Worksites are important community-based settings for health promotion activities (Glasgow, Vogt, & Boles, 1999; Sorensen et al., 1998). Small worksites employ many low-wage workers, who are at increased risk for behaviors linked to developing chronic diseases (including poor nutrition, lack of physical activity, tobacco use, and lack of preventive screenings) (Harris, Huang, Hannon, & Williams, 2011; Pampel, Krueger, & Denney, 2010). Many evidence-based health promotion best practices address these behaviors (CDC Task Force on Community Preventive Services, 2014), and previous research reveals that small, low-wage worksites engaged in health promotion interventions can increase their adoption of evidence-based best practices (Beresford et al., 2007; Laing et al., 2012; Sorensen et al., 2005). There is also evidence that low-wage workers hold positive attitudes toward workplace health promotion and would welcome employer efforts to support their health (Hammerback et al., 2015).
Despite the evidence above, employers at small, low-wage worksites often do not offer health promotion programs, largely due to lack of capacity and resources (Hannon et al., 2012), making them difficult to recruit for research studies. Although many researchers develop and test health promotion interventions for low-wage worksites (Barbeau et al., 2004; Thompson et al., 2005), there is currently a dearth of literature providing details about how worksites are recruited (Linnan et al., 2002; Linnan, Tate, et al., 2012; Thompson, van Leynseele, & Beresford, 1997). Studies that involve worksite-level recruitment for workplace health promotion interventions often report participation rates that are low, or lower than expected, which suggests that recruitment presents challenges (Egelhoff, Katz, Brosseau, & Hennrikus, 2015; Linnan et al., 2002). Low recruitment rates can impact external validity, which threatens the generalizability of the research (Barbeau et al., 2004; Biener, DePue, Emmons, Linnan, & Abrams, 1994). A slow pace of recruitment can also drain resources and discourage research staff. Most critically, sluggish recruitment results in fewer low-wage employees receiving health promotion interventions from which they may benefit. Determining which recruitment methods are most efficient and effective is of critical importance for all of these reasons.
This paper seeks to expand on the 2012 work of Laura Linnan and her colleagues on comparing recruitment processes for African-American beauty parlors (Linnan, Harrington, Bangdiwala, & Evenson, 2012). That work focused explicitly on three distinct strategies of worksite-level recruitment (phone call prior to visit, drop-in visit, and referral plus visit), and provided a uniquely rich amount of detail on each recruitment approach and the associated resource burden for study staff. We aim to continue the effort to lift the veil on recruitment practices, this time with a broader range of worksite types, by exploring the effectiveness of multiple methods used for recruiting small, low-wage worksites to the HealthLinks Trial (Hannon et al., 2016). In particular, we will detail how we leveraged relationships with several community partners to recruit worksites.
In addition to examining the efficiency and effectiveness of different recruitment methods for this study, this paper will also assess and compare the degree of worksites’ readiness to implement health promotion recruited through each method. Organizational readiness for change, which refers to organizational members’ shared resolve to implement a change and shared belief in their collective ability do so, is considered an important driver to successful adoption of complex changes (Weiner, 2009). We did this comparison, along with examining industry and size of recruited worksites, to determine if there were systematic differences between worksites recruited via each method. Specifically, we wanted to test whether worksites referred to us were more ready for health promotion than worksites we recruited through cold calls, which could have implications for the generalizability of our trial findings.
Methods
The Intervention
HealthLinks is an evidence-based workplace wellness program tailored to the needs of small, under-resourced worksites and was developed by the American Cancer Society (ACS) and the University of Washington Health Promotion Research Center (Laing et al., 2012). The goal of HealthLinks is to help small worksites implement a set of best practices, based on the Centers for Disease Control and Prevention’s Guide to Community Preventive Services (CDC Task Force on Community Preventive Services, 2014), and aimed at increasing physical activity, healthy eating, tobacco control, and appropriate cancer screening. HealthLinks provides small worksites with free tools and on-site technical assistance to implement the best practices. The current study focuses on recruitment for a 3-arm, randomized controlled trial of 78 worksites to test the effectiveness of HealthLinks on (a) worksite implementation of evidence-based practices described above, and (b) worker physical activity levels, healthy eating habits, cancer screening rates, and tobacco cessation attempts. The ACS HealthLinks Randomized Controlled Trial is described elsewhere (Hannon et al., 2016).
Setting
All worksites recruited for the HealthLinks trial were located in King County, Washington (which includes the Seattle metropolitan area).
Human Subjects Approval
Study protocols and materials were reviewed by the University of Washington Institutional Review Board. Upon IRB approval, the study was registered at Clinicaltrials.gov (NCT02005497).
Eligibility criteria
Eligible worksites employed 20–200 employees in total and were officially classified in one of the North American Industry Classification System (NAICS) industry codes that designate six large, low-wage industries (accommodation and food services; arts, entertainment, and recreation; education; health care and social assistance; other services excluding public administration; and retail trade) (Washington State Employment Security Department, 2016). Because participation in this trial was potentially a 3-year commitment, and a large proportion of new businesses are unable to stay in business that length of time (USSBA: U.S. Small Business Administration, 2014), eligible worksites had to have been in business for a minimum of 3 years at the time of recruitment. In addition, we required that a minimum of 20% of employees worked onsite at least one day per week, and that no worksite currently have an active wellness committee.
Recruitment procedures
Recruitment for this study was accomplished via three methods: 1) purchased list; 2) a list of eligible worksites provided to the research staff from a community partner (a health insurer); and 3) a relationship-based referral pipeline from several partners. Regardless of recruitment method, worksites screened as eligible were offered the opportunity to meet with members of the research staff in person to discuss the study (described below in “pitch meetings”). All worksites were contacted up to 15 times before being permanently classified as “non-contact.”
1. Purchased list (“cold calls”)
A list of worksites meeting our size and eligibility criteria was generated by Survey Sampling International (Shelton, CT). In King County, 1,167 worksites met these criteria. When available, this list included a contact name for a human resources manager or senior leader. The list was then randomly sequenced, and each of four research staffers responsible for recruitment (hereafter “recruiters”) were initially given a list of 150 worksites to “cold-call.”
2. List provided by community partner (“partner list”)
The second recruitment method we relied on was a list provided by one of our health insurer partners. The insurer provided us with a list of client worksites that they believed would be eligible for HealthLinks. No attempt to gauge interest in the program was made by the health insurer partner; instead, recruiters called each of these client worksites, indicated where the contact information had come from, and described the program.
3. Relationship-based referrals (“warm referrals”)
The final recruitment method we used was referral from community partners. We asked two insurers (both public sector) and three brokers (all private sector), whom we had either worked with in previous research projects and/or knew through participation on committees or other mutual engagements, to identify client worksites that met our size and industry criteria. The insurer or broker would then contact and describe the project to the client worksite by phone or email. At the health insurers, we worked with individual account representatives. Account representatives have their own slate of client worksites for which they serve as the primary contact, so we received referrals from multiple account representatives at both health insurers. Generally, the account representatives first sent the recruitment request to the client’s broker, who would then serve as liaison between the research team and the client. From the brokerages, we received referrals from individuals employed there who worked directly with employer clients. We also worked with an employer-member organization representing employers in Washington State. Referrals from this organization came either from an employee contact at the organization or a description in a members-only newsletter. Lastly, referrals were generated from a handful of community partners we had worked with on past projects who heard about the study and recommended it to their colleagues.
We refer to worksites contacted via pre-existing relationships with community partners as “warm referrals.”
Duplicates
Many of the warm referrals also appeared on the purchased list. If a referred worksite had not yet been contacted from the purchased list, we marked this worksite as “Do not call,” and considered it a referral. We then contacted the worksite based on the warmer recruitment approach (i.e., by responding to the email sent by the referral source or calling the worksite and referring to the list provided by the health insurer). If the worksite had been contacted on the purchased list but had not yet been screened, it was also marked as “Do not call” and the warmer recruitment approach was employed. If the worksite had been contacted and screened on the purchased list, and had declined a pitch meeting, we did not attempt to reach them through one of the warmer methods but instead marked them as “Declined to enroll.”
Pitch meetings
All worksites interested in hearing more about the HealthLinks study received an in-person visit from a two-person recruitment team. This introductory “pitch meeting” generally lasted 30–60 minutes and was held with either one worksite contact (usually the human resources manager that the recruiter had initially spoken to and screened for eligibility) or a team of people. When recruiters met with a team, it most often was due to a senior leader wanting to hear more about what participation would entail. During the meeting, the recruiters provided more details about the HealthLinks Trial, including the specific requirements for participation, and answered questions.
Study enrollment
Once participation requirements had been outlined and all questions answered, employers choosing to enroll in the HealthLinks trial were asked to sign a memorandum of understanding (MOU), which described each step of the trial and outlined the responsibilities of both the worksite and the research staff. Once the MOU had been signed, research staff would administer the baseline employer assessment and strategize how best to complete the employee surveys. Upon completion of baseline data collection, the worksite was considered officially enrolled.
Readiness for change
To capture the degree to which a worksite was ready to implement a workplace wellness program, we developed an instrument to be administered at baseline to each worksite (Hannon et al., 2017). We constructed a total readiness score based on the mean value of the scores on six scales that each capture a specific construct in the theory organizational readiness for change; context, change valence, informational assessment, change commitment, change efficacy, and wellness program effort (Hannon et al., 2017; Weiner, 2009).
Results
Overall recruitment
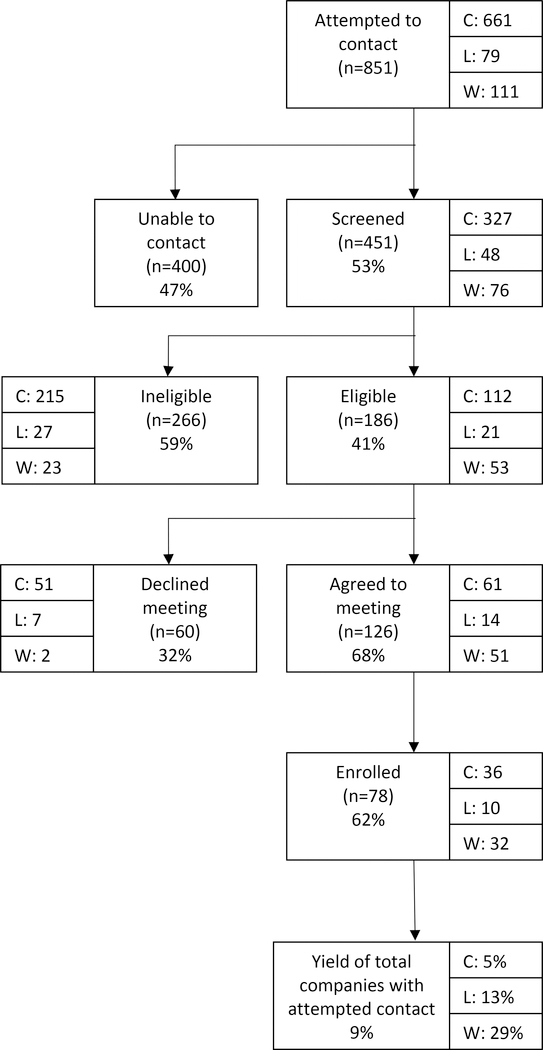
Of the 851 total worksites we attempted to contact, 451 (53%) were screened, and 186 (41% of those screened) were eligible. Among eligible worksites, 126 (68%) agreed to a pitch meeting, and 78 (62%) of the worksites that met with the recruitment team enrolled in the HealthLinks Trial (42% of eligible worksites). The overall recruitment yield (defined as the percentage of enrolled worksites divided by the number of worksites recruiters attempted to contact) was 9%. For worksites contacted via purchased list, the yield was 5%. The yield from the partner list was 13%. For worksites recruited via warm referral, the yield was 29%.
Details on the three recruitment strategies are provided below. Figure 1 provides an overview of recruitment yields for each method.
Figure 1.
Overview of Recruitment Yield by Strategy
Purchased List (cold calls)
Recruiters attempted to contact 661 worksites on the purchased list. Of those 661, 327 (49%) were screened, and 112 (34% of those screened) were eligible. Of the eligible worksites, 61 (54%) agreed to a meeting, and 36 (59% of those who received a meeting) enrolled.
Partner list (“lukewarm”)
We attempted to contact all 79 worksites provided to us by one of our health insurer partners. Of those, 48 (61%) were screened, and 21 (44%) of those screened were eligible. Among the eligible worksites, 14 (67%) agreed to an in-person meeting, and 10 (71%) of those worksites chose to enroll.
Warm referrals
Of the warm referrals, 76 of the 111 (68%) we attempted to contact were fully screened, and 53 (70%) of those screened were eligible for participation. Of those eligible worksites, 51 (96%) agreed to a pitch meeting, and 32 (63%) enrolled.
Within this category, most of the referrals (90) were originally generated from the two health insurers. When the types of warm referrals were compared, there were no meaningful differences on rates of screening, eligibility, agreement to meet, or enrollment across the community partner sub-categories.
Worksite characteristics
Worksite characteristics included worksite size, industry type (measured in the six categories described under “Eligibility Criteria” above), and average readiness for change. Differences in worksite characteristics between recruitment methods were assessed using analysis of variance. Average worksite size did not differ by recruitment method (F (2) = 2.80, p=.07). Representation of industries also did not differ by recruitment method (F (2) = 1.47, p=.27). Average readiness for change did not vary significantly by recruitment method (F (2) = .01, p=.99). Worksite characteristics are included in Table 1.
Table 1.
Company Characteristics by Referral Type
| All N=78 | Purchased List N=36 | Partner List N=10 | Warm Referrals N=32 | |||||
|---|---|---|---|---|---|---|---|---|
| Count | Percent | Count | Percent | Count | Percent | Count | Percent | |
| Worksite size (mean) | 76 | 65 | 107 | 80 | ||||
| Industry | ||||||||
| Accommodation and food services | 7 | 9% | 3 | 8% | 0 | -- | 4 | 13% |
| Arts, entertainment, and recreation | 3 | 4% | 2 | 6% | 1 | 10% | 0 | -- |
| Educational services | 8 | 10% | 2 | 6% | 3 | 30% | 3 | 9% |
| Health care and social assistance | 34 | 44% | 14 | 39% | 4 | 40% | 16 | 50% |
| Other services (expect public administration) | 15 | 19% | 10 | 28% | 2 | 20% | 3 | 9% |
| Retail trade | 11 | 14% | 5 | 14% | 0 | -- | 6 | 19% |
| Readiness (mean) | 3.30 | 3.30 | 3.31 | |||||
Note: Due to rounding, numbers may not total 100%
Discussion
This paper looks closely at three distinct methods of worksite recruitment: traditional cold calling from a purchased list; lukewarm referrals (a list provided by a community partner); and warm referrals via pre-existing relationships with community partners (primarily health insurers and brokers). It is clear from the overall results that, for this study, the warmer the referral source, the better.
Examining the recruitment process in detail helps explain why. First, eligibility was higher among the warmer referrals. Despite purchasing a list from a reputable list provider, most of the worksites screened from the purchased list were ineligible for the study, usually due to being too small (<20 employees). In contrast, only a third of the worksites recruited from warm referral were ineligible. Second, nearly all of the warm-referred worksites that were eligible for the study agreed to a pitch meeting, in contrast to two-thirds of worksites from the health insurer’s list, and about half of worksites from the purchased list. Given these two factors, the overall enrollment among eligible worksites was higher the warmer the recruitment method. It appears that much of the difference in the effectiveness of the three recruitment strategies is driven by identifying eligible worksites and convincing them to attend a pitch meeting.
The only result that is not clearly more favorable among the warm-referred worksites is the percentage of worksites who met with the recruiters who ultimately agreed to enroll in the study. This proportion is similar for the three methods. It appears that once the recruitment team was able to get some face time with the worksite, the playing field between recruitment methods was fairly level. This may reflect the fact that, in most cases, multiple organizational levels had to signal interest before the in-person meeting took place.
Though they were more effective, the warmer referral methods had challenges. Account representatives at health insurance worksites and brokers are busy, and it often took multiple tries, frequent prodding, and long waits to receive introductions to client worksites interested in participating in the HealthLinks trial. It was not uncommon to receive the bulk of the referrals from a few enthusiastic account representatives (generally vetted by brokers), and nothing at all from others.
In addition, working with brokers can be tricky. Health insurance brokerage is an extremely competitive industry (Karaca-Mandic, Feldman, & Graven, 2016), and individual brokers frequently view themselves as directly competing against other brokers at their brokerage, as well as brokers at other brokerages (Witt, Olsen, & Ablah, 2013). Even though we received many more referrals from account representatives at insurers than we did from the brokerages, we ultimately spent the bulk of our time dealing with questions and concerns from brokers. Most often, their inquiries focused on gaining a better understanding of what the program entailed, and what a research study would require from employers who participated. Once brokers were convinced that we were not selling anything, and that the HealthLinks program did not constitute a competitive threat to offerings delivered via the brokerage, most were willing to provide our contact information and details of the project to eligible clients.
We were also concerned that the worksites referred to us via community partners would look different than those identified through a purchased list. In particular, we wondered if the warm referrals, because they were often hand-picked as a “good prospect” for a wellness program by the partner, would be more ready to take on a wellness program than a worksite recruited from a purchased list and thus less generalizable to the population of small worksites in low-wage industries. However, this did not appear to be true, in that readiness scores did not differ based on recruitment method. We generally find that small worksites in low-wage industries are doing very little workplace health promotion (Hannon et al., 2012; Hannon et al., 2016), which may explain why recruitment method did not show differing levels of readiness. In populations of worksites where workplace health promotion activities are more prevalent (for example, large worksites), recruiting through warm referrals may lead to identifying worksites that are more ready for health promotion, and this should be explored in future research.
Study Limitations
This study had multiple limitations. First, the methods of warm referral, while all relationship-based, differ. Second, although we are able to say that the purchased list was randomly sequenced, we cannot say that it included all eligible worksites in King County. A number of eligible worksites recruited through the community partners did not appear on the purchased list. In addition, we were surprised by the large number of ineligible worksites on the purchased list. The literature suggests that purchased lists, even those from reputable worksites, are rarely entirely complete or accurate (Biener et al., 1994; Egelhoff et al., 2015; Thompson et al., 1997). Third, these results may not generalize beyond small, low-wage worksites.
Strengths
This study also has important strengths. First, it is the first study to compare a purchased-list approach with two different levels of warm referral. Second, it is one of just a few current papers that explores the nuts and bolts of recruitment, including how unexpected complications can arise. Working with brokers, in particular, proved effective but complex. Researchers are not always aware of the incentive structures facing our community partners, and this study forced us to learn more about these incentives. Third, there has been little prior research on how readiness for change may differ (or not) by recruitment method.
Conclusion
Our results indicate that leveraging relationships with community partners, including those that are in the private sector, can lead to more efficient recruitment of small, low-wage worksites to workplace health promotion studies. Partnering with entities such as insurers and brokers does come with complexities; researchers have long sensed the important role brokers play in assisting small employer with health insurance decisions (Conwell, 2002) and suspect they may also be pivotal in hindering or facilitating their wellness efforts. The workplace health promotion field would be well served by revealing more about how worksites are recruited for studies, including those with low-wage workforces. The rewards for doing so include more and better resources made available sooner to small, low-wage worksites and their employees.
Acknowledgements
This project was supported by grant 5R01CA160217 from the National Cancer Institute.
Footnotes
Conflict of Interests
The authors declared that they have no competing interests.
Contributor Information
Kristen Hammerback, Health Promotion Research Center, Department of Health Services, University of Washington.
Peggy A. Hannon, Health Promotion Research Center, Department of Health Services, University of Washington.
Amanda T. Parrish, Health Promotion Research Center, Department of Health Services, University of Washington.
Claire Allen, Health Promotion Research Center, Department of Health Services, University of Washington.
Marlana J. Kohn, Health Promotion Research Center, Department of Health Services, University of Washington.
Jeffrey R. Harris, Health Promotion Research Center, Department of Health Services, University of Washington.
References
- Barbeau EM, Wallace L, Lederman R, Lightman N, Stoddard A, & Sorensen G (2004). Recruiting small manufacturing worksites that employ multiethnic, low-wage workforces into a cancer prevention research trial. Preventing Chronic Disease, 1(3), A04. [PMC free article] [PubMed] [Google Scholar]
- Beresford SA, Locke E, Bishop S, West B, McGregor BA, Bruemmer B, … Thompson B (2007). Worksite study promoting activity and changes in eating (PACE): design and baseline results. Obesity, 15(Suppl 1), 4S–15S. [DOI] [PubMed] [Google Scholar]
- Biener L, DePue JD, Emmons KM, Linnan L, & Abrams DB (1994). Recruitment of work sites to a health promotion research trial. Implications for generalizability. Journal of Occupational and Environmental Medicine, 36(6), 631–636. [PubMed] [Google Scholar]
- CDC Task Force on Community Preventive Services. (2014). Guide to Community Preventive Services. Retrieved from www.thecommunityguide.org
- Conwell LJ (2002). The role of health insurance brokers: providing small employers with a helping hand. Issue Brief (Center for Studying Health System Change), 57, 1–4. [PubMed] [Google Scholar]
- Egelhoff C, Katz M, Brosseau LM, & Hennrikus D (2015). Creating a representative sample of small manufacturing businesses for an integrated workplace safety and smoking cessation intervention study. Journal of Occupational and Environmental Medicine, 57(7), 772–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, & Boles SM (1999). Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health, 89(9), 1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammerback K, Hannon PA, Harris JR, Clegg-Thorp C, Kohn M, & Parrish A (2015). Perspectives on workplace health promotion among employees in low-wage industries. American Journal of Health Promotion, 29(6), 384–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannon PA, Garson G, Harris JR, Hammerback K, Sopher CJ, & Clegg-Thorp C (2012). Workplace health promotion implementation, readiness, and capacity among midsize employers in low-wage industries: a national survey. Journal of Occupational and Environmental Medicine, 54(11), 1337–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannon PA, Hammerback K, Allen CL, Parrish AT, Chan KG, Kohn MJ, … Harris JR (2016). HealthLinks randomized controlled trial: Design and baseline results. Contemporary Clinical Trials, 48, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannon PA, Helfrich CD, Chan KG, Allen CL, Hammerback K, Kohn MJ, … Harris JR (2017). Development and pilot test of the workplace readiness questionnaire, a theory-based instrument to measure small workplaces’ readiness to implement wellness programs. American Journal of Health Promotion, 31(1), 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JR, Huang Y, Hannon PA, & Williams B (2011). Low-socioeconomic status workers: their health risks and how to reach them. Journal of Occupational and Environmental Medicine, 53(2), 132–138. [DOI] [PubMed] [Google Scholar]
- Karaca-Mandic P, Feldman R, & Graven P (2016). The role of agents and brokers in the market for health insurance. Journal of Risk and Insurance. [Google Scholar]
- Laing SS, Hannon PA, Talburt A, Kimpe S, Williams B, & Harris JR (2012). Increasing evidence-based workplace health promotion best practices in small and low-wage companies, Mason County, Washington, 2009. Preventing Chronic Disease, 9, E83. [PMC free article] [PubMed] [Google Scholar]
- Linnan L, Emmons KM, Klar N, Fava JL, LaForge RG, & Abrams DB (2002). Challenges to improving the impact of worksite cancer prevention programs: comparing reach, enrollment, and attrition using active versus passive recruitment strategies. Annals of Behavioral Medicine, 24(2), 157–166. [DOI] [PubMed] [Google Scholar]
- Linnan L, Harrington C, Bangdiwala K, & Evenson K (2012). Comparing Recruitment Methods to Enrolling Organizations into a Community-Based Intervention Trial: Results from the NC BEAUTY and Health Project. Journal of Clinical Trials, 2(119). [Google Scholar]
- Linnan L, Tate DF, Harrington CB, Brooks-Russell A, Finkelstein E, Bangdiwala S, … Britt A (2012). Organizational-and employee-level recruitment into a worksite-based weight loss study. Clinical Trials, 9(2), 215–225. [DOI] [PubMed] [Google Scholar]
- Pampel FC, Krueger PM, & Denney JT (2010). Socioeconomic disparities in health behaviors. Annual Review of Sociology, 36, 349–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Kaphingst K, & Wallace L (2005). Promoting behavior change among working-class, multiethnic workers: results of the healthy directions--small business study. American Journal of Public Health, 95(8), 1389–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Stoddard A, Hunt MK, Hebert JR, Ockene JK, Avrunin JS, … Hammond SK (1998). The effects of a health promotion-health protection intervention on behavior change: the WellWorks Study. American Journal of Public Health, 88(11), 1685–1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson B, Hannon PA, Bishop SK, West BE, Peterson AK, & Beresford SA (2005). Factors related to participatory employee advisory boards in small, blue-collar worksites. American Journal of Health Promotion, 19(6), 430–437. [DOI] [PubMed] [Google Scholar]
- Thompson B, van Leynseele J, & Beresford SA (1997). Recruiting worksites to participate in a health promotion research study. American Journal of Health Promotion, 11(5), 344–351. [DOI] [PubMed] [Google Scholar]
- USSBA: U.S. Small Business Administration. (2014). Advocacy: the voice of small business in government. Retrieved Mar 14, 2016 https://www.sba.gov/sites/default/files/advocacy/FAQ_March_2014_0.pdf
- Washington State Employment Security Department. (2016). Quarterly census of employment and wages. Retrieved from https://fortress.wa.gov/esd/employmentdata/reports-publications/industry-reports/quarterly-census-of-employment-and-wages
- Weiner BJ (2009). A theory of organizational readiness for change. Implementation Science, 4, 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt LB, Olsen D, & Ablah E (2013). Motivating factors for small and midsized businesses to implement worksite health promotion. Health Promotion Practice, 14(6), 876–884. [DOI] [PubMed] [Google Scholar]