumed the study powders and followed the instruction to avoid other soya- containing foods; thus, it is unlikely that these factors are responsible for our null findings. Multiple CVD risk factors, including both traditional and emerging risk factors, were also assessed. Although few of our female participants were premenopausal, vascular function may have been assessed in these women during different phases of their menstrual cycle. Future studies should test premenopausal female participants during the 1st week of their menstrual cycle to minimise potential hormonal effects on vascular function. Furthermore, due to the number of treatments, the duration of individual supplementation periods was constrained in order to maximise participant retention for the duration of the study. Longer periods of supplementation may be required to alter cholesterol efflux and/or macrovascular function. Additional research is also needed to directly compare the effects of soya protein, soya isoflavones and their combination.
Conclusions
Supplementation with an isoflavone-containing soya protein isolate (delivering 25 and 50 g/d soya protein) for 6 weeks did not alter ex vivo cholesterol efflux or measures of macrovascular function in adults with moderately elevated brachial blood pressure. Additional research is needed to determine whether consumption of a soya protein isolate with naturally occurring isoflavones reduces CVD risk by modifying ex vivo cholesterol efflux and macrovascular function. Future studies should employ longer periods of supplementation, and should be powered to analyse differences between equol producers and non-equol producers.
Supplementary Material
Acknowledgements
The authors would like to thank our research participants for their dedication to the project, as well as the nursing and clinical staff of the Clinical Research Center of the Pennsylvania State University. The authors would also like to acknowledge Cameron Lusk and Glenna Hughes for formulating and producing the soya and control powders.
DuPont Nutrition and Health provided financial support for the study. This project was also supported by the Penn State Clinical & Translational Research Institute, Pennsylvania State University Clinical and Translational Science Award (CTSA), National Institutes of Health/National Center for Advancing Translational Science (NIH/NCATS) grant no. UL1 TR000127. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or NCATS. P. M. K.-E. received funding from DuPont Nutrition and Health for the current study. Financial supporters had no role in the design and conduct of the study; in the collection, analysis and interpretation of the data; or in the preparation, review or approval of the manuscript.
Footnotes
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S000711451700143X
References
- 1.Khera AV, Cuchel M, de la Llera-Moya M, et al. (2011) Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl J Med 364, 127–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.deGoma EM, deGoma RL & Rader DJ (2008) Beyond high- density lipoprotein cholesterol levels evaluating high-density lipoprotein function as influenced by novel therapeutic approaches. J Am Coll Cardiol 51, 2199–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boden WE, Probstfield JL, Anderson T, et al. (2011) Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med 365, 2255–2267. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz GG, Olsson AG, Abt M, et al. (2012) Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med 367, 2089–2099. [DOI] [PubMed] [Google Scholar]
- 5.Barter PJ, Caulfield M, Eriksson M, et al. (2007) Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med 357, 2109–2122. [DOI] [PubMed] [Google Scholar]
- 6.Roman MJ, Devereux RB, Kizer JR, et al. (2007) Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart Study. Hypertension 50, 197–203. [DOI] [PubMed] [Google Scholar]
- 7.Waddell TK, Dart AM, Medley TL, et al. (2001) Carotid pressure is a better predictor of coronary artery disease severity than brachial pressure. Hypertension 38, 927–931. [DOI] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Services & US Department of Agriculture (2015) 2015–2020 Dietary Guidelines for Americans. Washington, DC: US Department of Health and Human Services & US Department of Agriculture. [Google Scholar]
- 9.Helal O, Berrougui H, Loued S, et al. (2013) Extra-virgin olive oil consumption improves the capacity of HDL to mediate cholesterol efflux and increases ABCA1 and ABCG1 expression in human macrophages. Br J Nutr 109, 1844–1855. [DOI] [PubMed] [Google Scholar]
- 10.Uto-Kondo H, Ayaori M, Ogura M, et al. (2010) Coffee consumption enhances high-density lipoprotein-mediated cholesterol efflux in macrophages. Circ Res 106, 779–787. [DOI] [PubMed] [Google Scholar]
- 11.Berrougui H, Grenier G, Loued S, et al. (2009) A new insight into resveratrol as an atheroprotective compound: inhibition of lipid peroxidation and enhancement of cholesterol efflux. Atherosclerosis 207, 420–427. [DOI] [PubMed] [Google Scholar]
- 12.Xia M, Hou M, Zhu H, et al. (2005) Anthocyanins induce cholesterol efflux from mouse peritoneal macrophages: the role of the peroxisome proliferator-activated receptor {gamma}-liver X receptor {alpha}-ABCA1 pathway. J Biol Chem 280, 36792–36801. [DOI] [PubMed] [Google Scholar]
- 13.Fuhrman B, Volkova N & Aviram M (2005) Pomegranate juice inhibits oxidized LDL uptake and cholesterol biosynthesis in macrophages. J Nutr Biochem 16, 570–576. [DOI] [PubMed] [Google Scholar]
- 14.McAnulty LS, Collier SR, Landram MJ, et al. (2014) Six weeks daily ingestion of whole blueberry powder increases natural killer cell counts and reduces arterial stiffness in sedentary males and females. Nutr Res 34, 577–584. [DOI] [PubMed] [Google Scholar]
- 15.Dohadwala MM, Holbrook M, Hamburg NM, et al. (2011) Effects of cranberry juice consumption on vascular function in patients with coronary artery disease. Am J Clin Nutr 93, 934–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Habauzit V, Verny MA, Milenkovic D, et al. (2015) Flavanones protect from arterial stiffness in postmenopausal women consuming grapefruit juice for 6 mo: a randomized, controlled, crossover trial. Am J Clin Nutr 102, 66–74. [DOI] [PubMed] [Google Scholar]
- 17.Figueroa A, Wong A, Hooshmand S, et al. (2013) Effects of watermelon supplementation on arterial stiffness and wave reflection amplitude in postmenopausal women. Menopause 20, 573–577. [DOI] [PubMed] [Google Scholar]
- 18.Figueroa A, Sanchez-Gonzalez MA, Perkins-Veazie PM, et al. (2011) Effects of watermelon supplementation on aortic blood pressure and wave reflection in individuals with prehypertension: a pilot study. Am J Hypertens 24, 40–44. [DOI] [PubMed] [Google Scholar]
- 19.Curtis PJ, Potter J, Kroon PA, et al. (2013) Vascular function and atherosclerosis progression after 1 y of flavonoid intake in statin-treated postmenopausal women with type 2 diabetes: a double-blind randomized controlled trial. Am J Clin Nutr 97, 936–942. [DOI] [PubMed] [Google Scholar]
- 20.Jovanovski E, Bosco L, Khan K, et al. (2015) Effect of spinach, a high dietary nitrate source, on arterial stiffness and related hemodynamic measures: a randomized, controlled trial in healthy adults. Clin Nutr Res 4, 160–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lynn A, Mathew S, Moore CT, et al. (2014) Effect of a tart cherry juice supplement on arterial stiffness and inflammation in healthy adults: a randomised controlled trial. Plant Foods Hum Nutr 69, 122–127. [DOI] [PubMed] [Google Scholar]
- 22.Bondonno CP, Liu AH, Croft KD, et al. (2014) Short-term effects of nitrate-rich green leafy vegetables on blood pressure and arterial stiffness in individuals with high-normal blood pressure. Free Radic Biol Med 77, 353–362. [DOI] [PubMed] [Google Scholar]
- 23.Lynn A, Hamadeh H, Leung WC, et al. (2012) Effects of pomegranate juice supplementation on pulse wave velocity and blood pressure in healthy young and middle-aged men and women. Plant Foods Hum Nutr 67, 309–314. [DOI] [PubMed] [Google Scholar]
- 24.Sacks FM, Lichtenstein A, Van Horn L, et al. (2006) Soy protein, isoflavones, and cardiovascular health: an American Heart Association Science Advisory for professionals from the Nutrition Committee. Circulation 113, 1034–1044. [DOI] [PubMed] [Google Scholar]
- 25.Kris-Etherton PM, Hecker KD, Bonanome A, et al. (2002) Bioactive compounds in foods: their role in the prevention of cardiovascular disease and cancer. Am J Med 113, Suppl. 9B, 71S–88S. [DOI] [PubMed] [Google Scholar]
- 26.Food and Drug Administration & Department of Health and Human Services (1999) Food labeling: health claims; soy protein and coronary heart disease. Fed Regist 64, 57699–57733. [PubMed] [Google Scholar]
- 27.Zhang X, Shu XO, Gao YT, et al. (2003) Soy food consumption is associated with lower risk of coronary heart disease in Chinese women. J Nutr 133, 2874–2878. [DOI] [PubMed] [Google Scholar]
- 28.Sasazuki S (2001) Case-control study of nonfatal myocardial infarction in relation to selected foods in Japanese men and women. Jpn Circ J 65, 200–206. [DOI] [PubMed] [Google Scholar]
- 29.Kokubo Y, Iso H, Ishihara J, et al. (2007) Association of dietary intake of soy, beans, and isoflavones with risk of cerebral and myocardial infarctions in Japanese populations: the Japan Public Health Center-based (JPHC) study cohort I. Circulation 116, 2553–2562. [DOI] [PubMed] [Google Scholar]
- 30.Wagner JD, Schwenke DC, Greaves KA, et al. (2003) Soy protein with isoflavones, but not an isoflavone-rich supplement, improves arterial low-density lipoprotein metabolism and atherogenesis. Arterioscler Thromb Vasc Biol 23, 2241–2246. [DOI] [PubMed] [Google Scholar]
- 31.Greaves KA, Parks JS, Williams JK, et al. (1999) Intact dietary soy protein, but not adding an isoflavone-rich soy extract to casein, improves plasma lipids in ovariectomized cynomolgus monkeys. J Nutr 129, 1585–1592. [DOI] [PubMed] [Google Scholar]
- 32.Anthony MS, Clarkson TB, Bullock BC, et al. (1997) Soy protein versus soy phytoestrogens in the prevention of diet-induced coronary artery atherosclerosis of male cynomolgus monkeys. Arterioscler Thromb Vasc Biol 17, 2524–2531. [DOI] [PubMed] [Google Scholar]
- 33.Badeau R, Jauhiainen M, Metso J, et al. (2007) Effect of isolated isoflavone supplementation on ABCA1-dependent cholesterol efflux potential in postmenopausal women. Menopause 14, 293–299. [DOI] [PubMed] [Google Scholar]
- 34.Tormala RM, Nikander E, Tiitinen A, et al. (2006) Serum cholesterol efflux potential in postmenopausal women treated with isolated isoflavones. Menopause 13, 96–101. [DOI] [PubMed] [Google Scholar]
- 35.Teede HJ, McGrath BP, DeSilva L, et al. (2003) Isoflavones reduce arterial stiffness: a placebo-controlled study in men and postmenopausal women. Arterioscler Thromb Vasc Biol 23, 1066–1071. [DOI] [PubMed] [Google Scholar]
- 36.Pase MP, Grima NA & Sarris J (2011) The effects of dietary and nutrient interventions on arterial stiffness: a systematic review. Am J Clin Nutr 93, 446–454. [DOI] [PubMed] [Google Scholar]
- 37.Nestel P, Fujii A & Zhang L (2007) An isoflavone metabolite reduces arterial stiffness and blood pressure in overweight men and postmenopausal women. Atherosclerosis 192, 184–189. [DOI] [PubMed] [Google Scholar]
- 38.Teede HJ, Giannopoulos D, Dalais FS, et al. (2006) Randomised, controlled, cross-over trial of soy protein with isoflavones on blood pressure and arterial function in hypertensive subjects. J Am Coll Nutr 25, 533–540. [DOI] [PubMed] [Google Scholar]
- 39.Teede HJ, Dalais FS, Kotsopoulos D, et al. (2001) Dietary soy has both beneficial and potentially adverse cardiovascular effects: a placebo-controlled study in men and postmenopausal women. J Clin Endocrinol Metab 86, 3053–3060. [DOI] [PubMed] [Google Scholar]
- 40.Chobanian AV, Bakris GL, Black HR, et al. (2003) The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 289, 2560–2572. [DOI] [PubMed] [Google Scholar]
- 41.Berryman CE, Grieger JA, West SG, et al. (2013) Acute consumption of walnuts and walnut components differentially affect postprandial lipemia, endothelial function, oxidative stress, and cholesterol efflux in humans with mild hypercholesterolemia. J Nutr 143, 788–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen CH, Nevo E, Fetics B, et al. (1997) Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Validation of generalized transfer function. Circulation 95, 1827–1836. [DOI] [PubMed] [Google Scholar]
- 43.Pauca AL, O’Rourke MF & Kon ND (2001) Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension 38, 932–937. [DOI] [PubMed] [Google Scholar]
- 44.Sharman JE, Lim R, Qasem AM, et al. (2006) Validation of a generalized transfer function to noninvasively derive central blood pressure during exercise. Hypertension 47, 1203–1208. [DOI] [PubMed] [Google Scholar]
- 45.Wilkinson IB, MacCallum H, Flint L, et al. (2000) The influence of heart rate on augmentation index and central arterial pressure in humans. J Physiol 525, 263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Laurent S, Cockcroft J, Van Bortel L, et al. (2006) Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 27, 2588–2605. [DOI] [PubMed] [Google Scholar]
- 47.Hazim S, Curtis PJ, Schar MY, et al. (2016) Acute benefits of the microbial-derived isoflavone metabolite equol on arterial stiffness in men prospectively recruited according to equol producer phenotype: a double-blind randomized controlled trial. Am J Clin Nutr 103, 694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Franke AA, Lai JF & Halm BM (2014) Absorption, distribution, metabolism, and excretion of isoflavonoids after soy intake. Arch Biochem Biophys 559, 24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zubik L & Meydani M (2003) Bioavailability of soybean iso- 55. flavones from aglycone and glucoside forms in American women. Am J Clin Nutr 77, 1459–1465. [DOI] [PubMed] [Google Scholar]
- 50.Johnson SA, Figueroa A, Navaei N, et al. (2015) Daily blueberry 56. consumption improves blood pressure and arterial stiffness in postmenopausal women with pre- and stage 1-hypertension: a randomized, double-blind, placebo-controlled clinical trial. J Acad Nutr Diet 115, 369–377. [DOI] [PubMed] [Google Scholar]
- 51.Tormala R, Appt S, Clarkson TB, et al. (2008) Equol production capability is associated with favorable vascular function in postmenopausal women using tibolone; no effect with soy 58. supplementation. Atherosclerosis 198, 174–178. [DOI] [PubMed] [Google Scholar]
- 52.Cassidy A, Brown JE, Hawdon A, et al. (2006) Factors affecting the bioavailability of soy isoflavones in humans after ingestion 59. of physiologically relevant levels from different soy foods. J Nutr 136, 45–51. [DOI] [PubMed] [Google Scholar]
- 53.Anderson JW, Johnstone BM & Cook-Newell ME (1995) Meta-analysis of the effects of soy protein intake on serum lipids. N Engl J Med 333, 276–282. [DOI] [PubMed] [Google Scholar]
- 54.Zhan S & Ho SC (2005) Meta-analysis of the effects of soy protein containing isoflavones on the lipid profile. Am J Clin Nutr 81, 397–408. [DOI] [PubMed] [Google Scholar]
- 55.Reynolds K, Chin A, Lees KA, et al. (2006) A meta-analysis of the effect of soy protein supplementation on serum lipids. Am J Cardiol 98, 633–640. [DOI] [PubMed] [Google Scholar]
- 56.Harland JI & Haffner TA (2008) Systematic review, meta-analysis and regression of randomised controlled trials reporting an association between an intake of circa 25 g soya protein per day and blood cholesterol. Atherosclerosis 200, 13–27. [DOI] [PubMed] [Google Scholar]
- 57.Tokede OA, Onabanjo TA, Yansane A, et al. (2015) Soya products and serum lipids: a meta-analysis of randomised controlled trials. Br J Nutr 114, 831–843. [DOI] [PubMed] [Google Scholar]
- 58.Dong JY, Tong X, Wu ZW, et al. (2011) Effect of soya protein on blood pressure: a meta-analysis of randomised controlled trials. Br J Nutr 106, 317–326. [DOI] [PubMed] [Google Scholar]
- 59.Setchell KD & Clerici C (2010) Equol: history, chemistry, and formation. J Nutr 140, 1355S–1362S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Setchell KD, Brown NM & Lydeking-Olsen E (2002) The clinical importance of the metabolite equol-a clue to the effectiveness of soy and its isoflavones. J Nutr 132, 3577–3584. [DOI] [PubMed] [Google Scholar]
- 61.Kreijkamp-Kaspers S, Kok L, Bots ML, et al. (2005) Randomized controlled trial of the effects of soy protein containing isoflavones on vascular function in postmenopausal women. Am J Clin Nutr 81, 189–195. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


