Abstract
Intra-articular glenohumeral injection is an important technique used to diagnose and treat shoulder disorders. However, it is frequently performed as an image-guided technique with the use of fluoroscopy, ultrasound, computed tomography, or magnetic resonance. The purpose of this Technical Note is to describe a transcoracoacromial ligament glenohumeral injection technique that uses anatomic surface landmarks to avoid the need for radiographic guidance. After identification of the anterolateral corner of acromion, the superior lateral border of the coracoid tip, and the curved depression of the distal clavicle, the needle entry site is determined at the trisection point between the distal and middle thirds of the line formed by the superior lateral border of the coracoid tip and the curved depression of the distal clavicle. The needle is first inserted perpendicular to the triangular plane of the 3 points and is then advanced toward the humeral head. This injection technique is highly accurate and reproducible and can be done in the outpatient clinic without the use of imaging guidance, reducing the costs and barriers of intra-articular glenohumeral injections for patients.
Intra-articular glenohumeral injection is a crucial technique for diagnosing and treating shoulder disorders1 and is routinely used by a variety of providers, including orthopaedic surgeons, rheumatologists, sports medicine specialists, primary care physicians, pain management specialists, and radiologists. Numerous techniques have been developed for glenohumeral injections since the introduction of shoulder arthrography and include fluoroscopy-guided,2, 3 ultrasound-guided,2, 3 and blind techniques.4 Accuracy rates of image-guided techniques are high and reproducible in awake patients, ranging from 63% to 100% for fluoroscopy-guided injection and 92% to 96% for ultrasound-guided injection.2, 3 Because of this reliability, radiographic guidance is frequently used for glenohumeral injections despite the significant disadvantages it may pose. These disadvantages include (1) the need for special imaging equipment, (2) the steep learning curve associated with the ultrasound-guided glenohumeral injection technique, and (3) radiation exposure and the potential side effects and cost of iodinated contrast material for fluoroscopy-guided injection.
Unguided glenohumeral injection techniques may offer an alternative to avoid such disadvantages; however, they may be less reliable with often lower accuracy rates compared with guided injection techniques.5 To date, there is no established technique for an accurate and reproducible unguided glenohumeral injection, despite the benefits of an accurately targeted injection for patients with shoulder symptoms, such as improved responses to therapeutic medications and reduced injury to surrounding structures.6, 7 The purpose of this Technical Note is to describe an unguided transcoracoacromial ligament glenohumeral injection technique8 that utilizes the geometry of bony surface landmarks for routine use in the outpatient clinic without radiographic guidance.
Surgical Technique
Preparation
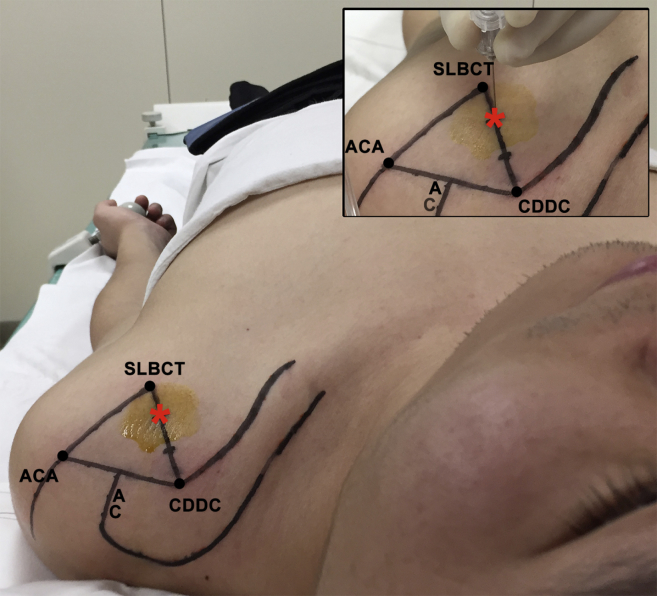
The patient is placed supine with the head at neutral position facing up. The shoulder is positioned in external rotation so that the arm is relaxed at the side with the palm facing up as much as possible to allow greater exposure of the anterior articular surface of the humeral head (Fig 1).
Fig 1.
Superior overall view of patient's position and left shoulder. The patient is positioned supine on the fluoroscopy table. The arm is positioned at the side while keeping palm externally rotated and the head facing up in neutral position. Three bony landmarks are accurately identified and marked over the skin: the anterolateral corner of the acromion (ACA), the superior lateral border of the coracoid tip (SLBCT), and the curved depression of the distal clavicle (CDDC). The acromioclavicular joint (AC) is approximately located at the midpoint of line segment ACA-CDDC. The entry site (*) is identified as the trisection point between the distal and middle thirds of line segment SLBCT-CDDC.
The anterolateral corner of the acromion (ACA), the superior lateral border of the coracoid tip (SLBCT), and the curved depression of the distal clavicle (CDDC) are identified by means of palpation and marked over the skin (Fig 1). After these 3 bony landmarks have been identified, a triangle is then created by connecting the ACA, SLBCT, and CDDC. The SLBCT-CDDC line segment is trisected with the injection entry point lying between the middle and distal thirds of the trisection (Fig 1).
Injection
The injection site is sterilely prepared. A 22-gauge, 65-mm-long needle connected to a short piece of extension tubing is punctured through the skin at the injection site at an angle perpendicular to the triangular ACA-SLBCT-CDDC plane (Fig 1). The needle is then advanced toward the humeral head until an endpoint is reached at the humeral head cartilage (Fig 2). The humeral head cartilage should feel characteristically soft and spongy and is the desired injection location.
Fig 2.
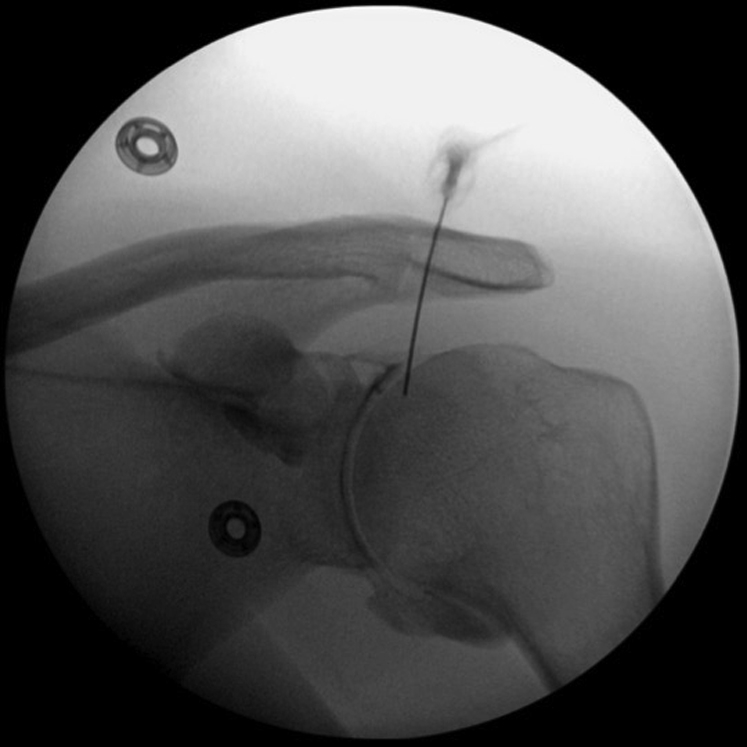
Anterior fluoroscopic view of left shoulder of patient positioned supine with arm externally rotated at the side, showing the needle positioned under the C-arm. The needle tip is in contact with the humeral head, which ensures that it has entered the capsule space of the glenohumeral joint. Fluoroscopy is performed for demonstration and research purposes only and is not required for this technique.
If no endpoint is found after the needle has been advanced two-thirds of the way in (approximately 40 mm), the needle tip has likely been inserted into the soft tissue surrounding the glenohumeral joint and is not actually inside the glenohumeral joint space (Table 1). In such a case, the needle is withdrawn so that the tip sits in the subcutaneous layer to allow for easier manipulation and is then redirected more laterally, posteriorly, and superiorly by rotating the needle hub about 20° toward the patient's chin with the patient's head still facing upward in neutral position.
Table 1.
Pearls and Pitfalls of Transcoracoacromial Ligament Glenohumeral Injection Technique
| Pearls | Pitfalls |
|---|---|
|
|
ACA, anterolateral corner of acromion; CDDC, curved depression of distal clavicle; SLBCT, superior lateral border of coracoid tip.
If there is bony resistance following shallow advancement of the initial needle insertion, then the needle tip has likely reached the cortical bone of the coracoid process instead of the desired humeral head cartilage. In this situation, the first solution is to redirect the needle while keeping the same entry site as explained in the previous case. The second solution is to reinsert the needle at a new insertion site approximately 7 mm toward the ACA and advance the needle in the usual manner, first perpendicular to the triangular plane and then toward the humeral head. The first solution is preferred to minimize puncture trauma and preserve patient tolerance.
After successful intra-articular placement of the needle, a solution of 2.5 mL of 1% anesthetic (lidocaine hydrochloride) and 1 mL of compound betamethasone (Diprospan, 5 mg of betamethasone dipropionate and 2 mg of betamethasone sodium phosphate in 1 mL; Merck) is injected. The patient's shoulder is then carefully exercised to allow even distribution of the injected medications.
After Injection
Patients are observed for complications for at least 30 minutes after injection and are given instructions for clinic follow-up in case of any adverse effects.
Discussion
This Technical Note demonstrates a transcoracoacromial ligament glenohumeral injection technique that does not require radiographic guidance (Video 1). Both the standardized injection protocol and the accurate identification of bony landmarks and entry site allow this technique to be highly reproducible for the outpatient clinic.
Glenohumeral corticosteroid injection is routinely performed to treat idiopathic adhesive capsulitis and has been shown to provide symptomatic relief by inhibiting inflammation and production of prostaglandin.9 However, the therapeutic benefits of the injection are largely affected by injection accuracy.6, 7 Glenohumeral injections are therefore often performed with imaging guidance to achieve high accuracy rates,2, 3 despite the drawbacks imaging guidance can confer.
The transcoracoacromial ligament glenohumeral injection technique has many advantages because of the avoidance of radiographic guidance (Table 2). This technique allows glenohumeral injections to be done more frequently and in the outpatient clinic without the need for special imaging equipment. In addition, no difficult learning curve is associated with the technique as seen in ultrasound-guided glenohumeral injection technique. Most importantly, the transcoracoacromial ligament glenohumeral injection technique benefits the patient by minimizing radiation exposure and avoiding the cost and possible side effects of iodinated contrast material required for a fluoroscopy-guided injection.
Table 2.
Advantages and Disadvantages of Using Bony Surface Landmarks for Transcoracoacromial Ligament Glenohumeral Injection Technique
| Advantages | Disadvantages |
|---|---|
|
|
The bony landmarks used with the transcoracoacromial ligament glenohumeral technique also follow intrinsic geometric relationships relative to each other, allowing this technique to be highly reproducible in locating the injection site. The acromioclavicular joint can be reliably identified as the midpoint of the ACA-CDDC line segment, allowing the CDDC to be located as equidistant and opposite the acromioclavicular joint -ACA line segment. The ACA-SLBCT-CDDC triangle is approximately isosceles with the ACA-SLBCT and SLBCT-CDDC congruent in length, which may be helpful for landmark localization.
This technique is limited by its reliance on adequate palpation and outlining of the ACA, SLBCT, CDDC, and their relevant geometries, which makes it difficult to use for patients with significant obesity or musculoskeletal shoulder deformities. The technique has been performed by an experienced shoulder fellowship-trained orthopaedic surgeon at the time of this writing; therefore, the learning curve is still unclear and the technique may not be appropriate for all providers.
The transcoracoacromial ligament glenohumeral injection technique uses the bony surface landmarks of the acromion, coracoid tip, and clavicle to offer an unguided method for glenohumeral injection in the outpatient clinic without special imaging equipment. By removing the barriers associated with radiographic guidance, this technique allows glenohumeral injections to be performed more routinely to treat patients with idiopathic adhesive capsulitis.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. This work was supported by the National Natural Science Foundation of China (81171706). Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The transcoracoacromial ligament glenohumeral injection technique can be performed without radiographic guidance by using the bony surface landmarks of the shoulder. The patient is positioned supine with the arm at the side, keeping the palm externally rotated and the head facing up in a neutral position. The video shows the steps of the technique performed on the patient's left shoulder. (1) Identification of the acromion (ACA), the curved depression of the distal clavicle (CDDC), and the superior lateral border of the coracoid tip (SLBCT). (2) Identification of needle insertion site at the junction between the distal and middle thirds of line SLBCT-CDDC. (3) Insertion of a 22-gauge spinal needle at insertion site with the trajectory perpendicular to the marked triangle. (4) Advancement of the needle toward the humeral head until the humeral head cartilage is reached. (5) Injection of medication including local anesthetic, corticosteroid, and/or hyaluronic acid. (6) Removal of the needle and appropriate care as needed.
References
- 1.McFarland E., Bernard J., Dein E., Johnson A. Diagnostic injections about the shoulder. J Am Acad Orthop Surg. 2017;25:799–807. doi: 10.5435/JAAOS-D-16-00076. [DOI] [PubMed] [Google Scholar]
- 2.Kane D., Koski J. Musculoskeletal interventional procedures: With or without imaging guidance? Best Pract Res Clin Rheumatol. 2016;30:736–750. doi: 10.1016/j.berh.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Amber K.T., Landy D.C., Amber I., Knopf D., Guerra J. Comparing the accuracy of ultrasound versus fluoroscopy in glenohumeral injections: A systematic review and meta-analysis. J Clin Ultrasound. 2014;42:411–416. doi: 10.1002/jcu.22154. [DOI] [PubMed] [Google Scholar]
- 4.Mattie R., Kennedy D.J. Importance of image guidance in glenohumeral joint injections: Comparing rates of needle accuracy based on approach and physician level of training. Am J Phys Med Rehabil. 2016;95:57–61. doi: 10.1097/PHM.0000000000000338. [DOI] [PubMed] [Google Scholar]
- 5.Simoni P., Grumolato M., Malaise O., Preziosi M., Pasleau F., de Lemos Esteves F. Are blind injections of gleno-humeral joint (GHJ) really less accurate imaging-guided injections? A narrative systematic review considering multiple anatomical approaches. Radiol Med. 2017;122:656–675. doi: 10.1007/s11547-017-0772-4. [DOI] [PubMed] [Google Scholar]
- 6.Song A., Katz J.N., Higgins L.D., Newman J., Gomoll A., Jain N.B. Outcomes of ultrasound-guided glen humeral corticosteroid injections in adhesive capsulitis. Br J Med Res. 2014;5:570–578. doi: 10.9734/BJMMR/2015/13478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho C.-H., Kim D.H., Bae K.-C., Lee D., Kim K. Proper site of corticosteroid injection for the treatment of idiopathic frozen shoulder: Results from a randomized trial. Joint Bone Spine. 2016;83:324–329. doi: 10.1016/j.jbspin.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 8.Shao X., Shi L.L., Wang P., Zou F., Wang J. Transcoracoacromial ligament glenohumeral injection technique: Accuracy of 116 injections in idiopathic adhesive capsulitis. Arthroscopy. 2018;34:2337–2344. doi: 10.1016/j.arthro.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 9.Xiao R.C., Walley K.C., DeAngelis J.P., Ramappa A.J. Corticosteroid injections for adhesive capsulitis: A review. Clin J Sport Med. 2017;27:308–320. doi: 10.1097/JSM.0000000000000358. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The transcoracoacromial ligament glenohumeral injection technique can be performed without radiographic guidance by using the bony surface landmarks of the shoulder. The patient is positioned supine with the arm at the side, keeping the palm externally rotated and the head facing up in a neutral position. The video shows the steps of the technique performed on the patient's left shoulder. (1) Identification of the acromion (ACA), the curved depression of the distal clavicle (CDDC), and the superior lateral border of the coracoid tip (SLBCT). (2) Identification of needle insertion site at the junction between the distal and middle thirds of line SLBCT-CDDC. (3) Insertion of a 22-gauge spinal needle at insertion site with the trajectory perpendicular to the marked triangle. (4) Advancement of the needle toward the humeral head until the humeral head cartilage is reached. (5) Injection of medication including local anesthetic, corticosteroid, and/or hyaluronic acid. (6) Removal of the needle and appropriate care as needed.