Abstract
Background
The Ho-Chi-Minh-city Heart Institute in Vietnam took part in the Optimize Heart Failure (OHF) Care Program, designed to improve outcomes following heart failure (HF) hospitalization by increasing patient awareness and optimizing HF treatment.
Methods
HF patients hospitalized with left ventricular ejection-fraction (LVEF) <50% were included. Patients received guideline-recommended HF treatment and education. Clinical signs, treatments and outcomes were assessed at admission, discharge, 2 and 6 months (M2, M6). Patients' knowledge and practice were assessed at M6 by telephone survey.
Results
257 patients were included. Between admission and M2 and M6, heart rate decreased significantly, and clinical symptoms improved significantly. LVEF increased significantly from admission to M6. 85% to 99% of patients received education. At M6, 45% to 78% of patients acquired knowledge and adhered to practice regarding diet, exercise, weight control, and detection of worsening symptoms. High use of renin-angiotensin-aldosterone-system inhibitors (91%), mineralocorticoid-receptor-antagonists (77%) and diuretics (85%) was noted at discharge. Beta-blocker and ivabradine use was less frequent at discharge but increased significantly at M6 (from 33% to 51% and from 9% to 20%, respectively, p < 0.001). There were no in-hospital deaths. Readmission rates at 30 and 60 days after discharge were 8.3% and 12.5%, respectively. Mortality rates at 30 days, 60 days and 6 months were 1.2%, 2.5% and 6.4%, respectively.
Conclusions
The OHF Care Program could be implemented in Vietnam without difficulty and was associated with high usage of guideline-recommended drug therapy. Although education was delivered, patient knowledge and practice could be further improved at M6 after discharge.
Keywords: Heart failure, Optimize, Education, Knowledge, Mortality, Readmission
1. Introduction
Heart failure (HF) is a common public health concern, not only in Europe and the United States (US) but also in Asia [[1], [2], [3], [4], [5]]. Indeed, HF is the leading cause of hospitalization in Europe and the US [2], and rehospitalization rates of nearly 30% have been reported at 2–3 months post-discharge [6]. The prevalence of HF is increasing in low- and middle-income countries due to the increasing prevalence of ischemic heart disease and hypertension [3,5,7]. Recent data show that HF prevalence in South East Asia is similar to global values, with HF accounting for up to 20% of hospitalizations and 30-day readmission rates of up to 15% (approximately 8% in Indonesia, Malaysia and Vietnam, 15% in Taiwan) [8]. Moreover, an increase in cardiovascular risk factors such as obesity, hypertension, and diabetes, related to changes in lifestyles in these countries, is likely responsible for the rise in HF prevalence [4,5,7,9].
Despite advances in treatment, readmission rates and mortality associated with HF remain high worldwide [5,10,11], resulting in high social and economic burden, particularly in low- and middle-income countries [8]. Several studies have highlighted the need for patient education and recall of lifestyle advice in order to optimize HF treatment and to improve HF outcomes [[12], [13], [14]].
Very few data have been published about heart failure in Vietnam. Hospitalization for HF in the Hanoi Heart Hospital in Vietnam accounts for 15% of total hospitalizations. The estimation of the average cost of HF hospitalization reported by this hospital is about 1000 US dollars/patient [8]. The GDP per capita in Vietnam is about 2481 US dollars. The financial burden of HF, principally due to the cost of hospitalization, appears important in Vietnam. The Ho-Chi-Minh city Heart Institute, the first specialized cardiovascular center in Vietnam, has taken part in the Optimize Heart Failure (OHF) Care Program since October 2016, serve as reference for other center/hospital in Vietnam, giving an opportunity to implement evidence-based medicine and enrich the available data on HF management in low- and middle-income countries.
The objectives of the OHF Care Program in our Institute are to improve HF patient outcomes by improving patient awareness of their condition, and by optimizing HF treatment according to a locally-agreed guideline (with checklists to improve guideline adherence in hospital and at subsequent clinic review) [15].
2. Methods
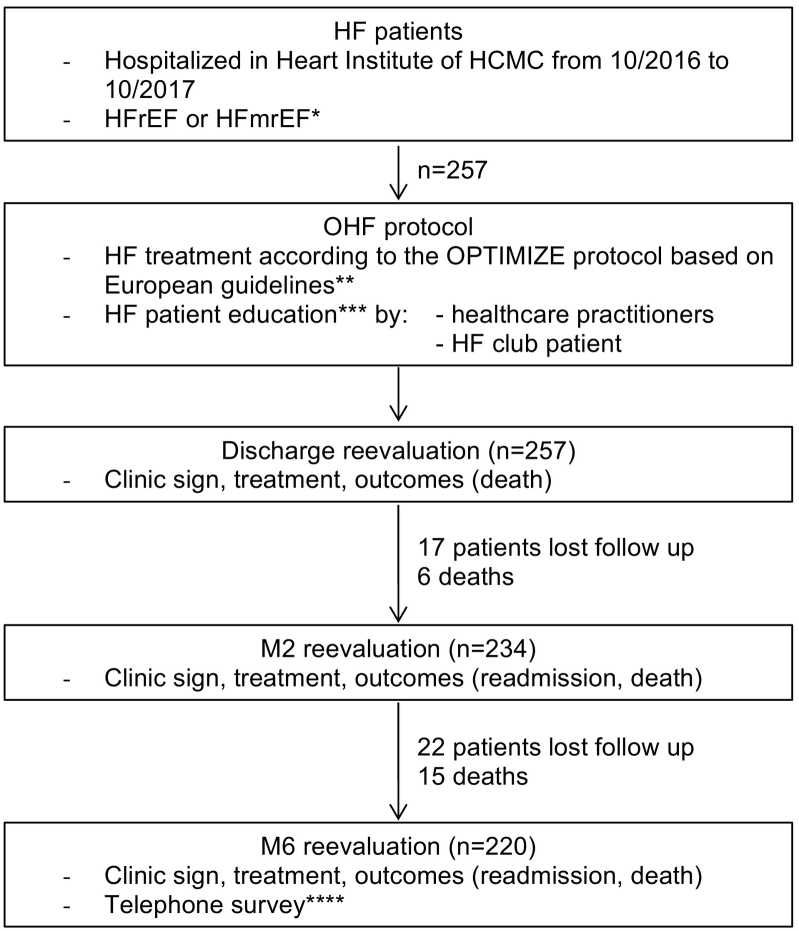
In this Program, we included all HF patients with left ventricular ejection fraction (LVEF) documented by echocardiography to be <50% and other echocardiography ESC criteria for HF mid-range EF (left ventricular hypertrophy and/or left atrial enlargement), hospitalized in Ho-Chi-Minh city Heart Institute from October 2016 to October 2017 (Fig. 1). Patients received HF treatment according to the OPTIMIZE protocol based on European guidelines (except angiotensin receptor neprilysin inhibitor that we do not have yet). HF patient education was directly delivered by healthcare practitioners (in hospital and in clinic after discharge), and through activities of the “HF club” patient support group, about the following 4 educational themes: diet (especially how to reduce salt intake, fat intake, and to achieve fluid restriction), exercise, weight control at home (recommending weighting every two weeks or one month, on the same day of the week and the same time of the day) and/or detection of worsening HF symptoms at home (such as dyspnea worsening, gain of >2 kg in two weeks, bloating, or oedema in the lower limbs).
Fig. 1.
Study design.
HF: heart failure; HCMC: Ho Chi Minh City; HFrEF: heart failure with reduced ejection fraction; HFmrEF: heart failure with mid-range ejection fraction; OHF: optimized heart failure care program; M2: at 2 months post discharge; M6: at 6 months post discharge.
* HFrEF: LVEF <40% documented by echocardiography; HFmrEF: 40% ≤ LVEF <50% and ESC criteria for HFmrEF (left ventricular hypertrophy and/or left atrial enlargement) documented by echocardiography.
** Except angiotensin receptor neprilysin inhibitor that we do not have yet.
*** 4 educational themes: diet (especially how to reduce salt intake, fat intake, and to achieve fluid restriction), exercise, weight control at home (recommending weighting every two weeks or one month, on the same day of the week and the same time of the day) and/or detection of worsening HF symptoms at home (such as dyspnea worsening, gain of >2 kg in two weeks, bloating, or oedema in the lower limbs).
**** Education/knowledge has been tested by a questionnaire conducted by 2 trained secretaries. The patients was asked if they heard the doctor's advice, described what was heard about diet, exercise, weight control and detection of worsening HF symptoms at home, and described what they had done at home, how they felt when done.
Data on clinical signs, treatment and outcomes (readmission and death at 30 days, 60 days and 6 months after discharge) were collected at admission (M0), discharge, 2 months (M2) and 6 months (M6) after discharge. LVEF was evaluated by echocardiography on admission and within 6 months post-discharge. For each HF pharmaceutical treatment, we recorded the proportion of patients who received ≥50% of target dose and the proportion of patients with contra-indication or intolerance, based on 2016 European guidelines [16]. We also performed a telephone survey with a questionnaire at 6 months after discharge to assess patient knowledge and practice on the four educational themes (except the practice of “detection of worsening HF symptom” was not measured). Education/knowledge has been tested by a questionnaire conducted by 2 trained secretaries only for telephone survey. The patients was asked if they heard the doctor's advice, described what was heard about diet, exercise, weight control and detection of worsening HF symptoms at home, and described what they had done at home, how they felt when done.
2.1. Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 22.0 and Microsoft Office Excel 2010. Normal distribution of the data was tested by means of the Kolmogorov-Smirnov test. Continuous variables are presented as mean ± standard deviation (SD) and categorical variables as number (n) and percentage (%). To determine the difference between the groups with continuous variables, we used Student's t-test; with categorical variables, we used chi-square test when there was a sufficient number of observations and Fisher's test when there were not. A p < 0.05 was considered as indicating statistical significance.
The survey was conducted according to the rules of the declaration of Helsinki and was approved by relevant ethical committees. All patients gave written informed consent to participate.
3. Results
From October 2016 through October 2017, we recruited 257 HF patients with LVEF <50% (nearly 70% chronic and 30% acute HF), hospitalized in our Institute. The baseline characteristics including age, gender, literacy, body mass index (BMI), systolic and diastolic blood pressure, hospitalization causes, etiology and co-morbidities are presented in Table 1.
Table 1.
Baseline characteristics of hospitalized heart failure patients with ejection fraction <50%.
| N = 257 | |
|---|---|
| Age (mean ± SD, years) | 64.4 ± 15.0 |
| Gender n (%) | |
| ▪ Men | 149 (58%) |
| ▪ Women | 108 (42%) |
| Literacy n (%) | |
| ▪ Primary school | 57 (22%) |
| ▪ High school | 190 (74%) |
| ▪ University | 10 (4%) |
| ▪ Post university | 0 (0%) |
| Hospitalization causes: n (%) | |
| ▪ Acute decompensated heart failure | 123 (47.9%) |
| ▪ Acute coronary syndrome | 97 (37.8%) |
| ▪ Arrhythmia | 15 (5.8%) |
| ▪ Infection (pulmonary, valvular, urinary, sepsis) | 15 (5.8%) |
| ▪ Other | 7 (2.7%) |
| Disease etiology for heart failure: n (%) | |
| ▪ Ischemic heart disease | 165 (64.2%) |
| ▪ Cardiomyopathy (essentially dilated cardiomyopathy) | 56 (21.8%) |
| ▪ Valvular heart disease | 24 (9.3%) |
| ▪ Arrhythmia | 6 (2.3%) |
| ▪ Other | 6 (2.3%) |
| Co-morbidities: n (%) | |
| ▪ Hypertension | 124 (48.2%) |
| ▪ Valvular heart disease | 104 (40.5%) |
| ▪ Overweight/obesity | 50/53 (40.1%) |
| ▪ Dyslipidemia | 85 (33.1%) |
| ▪ Arrhythmia including atrial fibrillation | 80 (31.1%) |
| ▪ Diabetes mellitus | 66 (25.7%) |
| ▪ Renal insufficiency | 54 (21.0%) |
| ▪ Cerebrovascular disease | 13 (5.0%) |
| ▪ COPD or asthma | 9 (3.5%) |
BMI: body mass index; COPD: chronic obstructive pulmonary disease; SD: standard deviation; Obesity: BMI ≥ 25; valvular heart disease was defined by mitral or aortic regurgitation more than grade 2/4, or/and valvular stenosis more than middle degree or/and valvular replacement; overweight: 23 ≤ BMI < 25; renal insufficiency was defined by eGFR <60 ml/p or presence of “renal insufficiency” in the previous diagnosis.
17 patients were lost to follow-up at M2 and 5 more patients at M6 (not including death, they decided to continue their survey in local hospital to have insurance reimbursement).
There was a significant fall in mean heart rate (HR) between admission (M0) and discharge (97.8 ± 22.2 vs. 78.5 ± 11.7, p < 0.001) and this change persisted to M6 (78.9 ± 13.6). We noted that the prevalence of atrial fibrillation was somewhat lower on admission than at M6 (22% vs. 29%, p = 0.09). The clinical signs were improved at M2 and M6 compared to M0 (Table 2). The New York Heart Association (NYHA) classification distribution similarly improved significantly at M2 and M6 compared to M0 (proportion of patients with NYHA class I&II rising from 46% at M0 to 97% at M2 and 99% at M6, both p < 0.001 compared to M0) (Table 2). The LVEF also increased modestly but significantly (36% ± 9 within M6 vs. 33% ± 9 at M0, t(229) = −4.140, p < 0.001).
Table 2.
Clinical characteristics at admission (M0), month 2 (M2) and month 6 (M6).
| n = 257 patients | M0 n = 257 |
M2 n = 234 |
M6 n = 220 |
p value M0 vs. M2 |
p value M2 vs. M6 |
|---|---|---|---|---|---|
| Clinical sign, n (%) | |||||
| ▪ Dyspnea | 205 (79.8%) | 85 (36.3%) | 49 (22.2%) | <0.001 | 0.002 |
| ▪ Orthopnea | 102 (39.7%) | 3 (1.2%) | 0 (0%) | <0.001 | 0.25 |
| ▪ Pulmonary congestion | 66 (27.3%) | 1 (0.4%) | 0 (0%) | <0.001 | 0.65 |
| NYHA I&II, n (%) | 117 (45.5%) | 228 (97.4%) | 218 (99.1%) | <0.001 | <0.001 |
| NYHA III&IV, n (%) | 140 (54.5%) | 6 (2.6%) | 2 (0.9%) | <0.001 | <0.001 |
NYHA: New York Heart Association.
In terms of patient education, although the percentages of patients who received education about diet, exercise, weight control at home and detection of worsening HF symptoms at home were high (over 85%), the percentages of patients who showed knowledge and reported adhering to the practice, as assessed by the telephone survey at M6, were moderate (Table 3).
Table 3.
Patient education, knowledge and practice.
| Education in hospitala n = 257 |
Knowledge of patient at M6b n = 220 |
Practice by patient and family at M6b n = 220 |
|
|---|---|---|---|
| Diet, n (%) | 254 (98.8%) | 159 (72.3%) | 171 (77.7%) |
| Exercise, n (%) | 219 (85.2%) | 147 (66.8%) | 138 (62.7%) |
| Weight control at home, n (%) | 230 (89.5%) | 119 (54.1%) | 98 (44.5%) |
| Detection of worsening HF symptoms at home, n (%) | 236 (91.8%) | 124 (56.4%) | Not measured |
Patient education was assessed by cardiologists; patient knowledge and practice were assessed at M6 by telephone survey.
Education/knowledge has been tested by a questionnaire conducted by 2 trained secretaries only for telephone survey. The patients was asked if they heard the doctor's advice, described what was heard about diet, exercise, weight control and detection of worsening HF symptoms at home, and described what they had done at home, how they felt when done.
For HF pharmaceutical treatment (Table 4), we followed European guidelines with: 91% of patients prescribed a renin-angiotensin system inhibitor (RAS) at discharge, 33% beta-blockers (BB) (rising to 50.5% at M6, p < 0.001), 77% mineralocorticoid receptor antagonists (MRA), 85% diuretics, 9% ivabradine (rising to 20.0% at M6 for HF patients with NYHA II-IV and sinus rhythm), 33% digoxin (with 23% treated for AF) and 16% isosorbide dinitrate. Although the percentages of patients who received ≥50% target dose of beta-blockers (BB) and of ivabradine were not high at discharge (12% for BB and 44% for ivabradine), these percentages significantly increased at M6 (36% for BB and 73% for ivabradine, p < 0.001 for M6 vs. discharge). MRAs were used with high prevalence of ≥50% target dose (90% for MRAs). The proportion of patients on MRA rose significantly at M6 compared with discharge (96% vs. 90%, p < 0.001).
Table 4.
Heart failure pharmaceutical treatment.
| Discharge n = 257 |
M6 n = 220 |
p value | |
|---|---|---|---|
| ACEIs/ARBs, n (%) | 235 (91.4%) | 173 (79.5%) | <0.001 |
| ▪ ≥50% of target dose, n (%) | 92 (41.8%) | 78 (45.1%) | 0.5 |
| ▪ Contra-indication or intolerant, n (%) | 22 (8.6%) | 25 (11.4%) | 0.5 |
| Beta-blockers, n (%) | 85 (33.1%) | 111 (50.5%) | <0.001 |
| ▪ ≥50% of target dose, n (%) | 10 (11.8%) | 40 (36.0%) | <0.001 |
| ▪ Contra-indication or intolerant, n (%) | 75 (29.2%) | 60 (27.3%) | NS |
| MRA, n (%) | 198 (77.0%) | 144 (65.5%) | <0.001 |
| ▪ ≥50% of target dose, n (%) | 178 (89.9%) | 138 (95.8%) | <0.001 |
| ▪ Contra-indication or intolerant, n (%) | 27 (10.5%) | 24 (10.9%) | NS |
| Diuretics, n (%) | 219 (85.2%) | 163 (74.1%) | <0.001 |
| ▪ ≥50% of target dose, n (%) | 175 (79.9%) | 124 (76.1%) | 0.5 |
| ▪ Contra-indication or intolerant, n (%) | 8 (3.1%) | 12 (5.5%) | NS |
| Ivabradine, n (%) | 23 (8.9%) | 44 (20.0%) | <0.001 |
| ▪ ≥50% of target dose, n (%) | 10 (43.5%) | 32 (72.7%) | <0.001 |
| ▪ Contra-indication or intolerant, n (%) | 102 (39.7%) | 88 (40.0%) | NS |
| Digoxin, n (%) | 84 (32.7%) | 73 (33.2%) | NS |
| Nitrate, n (%) | 102 (39.6%) | 76 (34.5%) | 0.005 |
| ▪ ISDN, n (%) | 42 (16.3%) | 36 (16.4%) | NS |
| ▪ ISMN, n (%) | 60 (23.3%) | 40 (18.1%) | 0.005 |
ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; ISDN: isosorbide dinitrate; ISMN: isosorbide mononitrate; MRA: mineralocorticoid receptor antagonist; NS: non statistical significance, p > 0.5.
The readmission rate at 30 days was 8.3% and at 60 days it was 12.5%. There were no in-hospital deaths. The mortality rate at 30 days after discharge was 1.2% (n = 3), rising to 2.5% (n = 6) at 60 days and to 6.4% (n = 15) at 6 months. The causes of death were worsening HF (n = 6), stroke (n = 4) and undefined raison (n = 5).
4. Discussion
We recruited 257 HF patients with LVEF <50% hospitalized in our Institute, the data clearly show a significant improvement in HF clinical signs at M6 compared to admission, accompanied by a significant improvement in mean heart rate and LVEF between M6 and admission.
Our Vietnamese HF patients, similarly to what has been observed in other South-East Asian countries (Indonesia, Malaysia, Philippines), are on average younger (58–64 years old) than in Europe (70 years), UK (80 years), US (74 years) and some Asian countries such as Hong Kong (77 years), Japan (73 years) and Korea (69 years) [[3], [4], [5],8,11]. This variation in age at admission for HF among Asian countries might be attributed to several factors including average life expectancy and stages of epidemiological transition [5,11,17]. There were more men (58%) than women in our population, but their percentage was similar to that reported in studies in Europe, US and other Asian countries [5,8,11].
The most frequent causes for hospitalization reported in our study were acute decompensated HF and acute coronary syndrome. The main etiologies were ischemic heart disease (64%) and dilated cardiomyopathy (22%). These results reflect the epidemiological transition from infection-related disease to non-communicable diseases, with the progressive disappearance of rheumatic valvular heart disease and the increase of ischemic heart disease, with social economic change in low- and middle-income countries [5,11,18]. Similarly, the main co-morbidities with HF are common cardiovascular risk factors, such as hypertension, dyslipidemia, overweight/obesity, diabetes mellitus, with frequency comparable to other Asian country, related to develop social economic situation and to changing lifestyles in Asia, particularly with higher fat intake, decrease in physical activity and presence of more stress [5,9,11,18].
Regarding HF patient outcomes, there were no in-hospital deaths and the rate of readmission after discharge at 30 days and 60 days was 8.3% and 12.5%, respectively. These results are better than those showed in registry without OHF Care Program [5,11] in several Asian centers and are the same as those shown in registry with OHF Care Program [8]. The mortality rate at 30 days after discharge in our population was 1.2%, similar to that noted in Malaysia but lower than those of Indonesia or Philippine or Russian, in which the OHF Care Program was involved [8,19]. Nevertheless, our mortality rates at 2 and 6 months after discharge are higher than those recently demonstrated in Russia [19].
In terms of patient education about heart failure, several studies have shown the necessity for and effectiveness of advice about lifestyle on better adherence to self-management strategies, improved quality of life and better prognosis among patients with HF [12,14,[20], [21], [22]]. In our OHF Care Program, a very high percentage of patients were educated about these four HF themes (99% for HF diet, 92% for detection of worsening HF symptom at home, 89% for weight control at home and 85% for appropriate exercise). The telephone survey at 6 months post-discharge showed that the percentage of patients retaining this knowledge and adhering to the practice was only moderate (72% and 78% for diet, 67% and 63% for exercise, 54% and 45% for weight control at home respectively, and only 56% of patients remember the education about detection of worsening HF symptom). Although only moderate, these rates seem to be higher than those reported by other surveys without OHF Care Program implementation. A trial in 2411 metropolitan Worcester residents hospitalized at 11 area medical centers, reported that provision of advice was documented on salt intake in 84%, low fat diet in 69%, increasing physical activity in 33%, regular weighing in 21%, and fluid restriction in 23% [21]. Another smaller prospective German study found that 51% of patients recalled receiving advice on regular weighting and 41% weighed themselves regularly one year after discharge [23]. In order to understand why the recall and implementation of advice is poor, qualitative studies are required as it is unclear whether patients had forgotten about the received advice or had chosen not to follow it. The authors concluded that it is insufficient merely to inform the patients about self-care behavior; instead, information has to be adapted to the actual needs and circumstances of the individual patient and the health professional should ensure that patients receive and understand advice, and are able to recall and follow it [13]. In our study, we did not have the data concerned this notion, but our registry have been showed that nearly 96% of them have literacy from secondary school or below. This may explain a part of the ability to understand the doctors' advices and need to re-establish advisory information many times so they can remember and implement them. Recently, a randomized clinical trial conducted on 100 patients with chronic HF showed that intensive education program (group education and telephone call within six consecutive weeks) about dietary sodium restriction for patients and their family members is more efficacious than routine education about sodium intake reduction [24]. In our Program, we educated patients about 4 HF themes above in hospital and in the out-patient visit after discharge, followed by a group education by club patients and their relatives, and with a check for information recall at six months post discharge. The percentage of HF patients who acquired this knowledge and adhered to the practice was only moderate, which might be affected by the general educational level of the population, the ability of patients and their relatives to receive and understand information and the ability of patients to change their habitual lifestyle. We believe we can do better in training our practitioners and nurses about counseling skills and continuing to remind and encourage our HF patients in their self-management at each out-patient visit.
In regard to the HF pharmaceutical treatment, it is clear that the OHF Care Program favors a net improvement in prescription of guidelines-recommended drug therapies in our Institute.
For RAAS, MRA and diuretic therapies, prescription rates were the same as in Europe [5,8,24,25] and higher than in other Asian countries and in USA [5,8,25]. These rates were lower at 6 months than at discharge, which may be associated with an increase in contra-indication or intolerance rates and with improvement in patient's clinical symptoms or NYHA classification. However, the rate of patients achieving ≥50% target dose for RAAS was not high at discharge or M6; this may be related to the lower tolerance in Asian HF patients (who have lower BMI) than in Caucasian patients, and lower blood pressure in our patients.
For beta-blockers and ivabradine, we found low rate of prescription at discharge, similar to other Asian countries (e.g. Hong Kong, Indonesia, Philippines) [8], but a significant increase was observed by M6, as well as the rate of patients achieving ≥50% target dose. This result may reflect the impact of the OHF Care Program on physician adherence to international guidelines and favors a significant improvement of mean heart rate in our HF patients at M6. The effect of optimization of heart rate-lowering therapy with beta-blocker and ivabradine on overall mortality and re-hospitalization over the subsequent 12 months in hospitalized HF patients was recently demonstrated [19], highlighting the importance of further improvement of adherence to guidelines to improve outcomes in HF patients.
From these results about target dose, we are conducting a real-world survey to determine principal causes for low rate of achieve target dose in Vietnamese HF patients, who have difference profile than Caucasian patients and may have difference target dose than others.
4.1. Study limitations
This study was subject to limitations inherent in its design (observational survey, without control group, conducted in one specialist center in Vietnam) which may have resulted in selection bias, in the estimation of education and treatment effects. Nevertheless, this survey assessed outcomes in regular clinical practice, reflecting adherence of practitioners to treatment guidelines and also patients' knowledge and adherence to advice in a real-world setting in Vietnam, a country from which data are lacking. After this pilot survey, the next follow-up manuscript will complete the lack of information regarding the determination of HF biological markers (such as NT-proBNP), the reasons for low beta-blockade usage and not obtaining the target dose of HF medication, and more detailed explanations about patient implementation of HF advice.
5. Conclusion
We have shown that the Optimize Heart Failure Care Program can be implemented in a middle-income country such as Vietnam without difficulty. Symptom control appears good during follow-up. Education was provided to a high proportion of patients, although patients did not always retain the information or follow the advice. The use of drug therapy (other than for beta-blockers) is good when compared with other countries. Low readmission and mortality rates may have beneficial on social-economic impact. This survey serves as reference for other center/hospital in Vietnam to implement OHF care program and can lead to other work more complete.
Conflicts of interest
Thi Nam Phuong DO has received speaker fees from Astra Zeneca, Boehringer Ingelheim, MSD, Novartis, Sanofi Aventis, Servier and investigator research from Astra Zeneca, MSD, Servier.
Quang Huan DO has received speaker fees from Abbott, Astra Zeneca, Boehringer Ingelheim, MSD, Novartis, Sanofi Aventis, Servier and principal investigator research from Astra Zeneca, MSD, Servier.
Martin R. COWIE has received speaker and consultancy fees from Servier.
Funding
This study was funded by Heart Institute of Ho Chi Minh city, Viet Nam and Servier, France.
Acknowledgments
We thank Weiwei.li-Bertheau who provided medical writing assistance.
References
- 1.Bui A.L., Horwich T.B., Fonarow G.C. Epidemiology and risk profile of heart failure. Nat. Rev. Cardiol. 2011;8(1):30–41. doi: 10.1038/nrcardio.2010.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ambrosy A.P. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J. Am. Coll. Cardiol. 2014;63(12):1123–1133. doi: 10.1016/j.jacc.2013.11.053. [DOI] [PubMed] [Google Scholar]
- 3.Guo Y., Lip G.Y., Banerjee A. Heart failure in East Asia. Curr. Cardiol. Rev. 2013;9(2):112–122. doi: 10.2174/1573403X11309020004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harikrishnan Sivadasan P., Sanjay G. Heart failure in South Asia. Curr. Cardiol. Rev. 2013;9(2):102–111. doi: 10.2174/1573403X11309020003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sakata Y., Shimokawa H. Epidemiology of heart failure in Asia. Circ. J. 2013;77(9):2209–2217. doi: 10.1253/circj.cj-13-0971. [DOI] [PubMed] [Google Scholar]
- 6.Gheorghiade M. Rehospitalization for heart failure: problems and perspectives. J. Am. Coll. Cardiol. 2013;61(4):391–403. doi: 10.1016/j.jacc.2012.09.038. [DOI] [PubMed] [Google Scholar]
- 7.Sanderson J., Tse T. BMJ Publishing Group Ltd.; 2003. Heart Failure: A Global Disease Requiring a Global Response. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reyes E.B. Heart failure across Asia: same healthcare burden but differences in organization of care. Int. J. Cardiol. 2016;223:163–167. doi: 10.1016/j.ijcard.2016.07.256. [DOI] [PubMed] [Google Scholar]
- 9.Lee S., Khurana R., Leong K.T.G. Heart failure in Asia: the present reality and future challenges. Eur. Heart J. Suppl. 2012;14(suppl_A):A51–A52. [Google Scholar]
- 10.Cleland J.G. The EuroHeart Failure survey programme — a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur. Heart J. 2003;24(5):442–463. doi: 10.1016/s0195-668x(02)00823-0. [DOI] [PubMed] [Google Scholar]
- 11.Shimokawa H. Heart failure as a general pandemic in Asia. Eur. J. Heart Fail. 2015;17(9):884–892. doi: 10.1002/ejhf.319. [DOI] [PubMed] [Google Scholar]
- 12.Krumholz H.M. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J. Am. Coll. Cardiol. 2002;39(1):83–89. doi: 10.1016/s0735-1097(01)01699-0. [DOI] [PubMed] [Google Scholar]
- 13.Lainscak M. Recall of lifestyle advice in patients recently hospitalised with heart failure: a EuroHeart Failure Survey analysis. Eur. J. Heart Fail. 2007;9(11):1095–1103. doi: 10.1016/j.ejheart.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Gonseth J. The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-analysis of published reports. Eur. Heart J. 2004;25(18):1570–1595. doi: 10.1016/j.ehj.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 15.Cowie M.R. The Optimize Heart Failure Care Program: initial lessons from global implementation. Int. J. Cardiol. 2017;236:340–344. doi: 10.1016/j.ijcard.2017.02.033. [DOI] [PubMed] [Google Scholar]
- 16.Ponikowski P. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 17.Atherton J.J. Patient characteristics from a regional multicenter database of acute decompensated heart failure in Asia Pacific (ADHERE International-Asia Pacific) J. Card. Fail. 2012;18(1):82–88. doi: 10.1016/j.cardfail.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Yusuf S. 104(22) 2001. Global Burden of Cardiovascular Diseases. Part I: General Considerations, the Epidemiologic Transition, Risk Factors, and Impact of Urbanization; pp. 2746–2753. [DOI] [PubMed] [Google Scholar]
- 19.Lopatin Y.M. Optimization of heart rate lowering therapy in hospitalized patients with heart failure: insights from the Optimize Heart Failure Care Program. Int. J. Cardiol. 2018;260:113–117. doi: 10.1016/j.ijcard.2017.12.093. [DOI] [PubMed] [Google Scholar]
- 20.Lainscak M. Nonpharmacologic measures and drug compliance in patients with heart failure: data from the EuroHeart Failure Survey. Am. J. Cardiol. 2007;99(6b):31d–37d. doi: 10.1016/j.amjcard.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Goldberg R.J. Use of nonpharmacologic treatment approaches in patients with heart failure. Int. J. Cardiol. 2006;110(3):348–353. doi: 10.1016/j.ijcard.2005.07.026. [DOI] [PubMed] [Google Scholar]
- 22.Lainscak M., Keber I. Patients' knowledge and beta blocker treatment improve prognosis of patients from a heart failure clinic. Eur. J. Heart Fail. 2006;8(2):187–190. doi: 10.1016/j.ejheart.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Scherer M. Transformation of general measures by patients in heart failure. Dtsch. Med. Wochenschr. 2006;131(13):667–671. doi: 10.1055/s-2006-933712. [DOI] [PubMed] [Google Scholar]
- 24.Akhondzadeh K., Najafi Ghezeljeh T., Haghani H. The effect of the education program on the adherence intention to the dietary sodium restriction and the amount of sodium intake in patients with chronic heart failure. Iran Red Crescent Med J. 2018:e12925. (In Press) [Google Scholar]
- 25.Youn Y.J. Treatment performance measures affect clinical outcomes in patients with acute systolic heart failure- report from the Korean Heart Failure Registry. Circ. J. 2012;76(5):1151–1158. doi: 10.1253/circj.cj-11-1093. [DOI] [PubMed] [Google Scholar]